Abstract
Background
Help seeking for online peer and other social support in response to depression and other mental health problems offers an electronic technology alternative to traditional mental health care. Here, with nationally representative samples of adult community residents in the USA, we study online peer support help seeking, estimate its occurrence, and investigate depression and other suspected predictors and correlates, some of which might prove to be causal influences.
Method
The data are from nationally representative probability sample surveys of the non-institutionalized US adult population, with a new independent sample assessed via confidential computerized self-assessment modules each year from 2004 to 2010, yielding estimates about online peer support. A total of 264 431 adults participated in these years.
Results
An estimated three per 1000 adults (0.3%) seek online peer support for mental health problems each year (95% confidence interval 0.0022–0.0036). Individuals with depression and/or serious psychological distress are strongly over-represented among these adult online peer support help seekers (odds ratio >7, p<0.001). Associations with college education, being non-Hispanic white, being female, and age are also noteworthy (p<0.05).
Conclusions
Online help seeking for mental health social support is becoming frequent enough for study in large sample national surveys, and might well be fostered by active neuropsychiatric ailments such as depression or other serious psychological distress. Open questions remain about whether the result is beneficial, or conditions required for efficacious online peer support, as might be disclosed in definitive evidence from randomized controlled trials.
Keywords: Internet self help, major depression, mental health treatment, online discussion forums, online social support, serious psychological distress
Introduction
In this new research report, we present an epidemiological community survey view of adults seeking help in the USA during the early 21st century, with a specific focus on Internet visits for mental health social support, chat room visits, and other forms of ‘online peer support’ (OPS). Drawing upon strengths of nationally representative sampling and standardized assessments of adult community residents, we sought to estimate the degree to which OPS help seeking might be linked with neuropsychiatric ailments, especially current depression or other forms of serious psychological distress (SPD), or with past depression in the absence of current illness. Subsidiary attention is given to other suspected predictors and correlates such as sex, age and socio-economic status. Initial exploratory analyses and sentinel estimates are based entirely on data from the 2009 National Survey of Drug Use and Health (NSDUH). Each analysis is replicated with NSDUH data from 2004 to 2008, and 2010, and a meta-analysis yields summary estimates.
In past research about the Internet and health, study samples often have been restricted to online help seekers, to convenience samples of patients, to the enrollee rosters of health care plans, or to selected samples of predefined subpopulations (e.g. university students). Better external generalizability can be gained via nationally representative sampling of community residents, but no prior surveys of national scope have produced OPS estimates for adults affected by mental health problems (e.g. Baker et al. 2003; Hesse et al. 2005; Powell & Clark, 2006; Ybarra & Suman, 2006; Atkinson et al. 2009; Fox & Jones, 2009; Fox, 2011). A highly publicized Pew study of online support in the USA addressed cancer and other chronic conditions, but not mental health support (Fox, 2011). In the USA, Australia and a handful of other countries there are nationwide studies that document patient use of Internet communication venues to access traditional health care resources and to gain health information (e.g. Baker et al. 2003; Powell & Clark, 2006; Ybarra & Suman, 2006; Atkinson et al. 2009). Several surveys have focused on acquisition or seeking of health information, including mental health, but did not address OPS (Hesse et al. 2005; Fox & Jones, 2011). In related research, Powell et al. (2003) used a convenience sample to estimate the proportion of online support seekers with major depression (MD) who also sought traditional care. The results indicated that among those with MD who were seeking help online, approximately 50% were not currently receiving traditional care (i.e. drug or psychological treatment). In this work with an epidemiological sample, we seek to estimate the association between MD and OPS, and also to explore subgroup variation among those who do and do not seek traditional treatment.
The effectiveness of health-related electronic support groups is being studied, but limitations have included constraints on generalizability due to highly selected samples, inter alia. Systematic reviews indicate that peer-to-peer interaction provided by OPS may be beneficial; no evidence of harm has been found (Eysenbach et al. 2004; Griffiths et al. 2010). In one review, Griffiths et al. (2010) looked only at randomized controlled trials of Internet interventions for anxiety and depression, noted diversity amongst various forms of Internet-based health interventions, and mentioned possible selection biases when evaluations failed to probe what prompted help seeking in the first place, as elucidated by others (Berger et al. 2005; Walther et al. 2005; Barak et al. 2009; Leykin et al. 2012). In summary, they concluded that ‘the Internet can be an effective medium for the delivery of interventions designed to reduce the symptoms of depression and anxiety conditions’ (Griffiths et al. 2010, p. S6).
With these systematic reviews and other reports as background (e.g. Owen et al. 2010), our research group looked for national survey estimates of OPS help seeking, and for evidence on whether OPS help seeking might depend upon adult depression or SPD. Analysing data from a September 2002 national survey of 7467 groups run by and for mental health consumers and/or families in the USA, Goldstrom et al. (2006) attempted to document an emerging ‘mental health self-help revolution’ in relation to a three-class typology (mental health mutual support groups, self-help organizations, and consumer-operated services), and noted that 40% of the groups maintained websites or a listserv, but did not estimate the volume of participation in OPS. Two prior reports based on NSDUH data gathered before 2009 differentiated ‘traditional’ and ‘alternative’ mental health care; neither considered OPS per se. Instead, online support groups and chat rooms were included in the ‘alternative ’ category, together with assorted ‘non-traditional’ mental health care services from telephone hotline operators, acupuncturists, massage therapists, herbalists, spiritual and religious advisors, as well as in-person support and self-help groups (United States Substance Abuse and Mental Health Services Administration, Office of Applied Studies, 2009). In a report based on NSDUH surveys between 2005 and 2008, an estimated 12–14% (almost 30 million) adults in the USA were found to be recent (past year) help seekers for ‘traditional’ mental health care defined to encompass in-patient and out-patient services combined with prescribing of psychotherapeutic medicines for mental health problems. By comparison, an estimated 1.1% (roughly 2.4 million adults) had recently sought help from ‘alternative’ mental health venues such as social support or self-help groups (Han et al. 2011), but no estimates differentiated in-person support or self-help from OPS, which is the primary focus here.
