Abstract
Objectives
To utilize novel methods to examine age-associations across an integrated brain network in healthy older adults (HOA) and individuals with late-life depression (LLD). Graph theory metrics describe the organizational configuration of both the global network and specified brain regions.
Design
Cross-sectional data were acquired. Graph theory was used to explore diffusion tensor imaging derived white matter networks.
Participants
48 HOA and 28 adults with LLD were recruited from the community.
Measurements
Global and local metrics in prefrontal, cingulate and temporal regions were calculated. Group differences and associations with age were explored.
Results
Group differences were noted in local metrics of the right prefrontal and temporal regions, no significant differences were observed on global metrics. Local (not global) metrics were associated with age differently across groups. For HOA, local metrics across all regions correlated with age whereas in LLD correlations were only observed within temporal regions. In keeping with hypothesized regions impacted by LLD, stronger hubs in right temporal regions were observed among HOA whereas LLD individuals were characterized by robust hubs in frontal regions.
Conclusion
We demonstrate widespread age-related changes in local network properties among HOA with different and more restricted local changes in LLD. Although a preliminary analysis, different patterns of correlations in local networks coupled with equivalent global metrics may reflect altered local structural brain networks in patients with LLD.
Keywords: Late-life depression, Graph theory, Network analysis, Diffusion tensor imaging, Age effects
Objective
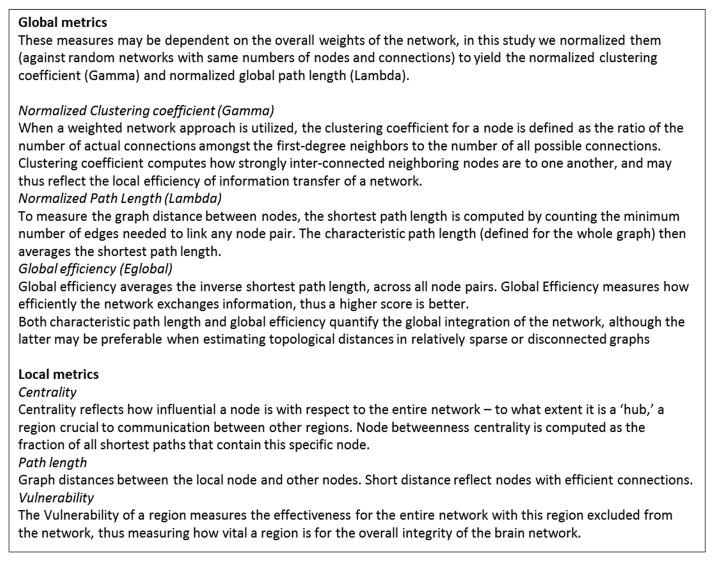
Healthy aging and late life depression (LLD) are associated with significant changes in the brain in both gray and white matter1-5. Studies have explored individual brain regions and specific white matter tracts, however few studies have utilized novel magnetic resonance imaging (MRI) analysis methods that incorporate graph theory. Graph theory enables examination of the whole brain's organizational properties by modeling it as an integrated network6, 7. In graph theory, a network is a set of nodes with connections (edges) between them. Various metrics have been proposed (see Rubinov & Sporns for a detailed review7) and it has been suggested that an optimized network can be described as a “small-world-network”, having high network efficiency and short path lengths6, 8. Thus, in a well-organized network such as the human brain one may identify a number of regions as hubs, i.e. regions that are highly connected internally but also with long range connections externally to other regions or hubs. Effective networks will be formed by a complex combination of efficiency and strength of connections both between and within brain regions; too many connections may be just as detrimental to a network as too few (see Figure 1 for description of metrics used in this study).
Figure 1.
Description of graph theory metrics.
