Abstract
Background One of the surgical treatment options for trapeziometacarpal (TMC) joint arthritis is a prosthetic ball-and-socket replacement. One of the complications in the postoperative setting is de Quervain tendinopathy.
Purposes Although this complication has been reported following a resection athroplasty, we questioned whether lengthening of the thumb following the Ivory (Memometal, Stryker Corporate, Kalamazoo, MI, USA) ball-and-socket arthroplasty could be a causal factor.
Methods In a prospective study regarding the overall outcome of the Ivory prosthesis, we analyzed 96 cases (83 patients; 69 female, 12 male, 8 bilateral) of primary implanted Ivory prosthesis and the incidence of de Quervain disease during the first year following surgery. We found a particularly high incidence (17%) of de Quervain tendinopathy the first year following this ball-and-socket arthroplasty. We measured the lengthening of the thumb radiographically in the group presenting de Quervain and the asymptomatic group and compared this measure between the two groups.
Results We did not find any measurable or statistically significant difference between the groups regarding lengthening.
Discussion These findings suggest that lengthening of the thumb following ball-and-socket arthroplasty is not a causal factor in the development of de Quervain tendinopathy within one year after surgery.
Keywords: trapeziometacarpal, ball-and-socket prosthesis, lengthening, de Quervain
Osteoarthritis at the base of the thumb can cause severe pain, weakness, and deformity and can result in marked disability. Shear stress forces, due to weakening of the palmar beak ligament, can cause damage to the articular cartilage that can progress to degenerative osteoarthritis.1
Initially, osteoarthritis of the trapeziometacarpal (TMC) joint should be treated conservatively. Surgery has been suggested in cases of pain that hampers the activities of daily life. In one study, patients treated conservatively had subjectively worse results than patients who underwent surgery.2
In most cases of basal joint osteoarthritis, surgery can be an option at stages II, III, and IV, as classified by Eaton.3
Indications for surgery in TMC arthritis are similar to the indications for arthroplasty of most joints: persistent pain, decreased function, instability, and failure of conservative management.
Many designs of carpometacarpal (CMC) arthroplasty as a treatment for end-stage TMC osteoarthritis have emerged in recent years. Vermeulen et al concluded in their systematic review that there exists no definite evidence that the arthroplasties are superior to alternative treatment methods such as a trapeziectomy, but they stipulated also that a prosthesis could have better outcome than the trapeziectomy, at least in the short term.1 In addition, the decreased rates of implant failure in recent studies suggest that improved newer total joint prostheses could have a significant positive effect on outcome.1 4 5
Total joint arthroplasty of the TMC joint was first described by de la Caffinnière.6 This procedure applies the same concept as a total hip replacement by creating a permanent swivel within the base of the thumb that obviates the need for ligament reconstruction, replaces the joint surface with a mechanical bearing surface, and provides stability for strong pinch and grasp.7
The aim of our study was to evaluate in a prospective single-center cohort study the overall midterm outcome of the Ivory (Memometal, Stryker Corporate, Kalamazoo, MI, USA) arthroplasty for TMC arthritis, specifically the incidence of de Quervain tenosynovitis within one year after an implantation of an Ivory prosthesis (Fig. 1) and its possible relation regarding lengthening of the thumb following this type of arthroplasty.
Fig. 1.

Ivory ball-and-socket TMC prosthesis.
Therefore we prospectively evaluated 121 cases of TMC prosthetic joint replacement between March 2005 and June 2010.
De Quervain tendinopathy is a stenosing condition of the first dorsal compartment of the wrist. Pain results from resisted gliding of the abductor pollicis longus (APL) and the extensor pollicis brevis (EPB) tendon in the fibro-osseus canal at zone 7 of the extensors of the upper limb. Finkelstein's test is considered to be a pathognomonic sign of this diagnosis.8 Other tests that can be used to assess de Quervain disease are the Eichhoff test,9 which is often confused with the Finkelstein; the Brunelli test10; the EPB entrapment test11; and, recently, wrist hyperflexion and abduction of the thumb (WHAT)test.12
Material and Methods
Study Design
In a prospective single-center cohort study regarding the overall outcome of the Ivory ball-and-socket arthroplasty, we also evaluated (over a period of 5 years and 3 months) 121 cases (a cohort of 106 patients) of TMC joint prosthetic replacement and the incidence of de Quervain disease during the first year following surgery.
All patients presented with an isolated TMC arthritis stage II and III according to Dell et al13 and were treated surgically using the Ivory ball-and-socket prosthesis. The arthroplasty is composed of an anatomical hydroxyapatite-covered metal stem, a double-coned hydroxyapatite-covered cup, and an ultrahigh-molecular-weight (UHMW)-polyethylene liner. Modularity is possible with different neck heights (short, medium, long). In addition, the neck can be fixed on the stem in different rotations (–30°, 0°, +30°) (Fig. 1).