In summary, previous research has examined many different uses of the Internet for health-related purposes. As illustrated in the preceding literature review, distinct forms of health-related Internet use exist such as information seeking, the online delivery of psychotherapy, online social support, and online contact with traditional health care providers. After scanning these related, yet somewhat disparate, research areas, it was difficult to identify any empirical studies that estimate the use of OPS groups using a nationally representative sample of the US population – let alone nationally representative samples spanning multiple years of assessment. This study fills that vacuum and provides a foundation for future research.
Method
Study population
Each year, the NSDUH study population is designed to encompass civilian, non-institutionalized US residents aged 12 years and older. The NSDUH seeks national representation via multi-stage area probability sampling. Participation levels generally are in the 65–80% range. A standardized audio-enhanced computer-assisted self-interview (ACASI) assessment protocol is administered during a home visit. The results are posted as public use datasets. Institutional review boards for human subject protection review and approve each year’s NSDUH survey protocol, as well as analysis protocols (United States Substance Abuse and Mental Health Services Administration, 2012).
This research report’s sentinel estimates are based on 38067 adult participants in the 2009 NSDUH survey, all of whom answered the OPS questions in the mental health services (MHS) assessment module and are included in the 2009 public use dataset (United States Substance Abuse and Mental Health Services Administration, 2009). Summed across all survey years from 2004 to 2010, the public use datasets include 264 431 adults in the seven independent replicate samples for meta-analysis summary estimates. (The 12- to 17-year-olds in NSDUH samples are not asked about OPS.)
Assessment
A module of standardized MHS questions is positioned midway through the multi-module NSDUH ACASI assessment, with coverage of help seeking via traditional or alternative MHS, including online support groups or chat rooms in the 12 months prior to assessment, with focus on ‘treatment, counseling, or support for problems with emotions, nerves, or mental health’. Appendix A shows the survey items. In addition, MD (recent and past), onset age, and depression spell recency are assessed in a separate multi-item ACASI module adapted from the National Comorbidity Survey. As described elsewhere (Blazer & Wu, 2009; United States Substance Abuse and Mental Health Services Administration, 2009), the NSDUH MD cases manifest at least five of nine criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). Here, MD case status refers to MD spell, rather than DSM-IV major depressive episode (MDE), for reasons outlined in methodological reports, including non-coverage of MDE diagnostic hierarchies and exclusion rules (United States Substance Abuse and Mental Health Services Administration, 2009; APA, 2010). Exact questions in the NSDUH MD module and other details are available online (section B.4.4; United States Substance Abuse and Mental Health Services Administration, 2012).
Associated covariates under study included SPD as measured by the K6 items on feeling nervous, hopeless, restless, depressed, lethargic and worthless during the worst mental health month of the past 12 months (Furukawa et al. 2003), as well as age, sex, race/ethnicity, income and educational attainment variables previously found to influence Internet access (Fox & Jones, 2009). Income and education are modeled separately, due to multicollinearity.
Statistical analysis
A standard ‘explore, analyse/estimate, explore’ cycle started with NSDUH 2009 data. After inspection of marginal distributions, logistic regression models for the 2009 survey weighted data estimated OPS–depression associations as odds ratios (ORs), 95% confidence intervals (CIs) and p values, using the Taylor series delta method for variance estimation, with survey subpopulation estimation for stratified subgroups. Then, the analyse/estimate step was repeated for the other six survey years, followed by a random-effects meta-analysis to derive summary estimates and the heterogeneity χ2, all via Stata software, version 11.0 (StataCorp LP, USA). In this work, we stress precision and focus on 95% CI; p values serve as an aid to interpretation.
Results
Table 1 describes the unweighted NSDUH 2009 adult sample as predominantly female (53%), non-Hispanic white (63%) and aged 18–24 years (50%); the same was true for the other survey years. According to weighted survey estimates from our exploratory analysis with 2009 data on the 12 months prior to assessment, an estimated three per 1000 community-dwelling adults in the USA (0.3%) sought help for mental health problems in the form of OPS and/or chat room activity (95% CI 0.0022–0.0036), with evidence of some subgroup variation as disclosed in the rightmost columns of Table 1. Subsequently, the meta-analysis showed no appreciable variation in this 0.3% estimate year-by-year, 2004–2010 (95% CI 0.0027–0.0033), as displayed in the Supplementary Online Appendix (eTable 1), along with estimated proportions and unweighted sample characteristics each year, 2004–2010 (eTables 2–7).
Table 1.
Selected characteristics of adult participantsa
| Unweighted number of adults: total | Unweighted % of adults: total | Unweighted number of adults who did or did not use online support
|
Weighted proportion using online support, estimated number per 10 000 adultsb | ||
|---|---|---|---|---|---|
| Did not use, n | Did use, n | ||||
| All persons | 38 067 | 100 | 37 924 | 143 | 30 |
| Sex | |||||
| Male | 17 773 | 46.7 | 17 734 | 39 | 16 |
| Female | 20 294 | 53.3 | 20 190 | 104 | 42 |
| Age, years | |||||
| 8–25 | 19 009 | 49.9 | 18 932 | 76 | 44 |
| 26–34 | 5 630 | 14.8 | 5 604 | 26 | 45 |
| 35–49 | 7 863 | 20.7 | 7 834 | 29 | 26 |
| 50+ | 5 566 | 14.6 | 5 554 | 12 | 20 |
| Race/ethnicity | |||||
| Non-Hispanic white | 24 138 | 63.4 | 24 031 | 107 | 37 |
| Non-Hispanic black | 4 675 | 12.3 | 4 668 | 7 | 10 |
| Non-Hispanic native American | 527 | 1.4 | 526 | 1 | –c |
| Non-Hispanic native Hawaiian/other Pacific islanders | 167 | 44 | 167 | 0 | –c |
| Non-Hispanic Asian Americans | 1 484 | 3.9 | 1 479 | 5 | –c |
| Non-Hispanic more than one race/ethnicity | 1 103 | 2.9 | 1 096 | 7 | 30 |
| Hispanic | 5 973 | 15.7 | 5 957 | 16 | 15 |
| Income | |||||
| Less than $20 000 | 9 552 | 25.1 | 9 520 | 32 | 22 |
| $20 000–$49 999 | 13 183 | 34.6 | 13 140 | 43 | 24 |
| $50 000–$74 999 | 6 128 | 16.1 | 6 103 | 25 | 47 |
| $75 000 or more | 9 204 | 24.2 | 9 160 | 44 | 29 |
| Education | |||||
| Less than high school | 6 416 | 16.8 | 6 401 | 15 | 15 |
| High school graduate | 12 498 | 32.8 | 12 464 | 34 | 18 |
| Some college | 11 097 | 29.2 | 11 046 | 51 | 37 |
| College graduate | 8 056 | 21.2 | 8 012 | 44 | 42 |
Data from the United States National Survey on Drug Use and Health, 2009 (n=38 067).