To date, brain imaging studies applying graph theory across the lifespan, have not provided consistent results and as yet, little work has been done to integrate findings into a cohesive theory. For example, in a graph analysis of gray matter volume across the lifespan, Wu and colleagues9 demonstrated that the gray matter network became more widely distributed from young adulthood through middle-age, and then became more localized in old-age. The authors describe this U-shaped curve as representing the development of a mature system followed by the randomization of that system as age-related decline impacts the brain. Although this description maps well onto the development and decline of brain networks, it does not reflect the pattern of cognitive changes observed across the lifespan, where optimal performance is generally observed in early adulthood. Some graph analyses have demonstrated less efficient global and local networks among older versus younger adults for both gray matter volume10 and white matter based on diffusion tensor imaging (DTI) whole brain tractography11. In contrast another structural connectivity study using DTI identified equivalent global efficiency but reduced local efficiency12. The authors suggest that this preserved global but decreased local efficiency may represent adaptation toward the use of alternative networks among older adults12. Despite these initial analyses of normal aging, little work has been done to understand how measures of network integrity may be impacted by current illness such as depression in aging.
A recent white matter graph study of remitted late-onset LLD identified reduced global efficiency and increased path length suggesting less efficient networks in recovered patients compared to healthy adults13. An earlier study from our group examining gray matter volume inter-correlations (rather than a white matter brain network as described in the current analysis), identified a similar pattern of lower global efficiency and higher global path length in LLD compared to a comparison group, as well as a higher global clustering coefficient in LLD14. Unfortunately the available methods precluded investigating individual differences. This study will expand on these structural network findings and examine individual differences in graph theory metrics not only as they relate to LLD and healthy older adults (HOA), but also how age may impact these findings. Here we use DTI whole brain tractography-derived white matter structural networks to examine group differences between LLD patients and HOA, associations with age are also examined. We focus on regions of interest in frontal, temporal and cingulate cortices as previous studies of the role of white matter underlying LLD and mood regulation have implicated white matter in these areas15-19. In addition, white matter tracts such as the uncinate fasciculus connecting frontal and temporal regions and the cingulum, the white matter tract that underlies the cingulate cortex, have demonstrated lower microstructural integrity in LLD compared to HOA3, 15, 20, 21. We hypothesize that there will be lower network Efficiency, longer Path Length, less Centrality and greater Vulnerability in patients with LLD compared to HOA in regions important for mood regulation or commonly affected in major depressive disorder, such as the prefrontal and cingulate cortex and the temporal lobes1, 19, 22-24 Furthermore we hypothesize that network efficiency will reduce with increasing age.
Methods
Participants and Procedures
Data were collected as part of a larger research study investigating LLD at the University of Illinois at Chicago (UIC). Individuals age 60 and older were recruited via community outreach (e.g., newspaper, radio, and television advertisements) and relevant outpatient clinics within the School of Medicine (e.g., mood and anxiety, geriatrics). The study was approved by the UIC Institutional Review Board and conducted in accordance with the Declaration of Helsinki.
Participants underwent a preliminary telephone screen. Exclusion criteria consisted of current or past history of brain disorders (i.e., dementia, stroke, seizure, head injury, loss of consciousness, etc.), history of substance abuse or dependence, an Axis I psychiatric disorder diagnosis (other than major depression for the LLD group), psychotropic medication use including antidepressant medications and the presence of metallic implant(s) that would preclude MRI. Thus, all study participants, including those diagnosed with major depression were free of any antidepressant medication for at least two weeks in order to study depressed mood in an untreated state.
After passing the telephone screen, participants were scheduled for a more detailed evaluation including cognitive, i.e., Mini-Mental State Examination (MMSE25 and affective, i.e., Structured Clinical Interview for DSM-IV (SCID26 screens for final inclusion/exclusion determination. Screening measures were administered by a trained research assistant, followed by an evaluation by a board certified (AK) or board eligible (OA) psychiatrist who completed the Hamilton Depression Rating Scale (HDRS27. All raters were blind to telephone screen information. Informed consent was obtained from all participants. After eligibility was confirmed, qualified participants were scheduled for a second visit during which they completed a neuropsychological assessment (not reported). A third visit involved MRI acquisition.
Final inclusion criteria for adults with LLD included a diagnosis of major depressive disorder based on the SCID and a score ≥15 on the 17-item HDRS. Healthy older adults (HOA) participants required an absence of depressive symptoms based on the SCID and a score ≤8 on the HDRS. All participants regardless of group, had an MMSE score ≥ 24, had scores within the normal range on the standardized neuropsychological assessment, and were native English speakers. The HOA group demonstrated no history of neurological or psychiatric illness, and no evidence of cognitive deficits on standardized neuropsychological assessments (not reported here). History of stable (e.g., diabetes, hypertension) or remitted medical illness (e.g., cancer) was not an exclusionary factor.