Previous ethical approval had been obtained in accordance with the requirements of the local ethics committee.
Patients: Inclusion Criteria
To guarantee precise comparative measurements preoperatively and postoperatively, we excluded all cases that did not have their preoperative X-rays at the radiology department of our institution. Out of the 121 cases (106 patients) operated during the mentioned period, 96 cases (83 patients), all of whom had a primary Ivory prosthesis implanted, were included in the study (69 females, 12 male, 8 bilateral). They all had their radiographies done preoperatively at our institution at the radiology department on the same device (Definium 8000, General Electric, Fairfield, CT, USA). The routine preoperative radiologic examination included a frontal view and a profile view according to Kapandji et al,14 Eaton views with and without stress, and a Bett view15 of the scaphotrapeziotrapezoid (STT) interval in radial and ulnar deviation.
Operative Technique
The procedure was performed under local-regional anesthesia using a plexic block and in a nonambulatory setting.
Before the surgical procedure was commenced, a mark was drawn on the skin of the index finger to indicate the length of the thumb column prior to the arthroplasty; comparison with this after the procedure would provide an indication of the appropriate lengthening required during prosthesis implantation.
The procedure began by exposing the TMC joint through an anterolateral approach according to the incision described by Gedda and Moberg16 (Fig. 2). This incision provides excellent visualization of the TMC joint and preserves the dorsal vascularity and ligamentous stability of the saddle joint. Injury to the palmar branch of the superficial radial nerve is avoided by direct meticulous exposure. Some anterior branches of the superficial branch are sacrificed.16 The APL slip to the opponens is de-inserted. The opponens and APL origin are then dissected from the anterior side of the TMC joint. The capsule is opened longitudinally, and the base of the thumb metacarpal is freed anterolaterally from all of its ligamentous and capsular attachments. The trapezium is also well exposed on its anterior side.
Fig. 2.
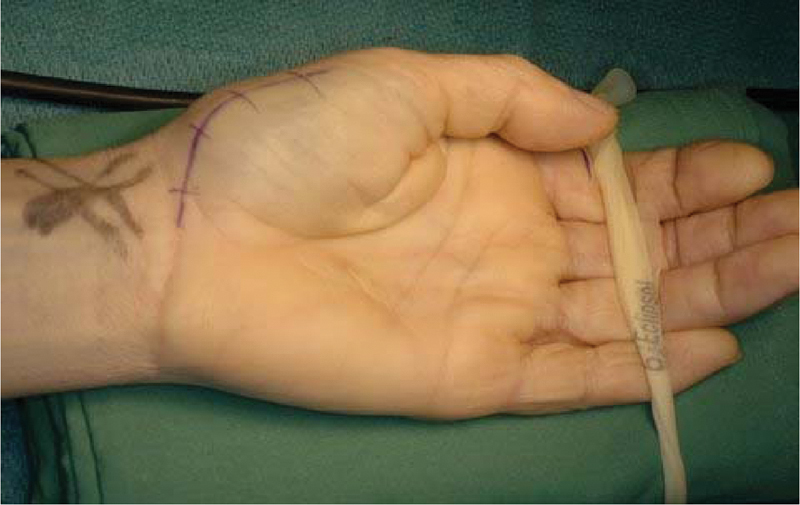
Anterolateral approach according to Gedda and Moberg.
Then, the Ivory prosthesis is put in place according to the manufacturer's instructions.17
Finally, the length of the thumb is measured such that its length is comparable with that at its preoperative measurement. The opponens slip of the APL is reinserted with Vicryl (Ethicon, Johnson & Johnson Inc., New Brunswick, NJ, USA) 3/0 cross stitches to obtain a hermetic closure of this junction. The incised skin is then closed with Ethylon (Ethicon, Johnson & Johnson Inc., New Brunswick, NJ, USA) 5.0 sutures, and a suction drain is left in situ. The hand is placed in a soft bandage and a forearm plaster cast taking the thumb.
Postoperative Care
The suction drain is removed 24 hours after surgery. A forearm cast is then applied that includes the metacarpophalangeal joint of the thumb but spares the interphalangeal joint. The cast remains in place for 3 weeks. Autogenous rehabilitation begins after 3 weeks in all and patients are told to avoid forceful pollicidigital gripping for 3 months. A removable thumb splint in thermoplastic material (Orfit, Orfit Industries, Wijnegem, Belgium) is provided to address periods between autogenous rehabilitation, for an additional month. No hand therapy program is necessary because autogenous rehabilitation enabled sufficient progress in recovery. After 3 months, normal occupational activities could be resumed. Patients were followed up on the first day postoperatively; at 10 days, 3 weeks, 6 weeks, 3 months, and 6 months; and thereafter annually with radiological records.
