Summary
Knowledge of the incubation period is essential in the investigation and control of infectious disease, but statements of incubation period are often poorly referenced, inconsistent, or based on limited data. In a systematic review of the literature on nine respiratory viral infections of public-health importance, we identified 436 articles with statements of incubation period and 38 with data for pooled analysis. We fitted a log-normal distribution to pooled data and found the median incubation period to be 5·6 days (95% CI 4·8–6·3) for adenovirus, 3·2 days (95% CI 2·8–3·7) for human coronavirus, 4·0 days (95% CI 3·6–4·4) for severe acute respiratory syndrome coronavirus, 1·4 days (95% CI 1·3–1·5) for influenza A, 0·6 days (95% CI 0·5–0·6) for influenza B, 12·5 days (95% CI 11·8–13·3) for measles, 2·6 days (95% CI 2·1–3·1) for parainfluenza, 4·4 days (95% CI 3·9–4·9) for respiratory syncytial virus, and 1·9 days (95% CI 1·4–2·4) for rhinovirus. When using the incubation period, it is important to consider its full distribution: the right tail for quarantine policy, the central regions for likely times and sources of infection, and the full distribution for models used in pandemic planning. Our estimates combine published data to give the detail necessary for these and other applications.
Introduction
Acute respiratory viruses cause substantial morbidity and mortality worldwide.1 Lower respiratory-tract infections are the leading cause of communicable disease death and among the top five contributors to disability-adjusted life years.2 Viruses are the primary cause of lower respiratory-tract infections in children and a substantial cause of such infections in all age-groups.3, 4
The incubation period of an infectious disease is the time between infection and symptom onset.5 This period is widely reported because it is useful in infectious disease surveillance and control, in which the time of symptom onset may be the only indication of the time of infection. Severe acute respiratory syndrome (SARS) offers a dramatic example: by rapidly determining the maximum incubation period of SARS, public-health officials were able to set quarantine periods and halt a potential pandemic without the aid of a vaccine or treatment.6, 7, 8, 9 The incubation period thus plays an essential part in surveillance for healthcare-associated infections,10, 11 and may aid in diagnosis if laboratory facilities are unavailable. The incubation period is clinically relevant in the administration of antiviral medications, many of which are most effective when given before or immediately after symptom onset.12 Epidemiological studies depend on the incubation period to identify potential sources of infection.13 Predictive models designed to inform policy decisions use the incubation period to evaluate the potential of surveillance programmes and interventions to confront emerging epidemics.14, 15 The length of the incubation period by comparison with the latent period (the time between infection and becoming infectious) determines the potential effectiveness of control measures that target symptomatic individuals.16
Statements of the incubation period are often imprecise, unsourced, or based on limited evidence—for example, “4–5 days” may refer to the most common range, the highest and lowest incubation periods in a study, or some other interval. Without knowing which summary measure is being stated, it is hard to use this information to make clinical or infection control decisions. Estimates given without attribution or based on few observations do not meet the standards of evidence we demand for modern medical information.
We reviewed the literature on nine respiratory viruses selected for their clinical or public-health importance: adenovirus, human coronavirus, SARS-associated coronavirus, influenza, measles, human metapneumovirus, parainfluenza, respiratory syncytial virus (RSV), and rhinovirus.17 By systematic review and analysis of published estimates and data, we aim to (1) capture the consensus in the medical literature on these incubation periods, (2) characterise the evidence underlying this consensus, and (3) provide improved estimates of incubation periods for these infections. Previous reviews show the importance of the incubation period to the epidemiology of both infectious and non-infectious disease.18, 19, 20 However, we know of no other attempt to combine published data and use a common method for estimating and reporting the incubation period for a broad range of respiratory virus infections.
Methods
Search strategy and selection criteria
For each virus, we searched PubMed, Google Scholar, and ISI Web of Knowledge 4.0 with no restrictions on language, although non-English documents were excluded on abstract review. Searches were done between May, 2007, and January, 2008, with no restriction on the earliest date of the articles returned. On PubMed, we searched for the terms “incubation”, “period”, and the virus name; on Google Scholar we searched for the phrases “incubation period of [virus name]” and “incubation period for [virus name]”; and on ISI Web of Knowledge, we searched for “incubation period” and the virus name. Each search was done with common variations of the virus name, specifically: “adenovirus”, “coronavirus”, “human coronavirus”, “HCoV”, “severe acute respiratory syndrome”, “SARS”, “influenza”, “measles”, “human metapneumovirus”, “hMPV”, “parainfluenza”, “HPIV”, “respiratory syncytial virus”, “RSV”, and “rhinovirus”. We also reviewed four widely used infectious disease references,3, 12, 21, 22 as well as several library catalogues and the Cochrane Library.
Non-English documents and dead links returned by Google Scholar were excluded from abstract review. Abstracts were reviewed by a single reviewer, and excluded from full-text review if they were definitively about a different disease, a non-human study, or a non-respiratory manifestation of the disease. Otherwise, all other articles returned by the searches were included in full-text review.
Assessment
Documents in the full-text review were classified as containing: (1) an incubation period estimate based on original data or analysis, (2) a sourced statement of the incubation period (ie, citation given), (3) an unsourced statement of the incubation period (ie, no citation given), and/or (4) no statement of the incubation period. Relevant citations were similarly reviewed. Documents were further classified based on whether they contained individual-level data appropriate for analysis. Each paper potentially containing original data was examined independently by two reviewers for figures, tables, or text describing individual-level incubation period data. Discrepancies between reviewers were resolved by discussion and consensus.
Data abstraction
Variance or SDs are rarely reported for incubation periods, which makes standard meta-analytic techniques ineffective. To confront this issue, we separately summarised the statements in the literature and reanalysed published individual-level data (via a pooled analysis). The pooled analysis allows standard treatment of censored observations (ie, those cases when the incubation period is not exactly observed) across studies.
We classified all statements of the incubation period (categories 1–3) into two types: statements of the interval of the incubation period (including maxima and minima), and statements of central tendency (ie, median, mode, or mean). Observations in tables, figures, or text that gave an exact incubation period, a range of possible times for exposure and symptom onset, or a range of potential incubation periods were included. If the incubation period was not measured exactly, data were represented as single interval-censored observations covering the range of possible incubation periods. For example, if an individual was infected between 0600 h on March 12 and 0600 h on March 14, and then developed symptoms between 0600 h on March 16 and 0600 h on March 17, we represent this as an interval-censored observation of an incubation period of between 2 and 5 days. We report the range of incubation periods such that an incubation period within that range would be consistent with the predictions of most investigators (ie, consistent with over 50% of published estimates), and the modal statement of central tendency.
Pooled analysis
In his classic paper, Sartwell19 showed that for most acute infectious diseases the log-incubation periods follow a normal distribution; hence the incubation period follows a log-normal distribution specified by the median incubation period and a dispersion factor.19, 23 In a normal distribution, approximately two-thirds of the data fall within one SD of the mean; similarly, in a log-normal distribution, approximately two-thirds of cases develop symptoms between median/dispersion and median×dispersion.