One hundred and forty-four individuals attended initial screening. Thirty-four individuals were excluded from analysis: 15 had past substance abuse or dependence (HOA=4, LLD=11); five had English as a second language (HOA=4, LLD=1); three were on contra-indicative medication (HOA=1, LLD=2); five had contra-indicative comorbidities (HOA=1, LLD=4); four individuals had sleep apnea (HOA=3, LLD=1), two had previous head trauma (HOA=1, LLD=1). Of these 110 individuals, 76 had complete imaging data available (T1-weighted and DTI); the final sample included 28 adults with LLD and 48 HOA. Note, there is substantial overlap with the sample of participants described by a previous analysis of gray matter network14.
Neuroimaging Protocol
Brain MRI were acquired on a Philips 3.0T Achieva scanner (Philips Medical Systems, Best, The Netherlands) using an 8-channel SENSE (Sensitivity Encoding) head coil. Participants were positioned comfortably on the scanner bed and fitted with soft ear plugs; foam pads were used to minimize head movement. Participants were instructed to remain still throughout the scan. High resolution three-dimensional T1-weighted images were acquired with a MPRAGE (Magnetization Prepared Rapid Acquisition Gradient Echo) sequence (field of view: FOV=240mm; 134 contiguous axial slices; TR/TE= 8.4/3.9ms; flip angle=8°; voxel size=1.1X1.1X1.1mm). DTI images were acquired using single-shot spin-echo echo-planar imaging (EPI) sequence (FOV=240mm; voxel size=0.83X0.83X2.2mm; TR/TE=6,994/71ms; Flip angle=90o). Sixty seven contiguous axial slices aligned to the anterior commissure–posterior commissure (AC-PC) line were collected in 32 gradient directions with b=700s/mm2 and one acquisition without diffusion sensitization (B0 image). Parallel imaging technique was utilized with factor at 2.5 to reduce scanning time to approximately 4 minutes. The acquisition of these images was part of a larger protocol.
Image Analysis
To generate brain network data, a pipeline was constructed which integrates multiple image analysis techniques. Diffusion weighted images were eddy current corrected using the automatic image registration tool in DTI-Studio (http://www.mristudio.org28) by registering all diffusion-weighted images to their corresponding b0 images. An eddy current correction technique using affine transformation was performed (rotation, translation, scaling and shear, 12-parameters). This was followed by the computation of diffusion tensors then deterministic tractography using Fiber Assignment by Continuous Tracking (FACT) algorithm built into the DTI-Studio program. For each subject, tractography was first performed by tracking the whole brain, initiating tracts at each voxel. Fiber tracking was stopped when FA value falls below 0.15 or a turning angle becomes larger than 60°.
T1-weighted images were used to generate label maps using the FreeSurfer image analysis suite (http://surfer.nmr.mgh.harvard.edu/) for volumetric segmentation29-31. Each label map is composed of 87 different gray matter regions of interest (ROIs), which include cortical and subcortical regions as well as the brainstem and cerebellum.
Brain gray matter structural networks were generated by counting the number of reconstructed streamlines connecting every pair of gray matter ROIs (i.e. the “nodes”). We investigated several hubs of interest, which are areas hypothesized to be important for mood regulation or are often affected in LLD1, 19, 22-24. To this end, hubs of interest were constructed by combining individual FreeSurfer areas of interest as follows: prefrontal cortex (PFC) – orbitofrontal cortex, inferior frontal gyrus and rostral division of the middle frontal gyrus; cingulate cortex – rostral anterior, caudal anterior and posterior divisions; temporal – entorhinal cortex, parahippocampal gyrus and middle temporal gyrus. Regions were combined in order to investigate the integral role of these hubs of interest with their sub-components combined, and to reduce the number of comparisons. The resulting matrices were then analyzed using a set of Matlab-based functions implemented in the Brain Connectivity Toolbox (http://brain-connectivity-toolbox.net/) to yield several graph theory metrics. In order to minimize multiple comparisons metrics were carefully selected to represent the network at both the global and local level, as well as describing how important a region is for the network as a whole and the connections between regions, see Figure 1. Global measures are reported for the normalized clustering coefficient (Gamma), normalized path length (Lambda) and global efficiency (Eglobal). Local measures reported are Centrality, Path Length and Vulnerability.