Estimates ‘per 10 000’ allowed integer display. Of course, 30 per 10 000=three per 1000 as stated in text.
Insufficient number of observations to produce estimate for this subgroup.
In addition to estimating the use of OPS among all adults, meta-analyses were conducted to estimate the proportion with OPS help seeking among adults with MD spells and SPD. From 2004–2010, for every 1000 adults with recent MD, approximately 18 sought OPS (95% CI 0.016–0.021). For every 1000 adults with recent SPD, approximately 15 sought OPS (95% CI 0.013–0.017). Meta-analyses also estimated the extent to which OPS is used with or in isolation from other forms of help seeking. Table 2 documents overlap in the use of OPS, in-person support groups, and traditional treatment (i.e. in-patient treatment, out-patient treatment, or prescribed medicine). To illustrate, among adults with recent OPS use, roughly one-quarter (26%) also had used an in-person support group (95% CI 0.22–0.30) and slightly more than one-half (57%) had recently received traditional treatment (95% CI 0.52–0.62). Attention now turns to our primary aim of estimating the associations between seeking OPS and having neuropsychiatric ailments.
Table 2.
Nationally representative epidemiological estimates of adult use of mental health support venuesa
| 2009
|
2004–2010
|
|||
|---|---|---|---|---|
| Proportion | 95% CI | Proportion | 95% CI | |
| All adults, n | 38 067 | 264 431 | ||
| Online peer support users | 0.003 | (0.002–0.004) | 0.003 | (0.0027–0.0033) |
| In-person support users | 0.010 | (0.008–0.012) | 0.011 | (0.010–0.011) |
| Traditional treatment users | 0.137 | (0.131–0.143) | 0.13 | (0.128–0.132) |
| Online peer support users, no in-person support | 0.002 | (0.001–0.003) | 0.002 | (0.002–0.002) |
| Online peer support users, no traditional treatment | 0.001 | (0.001–0.001) | 0.001 | (0.001–0.001) |
| Online peer support and in-person support users | 0.001 | (0.001–0.001) | 0.001 | (0.001–0.001) |
| Online peer support and traditional treatment users | 0.002 | (0.001–0.002) | 0.002 | (0.001–0.002) |
| Adult peer support users, n | 143 | 1013 | ||
| In-person support users | 0.30 | (0.177–0.421) | 0.26 | (0.219–0.304) |
| Traditional treatment users | 0.64 | (0.503–0.777) | 0.57 | (0.523–0.619) |
| In-person support users, n | 370 | 2717 | ||
| Online support users | 0.084 | (0.041–0.127) | 0.07 | (0.056–0.08) |
| Traditional treatment users, n | 5066 | 34 462 | ||
| Online support users | 0.014 | (0.010–0.018) | 0.01 | (0.011–0.015) |
CI, Confidence interval.
Weighted proportions from 2009 and meta-estimates from 2004–2010. Data from the United States National Survey on Drug Use and Health, 2004–2010.
In the exploratory analysis of NSDUH 2009 data, both before and after covariate adjustment, a strong OPS–MD association was observed; adults with a history of MD were over-represented among recent OPS help seekers. The covariate-adjusted OPS–MD OR was 7.7 [adjusted OR (aOR) 7.7, 95% CI 4.5–13.2, p<0.001], holding constant age, sex, race/ethnicity and income level, as shown in panel A of Table 3. With education replacing income in the regression model, the aOR estimate was 7.5 (p<0.001). Systematic replication using data from the other six independent national samples yielded a range of covariate-adjusted OR estimates from 5.5 (2004) to 10.3 (2010), and a meta-analytic summary estimate of 7.4 (95% CI 6.0–9.0). A heterogeneity χ2 p value of 0.63 indicates relative consistency of the year-specific estimates. The first rows of Table 3, panel A, present crude ORs, aORs and 95% CIs for the 2009 analysis and for the meta-analytic summary estimates based on all seven independent replicate samples. The Supplementary Online Appendix tables present year-specific OR estimates (eTables 8–9).
Table 3.