Methods
Patients presenting within the first year following surgery with spontaneous pain over the radial styloid were examined for de Quervain disease: local tenderness, swelling, painful mobilization of the thumb in ulnar deviation, and a positive Eichhoff test.9
All patients presenting with these signs and symptoms had an ultrasound at the radiology department of our institution. Confirmation by the radiologist yielded a positive diagnosis of de Quervain disease.18 19 20 21 22 23 24
Radiographic Analysis
All radiographs of the included cases were analyzed. Preoperative and postoperative radiographies in profile according to Kapandji et al14 were evaluated by one investigator: the distance between the subchondral line of the tuberculum of the scaphoid and the subchondral line of the head of the thumb metacarpal was measured preoperatively (a1/a2) (Fig. 3) and postoperatively (a1́/a2́) (Fig. 4).
Fig. 3.

a1/a2 interval length preoperatively measured in Kapandji profile view (superposition of the sesamoids).
Fig. 4.

a1'/a2' interval length postoperatively measured in Kapandji profile view (superposition of the sesamoids).
Individual Length measurement was performed by one investigator on digital radiographies (IMPAX 6.5.1.144, Agfa Healthcare, Mortsel, Belgium) pre- and postoperatively and compared.
Data Analysis
The difference in length of the metacarpal between pre- and postoperative was compared using a paired Student t-test, assuming equal variance, with post hoc tests for homogeneity of variance. The pre- and postoperative lengths of the de Quervain and non–de Quervain groups were also compared in the same way. Finally, the length of time after surgery at which de Quervain disease developed was correlated with the length difference between pre- and postoperative using a Pearson's r-test.
Results
The average onset of symptoms within the whole population was 3 months (range 1–12 months).
Ninety-six cases were finally included in the study. Fourteen cases (all female) presented with symptoms of de Quervain that were confirmed using ultrasound within the first year following surgery. The average age of the 83 patients was 60 years (range 33 to 88 years).
No male subjects developed de Quervain disease. The condition was addressed by an operation in 3 cases, while 11 healed with conservative treatment (corticoid infiltration and splinting). The average age of the population that developed de Quervain disease was 56 years (range 43–71), and the average age of the population that did not develop de Quervain disease was 61 years (range 33–84). Dominancy within the affected group was left side for 3 patients and right side for 11 patients. One patient was ambidextrous. Eight were affected on their dominant side (including the ambidexter) and 6 on the non-dominant side. Ten patients were manual workers: blue collar and housewives, 2 were white-collar workers, 2 were retired, and one subject was unemployed (Table 1). The average increase in length of the metacarpal of the affected group was 5.5 mm (range 2.3–8 mm), while the average increase of in length of the metacarpal of the non-affected group was 5.3 mm (range 0–14.6). Distribution regarding length preoperatively, postoperatively, and change in length is shown in Figs. 5, 6, and 7.
Table 1. Distribution of patients with and without de Quervain according to gender, age, activity, dominancy, affected limb, and increase in length.
| With dQ | Without dQ | |
|---|---|---|
| Gender | ||
| Male | 0 | 12 |
| Female | 14 | 70 |
| Age | ||
| Average age | 56 | 61 |
| Youngest | 43 | 33 |
| Oldest | 71 | 84 |
| Activities | ||
| Blue collar | 5 | 15 |
| White collar | 1 | 14 |
| Housewife/retired | 7 | 49 |
| Unemployed | 1 | 4 |
| Dominance | ||
| Left | 3 | 7 |
| Right | 11 | 69 |
| Ambidexter | 0 | 6 |
| Affected | ||
| Dominant | 8 | 29 |
| Nondominant | 6 | 47 |
| Ambidexter | 0 | 6 |
| Increase in length | ||
| Average | 5,5 | 5,3 |
| Shortest | 2,3 | 0 |
| Longest | 8 | 14,3 |
Fig. 5a, b.
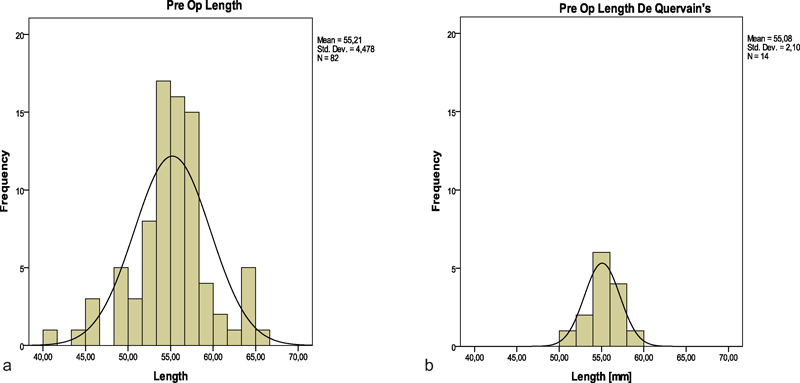
Preoperative length distributions within (a) the group without de Quervain and (b) the group with de Quervain disease.
