Abstract
Purpose
The relationship between body mass index (BMI) and the risk of inguinal hernia development is unclear. To explore the relationship, we determined whether the incidence of inguinal hernia repairs (IHR) varied across patients in different BMI categories.
Study Design
A population-based incidence study was undertaken. We reviewed all IHR performed on adult residents of Olmsted County, MN from 2004 to 2008. Cases were ascertained through the Rochester Epidemiology Project, a records-linkage system with more than 97% population coverage.
Results
During the study period, a total of 1,168 IHR were performed on 879 men and 107 women. The median BMI of the cohort was 26.7 kg/m2 (range 14.9 – 58.1; interquartile range 23.9 – 28.9). Incidence rates varied significantly as a function of BMI (p<0.001). Rates were highest among men who were either normal weight or overweight (419.8 and 421.1 per 100,000 person years for BMI<25 and BMI 25–29.9, respectively), and lowest for obese and morbidly obese men (273.5 and 99.4 per 100,000 person years for BMI 30–34.9 and BMI ≥35, respectively). Findings were similar across all age categories and in patients who had an IHR that was initial or recurrent, direct or indirect, and unilateral or bilateral.
Conclusions
The incidence of IHR decreased as BMI increased. Obese and morbidly obese patients had a lower incidence of IHR than those who were normal weight or overweight. The causal mechanisms leading to such a relationship are unclear and warrant further study.
Keywords: Obesity, inguinal hernia, repair, incidence, body mass index, population
Introduction
Inguinal hernias (IHs) are a common occurrence worldwide. The true incidence of IH is unknown, but nearly 800,000 are repaired each year in the USA alone, [1] and it’s estimated that nearly 1 in every 2 men will require an inguinal hernia repair (IHR) in his lifetime.[2] Increasing age, male gender, smoking, family history, connective tissue disorders, and increased intra-abdominal pressure have all been suggested as possible predisposing factors to develop an IH.[3] However, the relationship between IH development and body weight is controversial.
Because of the increased intra-abdominal pressure associated with being overweight, [4][5] obesity has intuitively been seen as a risk factor for the development of IH. However, recent epidemiologic studies have suggested the opposite: increased weight, along with higher body mass index (BMI), is associated with a decreased risk of requiring an IHR when compared with normal weight individuals.[6, 7][8] Nonetheless, obesity is an established risk factor that increases the risk of recurrence of an IHR.[6] Hence, it is possible that the interaction between body weight and the mechanisms behind the development and recurrence of an IH are different.
It is important to better understand and delineate the relationship between body weight and the risk of developing an IH, particularly in countries such as the USA, where a rising obesity epidemic has become a major health care problem.[9] To gain insight into this relationship, we sought to examine the impact of BMI on age- and sex-specific incidence rates of IHR in a well-defined USA population.
Methods
Our methods have been described previously.[2] Briefly, after obtaining both Olmsted Medical Center and Mayo Clinic Institutional Review Board approvals, we reviewed all historical IHRs performed on adult residents of Olmsted County, MN from January 1, 2004 through December 31, 2008.