Nationally representative epidemiological estimates of the association linking online peer support help seeking with MD and recent SPD, 2009 and 2004–2010a
| NSDUH 2009 weighted unadjusted estimates
|
NSDUH 2009 weighted adjusted estimates
|
NSDUH 2004–2010 weighted unadjusted meta-analysis summary
|
NSDUH 2004–2010 weighted adjusted meta-analysis summary
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | p | aORh | (95% CI) | p | OR | (95% CI) | aORh | (95% CI) | |
| Panel A | ||||||||||
| MD in lifetimeb | 9.6 | (5.6–16.4) | <0.001 | 7.7 | (4.5–13.2) | <0.001 | 9.5 | (7.6–11.6 | 7.4 | (6.0–9.0) |
| MD in past yearc | 10.4 | (6.7–16.1) | <0.001 | 8.8 | (5.5–13.9) | <0.001 | 10.0 | (8.2–12.2) | 8.2 | (6.7–10.0) |
| MD adult-onsetd | 0.43 | (0.18–1.0) | 0.062 | 0.46 | (0.17–1.2) | 0.120 | 0.45 | (0.33–0.58) | 0.5 | (0.38–0.67) |
| SPDe | 10.6 | (5.3–21.3) | <0.001 | 9.2 | (4.3–19.7) | <0.001 | 10 | (8.2–12.2) | 7.4 | (6.0–9.0) |
| Panel Bf | ||||||||||
| MD in past year, with pre-adult MD onset | 18.3 | (8.6–38.8) | <0.001 | 13.4 | (6.3–28.7) | <0.001 | 18.1 | (13.5–24.5) | 13.5 | (10.0–16.4) |
| MD in past year, with adult MD onset | 12.1 | (5.9–25.0) | <0.001 | 11.0 | (5.2–23.6) | <0.001 | 11.0 | (8.1–14.9) | 9.0 | (6.7–11.0) |
| No MD past year, but pre-adult MD onset | 14.4 | (5.0–41.3) | <0.001 | 10.5 | (3.8–29.0) | <0.001 | 11 | (7.4–14.9) | 6.7 | (4.5–10.0) |
| No MD past year, but adult MD onset | 2.3 | (0.65–8.2) | 0.19 | 1.8 | (0.52–6.5) | 0.34 | 3.3 | (2.5–4.9) | 2.7 | (1.8–4.1) |
| Panel Cg | ||||||||||
| MD in past year, with SPD | 15.8 | (8.9–27.8) | <0.001 | 12.3 | (1.3–20.5) | <0.001 | 14.9 | (12.1–20.1) | 11.0 | (9.0–15.0) |
| MD in past year, with no SPD | 9.7 | (3.1–30.7) | <0.001 | 8.9 | (2.7–29.6) | 0.001 | 7.4 | (5.5–11.0) | 7.4 | (5.0–10.0) |
| No MD in past year, with SPD | 8.3 | (2.7–25.4) | <0.001 | 6.1 | (2.0–18.4) | 0.002 | 10.7 | (7.4–16.4) | 7.4 | (5.5–11.0) |
| MD in past year and no SPD | 4.7 | (1.7–13.5) | 0.004 | 3.7 | (1.3–10.5) | 0.013 | 3.7 | (2.5–5.5) | 3.0 | (2.1–4.5) |
MD, Major depression; SPD, serious psychological distress; NSDUH, National Survey of Drug Use and Health; OR, odds ratio; CI, confidence interval; aOR, adjusted OR.
Data from the United States NSDUH, 2004–2010 (n for 2009=37 560 adults and n for 2004–2010=264 431). Weighted interview response rates for the computer-assisted interview (rates reflect original sample): 2010=74.7; 2009=75.7; 2008=74.4; 2007=73.9; 2006=74; 2005=76; 2004=77.
Reference category, adults with no history of recent or past MD.
Reference category, all other adults (never cases, and those with past MD).
Reference category, adults with earlier-onset depression spells (before age 18 years).
Reference category, adults with no recent SPD.
Reference category, adults with no history of recent or past MD.
Reference category, adults with no history of recent or past MD and no recent SPD.
Covariate adjustment for sex, age, race/ethnicity and income.
The exploratory NSDUH 2009 analysis probed whether the associations might be stronger for recently active MD. Nevertheless, according to covariate-adjusted OR estimates from the 2009 data, the odds of OPS help seeking for cases with recent depression (within 12 months of assessment) are an estimated 8.8 times greater than the corresponding OPS odds for adults without recent depression (95% CI 5.5–13.9, p<0.001; panel A of Table 3), not appreciably different from the association based on lifetime MD history. The meta-analytic summary estimate is 8.2 (aOR 8.2, 95% CI 6.7–10.0), based on year-specific aOR estimates, 2004–2010 (heterogeneity χ2 p=0.44; see Supplementary Online Appendix, eTables 10–11a). These study estimates changed modestly when the analysis model was re-specified to remove adults with a past history of depression from the multiple regression reference category (aOR 10.4, 95% CI 8.3–13.0, p<0.001; see eTables 10a, 11a).
Stratification by recent traditional mental health treatment experience sheds some light on whether OPS–depression associations might be due to referrals from MHS providers such as neuropsychiatrist specialists. OPS–depression associations were much attenuated when traditional treatment had occurred (meta-analytic aOR 2.2, 95% CI 1.8–2.5, heterogeneity χ2 p=0.45; data not shown in a table). Nonetheless, OPS–depression associations were quite strong for adults with no recent traditional treatment (meta-analytic aOR 9.0, 95% CI 6.0–12.2, heterogeneity χ2 p=0.45).
The exploratory NSDUH 2009 analysis suggested subgroup variation in the odds of OPS help-seeking behavior across adult subgroups defined by earlier-onset versus later-onset spells of depression (eTables 12, 13). Panel B in Table 3 details this subgroup variation. A strong association was found for adults having pre-adult onset of a depression spell combined with a recent MD spell (meta-analysis: aOR 13.5, 95% CI 10.0–16.4, heterogeneity χ2 p=0.86; Table 3, panel B). In contrast, the OPS–depression association was markedly smaller and was not statistically significant at p<0.05 in the contrast of non-cases versus adult-onset MD cases having no recent depression spells, initially estimated as aOR=1.8 (95% CI 0.52–6.5, p=0.34). The relatively weak association was confirmed in the meta-analysis, but was non-null (aOR 2.7, 95% CI 1.8–4.1; Table 3, panel B). Year-specific OPS–depression estimates for this subgroup variation are presented in the Supplementary Online Appendix (eTables 24–31).
The NSDUH 2009 data also were used to explore the possibility that OPS help seeking might be prompted by recent SPD in general rather than by MD specifically. Cases with SPD were some 9–11 times more likely to be recent OPS help seekers (crude unadjusted OR 10.6, aOR 9.2, 95% CI 4.3–19.7, p<0.001). As shown in Table 3, panel A, the corresponding meta-analytic aOR summary estimate was 7.4 (95% CI 6.0–9.0, heterogeneity χ2 p=0.83).
