Abstract
Background Union of a scaphoid fracture is difficult to assess on a standard series of radiographs. An unnecessary and prolonged immobilization is inconvenient and may impair functional outcome. Although operative treatment permits early mobilization, its influence on time to union is still uncertain.
Purpose To assess union of scaphoid waist fractures based on computed tomography (CT) scan at 6 weeks, and to compare time to union between conservative treatment and arthroscopically assisted screw fixation.
Patients and methods CT scan in the longitudinal axis of the scaphoid was used to provide fracture characteristics, and to assess bone union at 6 weeks in 65 consecutive patients with scaphoid waist fractures. In a randomized subgroup from this cohort with nondisplaced fractures, we compared time to union between conservative treatment (n = 23) and arthroscopically assisted screw fixation (n = 15).
Results Overall, at 6 weeks we found a 90% union rate for non- or minimally displaced fracture treated conservatively, and 82% for those who underwent surgery. In the randomized subgroup of nondisplaced fractures, no significant difference in time to union was demonstrated between those treated conservatively and those who underwent surgery. The conservatively treated fractures from this subgroup with prolonged time to union (10 to 14 weeks) were comminuted, demonstrating a radial cortical or corticospongious fragment.
Conclusion The majority of non- or minimally displaced scaphoid waist fractures are sufficiently treated with 6 weeks in a cast. Screw fixation does not reduce time to fracture union compared with conservative treatment.
Level of Evidence level II, Therapeutic study
Keywords: arthroscopy, bone union, CT scan, scaphoid fracture, wrist
After adequate conservative or operative management, union is achieved for ∼90% of nondisplaced scaphoid waist fractures,1 2 3 while prolonged time to union as well as a higher nonunion rate were demonstrated for displaced scaphoid fractures.4 5 The serious consequences of nonunion, such as progressive degenerative changes and carpal collapse, have resulted in a restrictive treatment regime with immobilization of nondisplaced scaphoid waist fractures for 8 to 12 weeks.6 7
There is an ongoing debate on the advantages of screw fixation versus conservative management of nondisplaced scaphoid waist fractures. A possible advantage of screw fixation is a reduced time to union, which could allow earlier mobilization and thereby improve functional outcome. However, these benefits may come with an increased rate of complications due to the surgical intervention.8 So far, comparative studies on time to union are mainly based on radiographs and not on computed tomography (CT) scans. Nevertheless, the latter have proven more reliable and accurate in the assessment of scaphoid fracture characteristics and union.9 10 Arthroscopically assisted screw fixation of scaphoid waist fractures is a well-established procedure.11 12 It has numerous advantages compared with an entirely percutaneous technique such as direct visualization of fracture reposition; aids in optimal guide wire positioning, checking countersinking of screw threads, and assessment of fixation stability; and allows evaluation of associated ligament injuries.
We have previously performed a study on consecutive scaphoid fractures, using magnetic resonance imaging (MRI) and CT reconstructions in the coronal and sagittal planes of the wrist.13 Since then, it has been suggested that many scaphoid fractures are probably overtreated and could safely be mobilized much earlier than previously recommended.14 15
The aim of this study was to reevaluate the CT scans obtained at 6 weeks, with reconstruction in the longitudinal axis of the scaphoid, to assess union of the scaphoid waist fractures. Furthermore, from a randomized subgroup of the patients with nondisplaced or minimally displaced scaphoid waist fracture, we were able to evaluate whether time to union differs between conservative management in a cast and arthroscopically assisted screw fixation.
Patients and Methods
During a 4-year period (2004–2008), consecutive patients presenting at our emergency department with posttraumatic radial wrist tenderness were asked to participate in a prospective study on diagnosis and treatment of scaphoid fractures. One study arm encompassed patients with scaphoid waist fracture regardless of the degree of fracture displacement. A subgroup from this prospective cohort with nondisplaced or minimally displaced scaphoid waist fractures (< 1 mm displacement and/or < 15° volar angulation)16 were randomized, using a blinded envelope system, to cast immobilization or arthroscopically assisted screw fixation (Fig. 1). The Regional Ethics Committee at Lund University approved the study (LU 459–03), and written informed consent was obtained from all eligible patients.