For each disease, all observations were pooled together as a single set of singly interval-censored observations, and maximum-likelihood estimates for the median and dispersion were found by use of standard techniques. Estimates of the 5th, 25th, 75th, and 95th percentiles were calculated, and CIs were obtained by use of the delta method.24 For one virus (human coronavirus), standard methods for maximum likelihood estimation did not converge, and an estimate obtained by use of Bayesian methods is reported. To account for the potential effect of differences between studies, hierarchical models allowing for study-specific medians were fit to the data. In most cases, these models produced estimates nearly identical to the pooled estimates (results not shown). Technical details are available in the webappendix. All analysis was done using the R statistical package (version 2·6). Specific estimates found in this review, all data used in pooled analyses, and a full bibliography (including excluded abstracts and study classification) are available from the authors on request.
Results
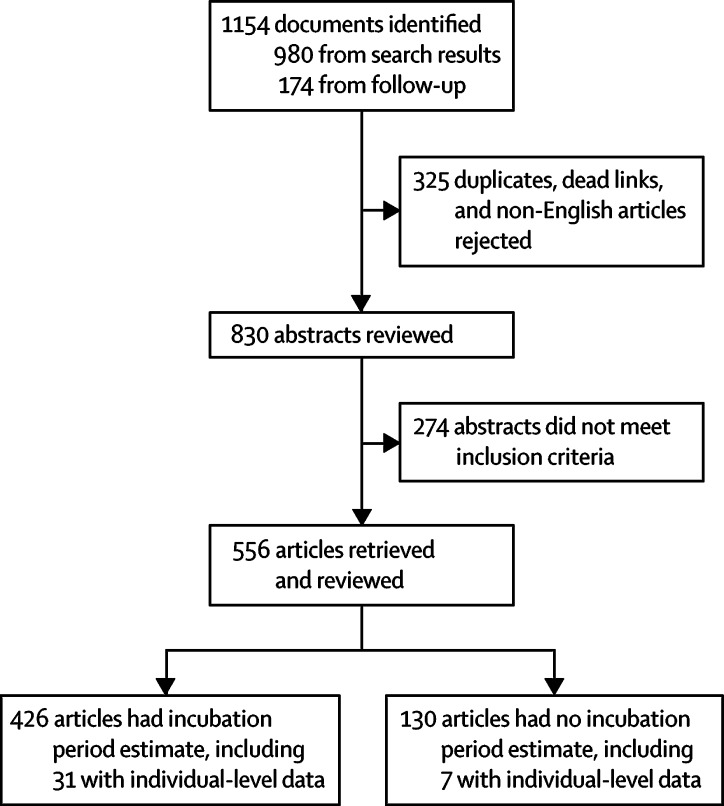
We identified 426 documents with one or more statements of incubation period (figure 1 ). Of the 441 estimates that appeared in these documents, 77 (17%) estimates were original, 168 (38%) gave a source, and 197 (45%) gave no source (table 1 ). 38 articles contained data appropriate for analysis (table 2 ). 24 (63%) were observational studies and 14 (37%) were experimental studies. Table 1 summarises the incubation periods stated in the literature and the underlying data. Estimates for the incubation period of SARS-associated coronavirus and influenza have the most support (more than ten studies). Relatively large experimental studies of parainfluenza and rhinovirus have been done, but few observational or experimental studies (six or fewer) were available for other diseases.
Figure 1.
Systematic review process
Table 1.
Summary of incubation period estimates in published literature
|
Literature estimates*(days) |
Number of estimates (%) |
Participants in experimental†studies (n) | |||||
|---|---|---|---|---|---|---|---|
| Range | Central tendency | Unsourced estimates | Sourced estimates | Original estimates [experimental/observational] | |||
| Adenovirus | 4–8 | 6 | 11 (73%) | 2 (13%) | 2 (13%) [1/1] | 14 | |
| Coronavirus | |||||||
| Human (non-SARS) | 2–5 | 3 | 2 (25%) | 4 (50%) | 2 (25%) [2/0] | 37 | |
| SARS-associated | 2–10 | 5 | 65 (37%) | 81 (46%) | 30 (17%) [0/30‡] | .. | |
| Influenza | 1–4 | 2 | 54 (50%) | 37 (35%) | 16 (15%) [5/11] | 133 | |
| Human metapneumovirus | .. | .. | 4 (44%) | 3 (33%) | 2 (22%) [0/2] | .. | |
| Measles | 8–14 | 10 | 32 (62%) | 16 (31%) | 5 (10%) [0/5] | .. | |
| Parainfluenza | 2–6 | 4 | 6 (35%) | 5 (29%) | 6 (35%) [4/2] | 97 | |
| Respiratory syncytial virus | 3–7 | 5 | 20 (48%) | 16 (38%) | 6 (14%) [1§/5] | 17 | |
| Rhinovirus | 2–4 | 2 | 4 (25%) | 4 (25%) | 8 (50%) [8¶/0] | 168 | |
| Total | .. | .. | 197 (45%) | 168 (38%) | 77 (17%) [21/56] | 466 | |
Literature estimates show the range of incubation periods consistent with most published estimates and the most frequently stated central tendency (eg, median, mean) for the incubation period; estimates that did not specify a type (eg, “the incubation period is 5 days”) were assumed to be statements of central tendency.
Observational studies did not always report a defined number of participants, so a subject count is only reported for experimental studies.
Original estimates for severe acute respiratory syndrome (SARS) are based on the same data.
A second experimental study with no observations beyond 5 days is not included.
Many rhinovirus studies report time to maximum symptom score rather than time to any symptom.
Table 2.