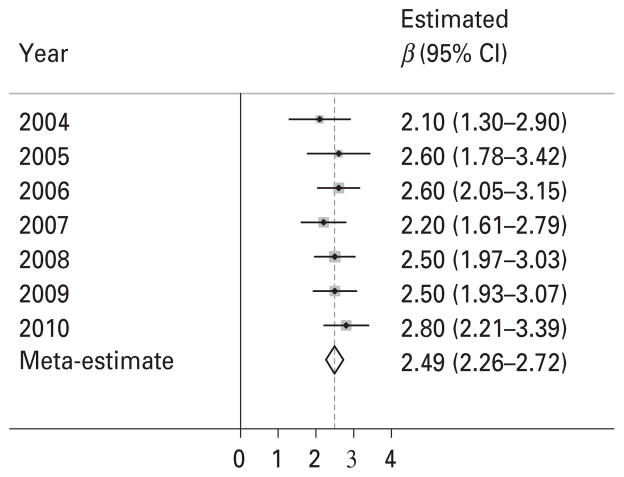
Co-occurrence of recent SPD and MD was studied using four subgroups as shown in panel C of Table 3. There was a moderately strong OPS–SPD association for adults recently affected by SPD but not MD (aOR from 2009=6.1, 95% CI 2.0–18.4, p=0.002); the meta-analysis summary estimate was 7.4 (95% CI 5.5–11.0; panel C of Table 3). Nonetheless, OPS–depression associations also were quite strong when there was recent MD but no recent SPD (meta-analytic aOR 7.4, 95% CI 5.0–10.0). Relative to the reference category (never MD and no recent SPD), the estimated odds of OPS help seeking were largest for recent MD cases with recent SPD (meta-analytic aOR 11.0, 95% CI 9.0–15.0; panel C of Table 3). Fig. 1 provides a display of the year-specific regression model slope estimates (i.e. β), as well as the meta-analysis summary estimate, with education replacing income as a facet of socioeconomic status. Anti-logged, the adjusted β of 2.49 yields a large OR estimate, 12.1 (95% CI 9.6–15.2), not appreciably different from the Table 3, panel C estimate.
Fig. 1.
Estimated association that links recently co-occurring major depression and serious psychological distress with recent seeking of online mental health support. Data from the United States National Surveys on Drug Use and Health, 2004–2010. Estimates are adjusted for sex, age, race/ethnicity and education. CI, Confidence interval.
OPS–depression associations are considerably smaller when past MD cases (i.e. lifetime but not recent MD) had no recent SPD (aOR from 2009=3.7, 95% CI 1.3–10.5, p=0.013; meta-analytic summary aOR 3.0, 95% CI 2.1–4.5; panel C of Table 3). Year-specific estimates were generally consistent and all meta-analyses from this work yielded heterogeneity χ2 p values greater than 0.20 (as presented in the Supplementary Online Appendix; eTables 14–23).
Whereas the focus of this report is on associations germane to MD and SPD, some readers may be interested in associations linking OPS with the background control variables. Table 4 presents initial estimates from NSDUH 2009 exploratory analyses, plus meta-analytic summary estimates from all seven replications (with covariates as listed in the footnote to Table 4, including MD and SPD). In summary, females (versus males) are over-represented among OPS help seekers, as are adults under the age of 50 years; minorities are under-represented (Table 4). For the most part, no appreciable income-related variation in OPS activities was seen, but an interesting pattern involves education. As shown in Table 4, better-educated adults in the USA are more likely to be OPS help seekers.
Table 4.
Nationally representative epidemiological estimates of the association linking online peer support help seeking with background predictors and correlatesa
| NSDUH 2009 weighted unadjusted
|
NSDUH 2009 weighted adjusted
|
NSDUH 2004–2010 weighted unadjusted meta-analysis summary
|
NSDUH 2004–2010 weighted adjusted meta-analysis summary
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | p | aORb | (95% CI) | p | OR | (95% CI) | aORb | (95% CI) | |
| Sex | ||||||||||
| Female | 2.6 | (1.5–4.6) | 0.001 | 2.1 | (1.2–3.8) | 0.010 | 2.4 | (1.9–3.0) | 1.9 | (1.5–2.4) |
| Male (ref) | 1.0 | – | – | 1.0 | – | – | 1.0 | – | 1.0 | – |
| Age, years | ||||||||||
| 18–25 | 2.2 | (1.2–4.1) | 0.012 | 2.1 | (1.2–4.0) | 0.015 | 3.3 | (2.5–4.5) | 2.7 | (2.0–4.1) |
| 26–34 | 2.2 | (1.1–4.4) | 0.022 | 2.0 | (1.0–3.9) | 0.040 | 4.1 | (2.7–5.5) | 3.3 | (2.4–5.0) |
| 35–49 | 1.3 | (0.6–2.5) | 0.461 | 1.1 | (0.6–2.2) | 0.690 | 3.0 | (2.3–4.1) | 2.5 | (1.8–3.3) |
| 50+(ref) | 1.0 | – | – | 1.0 | – | – | 1.0 | – | 1.0 | – |
| Race/ethnicity | ||||||||||
| Hispanic | 0.4 | (0.2–0.8) | 0.013 | 0.47 | (0.2–0.95) | 0.036 | 0.5 | (0.4–0.7) | 0.5 | (0.4–0.7) |
| Non-Hispanic black | 0.26 | (0.1–0.7) | 0.012 | 0.31 | (0.1–0.9) | 0.030 | 0.5 | (0.3–0.7) | 0.5 | (0.4–0.8) |
| Non-Hispanic white (ref) | 1.0 | – | – | 1.0 | – | – | 1.0 | – | 1.0 | – |
| Income ($US) | ||||||||||
| Under $20 000 (ref) | 1.0 | – | – | 1.0 | – | – | 1.0 | – | 1.0 | – |
| $20 000–$49 999 | 1.1 | (0.5–2.3) | 0.809 | 1.3 | (0.6–2.8) | 0.460 | 0.88 | (0.7–1.1) | 1.1 | (0.8–1.4) |
| $50 000–$74 999 | 2.1 | (1.0–4.3) | 0.042 | 2.4 | (1.2–5.0) | 0.020 | 0.93 | (0.7–1.2) | 1.0 | (0.8–1.4) |
| $75 000 or more | 1.3 | (0.7–2.5) | 0.440 | 1.7 | (0.9–3.2) | 0.120 | 0.83 | (0.6–1.1) | 1.0 | (0.8–1.3) |
| Educational attainment | ||||||||||
| Less than high school (ref) | 1.0 | – | – | 1.0 | – | – | 1.0 | – | 1.0 | – |
| High school graduate | 1.2 | (0.6–2.4) | 0.590 | 1 | (0.5–2.1) | 0.98 | 1.1 | (0.8–1.6) | 1.0 | (0.7–1.5) |
| Some college | 2.4 | (1.1–5.7) | 0.036 | 1.8 | (0.8–4.2) | 0.18 | 2.7 | (1.9–4.1) | 2 | (1.4–2.7) |
| College graduate | 2.7 | (1.2–6.5) | 0.022 | 2.4 | (0.98–5.9) | 0.056 | 2.7 | (2.1–4.5) | 2.7 | (1.9–4.1) |
NSDUH, National Survey of Drug Use and Health; OR, odds ratio; CI, confidence interval; aOR, adjusted OR; ref, reference.