Fig. 6a, b.
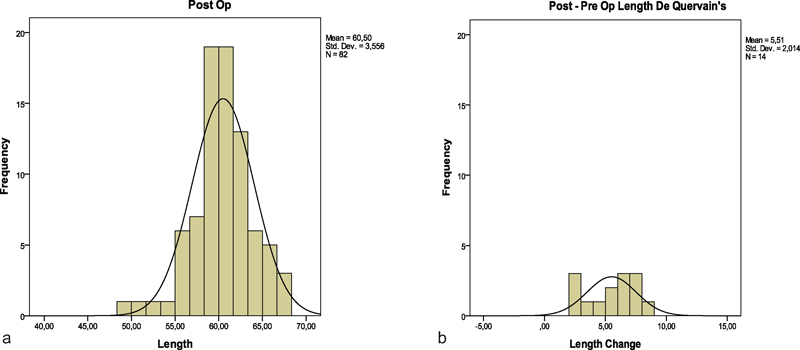
Postoperative length distribution within (a) the group without de Quervain, (b) and the group with de Quervain disease.
Fig. 7a, b.
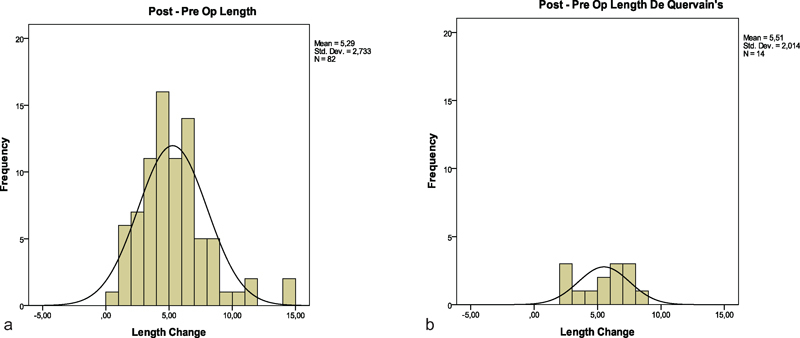
Difference in length distribution between a1'/a2' and a1/a2 in (a) the group without de Quervain and (b) the group with de Quervain.
The results show no significant difference between the two groups. There is no significant difference between the groups in the means of either the preoperative or postoperative data or the changes in length of the metacarpal pre- to postoperative between the groups. There is a difference in the mean change in length (nonsignificant) of around 0.2 mm, but this was within the measurement error.
There is also no significant correlation between the length of time after surgery and the length difference pre- to postoperative in the de Quervain group.
The difference in length increase between the population presenting with de Quervain disease and the nonaffected group was not statistically significant to correlate between the increase in length and the onset of de Quervain disease.
Discussion
As a possible cause for the development of de Quervain tendinopathy, after prosthetic arthroplasty, we focused on the increase in length of the thumb following the prosthetic replacement and the presence/absence of de Quervain disease.
The difference in length increase between the two groups in the study was, however, not statistically significant. On the basis that there is no difference in the change in length between the two groups, it would seem unlikely that the length change pre- to postoperative (which is a significant change in both groups) is a causative factor in the development of de Quervain disease. No studies have been reported comparing the lever arm at different lengths of the thumb and the incidence of de Quervain disease.
Very little is known about the occurrence of de Quervain disease after TMC arthroplasty within one year of follow-up. In examining the literature for a relationship between TMC osteoarthritis and the onset of de Quervain tenosynovitis after TMC arthroplasty, we only found two articles mentioning de Quervain disease as a complication after TMC arthroplasty.25 26
Amadio et al reported, in a retrospective study comparing a silicone spacer with a tendon spacer for trapezium resection arthroplasty, that three patients in the nonimplant group developed de Quervain tenosynovitis postoperatively. They confirmed de Quervain disease by surgical exploration, and each case revealed inflammation around the shortened, resutured abductor tendon slips, which, because of their increased bulk, were unable to pass smoothly through the first dorsal compartment.25 This feature is biomechanically understandable, since the resection of the trapezium implies a sagging of the base of the thumb metacarpal of variable importance. In that way it is unlikely that prosthetic interposition arthroplasty would enhance this type of conflict.
Ulrich-Vinther et al26 reported tendon problems as a complication after joint arthroplasty in their prospective 1-year follow-up study, comparing joint prosthesis with tendon interposition arthroplasty in 2008. Within 5 months after surgery, they reported two patients with a joint prosthesis and five patients with an interposition arthroplasty who went on to develop de Quervain tenosynovitis.26 The studies of Ulrich-Vinther and Amadio suggest that de Quervain tenosynovitis can occur either in resection arthroplasty with tendon interposition or in total joint replacement of the thumb.