Studies included in pooled analysis
| Location | Study type | N | Population | Infection mechanism | Comments | |
|---|---|---|---|---|---|---|
| Adenovirus | ||||||
| Commission on Acute Respiratory Disease (1947)25 | USA | Experimental | 14 | Adult male volunteers | Nasal spray | .. |
| Human coronavirus | ||||||
| Bradburne et al (1967)26 | UK | Experimental | 13 | Adult male and female volunteers | Nasal drops | .. |
| SARS-associated coronavirus | ||||||
| Chan et al (2004)27 | Hong Kong | Observational | 6 | Children and adults | Natural | Outbreak in an extended family |
| Chow et al (2004)28 | Singapore | Observational | 15 | Patients, visitors, and health-care workers | Natural | Hospital outbreak |
| Dwosh et al (2003)6 | Canada | Observational | 14 | Men and women aged 24–80 years | Natural | Hospital outbreak |
| Farewell et al (2005)29 | Hong Kong | Observational | 67 | Male and female | Natural | .. |
| Olsen et al (2003)30 | Airplane | Observational | 23 | Male and female | Natural | Outbreak due to transmission on aircraft |
| Poutanen et al (2003)31 | Canada | Observational | 6 | Men and women aged 24–78 years | Natural | 6 of the first 10 cases of SARS detected in Canada |
| Tsang et al (2003)32 | Hong Kong | Observational | 1 | 49-year-old man | Natural | Hospital outbreak |
| Tang et al (2003)33 | Hong Kong | Observational | 9 | Men and women aged 35–72 years | Natural | .. |
| Wong et al (2004)34 | Hong Kong | Observational | 16 | Male and female medical students | Natural | .. |
| Human metapneumovirus | ||||||
| Ebihara et al (2004)35 | Japan | Observational | 1 | 8-month-old boy | Natural | .. |
| Peiris et al (2003)36 | Hong Kong | Observational | 1 | Child | Natural | .. |
| Influenza A | ||||||
| Alford et al (1966)37 | USA | Experimental | 1 | Adult man (estimated age 21–40 years) | Inhalation | A2/Bethesda strain |
| Burnet and Foley (1940)38 | Australia | Experimental | 3 | Men and women aged 19–41 years | Nasal spray | Reid API strain |
| Couch et al (1971)39 | USA | Experimental | 7 | Men aged 21–40 years | Nasal drops | A2/Hong Kong strain |
| Henle et al (1943)40 | USA | Experimental | 11 | Boys aged 6–14 years | Inhalation | A/F-99 strain |
| Henle et al (1945)41 | USA | Experimental | 61 | Institutionalised boys | Nasal drops | A/PR-8, A/F-99, A/F-12 strains, 24 influenza B in the same study |
| Moser et al (1977)42 | Aeroplane | Observational | 37 | Passengers and crew on an airplane | Natural | A/H3N2 strain |
| Smorodintseff et al (1937)43 | USSR | Experimental | 2 | Male and female | Inhalation | Leningrad or WS strain |
| Influenza B | ||||||
| Francis et al (1944)44 | USA | Experimental | 54 | Male | Nasal spray | B/Lee strain |
| Henle et al (1945)41 | USA | Experimental | 24 | Institutionalised boys | Nasal drops | B/Lee strain, 61 influenza A in the same study |
| Influenza (unknown type) | ||||||
| Armstrong and Hopkins (1921)45 | USA | Observational | 27 | Men and women aged 19–84 years | Natural | Community-based outbreak in 1920 |
| MacDonald and Lyth (1918)46 | UK | Observational | 2 | Male | Natural | Exposure on a train |
| Measles | ||||||
| Goodall (1925)47 | UK | Observational | 4 | Children (male and female) | Natural | Hospital-based infection |
| Goodall (1931)48 | UK | Observational | 25 | .. | Natural | .. |
| Panum (1940)49 | Faroe Islands | Observational | 10 | Adult men | Natural | Ship-based infection in 1847 |
| Perucha et al (2006)50 | Spain | Observational | 3 | Aged 9 months to 32 years | Natural | .. |
| Pickles (1939)51 | UK | Observational | 2 | Male | Natural | .. |
| Stillerman and Thalhimer (1944)52 | USA | Observational | 6 | Aged 11–12 years | Natural | .. |
| Zingher and Mortimer (2005)53 | USA | Observational | 5 | Aged 1–5 years | Natural | Controls in a 1926 study on use of convalescent serum as prophylaxis |
| Simpson (1948)54 | UK | Observational | 1 | 4-year-old girl | Natural | .. |
| Parainfluenza virus | ||||||
| Kapikian et al (1961)55 | USA | Experimental | 9 | Male inmates aged 21–56 years | Throat swab, nasal spray, nasal drops | Type 3 virus |
| Tyrrell et al (1959)56 | UK | Experimental | 2 | Aged 18–45 years | Nasal drops | Type 3K virus |
| Respiratory syncytial virus | ||||||
| Johnson et al (1961)57 | USA | Experimental | 17 | Male inmates aged 21–35 years | Nasal/throat spray, nasal drops | .. |
| Kapikian et al (1961)58 | USA | Observational | 1 | Aged 6–50 months | Natural | .. |
| Sterner et al (1966)59 | Sweden | Observational | 6 | Aged 1–13 months | Natural | .. |
| Rhinovirus | ||||||
| Avila et al (2000)60 | USA | Experimental | 16 | Men and women aged 18–48 years, healthy and with allergies | Nasal challenge | RV-16 |
| Douglas et al (1967)61 | USA | Experimental | 12 | Adult male inmates | Inhalation, nasal drops | .. |
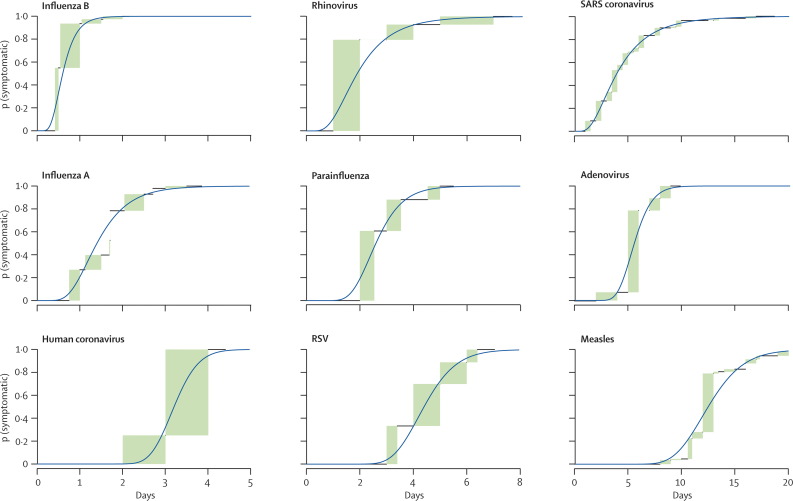
Our estimates of the full distribution of each incubation period using pooled data are shown in figure 2 and table 3 . Visual comparison of the log-normal fitted curves with non-parametric estimates shows high agreement (figure 2). We estimated times by which 5%, 25%, 50%, 75%, and 95% of cases would develop symptoms (table 1). If fewer than 20 observations were available, we did not estimate the 5th or 95th percentiles. No estimate was made for human metapneumovirus due to insufficient data (n=2). Median incubation periods ranged from a half-day (for influenza B) to 12 days (for measles). Dispersions ranged from 1·15 to 1·81, with all but SARS-associated coronavirus and rhinovirus being 1·51 or less, which suggest that, for most respiratory viruses, at least 90% of cases will develop symptoms between half and twice the median incubation period (because e 1·67×log(1·51)≈2).
Figure 2.
Parametric and non-parametric estimates of the incubation period
Cumulative percentage of cases developing symptoms by a given day under the estimates for the log-normal distribution (continuous line) are shown, compared with the non-parametric estimates calculated by the method of Turnbull62 (rectangles). Rectangular regions represent estimates with equivalent support (ie, not statistically distinguishable). RSV=respiratory syncytial virus. SARS=severe acute respiratory syndrome.
Table 3.