Data from the United States NSDUH, 2004–2010 (n for 2009=37 560 adults and n for 2004–2010=264 431).
All adjusted analyses include sex, age, race, income, major depression and serious psychological distress, except the adjusted analyses for the education variable, which did not include income in the model.
Discussion
In brief, three main discoveries can be seen in this study’s estimates from the initial NSDUH 2009 nationally representative US survey data, confirmed via a meta-analytic approach with annual surveys 2004–2010. First, as gauged by 95% CI for the study’s meta-analytic summary estimates, an estimated 2.7 to 3.3 per 1000 adults visit online mental health chat rooms or other peer social support groups each year, with no evidence of any increasing trend in such visits across the years 2004–2010, despite apparent increases in Internet access and online activities during this interval (Pew Internet and American Life Project, 2012). Second, adults with recent MD and/or SPD are markedly over-represented among OPS help seekers, but the OPS–depression association is modest among adults receiving traditional MHS (e.g. from specialists). Third, it is possible to map a few population subgroups now over-represented among the OPS help seekers. To illustrate, even with MD/SPD held constant via multiple logistic regression, OPS help seeking is more often seen among females (versus males), among adults aged under 50 years (versus 50+ years) and among the college-educated (versus those who never attended college). OPS help seeking is less often seen among traditionally disadvantaged Hispanic and non-Hispanic black minority subgroups in the USA (versus non-Hispanic whites).
Before any more detailed discussion of the study findings, several methodological limitations merit attention. First, whereas NSDUH samples include adolescents, only adults are asked about OPS; estimated OPS frequency might be greater in the newest generation of US adolescents. Second, the survey design thwarts firm causal inference. For example, we cannot tell whether psychiatric disturbances preceded the first OPS visit, or vice versa. Third, the survey modules include no questions on topics that one might wish to explore, such as frequency of Internet use. In addition, to protect privacy and confidentiality of individual participants, the NSDUH public use datasets do not include variables on area of residence (e.g. region, state, neighborhood), as might be used to study geographical variation within the USA or to construct multi-level models. Information of this type would help place OPS help seeking into a broader context. It is our expectation that future surveys will give more attention to the various types of online MHS and social support sites in the survey assessment modules. At best, the NSDUH assessment must be described as rudimentary. Nonetheless, this module is an important starting point. In future research, it should be possible to ask more specific questions about the types of online treatments and support services that have been sought by Internet users.
Keeping these limitations in mind, we think that the study estimates will be of interest because they help to fill an evidence gap about a novel form of help seeking for mental health problems, and they map out population subgroups and associations that deserve attention in more probing future studies. Estimates from this study help quantify precisely how much variation in the relationship between MD and OPS exists for those who do and do not seek traditional treatment. As noted in the Results section, the estimated OPS–depression association is only 2.2 for adults with recent traditional MHS use. In contrast, among adults without recent traditional MHS, the estimate is 9.0, due to a combination of lower levels of OPS help seeking among adults without depression plus higher levels of OPS help seeking among MD cases. Evaluated comparatively, adults with MD spells who have not received recent help from traditional MHS are more likely to be seeking OPS.
Whereas this cross-sectional study’s estimates cannot be interpreted with cause–effect thinking, it seems unlikely that going online to seek mental health social support or chat room self-help would be a potent cause of depression or psychological distress. Rather, the observed robust associations are more likely to arise because mental disturbances prompt online help seeking. Alternatively, it might be true that OPS activities displace other forms of more beneficial help seeking, irrespective of whether OPS is efficacious or inert. The result could be an association between ‘being a case with MD’ and ‘help seeking via OPS activities’ because this form of help seeking is associated with longer duration or persistence of the mental disturbance.
Our capacity to interpret the observed OPS associations with sex, age, race/ethnicity and education also is limited. For example, the under-representation of traditionally disadvantaged minority subpopulations may be reflective of a ‘digital divide’ generally, and might disappear in research that holds constant Internet access and frequency of Internet usage. Having said this, we note that in previous research women have been found to seek social support for mental health problems more often than men, online or offline (Thoits, 1995; Walther & Boyd, 2002), and the same seems to be true for subgroups of young-to-middle-aged adults (Han et al. 2011), and perhaps for college-educated adults (Folkman et al. 1987; Bauman et al. 1992). In this context, it may be pertinent to note that this study’s OPS associations tend to mirror previous results that women, younger individuals, educated individuals and non-Hispanic whites are more likely to seek online information or health services, including information about medical professionals and alternative treatments (Fox & Jones, 2009). Alternatively, some of the OPS subgroup variations observed in this study might be traced back to subgroup variations in unmet needs for mental health care (Kataoka et al. 2002; Barrio et al. 2008).