Our results suggest that the incidence of de novo de Quervain tendinopathy following trapeziometacarpal arthroplasty should not be neglected, since 15% of our cases developed a de Quervain tenosynovitis.
We were not able to find a significant difference in thumb lengthening after prosthetic joint replacement between the patients presenting de Quervain tenosynovitis after joint replacement and those not presenting with the symptoms.
The epidemiology of de Quervain tenosynovitis in a normal population is not well known according to the literature.27 In a study performed in 2006 in the Loire region of France, prevalence of de Quervain was 0.7% in men and 2.1% in women.28 The researchers report a prevalence of 4.5% in a segment of population of 50 to 59 years. This is significantly less than what we incidentally found in our series (17%). Wolfe et al report in a very large military database a detailed distribution of the incidence regarding age, race, rank, and years of service between male and female patients. They found the highest incidence rate ratio within the population older than 40 years, with an overall incidence rate of 1.37 per 1000 person years. However, all studies report a majority of female involvement regarding de Quervain disease.29
The pathophysiology of de Quervain disease is characterized by noninflammatory fibrosis of the tenosynovium. The etiology is presumed to be related to repetitive motion.30 The majority of patients presenting with de Quervain disease were female manual workers, which tends to support this theory.
The distribution of tendons within the first extensor compartment is also variable. Brunelli et al31 describe only one APL tendon in 2% of the dissected cadavers. In their study they found on average four or more tendon slips of the APL tendon in the first extensor compartment. The EPB tendon is present as a single tendon up to 96% of the surgical cases.32
Septation between the EPB and APL tendons in the first dorsal compartment is common. The incidence of the septum in cadaver studies varies from 24% to 77.5%. Ultrasound evaluation reports up to 73% of septation within the first extensor compartment.33 Most surgical series, however, report the presence of such a septum in 58 to 60% of cases,32 34 and therefore some investigators have suggested that the septum might play an important role in the etiology of the condition. Yet, following these suggestions, a human cadaver model study showed that septation and wrist position had a deleterious impact on the gliding capacity of the tendons of the first extensor compartment.30
Although the etiology of de Quervain disease is unknown, we hypothesize that its origin has different possible manifestations. In this study, the surgical approach proposed by Gedda and Moberg16 involves a deinsertion of (one of the) tendon(s) of the APL and its reinsertion at the end of the surgical procedure. This could be part of the trigger in developing de Quervain disease by augmenting the gliding resistance, since a perfect isometric reinsertion of the APL is not feasible. Concomitant diseases such as intersection syndrome and Wartenberg syndrome have been described together with de Quervain's disease.23 However, the combination of arthritis of the TMC joint and de Quervain disease has not, to our knowledge, been reported in the literature. This feature could illustrate the subsequent important lack of mobilization and subsequent antalgic decrease of power in the thumb in movements that frequently involve the tendons of the first extensor compartment.
Thus we could put forward the hypothesis that following prosthetic replacement of the TMC joint the quick relief of pain, the increased mobility of the TMC joint following a rather long interval of reduced function and mobility, and the adaptation of the structures to the new situation could increase the risk of developing de Quervain disease. That is, after a long period of decreased activity around the TMC joint due to arthritic pain, facilitating stenosis and adherences within the structures composing the first extensor compartment, a sudden increase in mobility (lengthening or activity) of the tendons might be the source of a de Quervain disease. The adaptation to the new anatomic situation (the prosthetic implant) might play a role in developing this symptomatology. Indeed, a majority of cases were diagnosed within 3 months following the procedure. Moreover, Domalain et al35 showed that, in a computer simulation, the muscle forces increased dramatically (up to 12 times that of normal) in the ball-and-socket TMC arthroplasty. They even stated that the large TMC joint forces found in their study could be related to the prevalence of implant dislocation. The results of this computational study have to be interpreted cautiously, because it does not address the reality each may encounter with an actual surgery.
On the other hand, the use of the anterior approach could be a trigger in developing the condition, since using this it is necessary to deinsert the APL partially, and reinsert it at the end of the surgical procedure. Many recent reports regarding various ball-and-socket replacements did not report any de Quervain disease following this type of surgery. All these reports used a dorsoradial incision between EPB and APL.36 37 38 39 40 41 42 The only study using a posterolateral approach for implantation of a ball and socket prosthesis and reporting de Quervain in the first year following implantation was that of Ulrich-Vinther et al.26
The unique mobility of the thumb contributes to the syndrome.43 An awkward wrist position is also generally accepted as a condition related to de Quervain disease. The specific position of risk is controversial. Some authors have stated that the repeated use of firm grasp, together with ulnar deviation of the wrist, could predispose to de Quervain disease. Others have reported an association with radial deviation.44 45 46 47 TMC arthroplasty corrects the adduction deformity of the thumb induced by the carpometacarpal osteoarthritis. If corrected, the tension load on the first dorsal compartment tendons changes significantly compared with the chronically deformed condition. Alternating friction levels may predispose the tenosynovium to mechanical injury.6 30 The results obtained in this study give us neither a statistical nor a measurable significant difference in lengthening between the group who develop de Quervain disease and those who do not after TMC arthroplasty. Moreover, all affected patients were female, and a majority were manual workers, implying that repetitive manual tasks coupled to an increase in power grip are likely to be factors in the development of de Quervain disease.