Olmsted County is located in southeastern Minnesota and has a population primarily of northern and central European descent. More than 70% of the population resides in Rochester, and the remainder of the county is rural. As of the 2010 USA Census, the population of Olmsted County was 146,446: 51% women, 18% older than the age of 65 years, and 90% Caucasian.[10]
To identify potential cases, we employed the Rochester Epidemiology Project (REP), a records-linkage system that provides a robust infrastructure for indexing and linking medical information of the county population. The REP covers more than 97% of the population of Olmsted County, with only the remaining 3% declining the use of their medical records for research.[11][12] We ascertained potential cases of IHR (both primary and recurrent) by searching the REP electronic diagnostic indexes for H-ICDA diagnostic codes[13] (55001, 55003, 55004, 55011, 55021, 55101, 55201, 55301, 55211), ICD-9 diagnostic codes[14] (550.01, 550.03, 550.11, 550.13, 550.91, 550.93), and Current Procedural Terminology (CPT) codes[15] (17.11-17.24, 53.00-53.17) related to IHR. The records of all patients with at least one of the aforementioned codes indexed during the study period were screened by the study team using a specifically designed form and following a manual of instructions. Study data were collected and managed using REDCap electronic data capture tools hosted at Mayo Clinic.[16]
Diagnostic Classification
We grouped IHR according to the order of occurrence in life (initial vs. second or more), laterality (unilateral vs. bilateral), and recurrence (recurrent vs. non-recurrent). We also sub-classified IH according to the type of hernia (direct or indirect). Height and weight data were abstracted for each patient on the day of their operation and used to calculate body mass index (BMI, kg/m2). Patients were categorized according to BMI as normal weight (<25), overweight (25–29.9), obese (30–34.9), and morbidly obese (≥35). We did not analyze underweight (<18.5) as a separate category since there were only 7 incident cases during our timeframe who were underweight.[17]
Data Analysis
Incident cases were defined as all subjects whose record revealed the presence of an IHR from January 1, 2004 through December 31, 2008 while they were county residents. Patients who moved to Olmsted County specifically for the treatment of their hernia were excluded. Incidence rates per 100,000 person-years were calculated using the incident cases of IHR as the numerator and age- and sex-specific estimates of the population of Olmsted County, Minnesota as the denominator. The populations at risk for the years 2004–2008 were obtained from the U.S. Intercensal Estimates.[10] We did not correct the denominators by removing prevalent cases of IHR because all subjects were considered at risk for a recurrent IHR.
To partition the person-years separately by BMI category, we used BMI information available for persons who were Olmsted County residents during the same timeframe as our study, who had been seen at the Mayo Clinic, and who had an electronically recorded height and weight. These data were available as part of the REP infrastructure.[12] We stratified persons by sex and by age categories that we had studied previously (18–29, 30–49, 50–59, 60–69, 70–79, and ≥80 years old). The median number of persons available in each of the 12 combinations of sex and age category who contributed information to the partitioning of the denominator population by BMI was 2,582 (ranging from 791 for men ≥80 years old to 6,957 for women 30–49 years old). We summarized the BMI categories within each of these 12 combinations (for example, among 18–29 year old men, there were 47%, 33%, 13%, and 7% who were normal weight, overweight, obese, and morbidly obese, respectively) and used these percentages to partition Olmsted County population counts. For the nearly 12,000 men aged 18–29 years old in Olmsted County in 2004, denominator person-years were partitioned into approximately 5,640, 3,960, 1,560, and 840 person-years for BMI categories <25, 25–29.9, 30–34.9, and ≥35, respectively. These partitioned population counts were then used as the denominators in the calculation of incidence rates.
The relationships of age category, sex, and BMI category with incidence of IHR were assessed by fitting Poisson regression models using the SAS procedure GEDMOD (SAS Institute Inc.; Cary, North Carolina). All hypothesis testing was two-sided and p-values <0.05 were considered statistically significant.
Results
During the study period, a total of 1,168 IHR were performed on 986 patients (879 men and 107 women) with an overall incidence of IHR of 355.9 per 100,000 person-years for men and 37.7 per 100,000 person-years for women (p<0.001). BMI data were available for 972 of the 986 patients (99%). The median BMI was 26.5 kg/m2 (range 16.6–58.1; interquartile range 24.3–29.3) for men and 23.4 kg/m2 (range 14.9–39.8; interquartile range 21.5–26.7) for women. Incidence rates varied by BMI (Table 1; Figure 1). Incidence rates for overweight men (421.1 per 100,000 person-years) were not statistically significantly different from normal weight men (419.8 per 100,000 person-years; p=0.97). However, incidence rates for obese (273.5 per 100,000 person-years) and morbidly obese (99.4 per 100,000 person-years) men were statistically significantly lower compared with normal weight men (p<0.001 for both). Incidence rates for women who were overweight (29.3 per 100,000 person-years), obese (16.3 per 100,000 person-years), and morbidly obese (12.4 per 100,000 person-years) were statistically significantly lower compared with normal weight women (57.5 per 100,000 person-years; p<0.01 for all three). Among men, incidence rates varied across age category (p<0.001); however, the decrease in incidence as BMI category increased was similar within each age category (p=0.60; Figure 2).