Statistical Analyses
All statistical analyses were performed in SPSS (PASW, version 18.0.SPSS, Chicago, IL). Group differences in both demographics and network metrics were examined using ANOVA and Chi-Squared, as appropriate. ANCOVA was used to examine group differences in global and local graph theory metrics, with age and sex included as covariates. Partial correlations were performed to explore associations between age and graph theory metrics controlling for sex, for each group separately. For the local metric analyses, false discovery rate (FDR; q<0.30 for false discovery rate bounds32, 33) was used to control for type I error rate for multiple comparisons.
Results
Demographics
There were no significant differences between the groups in either highest education level (LLD: mean=15.18 (3.29); HOA: mean=14.90 (2.90); F(1,74)=1.41, p=.698) or sex (LLD: males=28.6%; HOA: males=37.5%; X2=.626, p=.429). The HOA group were significantly older than the LLD group (LLD: mean=65.29 (7.19); HOA: mean=68.75 (5.77); F(1,74)=.5.31, p=.024). As expected, groups differed on HDRS scores. See Table 1 for demographic details.
Table 1. Demographic Information and Group Differences.
| HOA N=48 |
LLD N=28 |
Group differences | |
|---|---|---|---|
| Age - Mean (sd) ± | 68.75 (5.77) | 65.29 (7.19) | F=5.31, df=1,74, p=.024 * |
| Sex – N (m,f) + | 18,30 | 8,20 | X2=.626, df=1, p=.429 |
| Highest Education Level in Years - Mean (sd) ± | 14.90 (2.90) | 15.18 (3.29) | F=.152, df=1,74, p=.698 |
| HDRS - Mean (sd) | 1.60 (1.60) | 18.57 (2.73) | F=1160.12, df=1,74, |
| Range ± | 0-6 | 15-25 | p<.001 ** |
significant at 5% level;
significant at 1% level; Statistical analysis:
ANOVA;
Chi-square.
Sex differences
Although sex differences between the groups were not observed, the number of males in both groups was fewer than the number of females (HOA: males=18; females=30; LLD: males=8; females=28). For the LLD group in particular the uneven group and small n means comparison of sex differences should be treated with caution. Sex differences for each group were explored with ANOVA, see Supplementary Table 1. In the LLD group males demonstrated more efficient networks than females, but no sex differences were observed in the HOA group. To control for the different pattern of associations which may be due to the different statistical power in each group, sex was included as a covariate in further analysis.
Group differences
Due to the reported group differences in age and the sex differences on imaging metrics (as described above), these variables were included as covariates in the analyses.
Global Measures
ANCOVA did not reveal any significant group differences between the groups on any global measure; see Supplementary Table 2 for details.
Local Measures
ANCOVA (controlling for age and sex) identified group differences in the right PFC and right temporal regions. Specifically, Vulnerability was significantly higher in the right PFC in the LLD group compared to HOA. In contrast Vulnerability in the right temporal region was higher among HOA compared to the LLD group. Also in the right temporal region, Centrality was significantly lower in the LLD group compared to HOA. These differences remained significant after FDR correction. See Table 2 for details.
Table 2. Mean and Standard Deviations for Local Measures by Group; ANCOVA controlling for age and sex.