Percentiles of the time of symptom onset and dispersion for disease distributions
|
Estimate (95% CI) of time of symptom onset (days)* |
Dispersion (95% CI) | |||||
|---|---|---|---|---|---|---|
| 5th percentile | 25th percentile | 50th percentile (median) | 75th percentile | 95th percentile | ||
| Adenovirus | .. | 4·8 (4·0–5·5) | 5·6 (4·8–6·3) | 6·5 (5·6–7·4) | .. | 1·26 (1·13–1·38) |
| Human coronavirus† | .. | 2·9 (2·5–3·3) | 3·2 (2·8–3·7) | 3·5 (3·1–4·2) | .. | 1·15 (1·07–1·34) |
| SARS-associated coronavirus | 1·5 (1·2–1·7) | 2·7 (2·3–3·0) | 4·0 (3·6–4·4) | 5·9 (5·3–6·6) | 10·6 (8·9–12·2) | 1·81 (1·67–1·95) |
| Influenza A‡ | 0·7 (0·6–0·8) | 1·1 (1·0–1·2) | 1·4 (1·3–1·5) | 1·9 (1·7–2·1) | 2·8 (2·5–3·2) | 1·51 (1·43–1·60) |
| Influenza B | 0·3 (0·2–0·3) | 0·4 (0·4–0·5) | 0·6 (0·5–0·6) | 0·7 (0·7–0·8) | 1·1 (0·9–1·3) | 1·51 (1·37–1·64) |
| Measles | 8·9 (8·1–9·8) | 10·9 (10·2–11·6) | 12·5 (11·8–13·3) | 14·4 (13·5–15·3) | 17·7 (16·1–19·2) | 1·23 (1·18–1·28) |
| Parainfluenza | .. | 2·1 (1·6–2·6) | 2·6 (2·1–3·1) | 3·2 (2·5–3·8) | .. | 1·35 (1·16–1·55) |
| Respiratory syncytial virus | 3·1 (2·5–3·8) | 3·8 (3·3–4·4) | 4·4 (3·9–4·9) | 5·1 (4·5–5·7) | 6·3 (5·2–7·3) | 1·24 (1·13–1·35) |
| Rhinovirus | 0·8 (0·4–1·2) | 1·3 (0·9–1·8) | 1·9 (1·4–2·4) | 2·7 (2–3·4) | 4·5 (2·9–6·2) | 1·68 (1·36–2·01) |
Based on a log-normal distribution of the incubation period; 5th and 95th percentiles are not presented for viruses with fewer than 20 observations.
Bayesian methods were used for the estimation of the human coronavirus incubation period.
The estimate for influenza A includes one experimental study with substantially different results from the rest;41 if this study is excluded, we estimate the 5th, 25th, 50th, 75th and 95th percentiles to be 1·4 (1·2–1·5), 1·7 (1·5–1·8), 1·9 (1·8–2·0), 2·2 (2·1–2·3), and 2·7 (2·4–2·9), respectively, with dispersion of 1·23 (1·17–1·29). SARS=severe acute respiratory syndrome.
Adenovirus
Adenoviruses circulate widely, and most adults show evidence of past exposure.4 Clinical manifestations vary between the 51 serotypes,63 but commonly include cold symptoms, pharyngitis, tonsilitis, otitis media, and pharyngoconjunctival fever. Less common sequelae are severe pneumonia, conjunctivitis, cystitis, encephalitis, and meningitis.12
15 papers stated the incubation period of respiratory disease due to adenovirus. Of 13 articles without original data, none cited an original source. Two original studies were found: an experimental study of adenovirus infection in 1947 reported the incubation period to be 5–6 days,25 and an observational study of secondary infections in families found the mean incubation period to be 10 days.64 Statements varied from a few days to over a week, but most were consistent with an incubation period of 4–8 days (table 1).
Based on 14 observations from a single experimental study,25 we estimate the median incubation period of respiratory illness due to adenovirus to be 5·6 days (95% CI 4·8–6·3), with a dispersion of 1·26 (95% CI 1·13–1·38). 25% of cases will develop symptoms by 4·8 days (95% CI 4·0–5·5), and 75% by 6·5 days (95% CI 5·6–7·4) after infection. Because of limited data, the 5th and 95th percentiles were not estimated.
Coronaviruses
An estimated 10–30% of colds are caused by coronaviruses.4 Coronaviruses usually cause a mild upper respiratory-tract infection, and have been associated with otitis media, asthma exacerbation, and pneumonia.4 In late 2002, a novel virus, SARS-associated coronavirus, emerged in Asia, causing over 8000 cases worldwide. SARS-associated coronavirus differs clinically from other coronaviruses, causing a biphasic illness. In the first phase, myalgia, cough, dyspnoea, fever with diarrhoea and other gastrointestinal symptoms are common. In the second phase, patients develop respiratory distress syndrome, sometimes requiring ventilation and intensive care.12
Human coronaviruses other than SARS
Of nine papers providing an incubation period for human coronavirus, two were based on original data and four were sourced. All sourced estimates cited a 1967 experimental study, which found the incubation period to range from 2 days to 4 days, with a mean of 3·3 days.26 An experimental study by Tyrell and colleagues65 found similar results. Most published estimates for human coronavirus are consistent with an incubation period of 2–5 days (table 1).
Based on 13 observations from one experimental study,26 we estimate the median incubation period of human coronavirus to be 3·2 days (95% CI 2·8–3·7), and the dispersion to be 1·15 (95% CI 1·07–1·34). 25% of cases will develop symptoms by 2·9 days (95% CI 2·5–3·3), and 75% by 3·5 days (95% CI 3·1–4·2) after infection. There were insufficient data to confidently estimate the 5th or 95th percentiles.
SARS-associated coronavirus
We found many studies on the incubation of SARS-associated coronavirus, including a comprehensive review,66 sophisticated statistical analyses,23, 67, 68 and attempts to synthesise available data.7 However, reporting of these results has not been previously standardised.
We found 168 sources with estimates for the incubation period of SARS-associated coronavirus. Public concern and the importance of quarantine for controlling SARS-associated coronavirus contribute to frequent statements of the incubation period.8, 9, 69 Most (n=81) of the published estimates were sourced, with 65 unsourced, and 30 original estimates. The most cited sources are Donnelly and colleagues'67 early analysis of the Hong Kong outbreak, and the consensus estimate published by WHO.7 Most estimates for SARS-associated coronavirus are consistent with an incubation period of 2–10 days (table 1).
Based on 157 observations from nine observational studies,6, 27, 28, 29, 30, 31, 32, 33, 34 we estimate the median incubation period of SARS-associated coronavirus to be 4·0 days (95% CI 3·6–4·4), and the dispersion to be 1·81 (95% CI 1·67–1·95). 5% of SARS-associated coronavirus cases will develop symptoms by 1·5 days (95% CI 1·2–1·7), and 95% by 10·6 days (95% CI 8·9–12·2) after infection.
Influenza
Influenza causes 250 000 to 500 000 deaths worldwide each year.70 Illness often has an abrupt onset and ranges from asymptomatic infection to primary viral pneumonia that progresses to death.3 Symptoms include fever, chills, cough, headache, diffuse myalgia, and upper respiratory-tract infection. Gastrointestinal symptoms are common in children.3
We identified 107 documents that stated an incubation period for influenza. 54 provided no source and 16 were based on original data. The earliest data comes from 1891,71 and the most recent from 2006.72 Most sourced estimates derive from a 1979 observational study by Moser and colleagues,42 in which 37 airline passengers developed influenza after exposure to a single case. All became symptomatic 12–84 h after exposure (median 38 h). In a highly cited 1998 paper, Cox and Fukuda73 summarised these results, codifying the estimate as 1–4 days, with which most estimates for influenza are consistent (table 1). Many original studies of influenza's incubation period remain uncited. Several pre-1918 reports, a series of papers on the 1918 pandemic, and a flurry of experimental studies published in the 1930s and 1940s after discovery of the virus remain underused.