Table 1.
Age- and Sex-Specific Incidence Rates of Inguinal Hernia Repairs by BMI in Olmsted County, MN, 2004–2008*
| Age, years | ||||||||
|---|---|---|---|---|---|---|---|---|
| BMI | Sex | 18–29 | 30–49 | 50–59 | 60–69 | 70–79 | ≥80 | Total |
| <25 | Women | 9.3 (4) | 40.5 (18) | 48.7 (7) | 223.3 (17) | 219.4 (12) | 179.9 (12) | 57.5 (70) |
| Men | 160.9 (46) | 388.3 (83) | 836.1 (58) | 1131.8 (43) | 1023.0 (31) | 709.1 (16) | 419.8 (277) | |
| Total | 69.6 (50) | 153.4 (101) | 305.1 (65) | 525.7 (60) | 505.9 (43) | 313.7 (28) | 184.8 (347) | |
| 25-29.9 | Women | 0 (0) | 17.9 (5) | 45.5 (6) | 10.9 (1) | 104.2 (7) | 80.6 (4) | 29.3 (23) |
| Men | 135.6 (27) | 306.0 (127) | 668.6 (112) | 868.0 (87) | 658.0 (45) | 478.6 (18) | 421.1 (416) | |
| Total | 74.2 (27) | 190.3 (132) | 394.2 (118) | 458.0 (88) | 383.6 (52) | 252.2 (22) | 247.7 (439) | |
| 30-34.9 | Women | 0 (0) | 0 (0) | 11.7 (1) | 54.4 (3) | 56.4 (2) | 38.4 (1) | 16.3 (7) |
| Men | 101.1 (8) | 202.7 (45) | 293.6 (31) | 429.3 (29) | 587.5 (23) | 539.2 (9) | 273.5 (145) | |
| Total | 54.6 (8) | 117.7 (45) | 167.6 (32) | 260.9 (32) | 335.1 (25) | 233.9 (10) | 158.4 (152) | |
| ≥35 | Women | 0 (0) | 18.3 (3) | 11.8 (1) | 0 (0) | 0 (0) | 84.4 (1) | 12.4 (5) |
| Men | 64.8 (3) | 78.0 (10) | 135.8 (8) | 177.6 (7) | 69.5 (1) | 0 (0) | 99.4 (29) | |
| Total | 26.6 (3) | 44.5 (13) | 62.7 (9) | 76.9 (7) | 24.7 (1) | 60.7 (1) | 48.8 (34) | |
Data are presented as incidence rates per 100,000 person-years followed by the number of incident cases in parentheses. There were 187,778 total person-years for Olmsted County residents with BMI <25; 177,196 for BMI 25–29.9; 95,966 for BMI 30–34.9; and 69,662 BMI ≥35.
Figure 1.