A variety of explanations have been offered to account for differences in mental health treatment service use across US subpopulations defined by race and ethnicity, including special challenges faced by some members of disadvantaged minority subpopulations in this country. Some of these explanations (e.g. language barriers, English language fluency) seem more applicable to the context of online support than others (e.g. illegal residency status). As is true for the primary OPS–depression association observed here, more research will be needed to clarify the interpretation of these basic OPS associations. A basis for theoretical grounding for these future investigations can be found in research on diffusion of innovations generally, as well as subgroup variations in the adoption of new medical treatments specifically. To illustrate, Srole et al. (1962) in the classic midtown Manhattan mental health survey of the 1950s expressed a view that psychotherapy, upon introduction, was rejected by older adults, perhaps because they did not see it as an acceptable form of treatment for mental health problems. Studies on adoption of new medicines (e.g. prescribing of newly marketed psychotherapeutic drugs) also have highlighted education specifically or socio-economic status generally as partial determinants of disparities, but such disparities may only exist for those with a low to moderate need for treatment (Manheimer et al. 1968; United States Substance Abuse and Mental Health Services Administration, 2012).
To conclude by placing the current study estimates into a larger context, there are recent estimates that approximately 60% of adults in the USA now go online for health information and that roughly 80% of all adults have some degree of access to the Internet, either at home, school, work, or via a neighbor or relative living close by (Pew Internet and American Life Project, 2012). By comparison, in 2000, fewer than one-half of US adults had access to the Internet. For this reason, we were somewhat surprised to find no increase in our relatively stable estimate of about 0.3% for OPS help seeking each year from 2004 to 2010. Nonetheless, our forecast is one that posits a future increase, in that commercial services already are attempting to address what US adults have reported as considerable unmet need for mental health care (United States Substance Abuse and Mental Health Services Administration, 2012). If we are correct, the most pressing need may be for definitive evidence about the conditions under which OPS and services can be most efficacious; randomized controlled trials are needed.
Supplementary Material
Acknowledgments
This study was supported with funds from the National Institute on Drug Abuse grants R01DA016558, K05DA015799 (to J.C.A.) and T32DA021129, as well as Michigan State University (MSU). The content is the sole responsibility of the authors and does not necessarily represent the official views of MSU, the National Institute on Drug Abuse, or the National Institutes of Health. The authors wish to thank the United States Substance Abuse and Mental Health Services Administration Office of Applied Studies (now the Center for Behavioral Health Statistics and Quality) for completion of its annual nationally representative surveys on drug use and health, as well as its direction and supervision of the annual data gathering and preparation of public use datasets. Financial disclosure statements document federal support of the research and research training and occasional technical assistance and consultation in pharmaceutical industry research and for non-profit foundations, educational institutions, and the federal government.
Appendix A. NSDUH Assessment of Online Mental Health Support
-
All adults are first asked the following question within the ‘Adult Mental Health Service Utilization’ portion of the NSDUH:
‘Earlier, we asked whether you have received prescription medicines, inpatient treatment or outpatient treatment for your emotions, nerves or mental health. The list below contains possible sources of treatment, counseling or support that were not mentioned before.
Acupuncturist or acupressurist
Chiropractor
Herbalist
In-person support group or self-help group
Internet support group or chat room
Spiritual or religious advisor, such as a pastor, priest, rabbi
Telephone hotline
Massage therapist
Did you receive treatment, counseling or support from any other sources such as these during the past 12 months?’ Response options were ‘yes’ or ‘no’.
-
Adults who responded ‘yes’ to the above question were then asked to indicate:
‘From what source did you receive other treatment, counseling or support for problems with your emotions, nerves or mental health in the past 12 months? To select more than one source from the list, press the space bar between each number you type.’
Acupuncturist or acupressurist
Chiropractor
Herbalist
In-person support group or self-help group
Internet support group or chat room
Spiritual or religious advisor, such as a pastor, priest, rabbi
Telephone hotline
Massage therapist
Other (specify)
AUALINET is a binary summary variable based on this multiple response variable; it encodes which respondent did or did not make use of an ‘Internet support group or chat room’.
The main outcome measure employed in this study was constructed as follows:
0=Adults whose mental health help-seeking experience did not include use of an ‘Internet support group or chat room’.
1=Adults whose mental health help-seeking experience did include use of an ‘Internet support group or chat room’.
Footnotes
Declaration of Interest
None.
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291713000172.