Fig. 1.
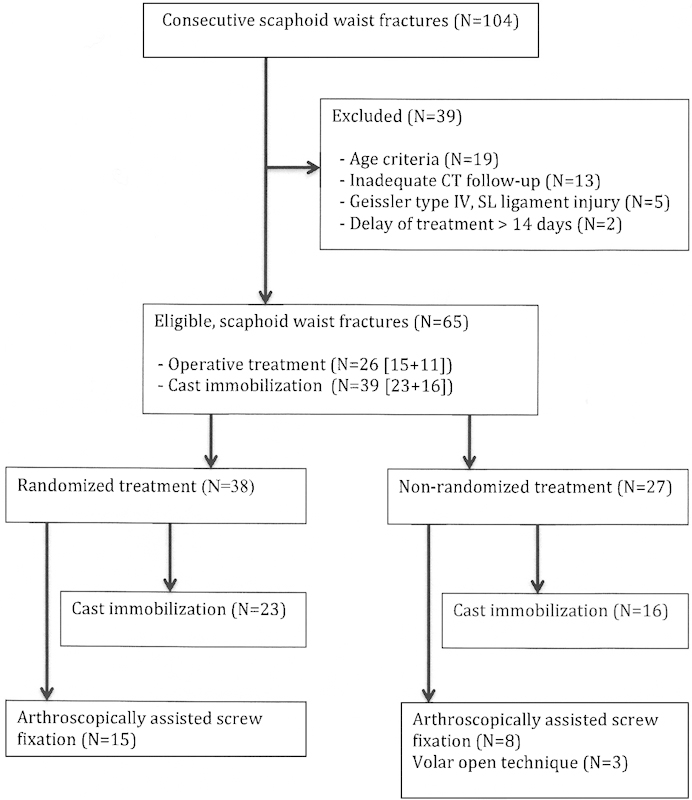
Flowchart of the study.
For the purpose of this study, only patients who, in addition to the initial CT scan, had a CT scan done at 6 weeks of follow-up were included. We excluded patients with a fracture of the distal or proximal third of the scaphoid, associated perilunate injuries, age below 16 or above 65 years, or a delay from injury to treatment of more than 14 days. However, we allowed inclusion of patients with concomitant nondisplaced distal radius or carpal fracture that would not require an immobilization period longer than the one necessary for treatment of the scaphoid fracture. The randomized subgroup of patients with non- or minimally displaced scaphoid waist fracture was followed with CT scans at 10 and 14 weeks and 6 and 12 months.
Imaging Protocol
Conventional radiographs (AXIOM Aristos FX; Siemens AG, Forchheim, Germany) of the wrist, posteroanterior (PA) and lateral projections, were obtained together with four views of the scaphoid (PA with ulnar deviation, with the central beam angled 10° cranially, 10° caudally, 20° ulnarly. and 20° radially). CT (Somatom Sensation 16; Siemens AG, Forchheim, Germany) was performed with the patient positioned prone on the CT table with the arm above the head, the forearm in pronation, and the wrist in neutral flexion and neutral radial-ulnar deviation. Scout images were taken to ensure correct scanning plane. Axial sections of 0.6-mm thick slices were obtained, allowing 1- or 2-mm thick reconstructions in the coronal and sagittal planes defined by the long axis of the scaphoid.