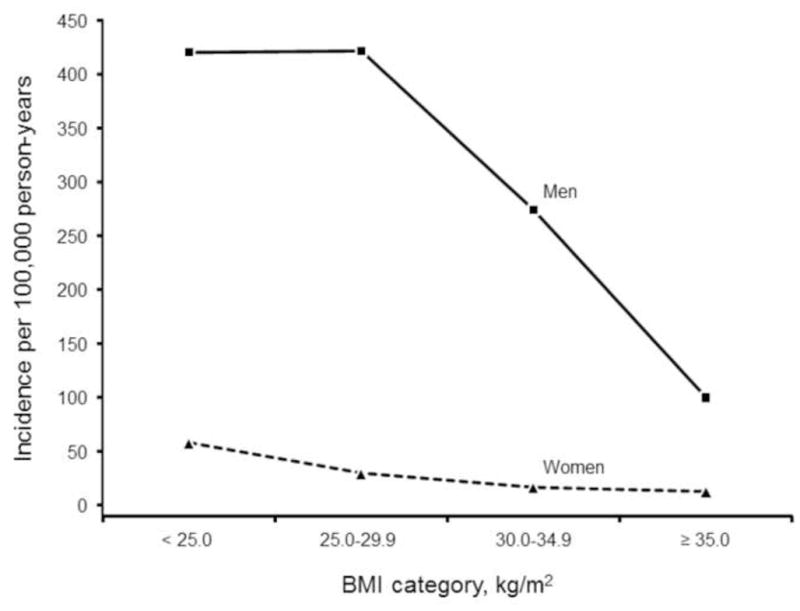
Incidence of Inguinal Hernia Repairs by BMI Category
Figure 2.
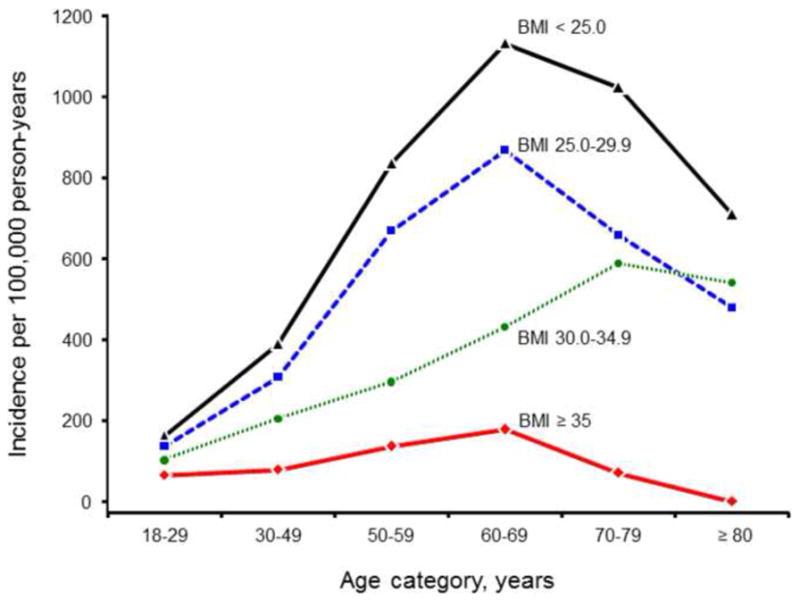
Incidence of Inguinal Hernia Repairs by Age and BMI category for Men
Among men, this trend of decreasing incidence with increasing BMI was consistent in both initial (N=797) and recurrent (N=56) IHR (Figure 3). Normal weight and overweight men with an initial IHR (unilateral or bilateral) had maximum incidence rates of 371.3 and 384.6 per 100,000 person-years, respectively, whereas these rates were 250.9 and 96.0 per 100,000 person-years for obese and morbidly obese men, respectively. Rates for recurrent IHR had a maximum incidence rate of 33.3 per 100,000 person years for normal weight men, and rates of 24.3, 15.1 and 3.4 per 100,000 person years for overweight, obese and morbidly obese men, respectively.
Figure 3.