We extracted 85 observations of the incubation period of influenza A from six experimental studies,37, 38, 39, 40, 41, 43 78 observations of the incubation period of influenza B from two experimental studies,41, 44 and 66 observations of the incubation period of influenza A or an unknown strain from three observational studies.42, 45, 46 Unknown strains were presumed to be influenza A due to their occurrence during influenza A pandemics.
We estimate the median incubation period of influenza A to be 1·4 days (95% CI 1·3–1·5), and the dispersion to be 1·51 (95% CI 1·43–1·60). 5% of influenza A cases will develop symptoms by 0·7 days (95% CI 0·6–0·8), and 95% by 2·8 days (95% CI 2·5–3·2) after infection. Incubation period estimates for influenza A were sensitive to a single study with substantially different findings from other studies.41 Excluding this study resulted in a median incubation period of influenza A of 1·9 days (95% CI 1·8–2·0), with dispersion of 1·22 (95% CI 1·17–1·29).
We estimate the median incubation period of influenza B to be 0·6 days (95% CI 0·5–0·6), and the dispersion to be 1·51 (95% CI 1·37–1·64). 5% of influenza B cases will develop symptoms by 0·3 days (95% CI 0·2–0·3), and 95% by 1·1 days (95% CI 0·9–1·3) after infection. Both studies of influenza B define symptom onset as the first instance of fever, potentially shortening the incubation period estimate compared with that seen in clinical practice.
Measles
Globally, measles causes an estimated 500 000 deaths each year in children aged under 5 years.74 The first symptoms include fever, malaise, cough, conjunctivitis, coryza, and Koplik's spots.12 These symptoms are followed by an erythematous maculopapular rash. Complications include otitis media, pneumonia, convulsions, and encephalitis.
Of 52 documents with statements of the measles incubation period, 31 were unsourced, 16 provided a source, and five were based on observational data. The distinctive clinical presentation of measles allowed observations of the incubation period as early as 1847.49 Most estimates for measles are consistent with an incubation period of 8–14 days (table 1). Some of the variability in estimates stems from the use of two clinical definitions of symptom onset: the appearance of rash and the first symptoms of illness. We have excluded those studies that reported just the time to rash, as our interest was the time until first symptoms. However, not all the reports stated the specific symptom used by the authors to mark the end of the incubation period.
Based on 55 observations from eight observational studies,47, 48, 49, 50, 51, 52, 53, 54 we estimate the median incubation period of measles to be 12·5 days (95% CI 11·8–13·2), and the dispersion to be 1·23 (95% CI 1·18–1·28). 5% of measles cases will develop symptoms before 8·9 days (95% CI 8·1–9·8), and 95% by 17·7 days (95% CI 16·1–19·2) after infection.
Metapneumovirus
Human metapneumovirus, first described in 2001, contributes to morbidity and hospital admission in all age-groups.12 Clinically, human metapneumovirus causes illness ranging from upper respiratory-tract symptoms to bronchiolitis and pneumonia requiring ventilation.12 Clinical examination of the lungs is abnormal in a quarter to a third of adults. Febrile seizures are reported in up to 16% of children.75
Little is known about the incubation period of human metapneumovirus. We found only two reported observations of serial transmissions suggesting incubation periods of 5–6 days36 and 4–6 days.35 The incubation period of human metapneumovirus may be similar to that of RSV due to similarities between these viruses.22
Parainfluenza
Parainfluenza viruses cause upper respiratory-tract infection, pneumonia, and bronchiolitis, and are a major cause of croup.12 Initial symptoms include coryza, sore throat, hoarseness, and dry cough.4 Four antigenically distinct serotypes exist, each with characteristic seasonal and age-specific pattern of infection. Most children are infected by multiple serotypes by age 5 years.76
We found 14 documents with statements of the incubation period for parainfluenza that provided six original estimates, four sourced estimates, and six unsourced estimates. Four experimental and two observational studies include one exceptional observation (not included in the pooled analysis) of respiratory illness with virological evidence of parainfluenza infection, with an incubation period of 10–29 weeks.77 These cases occurred during a period of winter isolation of Antarctic researchers, and may indicate sustained asymptomatic transmission or the ability of the virus to viably persist in exceptionally cold conditions. Most estimates for parainfluenza are consistent with an incubation period of 2–6 days (table 1).
Based on 11 observations from two experimental studies,55, 56 we estimate the median incubation period for parainfluenza to be 2·6 days (95% CI 2·1–3·1), with a dispersion of 1·35 (95% CI 1·16–1·55). 25% of cases develop symptoms by 2·1 days (95% CI 1·6–2·6), and 75% by 3·2 days (95% CI 2·5–3·8) after infection. There were insufficient data to confidently estimate the 5th or 95th percentiles.
Respiratory syncytial virus
RSV is an important cause of morbidity among children and mortality among elderly and immunocompromised people. Prospective studies have found that 40% of all lower respiratory-tract infections in the first year of life involve RSV.22 RSV usually causes a upper respiratory-tract infection and is then cleared, but in 25–40% of cases, infection progresses to the lower respiratory tract, often manifesting as pneumonia or bronchiolitis.3
In 40 documents with statements of the incubation period of RSV, 20 (48%) estimates were unsourced, 16 (38%) were sourced, and six (14%) were based on original data. Two estimates based on original data refer to the same experimental study.57, 78 This study and three observational studies make up the data supporting most statements of the incubation period.58, 59, 79 Most estimates for RSV are consistent with an incubation period of 3–7 days (table 1).
Based on 17 observations from one experimental study,57 and seven observations from two observational studies,58, 59 we estimate the median incubation period of RSV to be 4·4 days (95% CI 3·9–4·9), with a dispersion of 1·24 (95% CI 1·13–1·35). 5% of cases will develop symptoms before 3·1 days (95% CI 2·5–3·8), and 95% by 6·3 days (95% CI 5·2–7·3) after infection.
Rhinovirus
Rhinovirus causes an estimated 50% of colds. Symptoms include rhinorrhoea, nasal congestion, headache, sore throat, and cough.4 Complications include sinusitis, otitis media, and exacerbation of asthma or chronic obstructive pulmonary disease.3
We found 15 articles on the incubation period of rhinovirus. There were twice as many original (eight) as sourced (four) or unsourced (four) estimates. Low estimates of the incubation period are less than half a day.3, 80, 81 Many experimental studies of rhinovirus infection report the time to peak mean symptom score of participants as a measure of the incubation period.82, 83 This method may bias estimates of the incubation period to be longer, because the time of most severe symptoms will usually follow the time of first symptoms. Most estimates are consistent with an incubation period of 2–4 days (table 1).
Based on 28 observations from two experimental studies,60, 61 we estimate the median incubation period of rhinovirus to be 1·9 days (95% CI 1·4–2·4), and the dispersion to be 1·68 (95% CI 1·36–2·01). 5% of cases will develop symptoms by 0·8 days (95% CI 0·4–1·2), and 95% by 4·5 days (95% CI 2·9–6·2) after infection.