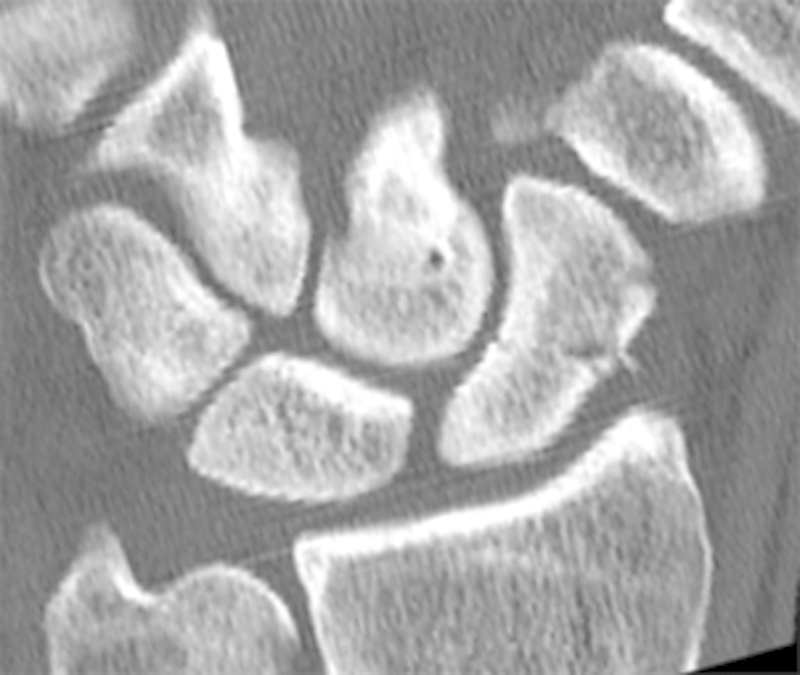
One senior musculoskeletal radiologist (JB), together with one of the senior authors (NT), evaluated all of the radiographic examinations. Fracture gap and translation (step-off) were measured on the coronal and sagittal images of the initial CT scan (Fig. 2). The maximum value measured was used to categorize the fracture as: minimally displaced (≤ 0.5 mm), moderate (1 mm), or severely displaced (≥ 1.5.mm).5 The percentage of bone contact over the fracture cross section at follow-up was graded as 0 to 24%, 25 to 49%, 50 to 74%, 75 to 99%, or 100%.17 The grading was estimated by using average measurements from four sagittal and coronal cuts. Ultimately, it was assessed whether the fracture had united, defined as not just bone contact but as a continuous trabecular pattern over more than 50% of the cross section of the fracture.5 14 Our reference standard to confirm fracture union was based on an additional CT scan obtained at least 6 months after treatment.18
Fig. 2.

Sagittal CT scan of a displaced scaphoid waist fracture demonstrating fracture gap and translation (step-off).
Treatment Regime
Conservative treatment consisted of immobilization in a standard below-elbow plaster cast incorporating the thumb up to the interphalangeal joint.
Using a 2.7-mm arthroscope, standard radiocarpal and midcarpal arthroscopy was performed with the hand in a vertical traction tower. We applied 3 to 5 kg of traction. As needed, blood, debris, and synovitis were removed with a shaver. To allow placement of a guide wire in the central axis of the scaphoid, the wrist was flexed and kept in slight ulnar deviation. Fracture reduction was obtained with a small periosteal elevator inserted through the radial midcarpal portal or by using Kirschner wires (K-wires) as joysticks to manipulate the proximal and distal fragments. For this purpose an additional scaphotrapeziotrapezoid portal was created if required. After fracture reduction a central guide wire was inserted in an antegrade fashion from the proximal to the distal pole. Osteosyntesis was performed with a headless compression screw (HBS 3.0 mm, KLS Martin Group, Mühlheim, Germany, or TwinFix 3.2 mm, Stryker, Kalamazoo, MI, USA). Fracture reduction and position of the compression screw, were confirmed by midcarpal arthroscopy and fluoroscopy at multiple angles. Fracture stability was assessed during arthroscopy by deviating the wrist in ulnar and radial direction, and by manipulating with a probe at the fracture site. When the fracture fixation was considered stable, the wrists of the patients in the randomized group were immobilized in a cast for 2 weeks, followed by wrist mobilization. Those who did belong to the randomized subgroup were immobilized until the treating surgeon considered the fracture to be united. If fracture reduction or stability could not be achieved by the arthroscopic technique, we immediately converted to a standard, open volar approach followed by screw fixation, which was inserted in a retrograde fashion.