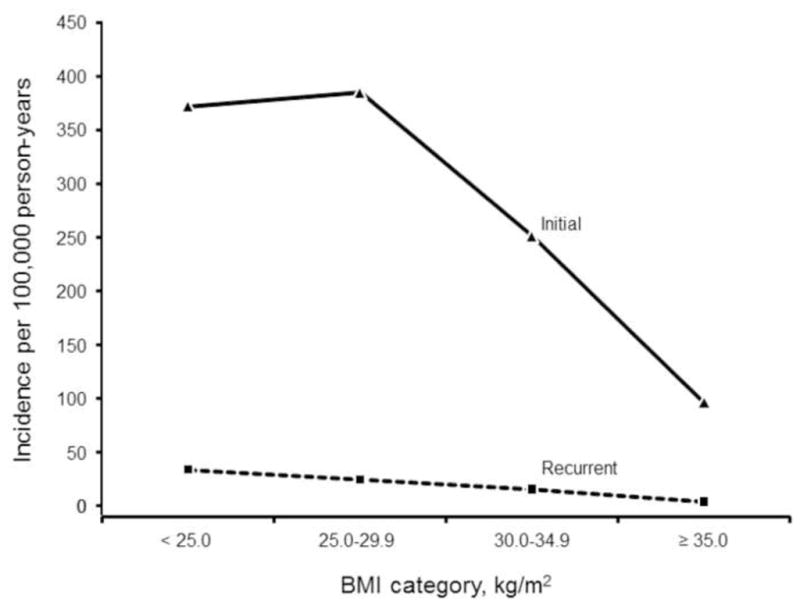
Incidence of Inguinal Hernia Repairs by Initial versus Recurrent for Men
This trend was also consistent in both unilateral (N=626) and bilateral (N=171) IHR (both initial). Men with unilateral IHR had maximum incidence rates of 283.4 and 301.6 per 100,000 person-years when normal weight and overweight, respectively, whereas these rates were 201.9 and 89.1 per 100,000 person-years for obese and morbidly obese men, respectively. Men with bilateral IHR had maximum incidence rates of 87.9 and 83.0 per 100,000 person-years when normal weight and overweight, respectively, decreasing to 49.1 and 6.9 per 100,000 person-years for obese and morbidly obese men, respectively. Among the 626 men with initial unilateral IHR, there were 405 indirect, 148 direct, 55 pantaloon, 2 femoral, and 16 missing type of hernia. Indirect IHR had maximum incidence rates of 178.8 and 201.4 per 100,000 person-years for normal weight and overweight men, respectively, decreasing to 126.4 and 58.3 per 100,000 person-years for obese and morbidly obese men, respectively. Direct IHR had maximum incidence rates of 68.2 and 70.9 per 100,000 person-years for normal weight and overweight men, respectively, decreasing to 47.2 and 17.1 per 100,000 person-years for obese and morbidly obese men, respectively.
Discussion
This population-based study of Olmsted County, MN provides a robust resource to accurately examine the effects of BMI on IHR incidence. Our study shows that the incidence of IHR varies by BMI, with rates decreasing as BMI increases.
Our findings are consistent with previous findings in USA populations. The National Health and Nutrition Examination Survey (NHANES) examined the risk factors for incident IH development among adults.[3] Investigators found that patients with higher weight, and consequently higher BMI, had a significantly decreased risk of developing IH throughout their lifetime. Although our outcome (IH repair) was different than that used in the NHANES study (IH development), ascertainment bias could still be present in both studies. The IH diagnosis spectrum can be viewed through the lens of the iceberg analogy, where the tip of the iceberg corresponds to the operative confirmation of IH through inguinal exploration, and the portion of the iceberg below the waterline represents both patients with a clinical diagnosis (either by self-awareness, physical exam, or imaging) of IH and patients who are unaware of the presence of their IH. Clearly, ascertainment bias could be present at each diagnostic level. We decided to focus on the tip of the iceberg (i.e., IH that are repaired) to examine the societal impact of the relationship between IHR and BMI on healthcare resource utilization.
Though obesity is not as prevalent in Sweden as it is in the USA, [18] Swedish-based population studies have also attributed a “protective” effect to obesity in the development of IH.[6][7] Interestingly, data from the Swedish hernia registry showed that the relationship of BMI with post-operative complications after IHR was U-shaped, where complication rates were highest in patients who were underweight or obese.[6] Others have also encountered increased risk for re-admission for obese patients after IHR.[19] Hence, it appears that although obese patients are at low risk to develop an IH, when they have one, they are at increased risk for complications.