Discussion
Of the 82% of incubation period estimates not based on original data, most were given without citation. This suggests that the incubation period for many diseases may be considered common knowledge in the medical community. However, our Review found that the evidence supporting the reported incubation period was minimal for many diseases. For some diseases (eg, influenza) estimates and data produced using sound methods exist, although they are rarely referenced.
Several sources of uncertainty exist in the measuring of incubation period. Estimates depend on the time of infection, which cannot be observed directly. The time of exposure bounds the time of infection, but is rarely available. Observational studies may not include all infected cases, thus the methods by which cases are identified are themselves a potential source of bias. Experimental infection and natural experiments (eg, aeroplane infections)42 may differ from normal exposure in ways that affect the incubation period. Routes of administration, changes in infectious dose, or differing periods of exposure to infectious individuals may modify the time to symptom onset. Most experimental studies use healthy adult volunteers, yet severe disease is concentrated in children and the elderly. Variation between studies in the definition of symptom onset and inclusion criteria may thus affect our estimates. Precise guidelines on the start of the symptomatic period for each disease would remove some of this variation.
Despite potential sources of between-study variation, when we checked our pooled analysis against a hierarchical model we found nearly identical estimates for the median and dispersion of most diseases. For those that were shifted (influenza A and B), estimates of the median, 5th, and 95th percentiles were no more than a third of a day longer. This suggests that study effects may be less than one would assume; however, the small number of studies, and their relatively small size, leave open the possibility that factors specific to the included studies may have affected our results.
The results presented here are limited by our review's focus on published data. For some diseases (adenovirus, human coronavirus, influenza B, parainfluenza, and rhinovirus) estimates are still based on one or two studies and fewer than 100 observations. This necessarily leaves uncertainty in our results, and perhaps bias if these studies were atypical. We found eight instances (excluding SARS, for which there is ample evidence) in which a study that might contain data on the incubation period was done but the information necessary to estimate the incubation period was not published. These studies were mostly done over 30 years ago, and we felt it unlikely that the original data could be easily obtained. A motivated researcher who could obtain this or other unpublished data would add much to our results. More data is clearly needed if we are to understand how factors such as virus morphology, host status, climate, and infectious dose influence the incubation period.
We have combined published empirical data to provide estimates of the incubation period for nine important respiratory viruses. Previously published estimates generally only provide estimates of the centre of the incubation period distribution. However, the aspect of the distribution that is of interest varies by application: the right tail (eg, 95th percentile) is important in bounding the time of symptom onset for quarantine, the central region (eg, 25th to 75th percentiles) helps to identify the most likely time and source of infection, and the full distribution informs models for use in pandemic planning. Our comprehensive systematic review pools published data to characterise the entire incubation period distribution including the left and right tails, which makes the incubation period more useful in research, clinical practice, and public-health policy.
Search strategy and selection criteria
These are described in detail in the Methods section.
Acknowledgments
Acknowledgments
DATC's work on this project was funded by a grant from the NIH (U01-GM070708) and he holds a Career Award at the Scientific Interface from the Burroughs Welcome Fund. JL, NGR, and RB were funded by a grant from the US Department of Homeland Security (N00014-06-1-0991). TP was funded by a grant from the US Centers for Disease Control (HK00014). We thank Daniel Landau of postalmodern.com, USA, for freely providing and maintaining a library and version control system, and Jennifer Anderson, of the Carnegie Institution of Washington, USA, for her editorial assistance.
Conflicts of interest
We declare that we have no conflicts of interest.
Web Extra Material
References
- 1.Graham NM. The epidemiology of acute respiratory infections in children and adults: a global perspective. Epidemiol Rev. 1990;12:149–178. doi: 10.1093/oxfordjournals.epirev.a036050. [DOI] [PubMed] [Google Scholar]
- 2.WHO . The world health report 2004—changing history. World Health Organization; Geneva: 2004. [Google Scholar]
- 3.Mandell GL, Dolin R, Bennett JE. Principles and practice of infectious disease. Elsevier/Churchill Livingstone; New York: 2005. [Google Scholar]
- 4.Cohen J, Powderly WG. Infectious diseases. 2nd edn. Mosby; New York: 2004. [Google Scholar]
- 5.Nelson KE, Williams CM. Infectious disease epidemiology, theory and practice. Jones & Bartlett Publishers; Sudbury, MA: 2006. [Google Scholar]
- 6.Dwosh HA, Hong HHL, Austgarden D, Herman S, Schabas R. Identification and containment of an outbreak of SARS in a community hospital. CMAJ. 2003;168:1415–1420. [PMC free article] [PubMed] [Google Scholar]
- 7.WHO Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). May, 2003 [WHO/CDS/CSR/GAR/2003.11] http://www.who.int/csr/sars/en/WHOconsensus.pdf (accessed Feb 20, 2009).
- 8.Twu SJ, Chen TJ, Chen CJ. Control measures for severe acute respiratory syndrome (SARS) in Taiwan. Emerg Infect Dis. 2003;9:718–720. doi: 10.3201/eid0906.030283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention . Public health guidance for community-level preparedness and response to severe acute respiratory syndrome (SARS) Centers for Disease Control and Prevention; Atlanta: 2005. [Google Scholar]
- 10.Lessler J, Brookmeyer R, Perl TM. An evaluation of classification rules based on date of symptom onset to identify health-care associated infections. Am J Epidemiol. 2007;166:1220–1229. doi: 10.1093/aje/kwm188. [DOI] [PubMed] [Google Scholar]
- 11.Karanfil LV, Conlon M, Lykens K. Reducing the rate of nosocomially transmitted respiratory syncytial virus. Am J Infect Control. 1999;27:91–96. doi: 10.1016/s0196-6553(99)70087-8. [DOI] [PubMed] [Google Scholar]
- 12.Pickering LK. Red book: 2006 report of the Committee on Infectious Diseases. American Academy of Pediatrics; Elk Grove Village, IL: 2006. [Google Scholar]