Study Population
We identified 103 consecutive patients with 104 scaphoid waist fractures (Fig. 1). Thirteen patients were excluded because of inadequate CT scan follow-up, 19 due to age criterion, two because of a delay in treatment of more than 14 days, and five who had K-wire fixation due to a complete (i.e., Geissler grade IV) scapholunate ligament disruption, found in association with the scaphoid fracture. This left 65 scaphoid fractures in 64 patients who were included in the study. Thirty-nine fractures (34 males and 5 females, median age of 28, range 17 to 62 years) were treated conservatively in a plaster cast. Twenty-six fractures were treated operatively (22 males and 4 females, median age of 31, range 16 to 63 years). Out of the 65 fractures, 38 non- or minimally displaced scaphoid waist fracture (< 1 mm displacement and/or < 15° volar angulation) had been randomized to cast immobilization or arthroscopically assisted screw fixation.
Twenty-seven nondisplaced as well as displaced fractures, not being part of a randomized protocol, were treated according to the clinical judgment of the surgeon, of which three cases with severe fracture displacement were converted from arthroscopic technique to open volar approach. The department protocol recommended operative treatment when fracture displacement was > 1 mm.
Statistics
The presence of a linear trend between degree of fracture dislocation and fracture union at 6 weeks was tested using the linear-by-linear association test. We evaluated differences in union of randomized non- or minimally displaced scaphoid waist fracture with Fisher's exact test. Statistical analysis was performed using SPSS 20.0 for Windows (SPSS Inc., Chicago, IL, USA). p < 0.05 was considered statistically significant.
Results
Fracture characteristic are specified in Tables 1 and 2. Fracture comminution, represented by a separate cortical or corticospongious fragment on the radial side of the scaphoid was not uncommon (34%), even for the non- or minimally displaced scaphoid fractures (Fig. 3). Two cases of concomitant nondisplaced distal radius fracture were found in both treatment groups. In addition, the conservatively treated group included one wrist with concomitant capitate fracture and one with a combined capitate and triquetrum fracture. The operated group included one wrist with a concomitant capitate fracture. With the exception of three, the associated fractures were visible only on MRI.
Table 1. CT investigation on 39 conservatively treated scaphoid waist fractures.
| Non- or minimal displacement (N = 30) |
Moderate displacement (N = 6) |
Severe displacement (N = 3) |
|
|---|---|---|---|
| Fracture characteristics | |||
| Transverse | 23 | 5 | 1 |
| Oblique | 7 | 1 | 2 |
| Comminuted | 11 | 4 | 3 |
| Bone contact (6 wks) | |||
| 100% | 18 | 3 | 0 |
| 75–99% | 11 | 2 | 2 |
| 50–74% | 0 | 0 | 0 |
| 25–49% | 1 | 1 | 0 |
| 0–24% | 0 | 0 | 1 |
| Overall assessment of fracture union (6 wk) | |||
| Union | 27 | 5 | 2 |
| Uncertain union | 3 | 1 | 1 |
Table 2. CT investigation on 26 operatively treated scaphoid waist fractures.
| Non- or minimal displacement (N = 11) |
Moderate displacement (N = 5) |
Severe displacement (N = 10) |
|
|---|---|---|---|
| Fracture characteristics | |||
| Transverse | 10 | 3 | 6 |
| Oblique | 1 | 2 | 4 |
| Comminuted | 3 | 5 | 9 |
| Bone contact (6 wk) | |||
| 100% | 10 | 2 | 1 |
| 75–99% | 1 | 3 | 5 |
| 50–74% | 0 | 0 | 1 |
| 25–49% | 0 | 0 | 0 |
| 0–24% | 0 | 0 | 3 |
| Overall assessment of fracture union (6 wk) | |||
| Union | 9 | 5 | 4 |
| Uncertain union | 2 | 0 | 6 |
Fig. 3.
CT scan of a nondisplaced scaphoid waist fracture with a comminuted radial fragment.