References
- APA. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. 4. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Atkinson NL, Saperstein SL, Pleis J. Using the Internet for health-related activities: findings from a national probability sample. Journal of Medical Internet Research. 2009;11:e4. doi: 10.2196/jmir.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker L, Wagner TH, Singer S, Bundorf MK. Use of the Internet and e-mail for health care information: results from a national survey. Journal of the American Medical Association. 2003;289:2400–2406. doi: 10.1001/jama.289.18.2400. [DOI] [PubMed] [Google Scholar]
- Barak A, Proudfoot JG, Klein B. Defining Internet-supported therapeutic interventions. Annals of Behavioral Medicine. 2009;38:4–17. doi: 10.1007/s12160-009-9130-7. [DOI] [PubMed] [Google Scholar]
- Barrio C, Palinkas LA, Yamada AM, Fuentes D, Criado V, Garcia P, Jeste DV. Unmet needs for mental health services for Latino older adults: perspectives from consumers, family members, advocates, and service providers. Community Mental Health Journal. 2008;44:57–74. doi: 10.1007/s10597-007-9112-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman LJ, Gervey R, Siegel K. Factors associated with cancer patients’ participation in support groups. Journal of Psychosocial Oncology. 1992;10:1–20. [Google Scholar]
- Berger M, Wagner TH, Baker LC. Internet use and stigmatized illness. Social Science and Medicine. 2005;61:1821–1827. doi: 10.1016/j.socscimed.2005.03.025. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Wu LT. The epidemiology of substance use and disorders among middle aged and elderly community adults: National Survey on Drug Use and Health (NSDUH) American Journal of Geriatric Psychiatry. 2009;17:237–245. doi: 10.1097/JGP.0b013e318190b8ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A. Health related virtual communities and electronic support groups: systematic review of the effects of online peer to peer interactions. British Medical Journal. 2004;328:1166. doi: 10.1136/bmj.328.7449.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS, Pimley S, Novacek J. Age differences in stress and coping processes. Psychology and Aging. 1987;2:171–184. doi: 10.1037//0882-7974.2.2.171. [DOI] [PubMed] [Google Scholar]
- Fox S. [Accessed 1 April 2012.];Peer-to-peer healthcare. 2011 ( http://www.pewinternet.org/Reports/2011/P2PHealthcare.aspx)
- Fox S, Jones S. [Accessed 1 April 2012.];The social life of health information. 2009 ( http://www.pewinternet.org/~/media//Files/Reports/2009/PIP_Health_2009.pdf)
- Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychological Medicine. 2003;33:357–362. doi: 10.1017/s0033291702006700. [DOI] [PubMed] [Google Scholar]
- Goldstrom ID, Campbell J, Rogers JA, Lambert DB, Blacklow B, Henderson MJ, Manderscheid RW. National estimates for mental health mutual support groups, self-help organizations, and consumer-operated services. Administration and Policy in Mental Health and Mental Health Services Research. 2006;33:92–103. doi: 10.1007/s10488-005-0019-x. [DOI] [PubMed] [Google Scholar]
- Griffiths KM, Farrer L, Christensen H. The efficacy of Internet interventions for depression and anxiety disorders: a review of randomised controlled trials. Medical Journal of Australia. 2010;192:S4–S11. doi: 10.5694/j.1326-5377.2010.tb03685.x. [DOI] [PubMed] [Google Scholar]
- Han B, Gfroerer JC, Colpe LJ, Barker PR, Colliver JD. Serious psychological distress and mental health service use among community-dwelling older U.S. adults. Psychiatric Services. 2011;62:291–298. doi: 10.1176/ps.62.3.pss6203_0291. [DOI] [PubMed] [Google Scholar]
- Hesse BW, Nelson DE, Kreps GL, Croyle RT, Arora NK, Rimer BK, Viswanath K. Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Archives of Internal Medicine. 2005;165:2618–2624. doi: 10.1001/archinte.165.22.2618. [DOI] [PubMed] [Google Scholar]
- Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among US children: variation by ethnicity and insurance status. American Journal of Psychiatry. 2002;159:1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Leykin Y, Munoz RF, Contreras O. Are consumers of Internet health information “cyberchondriacs” ? Characteristics of 24,965 users of a depression screening site. Depression and Anxiety. 2012;29:71–77. doi: 10.1002/da.20848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manheimer DI, Mellinger GD, Balter MB. Psychotherapeutic drugs: use among adults in California. California Medical Journal. 1968;109:445–451. [PMC free article] [PubMed] [Google Scholar]
- Owen JE, Boxley L, Goldstein MS, Lee JH, Breen N, Rowland JH. Use of health-related online support groups: population data from the California health interview survey complementary and alternative medicine study. Journal of Computer Mediated Communication. 2010;15:427–446. [Google Scholar]
- Pew Internet and American Life Project. [Accessed 4 May 2012.];Usage over time. 2012 ( http://pewinternet.org/Trend-Data/Usage-Over-Time.aspx)
- Powell J, Clarke A. Internet information-seeking in mental health: population survey. British Journal of Psychiatry. 2006;189:273–277. doi: 10.1192/bjp.bp.105.017319. [DOI] [PubMed] [Google Scholar]
- Powell J, McCarthy N, Eysenbach G. Cross-sectional survey of users of Internet depression communities. BMC Psychiatry. 2003;3:19. doi: 10.1186/1471-244X-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srole L, Langer TS, Michael ST, Opler MK, Rennie TAC. Mental Health in the Metropolis: The Midtown Manhattan Study. McGraw Hill; New York: 1962. [Google Scholar]
- Thoits PA. Stress, coping, and social support processes: Where are we? What next ? Journal of Health and Social Behavior. 1995;35:53–79. [PubMed] [Google Scholar]
- United States Substance Abuse and Mental Health Services Administration. [Accessed 1 December 2011.];National Survey on Drug Use and Health. 2009 ( http://dx.doi.org/10.3886/ICPSR29621.v1)
- United States Substance Abuse and Mental Health Services Administration, Office of Applied Studies. The NSDUH report: Mental health support and self-help groups. Rockville, MD: 2009. [Accessed 7 May 2012.]. ( http://www.samhsa.gov/data/2k9/161/161MHSupportGroup.htm) [Google Scholar]
- United States Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Mental health findings. Rockville, MD: 2012. [Accessed 28 January 2013.]. pp. 11–4667. NSDUH Series H-42, HHS Publication No. (SMA) ( http://www.samhsa.gov/data/nsduh/2k10MH_Findings/2k10MHResults.htm#B.4) [Google Scholar]
- Walther JB, Boyd S. Attraction to computer-mediated social support. In: Lin CA, Atkin D, editors. Communication Technology and Society: Audience Adoption and Uses. Hampton Press; Cresskill, NJ: 2002. pp. 153–188. [Google Scholar]
- Walther JB, Pingree S, Hawkins RP, Buller DB. Attributes of interactive online health information systems. Journal of Medical Internet Research. 2005;7:e33. doi: 10.2196/jmir.7.3.e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ybarra ML, Suman M. Help seeking behavior and the Internet: a national survey. International Journal of Medical Informatics. 2006;75:29–41. doi: 10.1016/j.ijmedinf.2005.07.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.