Other reasons for the development of de Quervain tenosynovitis, such as the increase in activity of the thumb after successful surgery that eliminates preoperative longstanding pain and antalgic lack of movement, cannot be ruled out. A significant limitation of the study is that it was not a controlled trial. In conclusion, we suggest that pain relief following the ball-and-socket prosthetic arthroplasty and the increase in muscle force and adapted activity might be a possible cause of de Quervain tendinopathy. According to this study, however, it seems unlikely that the metacarpal length change pre- to postoperative (which is significant in both groups) is a causative factor in the development of de Quervain disease.
Acknowledgments
The authors would like to thank Kim Jones, PhD, and Malcolm Forward, PhD, C.Eng., for the statistics and help in writing this manuscript. Thanks to Sofia Pensaert for verifying and correcting the manuscript.
Footnotes
Funding This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Ethical Approval This study received the approval of the Leading Ethics Committee OG 065 of the AZ Sint–Jan AV Brugge–Oostende, campus Brugge, Brugge, Belgium. Conflict of Interest Jean F Goubau is financially supported by Stryker Corporate, Kalamazoo, Michigan, USA, and his payment from the company consists only of expenses for these demonstrations and attending the French Hand Society and European Hand Surgery congresses.
References
- 1.Vermeulen G M, Slijper H, Feitz R, Hovius S ER, Moojen T M, Selles R W. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011;36(1):157–169. doi: 10.1016/j.jhsa.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 2.Damen A, Withag K M, van der Lei B, den Dunnen W FA, Robinson P H. Conservative treatment of CMC-1 osteoarthritis. Eur J Plast Surg. 2001;24:33–37. [Google Scholar]
- 3.Eaton R G, Glickel S Z. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin. 1987;3(4):455–471. [PubMed] [Google Scholar]
- 4.Martou G, Veltri K, Thoma A. Surgical treatment of osteoarthritis of the carpometacarpal joint of the thumb: a systematic review. Plast Reconstr Surg. 2004;114(2):421–432. doi: 10.1097/01.prs.0000131989.86319.b1. [DOI] [PubMed] [Google Scholar]
- 5.Wajon A, Ada L, Edmunds I. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2005;(4):CD004631. doi: 10.1002/14651858.CD004631.pub2. [DOI] [PubMed] [Google Scholar]
- 6.de la Caffiniere J Y, Aucouturier P. Trapezio-metacarpal arthroplasty by total prosthesis. Hand. 1979;11(1):41–46. doi: 10.1016/s0072-968x(79)80007-8. [DOI] [PubMed] [Google Scholar]
- 7.Cooney W P, Linscheid R L, Askew L J. Total arthroplasty of the thumb trapeziometacarpal joint. Clin Orthop Relat Res. 1987;(220):35–45. [PubMed] [Google Scholar]
- 8.de Quervain F. On a form of chronic tendovaginitis by Dr. Fritz de Quervain in la Chaux-de-Fonds. 1895. Am J Orthop. 1997;26(9):641–644. [PubMed] [Google Scholar]
- 9.Eichhoff E. Zur pathogenese der Tenovaginitis stenosans. Bruns Beitr Klin Chir. 1927;139:746–755. [Google Scholar]
- 10.Brunelli G. Finkelstein's versus Brunelli's test in De Quervain tenosynovitis [in French] Chir Main. 2003;22(1):43–45. doi: 10.1016/s1297-3203(02)00005-7. [DOI] [PubMed] [Google Scholar]
- 11.Alexander R D, Catalano L W, Barron O A, Glickel S Z. The extensor pollicis brevis entrapment test in the treatment of de Quervain's disease. J Hand Surg Am. 2002;27(5):813–816. doi: 10.1053/jhsu.2002.35309. [DOI] [PubMed] [Google Scholar]
- 12.Goubau J F Goubau L Van Tongel A Van Hoonacker P Kerckhove D Berghs B The wrist hyperflexion and abduction of the thumb (WHAT) test: a more specific and sensitive test to diagnose de Quervain tenosynovitis than the Eichhoff's test J Hand Surg Eur Vol 201439E3[Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Dell P C, Brushart T M, Smith R J. Treatment of trapeziometacarpal arthritis: results of resection arthroplasty. J Hand Surg Am. 1978;3(3):243–249. doi: 10.1016/s0363-5023(78)80088-4. [DOI] [PubMed] [Google Scholar]