In the conservatively treated group (Table 1), 24 fractures were immobilized in a cast for 5 to 8 weeks, eleven for 10 to 12 weeks, and four from 13 to 16 weeks. The 6-week CT scan demonstrated that 27/30 or 90% of the non- or minimally displaced fractures had united (Fig. 4). The number of patients with moderate or severe fracture displacement was too small to provide valid frequencies on fracture union. Therefore, a linear association between fracture displacement and fracture union could not be demonstrated (p = 0.47). Of the five fractures with uncertain union at 6 weeks, four were classified as healed after 10 weeks, and one after 14 weeks.
Fig. 4.
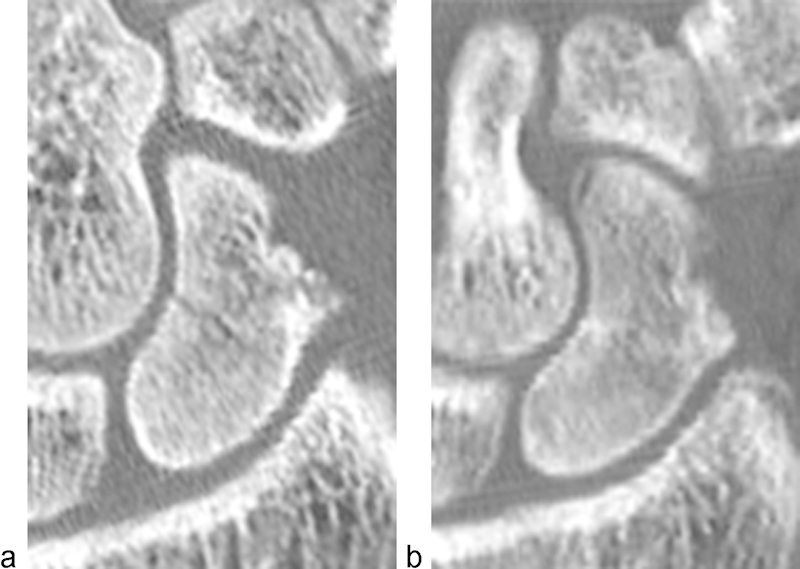
CT scan of a non-displaced scaphoid waist fracture (a), which at 6 weeks had united throughout the cross section of the fracture (b).
In the operatively treated group (Table 2), 17 fractures were immobilized in plaster for 2 weeks, two for 3 to 4 weeks, five for 6 weeks, and two for 10 weeks. In this group the union rate at 6 weeks for non- or minimally displaced fractures were 82%, and dropping to 40% for the severely displaced fractures. However, the numbers in the moderate and severe displacement groups were too small to make conclusions with regards to any association between fracture displacement and fracture union (p = 0.06). At 6 weeks, of the eight fractures with uncertain union, four were classified as united at 10 weeks, one at 6 months, two at 12 months, and one had developed into a nonunion. All fractures with prolonged time to union (> 14 weeks) were primarily classified as severely displaced.
In the randomized subgroup of patients (Table 3) with non- or minimally displaced scaphoid waist fracture, 23 were treated with cast immobilization, and 15 underwent arthroscopically assisted screw fixation. Eleven of the conservatively treated fractures were immobilized in a cast for 6 to 8 weeks, nine for 10 to 12 weeks, and three for 13 to 16 weeks. Based on the reevaluation of the CT scans, we found that 83% of these fractures had united at 6 weeks, 96% after 10 weeks, and 100% at 14 weeks. All four fractures that united later than 6 weeks were comminuted. In the operated group, 11 were immobilized in a cast for 2 weeks, three for 6 weeks, and one for 10 weeks. The CT scan demonstrated that 80% had united at 6 weeks, increasing to 94% after 10 weeks. One fracture did not unite until 1 year after surgery. We were not able to demonstrate any significant difference in union rate between the two treatment groups at any measure point (p = 1.00).