- 13.Ahrens W, Pigeot I, editors. Handbook of epidemiology. Springer-Verlag; Berlin: 2005. [Google Scholar]
- 14.Ferguson NM, Cummings DAT, Cauchemez S. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437:209–214. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- 15.Longini IM, Nizam A, Xu S. Containing pandemic influenza at the source. Science. 2005;309:1083–1087. doi: 10.1126/science.1115717. [DOI] [PubMed] [Google Scholar]
- 16.Fraser C, Riley S, Anderson R, Ferguson NM. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci USA. 2004;101:6146–6151. doi: 10.1073/pnas.0307506101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feigin RD. Textbook of pediatric infectious disease. 5th edn. Saunders; Philadelphia: 2004. [Google Scholar]
- 18.Rothman KJ. Induction and latent periods. Am J Epidemiol. 1981;114:253–259. doi: 10.1093/oxfordjournals.aje.a113189. [DOI] [PubMed] [Google Scholar]
- 19.Sartwell PE. The distribution of incubation periods of infectious disease. Am J Hyg. 1950;51:310–318. doi: 10.1093/oxfordjournals.aje.a119397. [DOI] [PubMed] [Google Scholar]
- 20.Armenian HK, Lilienfeld AM. Incubation period of disease. Epidemiol Rev. 1983;5:1–15. doi: 10.1093/oxfordjournals.epirev.a036254. [DOI] [PubMed] [Google Scholar]
- 21.Heymann DL, editor. Control of communicable diseases manual. 18th edn. American Public Health Association; Washington, DC: 2004. [Google Scholar]
- 22.Howley PM, Knipe DM, Fields BN, editors. Field's virology. 5th edn. Lippincott Williams & Wilkins; Philadelphia: 2007. [Google Scholar]
- 23.Cowling BJ, Muller MP, Wong IOL. Alternative methods of estimating an incubation distribution: examples from severe acute respiratory syndrome. Epidemiology. 2007;18:253–259. doi: 10.1097/01.ede.0000254660.07942.fb. [DOI] [PubMed] [Google Scholar]
- 24.Rice JA. Mathematical statistics and data analysis. 2nd edn. Duxbury Press; Belmont, CA: 1995. [Google Scholar]
- 25.Commission on Acute Respiratory Disease Experimental transmission of minor respiratory illness to human volunteers by filter-passing agents. I. Demonstration of two types of illness characterized by long and short incubation periods and different clinical features. J Clin Invest. 1947;26:957–982. doi: 10.1172/JCI101891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bradburne AF, Bynoe ML, Tyrrell DA. Effects of a “new” human respiratory virus in volunteers. Br Med J. 1967;3:767–769. doi: 10.1136/bmj.3.5568.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan WM, Kwan YW, Wan HS, Leung CW, Chiu MC. Epidemiologic linkage and public health implication of a cluster of severe acute respiratory syndrome in an extended family. Pediatr Infect Dis J. 2004;23:1156–1159. [PubMed] [Google Scholar]
- 28.Chow KY, Lee CE, Ling ML, Heng DMK, Yap SG. Outbreak of severe acute respiratory syndrome in a tertiary hospital in Singapore, linked to an index patient with atypical presentation: epidemiological study. BMJ. 2004;328:195. doi: 10.1136/bmj.37939.465729.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farewell VT, Herzberg AM, James KW, Ho LM, Leung GM. SARS incubation and quarantine times: when is an exposed individual known to be disease free? Stat Med. 2005;24:3431–3445. doi: 10.1002/sim.2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Olsen SJ, Chang HL, Cheung TYY. Transmission of the severe acute respiratory syndrome on aircraft. N Engl J Med. 2003;349:2416–2422. doi: 10.1056/NEJMoa031349. [DOI] [PubMed] [Google Scholar]
- 31.Poutanen SM, Low DE, Henry B. Identification of severe acute respiratory syndrome in Canada. N Engl J Med. 2003;348:1995–2005. doi: 10.1056/NEJMoa030634. [DOI] [PubMed] [Google Scholar]
- 32.Tsang KW, Ho PL, Ooi GC. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1977–1985. doi: 10.1056/NEJMoa030666. [DOI] [PubMed] [Google Scholar]
- 33.Tang HL, Cheuk A, Chu KH. Severe acute respiratory syndrome in haemodialysis patients: a report of two cases. Nephrol Dial Transplant. 2003;18:2178–2181. doi: 10.1093/ndt/gfg454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wong TW, Lee CK, Tam W. Cluster of SARS among medical students exposed to single patient, Hong Kong. Emerg Infect Dis. 2004;10:269–276. doi: 10.3201/eid1002.030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ebihara T, Endo R, Kikuta H. Human metapneumovirus infection in Japanese children. J Clin Microbiol. 2004;42:126–132. doi: 10.1128/JCM.42.1.126-132.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peiris JSM, Tang WH, Chan KH. Children with respiratory disease associated with metapneumovirus in Hong Kong. Emerg Infect Dis. 2003;9:628–633. doi: 10.3201/eid0906.030009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alford RH, Kasel JA, Gerone PJ, Knight V. Human influenza resulting from aerosol inhalation. Proc Soc Exp Biol Med. 1966;122:800–804. doi: 10.3181/00379727-122-31255. [DOI] [PubMed] [Google Scholar]
- 38.Burnet FM, Foley M. The results of intranasal inoculation of modified and unmodified influenza virus strains in human volunteers. Med J Aust. 1940;2:655–659. [Google Scholar]
- 39.Couch RB, Douglas RG, Fedson DS, Kasel JA. Correlated studies of a recombinant influenza-virus vaccine. 3. Protection against experimental influenza in man. J Infect Dis. 1971;124:473–480. doi: 10.1093/infdis/124.5.473. [DOI] [PubMed] [Google Scholar]
- 40.Henle W, Henle G, Stokes J., Jr. Demonstration of the efficacy of vaccination against influenza type a by experimental infection of human beings. J Immunol. 1943;46:163–175. [Google Scholar]
- 41.Henle W, Henle G, Stokes J, Jr, Maris EP. Experimental exposure of human subjects to viruses of influenza. J Immunol. 1945;52:145–165. [PubMed] [Google Scholar]
- 42.Moser MR, Bender TR, Margolis HS, Noble GR, Kendal AP, Ritter DG. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol. 1979;110:1–6. doi: 10.1093/oxfordjournals.aje.a112781. [DOI] [PubMed] [Google Scholar]
- 43.Smorodintseff A, Tushinsky A, Korovin A. Investigation of volunteers with the influenza virus. Am J Med Sci. 1937;194:159–170. [Google Scholar]
- 44.Francis T, Pearson HE, Salk JE, Brown PN. Immunity in human subjects artificially infected with influenza virus, type B. Am J Public Health Nations Health. 1944;34:317–334. doi: 10.2105/ajph.34.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Armstrong C, Hopkins R. An epidemiologic study of the 1920 epidemic of influenza in an isolated rural community. Public Health Rep. 1921;36:1671–1702. [Google Scholar]
- 46.MacDonald P, Lyth JC. Incubation period of influenza. BMJ. 1918;2:488. doi: 10.1136/bmj.2.3018.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goodall EW. Measles with an illness at infection. Clin J. 1925;54:69. [Google Scholar]
- 48.Goodall EW. Incubation period of measles. BMJ. 1931;1:73–74. [Google Scholar]