Several possible explanations have been postulated to account for obesity as a “protective” factor in the development of IH: 1) Excess intra-abdominal or pre-peritoneal fat could provide a barrier effect by acting as a “plug” to prevent herniation of abdominal contents; 2) Patients who are obese could have poor overall health due to obesity related comorbidities, making them non-suitable candidates for an elective operation such as an IHR; 3) Though the degree and type of physical activity is a controversial risk factor for the development of an IH, [3, 20] obese individuals may be less physically active than non-obese individuals, and 4) The clinical diagnosis or self-awareness of an IH could be more difficult in obese individuals due to body habitus. Despite the increased diagnostic challenge of detecting an IH in an obese patient, they are often exposed to more healthcare contact due to obesity related comorbidities and hence are at higher likelihood of discovery. Nonetheless, further studies examining measures of obesity that more directly reflect intra-abdominal pressure (e.g., waist diameter and intra-abdominal visceral fat) as protective factors for IH may prove fruitful in corroborating or refuting the observations encountered so far, as BMI is a reflection of overall body weight and may not be the best measure of intra-abdominal pressure.[21]
This study has several strengths. Population-based samples avoid referral bias seen in hospital-based convenience samples. The REP covers the two hospitals where IHR are performed in the area (Olmsted Medical Center and Mayo Clinic); it encompasses academic and community practice patterns, as well as inpatient and outpatient surgery. Weaknesses of our study include, but are not limited to, the possibility that there could have been some Olmsted County residents who chose to undergo an IHR elsewhere, thus not being captured by the REP. We believe that this is of minimal impact given the facilities and physicians available in the county, and the nature of the disease. In addition, epidemiologic data generated from Olmsted County may not be generalizable to the USA population. Though previous reports have shown that age, sex, and ethnic characteristics of Olmsted County are similar to those of Minnesota and the Upper-Midwest, Olmsted County is less ethnically diverse than the USA population, more highly educated, and wealthier.[12][22] Lastly, the BMI data used to partition person-years were only available for persons seen at Mayo Clinic. As such, we assumed that the distribution of BMI among persons seen at Mayo Clinic was similar to the distribution of BMI among all Olmsted County residents during the study timeframe.
In summary, the findings from this study allow us to better understand the interplay between the incidence of IHR and BMI in a well-defined USA population. This study provides insight into the possible mechanisms behind the decrease in IH risk in obese patients, but further research is needed to test this hypothesis. Because IHR are common, recognizing trends[23] and factors that increase or decrease their risk will allow better planning and anticipation of healthcare needs.
Acknowledgments
Support & Grants: This publication was made possible by the Rochester Epidemiology Project (Grant Number R01 AG034676 from the National Institute on Aging) and by Grant Number 1 UL1 RR024150 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and the NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
SELECTED ABBREVIATIONS AND DEFINITIONS
- IH
Inguinal hernia
- IHR
Inguinal hernia repair
- BMI
Body mass index
- REP
Rochester Epidemiology Project
- USA
United States of America
- H-ICDA
Hospital adaptation of international classification of diseases
- ICD-9
International classification of diseases, 9th edition
- CPT
Current procedural terminology
- NHANES
National Health and Nutrition Examination Survey
Footnotes
Presentations: Presented in part as poster presentation at the 5th International Hernia Congress, American and European Hernia Society, March 2012, New York, NY
Disclosures: None
Summative Disclosure Statement
BZ, TR, RH, CL, BG, and DF declare no conflicts of interest
References