Table 3. CT investigation of union on a randomized subgroup of non- or minimally displaced scaphoid waist fractures.
| 6 wks | 10 wks | 14 wks | 6 months | 12 months | |
|---|---|---|---|---|---|
| Cast immobilization (N = 23) | |||||
| Union | 19 | 22 | 23 | 23 | 23 |
| Uncertain union | 4 | 1 | 0 | 0 | 0 |
| Internal fixation (N = 15) | |||||
| Union | 12 | 14 | 14 | 14 | 15 |
| Uncertain union | 3 | 1 | 1 | 1 | 0 |
Discussion
In this study, we focus on how a detailed radiographic assessment of fracture union, using CT scan in the longitudinal axis of the scaphoid, could help shortening the period of cast immobilization. Furthermore, we had the possibility to compare time to union between screw fixation and cast immobilization of non- or minimally displaced scaphoid waist fractures. We found that 90% of non- or minimally displaced scaphoid waist fractures were sufficiently treated with 6 weeks of immobilization in a cast. In a randomized subgroup of the nondisplaced scaphoid fractures, we were not able to demonstrate any difference in time to union between those who were treated conservatively in a cast and those who underwent screw fixation. Finally, we observed that the presence of fracture comminution might be associated with prolonged time to fracture union.
Generally, a scaphoid waist fracture with a displacement > 1 mm has been considered unstable and therefore a candidate for screw fixation.16 We found that fractures with a displacement < 1.5 mm healed uneventfully, within 6 to 10 weeks of conservative treatment.. In a recent study, scaphoid fractures with dorsal or volar gapping of ≤ 2 mm all united after conservative treatment, and ∼40% of those with ≥ 3 mm of gapping united. The authors advocated ≥ 3 mm of gapping as an indication for screw fixation.15 The apparent differences in recommendation for treatment based on fracture displacement may illustrate that CT scans cannot be relied on to determine whether a displaced or nondisplaced fracture is actually unstable.19 Further knowledge on the association between radiologic fracture displacement, biomechanical instability, and development of nonunion is needed.
A large number of non- or minimally displaced fractures demonstrated comminution in terms of a radial-sided cortical or corticospongious fragment. Previously, a strong correlation was demonstrated between scaphoid fracture comminution and arthroscopically verified fracture instability.20 While this association seems comprehensible for displaced scaphoid fractures, the importance for nondisplaced fractures is undetermined. Even though instability has been demonstrated by arthroscopy of radiographical nondisplaced fractures, our results suggest that the clinical importance is relatively minor, though a somewhat longer time to union could be expected (10 weeks). A larger-scale study is needed to determine the influence of fracture comminution on healing of non or minimally displaced scaphoid waist fractures.
In randomized trials on treatment of non- or minimally displaced scaphoid fractures, time to union varied considerably. Fractures treated with screw fixation were reported to unite more rapidly, with a mean value of 6 and 9 weeks, compared with those who were treated conservatively, from 10 to 14 weeks.1 3 7 However, these results are based on evaluation of radiographs, which have been proven less accurate than CT scans for assessment of scaphoid fracture union.9 10 First, the general definition of union is debatable. Second, it is difficult to obtain good-quality radiographs in the same plane as the fracture line. Finally, various patterns of partial union obscure interpretation.17 18 Even when using CT scans, interpretation of fracture union can be a challenge. In nondisplaced fractures, bone contact over the fracture site will be substantial, which does not necessarily mean that there is trabecular bridging. Also, if anatomic reduction and good compression are achieved after screw fixation, the fracture will look united straightaway.
The period of immobilization is not comparable between our patient groups. During the treatment period, this discrepancy displays the traditional cautiousness of the treating surgeon to avoid nonunion and its complications. In the current study, it reflects that results from the detailed CT evaluation were not available at the time of treatment. Nevertheless, our results suggest that the majority of non- or minimally displaced scaphoid waist fractures, unite after six weeks of conservative treatment in a cast. Furthermore, two weeks of immobilization seems sufficient after stable screw fixation. A general recommendation on conservative management versus operative treatment requires data on long-term functional and radiologic outcome.