| Right | Left | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Mean (SD) | ANCOVA (df=1,72) | FDR | Mean (SD) | ANCOVA (df=1,72) | ||||
|
| ||||||||
| HOA | LLD | HOA | LLD | |||||
| PFC | 182.36 | 238.60 | F=3.36 | 240.35 | 244.08 | F=.102 | ||
| Centrality | (99.87) | (140.38) | p=.071 | (124.75) | (163.38) | p=.751 | ||
|
| ||||||||
| .012 | .012 | F=.103 | .013 | .012 | F=.172 | |||
| Path length | (.003) | (.002) | p=.749 | (.002) | (.003) | p=.679 | ||
|
| ||||||||
| .003 | .006 | F=4.36 | .005 | .006 | F=.001 | |||
| Vulnerability | (.005) | (.006) | p=.040 * | q=.28 | (.005) | (.006) | p=.973 | |
|
| ||||||||
| Cingulate | 133.52 | 150.02 | F=.417 | 130.94 | 131.22 | F=.002 | ||
| Centrality | (103.38) | (113.35) | p=.520 | (84.35) | (93.87) | p=.969 | ||
|
| ||||||||
| .012 | .011 | F=.206 | .011 | .011 | F=.570 | |||
| Path length | (.003) | (.003) | p=.651 | (.002) | (.002) | p=.453 | ||
|
| ||||||||
| .002 | .003 | F=.910 | .002 | .002 | F=.001 | |||
| Vulnerability | (.005) | (.005) | p=.343 | (.004) | (.005) | p=.975 | ||
|
| ||||||||
| Temporal | 136.20 | 82.62 | F=6.22 | 108.28 | 79.81 | F=3.31 | ||
| Centrality | (97.72) | (80.19) | p=.015 * | q=.16 | (98.44) | (84.46) | p=.073 | |
|
| ||||||||
| .019 | .018 | F=.017 | .018 | .018 | F=1.66 | |||
| Path length | (.007) | (.004) | p=.896 | (.005) | (.005) | p=.201 | ||
|
| ||||||||
| .001 | -.002 | F=7.34 | -.001 | -.002 | F=1.52 | |||
| Vulnerability | (.005) | (.004) | p=.008 ** | q=.16 | (.005) | (.004) | p=.222 | |
|
| ||||||||
| N | 48 | 28 | 48 | 28 | ||||
significant at 5% level;
significant at 1% level. Items in bold remain significant after FDR correction (q<.3); FDR correction was applied to the 18 comparisons included in the table above.
Correlations with Age
Given sex differences on these metrics and the lack of statistical power to split the groups for a depression by sex consideration of age associates, sex was included as a control variable in the following analysis.
Global Measures
No significant correlations were observed between global network measures and age in either group (controlling for sex).
Local Measures
Correlations were performed separately for HOA and LLD individuals controlling for sex, see Table 3 for details. HOA: After FDR, age correlated significantly with Path Length metrics in bilateral PFC and temporal lobes and right cingulate. LLD: After FDR, age correlated with bilateral Path Length and right centrality in the temporal lobe.
Table 3. Correlations between Local Metrics and Age for both groups controlling for sex.
| HOA | LLD | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Right | Left | Right | Left | |||||
| Correlation | FDR | Correlation | FDR | Correlation | FDR | Correlation | FDR | |
| PFC | r=.071 | r=-.144 | r=-. 119 | r=-.298 | ||||
| Centrality | p=.638 | p=.344 | p=.556 | p=.131 | ||||
|
| ||||||||
| r=.426 | r=.371 | r=.274 | r=.295 | |||||
| Path length | p=.003 ** | q=.018 | p=.010 * | q=.036 | p=.167 | p=.136 | ||
|
| ||||||||
| r=.092 | r=-.221 | r=-.113 | r=-.270 | |||||
| Vulnerability | p=.540 | p=.136 | p=.575 | p=.174 | ||||
|
| ||||||||
| Cingulate | r=.001 | r=.274 | r=.146 | r=-.213 | ||||
| Centrality | p=.944 | p=.062 | p=.468 | p=.286 | ||||
|
| ||||||||
| r=.444 | r=.259 | r=.236 | r=.233 | |||||
| Path length | p=.002 ** | q=.018 | p=.079 | p=.236 | p=.243 | |||
|
| ||||||||
| r=.089 | r=.229 | r=.083 | r=-.032 | |||||
| Vulnerability | p=.553 | p=.122 | p=.680 | p=.874 | ||||
|
| ||||||||
| Temporal | r=. 114 | r=-.336 | r=-.401 | r=-.224 | ||||
| Centrality | p=.444 | p=.021 * | q=.063 | p=.038 * | q=.228 | p=.261 | ||
|
| ||||||||
| r=.565 | r=.402 | r=.476 | r=.654 | |||||
| Path length | p<.001 ** | q<.001 | p=.005 ** | q=.023 | p=.012 * | q=.108 | p<.001 ** | q=.004 |
|
| ||||||||
| r=.123 | r=-.217 | r=-.379 | r=-.180 | |||||
| Vulnerability | p=.409 | p=.143 | p=.051 | p=.370 | ||||
|
| ||||||||
| N=48 (df=45) | N=28 (df=25) | |||||||
Partial correlation controlling for sex.
significant at 5% level
significant at 1% level. Items in bold remain significant after FDR correction (q<.3); FDR was applied to the 18 correlations for the HOA; and separately for the 18 correlations for the LLD group.