- 14.Kapandji A I, Kapandji T G. New radiologic data on the trapezo-metacarpal joint. The results of 330 cases [in French] Ann Chir Main Memb Sup. 1993;4:263–274. doi: 10.1016/s0753-9053(05)80025-0. [DOI] [PubMed] [Google Scholar]
- 15.Taleisnik J. New York, NY: Churchill Livingstone; 1985. The Wrist. 1st ed; pp. 95–96. [Google Scholar]
- 16.Gedda K O, Moberg E. Open reduction and osteosynthesis of the so-called Bennett's fracture in the carpo-metacarpal joint of the thumb. Acta Orthop Scand. 1952;22(1-4):249–257. doi: 10.3109/17453675208989009. [DOI] [PubMed] [Google Scholar]
- 17.Goubau J F, Goorens C K, Van Hoonacker P, Berghs B, Kerckhove D, Scheerlinck T. Clinical and radiological outcomes of the Ivory arthroplasty for trapeziometacarpal joint osteoarthritis with a minimum of 5 years of follow-up: a prospective single-centre cohort study. J Hand Surg Eur Vol. 2013;38:866–874. doi: 10.1177/1753193413488494. [DOI] [PubMed] [Google Scholar]
- 18.Luchetti R, Atzei A, Fairplay T A. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. Tendon disorders: de Quervain's disease, trigger finger, and generalized tenosynovitis; pp. 779–997. [Google Scholar]
- 19.Giovagnorio F, Andreoli C, De Cicco M L. Ultrasonographic evaluation of de Quervain disease. J Ultrasound Med. 1997;16(10):685–689. doi: 10.7863/jum.1997.16.10.685. [DOI] [PubMed] [Google Scholar]
- 20.Grassi W, Filippucci E, Farina A, Cervini C. Sonographic imaging of tendons. Arthritis Rheum. 2000;43(5):969–976. doi: 10.1002/1529-0131(200005)43:5<969::AID-ANR2>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 21.Kamel M, Moghazy K, Eid H, Mansour R. Ultrasonographic diagnosis of de Quervain's tenosynovitis. Ann Rheum Dis. 2002;61(11):1034–1035. doi: 10.1136/ard.61.11.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diop A N, Ba-Diop S, Sane J C. et al. Role of ultrasound in the management of de Quervain's tenosynovitis: review of 22 cases [in French] J Radiol. 2008;89(9 Pt 1):1081–1084. doi: 10.1016/s0221-0363(08)73912-x. [DOI] [PubMed] [Google Scholar]
- 23.De Maeseneer M, Marcelis S, Jager T, Girard C, Gest T, Jamadar D. Spectrum of normal and pathologic findings in the region of the first extensor compartment of the wrist: sonographic findings and correlations with dissections. J Ultrasound Med. 2009;28(6):779–786. doi: 10.7863/jum.2009.28.6.779. [DOI] [PubMed] [Google Scholar]
- 24.Volpe A, Pavoni M, Marchetta A. et al. Ultrasound differentiation of two types of de Quervain's disease: the role of retinaculum. Ann Rheum Dis. 2010;69(5):938–939. doi: 10.1136/ard.2009.123026. [DOI] [PubMed] [Google Scholar]
- 25.Amadio P C, Millender L H, Smith R J. Silicone spacer or tendon spacer for trapezium resection arthroplasty—comparison of results. J Hand Surg Am. 1982;7(3):237–244. doi: 10.1016/s0363-5023(82)80173-1. [DOI] [PubMed] [Google Scholar]
- 26.Ulrich-Vinther M, Puggaard H, Lange B. Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J Hand Surg Am. 2008;33(8):1369–1377. doi: 10.1016/j.jhsa.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 27.Wolf J M, Sturdivant R X, Owens B D. Incidence of de Quervain's tenosynovitis in a young, active population. J Hand Surg Am. 2009;34(1):112–115. doi: 10.1016/j.jhsa.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 28.Roquelaure Y, Ha C, Leclerc A. et al. Epidemiologic surveillance of upper-extremity musculoskeletal disorders in the working population. Arthritis Rheum. 2006;55(5):765–778. doi: 10.1002/art.22222. [DOI] [PubMed] [Google Scholar]
- 29.Lane L B, Boretz R S, Stuchin S A. Treatment of de Quervain's disease:role of conservative management. J Hand Surg [Br] 2001;26(3):258–260. doi: 10.1054/jhsb.2001.0568. [DOI] [PubMed] [Google Scholar]