A strategy of aggressive conservative management of non- or minimally displaced scaphoid waist fractures recommends operative treatment if CT scan at 6 weeks demonstrates uncertain union.8 We found that fractures that had not united at 6 weeks eventually united within 14 weeks of cast immobilization. The aggressive management strategy could therefore lead to unnecessary surgical intervention. For those with uncertain union we advocate postponing a decision to operate until after a CT scan at 14 weeks. We acknowledge that a repeated CT scan will result in an increased radiation load for the patient. However, as long as it is done with the injured wrist kept above the head, the effective radiation dose is as low as 0.03mSv, which is equivalent to one week of background radiation.21
Our study encompasses a consecutive series of patients with scaphoid waist fracture. However, there are several limitations. One weakness is the small sample size, which hampers our ability to compare time to union between fractures with different categories of displacement. Our reference standard for union is incomplete, as seven of the patients did not attend a 6- or 12-month CT scan. In our region (the southern part of Sweden) treatment of scaphoid nonunion is centralized at our department, so patients with prolonged symptoms, or who later on develop a nonunion, are most likely to be referred back to us. Either way, we looked through the regional radiology database and did not find any sign of nonunion among those who later on, for some reason, had had a radiographic examination of the hand in question. We did not test the interobserver reproducibility of the diagnosis of fracture union on the CT scans. Instead, resembling clinical practice, we did a consensus reading by the radiologist and one of the surgeons as described previously. However, it is reassuring that a substantial agreement has been demonstrated among multiple observers who evaluated scaphoid union on CT scans.22
With these limitations in mind, the clinical implication of our results is that we now treat non- or minimally displaced scaphoid waist fractures with 6 weeks of immobilization in a cast. In cases of uncertain union, a decision to recommend surgical intervention awaits a repeated CT scan at 14 weeks.
Note
Financial support has been received from Region Skåne and Skåne University Hospital.
Conflict of Interest None
Ethics
The Regional Ethics Committee at Lund University approved the study (LU 459–03).
References
- 1.Bond C D, Shin A Y, McBride M T, Dao K D. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001;83-A(4):483–488. doi: 10.2106/00004623-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Adolfsson L, Lindau T, Arner M. Acutrak screw fixation versus cast immobilisation for undisplaced scaphoid waist fractures. J Hand Surg [Br] 2001;26(3):192–195. doi: 10.1054/jhsb.2001.0558. [DOI] [PubMed] [Google Scholar]
- 3.McQueen M M, Gelbke M K, Wakefield A, Will E M, Gaebler C. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid: a prospective randomised study. J Bone Joint Surg Br. 2008;90(1):66–71. doi: 10.1302/0301-620X.90B1.19767. [DOI] [PubMed] [Google Scholar]
- 4.Clay N R, Dias J J, Costigan P S, Gregg P J, Barton N J. Need the thumb be immobilised in scaphoid fractures? A randomised prospective trial. J Bone Joint Surg Br. 1991;73(5):828–832. doi: 10.1302/0301-620X.73B5.1894676. [DOI] [PubMed] [Google Scholar]
- 5.Bhat M, McCarthy M, Davis T R, Oni J A, Dawson S. MRI and plain radiography in the assessment of displaced fractures of the waist of the carpal scaphoid. J Bone Joint Surg Br. 2004;86(5):705–713. doi: 10.1302/0301-620x.86b5.14374. [DOI] [PubMed] [Google Scholar]
- 6.Ram A N, Chung K C. Evidence-based management of acute nondisplaced scaphoid waist fractures. J Hand Surg Am. 2009;34(4):735–738. doi: 10.1016/j.jhsa.2008.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arora R, Gschwentner M, Krappinger D, Lutz M, Blauth M, Gabl M. Fixation of nondisplaced scaphoid fractures: making treatment cost effective. Prospective controlled trial. Arch Orthop Trauma Surg. 2007;127(1):39–46. doi: 10.1007/s00402-006-0229-z. [DOI] [PubMed] [Google Scholar]