- 1.Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. The Surgical clinics of North America. 2003;83:1045–51. v–vi. doi: 10.1016/S0039-6109(03)00132-4. [DOI] [PubMed] [Google Scholar]
- 2.Zendejas B, Ramirez T, Jones T, et al. Incidence of Inguinal Hernia Repairs in Olmsted County, MN: A Population-Based Study. Annals of surgery. 2013;257:520–6. doi: 10.1097/SLA.0b013e31826d41c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruhl CE, Everhart JE. Risk factors for inguinal hernia among adults in the US population. American journal of epidemiology. 2007;165:1154–61. doi: 10.1093/aje/kwm011. [DOI] [PubMed] [Google Scholar]
- 4.Noblett KL, Jensen JK, Ostergard DR. The relationship of body mass index to intra-abdominal pressure as measured by multichannel cystometry. International Urogynecology Journal And Pelvic Floor Dysfunction. 1997;8:323–326. doi: 10.1007/BF02765589. [DOI] [PubMed] [Google Scholar]
- 5.Varela JE, Hinojosa M, Nguyen N. Correlations between intra-abdominal pressure and obesity-related co-morbidities. Surgery for obesity and related diseases: official journal of the American Society for Bariatric Surgery. 5:524–8. doi: 10.1016/j.soard.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Rosemar A, Angerås U, Rosengren A, Nordin P. Effect of body mass index on groin hernia surgery. Annals of surgery. 2010;252:397–401. doi: 10.1097/SLA.0b013e3181e985a1. [DOI] [PubMed] [Google Scholar]
- 7.Rosemar A, Angerås U, Rosengren A. Body mass index and groin hernia: a 34-year follow-up study in Swedish men. Annals of surgery. 2008;247:1064–8. doi: 10.1097/SLA.0b013e31816b4399. [DOI] [PubMed] [Google Scholar]
- 8.Liem MS, Van der Graaf Y, Zwart RC, et al. Risk factors for inguinal hernia in women: a case-control study. The Coala Trial Group. American journal of epidemiology. 1997;146:721–6. doi: 10.1093/oxfordjournals.aje.a009347. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiologic reviews. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 10.US Census Bureau. [Accessed 20 Aug 2011]; http://www.census.gov.
- 11.Melton LJI. History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Yawn BP, et al. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. American journal of epidemiology. 2011;173:1059–68. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Commission on Professional and Hospital Activities. H-ICDA, Hospital Adaptation of ICDA. Ann Arbor, MI: 1973. [Google Scholar]
- 14.Centers for Disease Control and Prevention. [Accessed 20 Aug 2011];Classification of Diseases, Functioning, and Disability. http://www.cdc.gov/nchs/icd.htm.
- 15.American Medical Association. [Accessed 20 Aug 2011];Current Procedural Terminology. http://www.ama-assn.org.
- 16.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. [Accessed 3 Apr 2013];BMI Classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.
- 18.Lilja M, Eliasson M, Stegmayr B, et al. Trends in obesity and its distribution: data from the Northern Sweden MONICA Survey, 1986–2004. Obesity (Silver Spring, Md) 2008;16:1120–8. doi: 10.1038/oby.2008.230. [DOI] [PubMed] [Google Scholar]
- 19.Lindström D, Sadr Azodi O, Bellocco R, et al. The effect of tobacco consumption and body mass index on complications and hospital stay after inguinal hernia surgery. Hernia: the journal of hernias and abdominal wall surgery. 2007;11:117–23. doi: 10.1007/s10029-006-0173-4. [DOI] [PubMed] [Google Scholar]
- 20.Carbonell JF, Sanchez JL, Peris RT, et al. Risk factors associated with inguinal hernias: a case control study. The European journal of surgery = Acta chirurgica. 1993;159:481–6. [PubMed] [Google Scholar]
- 21.Lambert DM, Marceau S, Forse RA. Intra-abdominal pressure in the morbidly obese. Obesity surgery. 2005;15:1225–32. doi: 10.1381/096089205774512546. [DOI] [PubMed] [Google Scholar]
- 22.St Sauver JL, Grossardt BR, Leibson CL, et al. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clinic proceedings Mayo Clinic. 2012;87:151–60. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zendejas B, Ramirez T, Jones T, et al. Trends in the utilization of inguinal hernia repair techniques: a population-based study. American Journal of Surgery. 2012;203:1–5. doi: 10.1016/j.amjsurg.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]