- 30.Kutsumi K, Amadio P C, Zhao C, Zobitz M E, An K N. Gliding resistance of the extensor pollicis brevis tendon and abductor pollicis longus tendon within the first dorsal compartment in fixed wrist positions. J Orthop Res. 2005;23(2):243–248. doi: 10.1016/j.orthres.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 31.Brunelli G A, Brunelli G R, Mattiuzzo V. Trapezio metacarpal instability and arthritis: etiopathogenetic interpretation and surgical technique. Surg Technol Int. 1995;IV:435–439. [PubMed] [Google Scholar]
- 32.Bahm J, Szabo Z, Foucher G. The anatomy of de Quervain's disease. A study of operative findings. Int Orthop. 1995;19(4):209–211. doi: 10.1007/BF00185223. [DOI] [PubMed] [Google Scholar]
- 33.Choi S J, Ahn J H, Lee Y J. et al. de Quervain disease: US identification of anatomic variations in the first extensor compartment with an emphasis on subcompartmentalization. Radiology. 2011;260(2):480–486. doi: 10.1148/radiol.11102458. [DOI] [PubMed] [Google Scholar]
- 34.Kulthanan T, Chareonwat B. Variations in abductor pollicis longus and extensor pollicis brevis tendons in the Quervain syndrome: a surgical and anatomical study. Scand J Plast Reconstr Surg Hand Surg. 2007;41(1):36–38. doi: 10.1080/02844310600869720. [DOI] [PubMed] [Google Scholar]
- 35.Domalain M F, Seitz W H, Evans P J, Li Z M. Biomechanical effect of increasing or decreasing degrees of freedom for surgery of trapeziometacarpal joint arthritis: a simulation study. J Orthop Res. 2011;29(11):1675–1681. doi: 10.1002/jor.21453. [DOI] [PubMed] [Google Scholar]
- 36.Seng V S, Chantelot C. Isis(®) trapeziometacarpal prosthesis in basal thumb osteoarthritis: 30 months follow-up in 30 cases [in French] Chir Main. 2013;32(1):8–16. doi: 10.1016/j.main.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 37.Hernández-Cortés P, Pajares-López M, Robles-Molina M J, Gómez-Sánchez R, Toledo-Romero M A, De Torres-Urrea J. Two-year outcomes of Elektra prosthesis for trapeziometacarpal osteoarthritis: a longitudinal cohort study. J Hand Surg Eur Vol. 2012;37(2):130–137. doi: 10.1177/1753193411414505. [DOI] [PubMed] [Google Scholar]
- 38.Regnard P J. Electra trapezio metacarpal prosthesis: results of the first 100 cases. J Hand Surg [Br] 2006;31(6):621–628. doi: 10.1016/j.jhsb.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 39.Klahn A, Nygaard M, Gvozdenovic R, Boeckstyns M EH. Elektra prosthesis for trapeziometacarpal osteoarthritis: a follow-up of 39 consecutive cases. J Hand Surg Eur Vol. 2012;37(7):605–609. doi: 10.1177/1753193412443501. [DOI] [PubMed] [Google Scholar]
- 40.Pritchett J W, Habryl L S. A promising thumb basal joint hemiarthroplasty for treatment of trapeziometacarpal osteoarthritis. Clin Orthop Relat Res. 2012;470(10):2756–2763. doi: 10.1007/s11999-012-2367-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hansen T B, Stilling M. Equally good fixation of cemented and uncemented cups in total trapeziometacarpal joint prostheses. A randomized clinical RSA study with 2-year follow-up. Acta Orthop. 2013;84(1):98–105. doi: 10.3109/17453674.2013.765625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eecken S V, Vanhove W, Hollevoet N. Trapeziometacarpal joint replacement with the Arpe prosthesis. Acta Orthop Belg. 2012;78(6):724–729. [PubMed] [Google Scholar]
- 43.Leào L. De Quervain's disease; a clinical and anatomical study. J Bone Joint Surg Am. 1958;40-A(5):1063–1070. [PubMed] [Google Scholar]
- 44.Reid D A, Ellis V H. Stenosing tendovaginitis at the radial styloid process. Review of 30 cases. Lancet. 1951;1(6665):1149–1151. doi: 10.1016/s0140-6736(51)92658-x. [DOI] [PubMed] [Google Scholar]
- 45.Finkelstein H. Stenosing tenovaginitis at the radial styloid process. J Bone Joint Surg Am. 1930;12:509–540. [Google Scholar]
- 46.Lipscomb P R. Stenosing tenosynovitis at the radial styloid process (de Quervain's disease) Ann Surg. 1951;134(1):110–115. doi: 10.1097/00000658-195107000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Muckart R D. Stenosing tendovaginitis of abductor pollicis longus and extensor pollicis brevis at the radial styloid (de Quervain's disease) Clin Orthop Relat Res. 1964;33(33):201–208. [PubMed] [Google Scholar]