- 8.Ibrahim T, Qureshi A, Sutton A J, Dias J J. Surgical versus nonsurgical treatment of acute minimally displaced and undisplaced scaphoid waist fractures: pairwise and network meta-analyses of randomized controlled trials. J Hand Surg Am. 2011;36(11):1759–17680. doi: 10.1016/j.jhsa.2011.08.033. [DOI] [PubMed] [Google Scholar]
- 9.Dias J J, Taylor M, Thompson J, Brenkel I J, Gregg P J. Radiographic signs of union of scaphoid fractures. An analysis of inter-observer agreement and reproducibility. J Bone Joint Surg Br. 1988;70(2):299–301. doi: 10.1302/0301-620X.70B2.3346310. [DOI] [PubMed] [Google Scholar]
- 10.Grewal R, Suh N, Macdermid J C. Use of computed tomography to predict union and time to union in acute scaphoid fractures treated nonoperatively. J Hand Surg Am. 2013;38(5):872–877. doi: 10.1016/j.jhsa.2013.01.032. [DOI] [PubMed] [Google Scholar]
- 11.Slade J F III, Gillon T. Retrospective review of 234 scaphoid fractures and nonunions treated with arthroscopy for union and complications. Scand J Surg. 2008;97(4):280–289. doi: 10.1177/145749690809700402. [DOI] [PubMed] [Google Scholar]
- 12.Slutsky D J, Trevare J. Use of arthroscopy for the treatment of scaphoid fractures. Hand Clin. 2014;30(1):91–103. doi: 10.1016/j.hcl.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Jørgsholm P, Thomsen N O, Besjakov J, Abrahamsson S O, Björkman A. The benefit of magnetic resonance imaging for patients with posttraumatic radial wrist tenderness. J Hand Surg Am. 2013;38(1):29–33. doi: 10.1016/j.jhsa.2012.09.034. [DOI] [PubMed] [Google Scholar]
- 14.Geoghegan J M, Woodruff M J, Bhatia R. et al. Undisplaced scaphoid waist fractures: is 4 weeks' immobilisation in a below-elbow cast sufficient if a week 4 CT scan suggests fracture union? J Hand Surg Eur Vol. 2009;34(5):631–637. doi: 10.1177/1753193409105189. [DOI] [PubMed] [Google Scholar]
- 15.Amirfeyz R, Bebbington A, Downing N D, Oni J A, Davis T R. Displaced scaphoid waist fractures: the use of a week 4 CT scan to predict the likelihood of union with nonoperative treatment. J Hand Surg Eur Vol. 2011;36(6):498–502. doi: 10.1177/1753193411403092. [DOI] [PubMed] [Google Scholar]
- 16.Cooney W P, Dobyns J H, Linscheid R L. Fractures of the scaphoid: a rational approach to management. Clin Orthop Relat Res. 1980;(149):90–97. [PubMed] [Google Scholar]
- 17.Singh H P, Forward D, Davis T R, Dawson J S, Oni J A, Downing N D. Partial union of acute scaphoid fractures. J Hand Surg [Br] 2005;30(5):440–445. doi: 10.1016/j.jhsb.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Dias J J. Definition of union after acute fracture and surgery for fracture nonunion of the scaphoid. J Hand Surg [Br] 2001;26(4):321–325. doi: 10.1054/jhsb.2001.0596. [DOI] [PubMed] [Google Scholar]
- 19.Buijze G A, Jørgsholm P, Thomsen N O, Bjorkman A, Besjakov J, Ring D. Diagnostic performance of radiographs and computed tomography for displacement and instability of acute scaphoid waist fractures. J Bone Joint Surg Am. 2012;94(21):1967–1974. doi: 10.2106/JBJS.K.00993. [DOI] [PubMed] [Google Scholar]
- 20.Buijze G A, Jørgsholm P, Thomsen N O, Björkman A, Besjakov J, Ring D. Factors associated with arthroscopically determined scaphoid fracture displacement and instability. J Hand Surg Am. 2012;37(7):1405–1410. doi: 10.1016/j.jhsa.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Biswas D, Bible J E, Bohan M, Simpson A K, Whang P G, Grauer J N. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91(8):1882–1889. doi: 10.2106/JBJS.H.01199. [DOI] [PubMed] [Google Scholar]
- 22.Buijze G A Wijffels M M Guitton T G Grewal R van Dijk C N Ring D; Science of Variation Group. Interobserver reliability of computed tomography to diagnose scaphoid waist fracture union J Hand Surg Am 2012372250–254. [DOI] [PubMed] [Google Scholar]