- 49.Panum PL. Observations made during the epidemic of measles on the Faroe Islands in the year 1846. Delta Omega Society; New York: 1940. [Google Scholar]
- 50.Perucha M, Ramalle-Gómara E, Lezaun ME. A measles outbreak in children under 15 months of age in La Rioja, Spain, 2005–2006. Eur Surveill. 2006;11:267–270. [PubMed] [Google Scholar]
- 51.Pickles W. Epidemiology in country practice. Williams and Wilkins; Baltimore: 1939. [Google Scholar]
- 52.Stillerman M, Thalhimer W. Attack rate and incubation period of measles—significance of age and of conditions of exposure. Am J Dis Child. 1944;67:15–21. [Google Scholar]
- 53.Zingher A, Mortimer P. Convalescent whole blood, plasma and serum in the prophylaxis of measles: JAMA, 12 April, 1926; 1180–1187. Rev Med Virol. 2005;15:407–421. doi: 10.1002/rmv.480. [DOI] [PubMed] [Google Scholar]
- 54.Simpson REH. The period of transmission in certain epidemic diseases—an observational method for its discovery. Lancet. 1948;255:755–760. doi: 10.1016/s0140-6736(48)91328-2. [DOI] [PubMed] [Google Scholar]
- 55.Kapikian AZ, Chanock RM, Reichelderfer TE, Ward TG, Huebner RJ, Bell JA. Inoculation of human volunteers with parainfluenza virus type 3. JAMA. 1961;178:537–541. doi: 10.1001/jama.1961.03040450001001. [DOI] [PubMed] [Google Scholar]
- 56.Tyrrell DA, Bynoe ML, Petersen KB, Sutton RN, Pereira MS. Inoculation of human volunteers with parainfluenza viruses types 1 and 3 (HA 2 and HA 1) BMJ. 1959;2:909–911. doi: 10.1136/bmj.2.5157.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Johnson KM, Chanock RM, Rifkind D, Kravetz HM, Knight V. Respiratory syncytial virus. IV. Correlation of virus shedding, serologic response, and illness in adult volunteers. JAMA. 1961;176:663–667. [PubMed] [Google Scholar]
- 58.Kapikian AZ, Bell JA, Mastrota FM, Johnson KM, Huebner RJ, Chanock RM. An outbreak of febrile illness and pneumonia associated with respiratory syncytial virus infection. Am J Hyg. 1961;74:234–248. doi: 10.1093/oxfordjournals.aje.a120216. [DOI] [PubMed] [Google Scholar]
- 59.Sterner G, Wolontis S, Bloth B, de Hevesy G. Respiratory syncytial virus. An outbreak of acute respiratory illnesses in a home for infants. Acta Paediatr Scand. 1966;55:273–279. doi: 10.1111/j.1651-2227.1966.tb17654.x. [DOI] [PubMed] [Google Scholar]
- 60.Avila PC, Abisheganaden JA, Wong H. Effects of allergic inflammation of the nasal mucosa on the severity of rhinovirus 16 cold. J Allergy Clin Immunol. 2000;105:923–932. doi: 10.1067/mai.2000.106214. [DOI] [PubMed] [Google Scholar]
- 61.Douglas RG, Rossen RD, Butler WT, Couch RB. Rhinovirus neutralizing antibody in tears, parotid saliva, nasal secretions and serum. J Immunol. 1967;99:297–303. [PubMed] [Google Scholar]
- 62.Turnbull BW. The empirical distribution function with arbitrarily grouped, censored and truncated data. J R Stat Soc B. 1976;38:290–295. [Google Scholar]
- 63.Shinozaki T, Fujita Y, Araki K, Tajima T, Kobayashi M, Abe T. Clinical features of enteric adenovirus infection in infants. Acta Paediatr Jpn. 1991;33:623–627. doi: 10.1111/j.1442-200x.1991.tb01875.x. [DOI] [PubMed] [Google Scholar]
- 64.Ruuskanen O, Mertsola J, Meurman O. Adenovirus infection in families. Arch Dis Child. 1988;63:1250–1253. doi: 10.1136/adc.63.10.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tyrrell DA, Cohen S, Schlarb JE. Signs and symptoms in common colds. Epidemiol Infect. 1993;111:143–156. doi: 10.1017/s0950268800056764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Donnelly CA, Fisher MC, Fraser C. Epidemiological and genetic analysis of severe acute respiratory syndrome. Lancet Infect Dis. 2004;4:672–683. doi: 10.1016/S1473-3099(04)01173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Donnelly CA, Ghani AC, Leung GM. Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet. 2003;361:1761–1766. doi: 10.1016/S0140-6736(03)13410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention Severe acute respiratory syndrome—Singapore, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:405–411. [PubMed] [Google Scholar]
- 69.Svoboda T, Henry B, Shulman L. Public health measures to control the spread of the severe acute respiratory syndrome during the outbreak in Toronto. N Engl J Med. 2004;350:2352–2361. doi: 10.1056/NEJMoa032111. [DOI] [PubMed] [Google Scholar]
- 70.WHO Influenza (fact sheet no. 211) March, 2003. http://www.who.int/mediacentre/factsheets/fs211/en/ (accessed Feb 20, 2009).
- 71.Parsons H. Report on the influenza epidemic of 1889–90. Local Government Board, HMSO; London: 1891. [Google Scholar]
- 72.Oner AF, Bay A, Arslan S. Avian influenza A (H5N1) infection in eastern Turkey in 2006. N Engl J Med. 2006;355:2179–2185. doi: 10.1056/NEJMoa060601. [DOI] [PubMed] [Google Scholar]
- 73.Cox NJ, Fukuda K. Influenza. Infect Dis Clin North Am. 1998;12:27–38. doi: 10.1016/s0891-5520(05)70406-2. [DOI] [PubMed] [Google Scholar]
- 74.WHO Progress in reducing global measles deaths: 1999–2003. Wkly Epidemiol Rec. 2005;80:78–81. [PubMed] [Google Scholar]
- 75.Falsey AR, Erdman D, Anderson LJ, Walsh EE. Human metapneumovirus infections in young and elderly adults. J Infect Dis. 2003;187:785–790. doi: 10.1086/367901. [DOI] [PubMed] [Google Scholar]
- 76.Henrickson KJ, Kuhn SM, Savatski LL. Epidemiology and cost of infection with human parainfluenza virus types 1 and 2 in young children. Clin Infect Dis. 1994;18:770–779. doi: 10.1093/clinids/18.5.770. [DOI] [PubMed] [Google Scholar]
- 77.Muchmore HG, Parkinson AJ, Humphries JE. Persistent parainfluenza virus shedding during isolation at the South Pole. Nature. 1981;289:187–189. doi: 10.1038/289187a0. [DOI] [PubMed] [Google Scholar]
- 78.Kravetz HM, Knight V, Chanock RM. Respiratory syncytial virus. III. Production of illness and clinical observations in adult volunteers. JAMA. 1961;176:657–663. [PubMed] [Google Scholar]
- 79.Lee CY, Funk GA, Chen ST, Huang YT, Wei HY. An outbreak of respiratory syncytial virus infection in an infant nursery. Taiwan Yi Xue Hui Za Zhi. 1973;72:39–46. [PubMed] [Google Scholar]
- 80.Harris JM, Gwaltney JM. Incubation periods of experimental rhinovirus infection and illness. Clin Infect Dis. 1996;23:1287–1290. doi: 10.1093/clinids/23.6.1287. [DOI] [PubMed] [Google Scholar]
- 81.Blomqvist S. Epidemiology of human rhinoviruses [dissertation]. Faculty of Biosciences, University of Helsinki. November, 2004. http://ethesis.helsinki.fi/julkaisut/bio/bioja/vk/blomqvist/epidemio.pdf (accessed Feb 20, 2009).
- 82.Douglas RG, Cate TR, Gerone PJ, Couch RB. Quantitative rhinovirus shedding patterns in volunteers. Am Rev Respir Dis. 1966;94:159–167. doi: 10.1164/arrd.1966.94.2.159. [DOI] [PubMed] [Google Scholar]
- 83.Tyrrell DA, Cohen S, Schlarb JE. Signs and symptoms in common colds. Epidemiol Infect. 1993;111:143–156. doi: 10.1017/s0950268800056764. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.