Conclusions
We analyzed structural brain networks of older adults with and without depression, assessing associations with age. Differences between individuals with LLD and HOA were observed for local metrics in right PFC and temporal regions particularly for Vulnerability. Vulnerability in the right PFC was higher in the LLD group compared to the HOA; whereas in the right temporal region Vulnerability was higher among HOA: indicating that for LLD individuals frontal regions are vital to the efficiency of the network, whereas in HOA temporal regions are more important. Although a preliminary analysis, this suggests that the network that supports functional operations is organized differently in LLD compared to HOA. Results presented here show similarities to our previous findings, despite using different methods and examining different brain tissue. In both Ajilore and colleagues' examination of inter-correlations between gray matter volumes and the current investigation of white matter, stronger hubs in right temporal regions are observed among HOA whereas LLD individuals are characterized by robust hubs in frontal regions14.
In the current study, patients with LLD have a network that is globally as efficient as that of HOA, unlike findings from a few previous studies; however there are key differences in participants and study design13, 14. Although measuring white matter networks in a similar sample size, Bai and colleagues examined remitted late-onset LLD patients, compared to the currently depressed sample including both early- and late-onset LLD in this study13. Thus differences in results may reflect the dependence of network properties on current mood state, as well as the onset or illness duration. Although results here are preliminary, these findings may suggest that reorganization of brain networks is occurring in subjects with LLD. One possible explanation for such reorganization is that some form of compensation may have taken place, as has been hypothesized in aging12, with the local network being restructured to maintain function in the face of brain changes associated with LLD. Our results suggest that in LLD individuals may utilize frontal regions to support function rather than relying on temporal regions (as in HOA). This may indicate that the reduced efficiency of the temporal lobe often observed in depression34, 35, leads to a reliance on more distributed possibly less efficient networks.
Significant correlations were observed between local metrics and age particularly among healthy older adults, whereas no such associations were observed in global metrics. Although two previous studies have identified age-related declines in global efficiency in healthy aging10, 11, one other study identified a similar pattern to that reported here – i.e., no age-related global effects but significant local associations with age12. Additionally, different patterns of correlations were observed between groups when exploring the relationship between age and local network metrics. Age effects in the HOA group were widespread across the whole brain as reported previously11; with longer Path Length in frontal, cingulate and temporal regions associated with older age. These prevalent age effects may reflect age-related cortical disconnection and contribute to the cognitive changes observed with normal aging36-38. In contrast among LLD patients, older age was positively correlated with metrics only in the temporal region. This pattern suggests that in LLD the network properties of the temporal lobe is impacted by disease-age interactions39, 40, instead of a more widespread pattern observed among HOA. This is consistent with a previous study suggesting that whereas the dorsolateral prefrontal cortex appears to respond to treatment, other brain regions are not treatment responsive and may represent underlying brain dysfunction in depression41.
Results in this study should be carefully interpreted in the context of study limitations. Graph theory methods have only recently been applied to examine brain networks and the optimal combination of image acquisition protocol and pre/post processing techniques have yet to be established. While these results contribute to the growing iterature, the lack of a “gold standard” for comparison means that they should be interpreted thoughtfully and with attention to new findings as well as the field as a whole. Despite this caveat, we demonstrated findings similar to those reported in studies using different graph theory methods; moreover the current method builds on our previous study by examining white matter networks (compared to previous gray matter analysis), and allows us to examine individual differences and correlations with age not possible in the previous analysis12, 14. DTI also has limitations including the possibility of spurious streamlines that may not be supported by evidence. Moreover, the graph-theoretical analyses similar to our pipeline implementation have been shown to be dependent on the streamline reconstruction technique 42, the choice of neuro-anatomical atlases for the definition of the “hubs”43, and different matrix normalization strategies44. Also, in this study we used 12-parameter affine transformations for realigning the MPRAGE and DTI spaces, which only incompletely corrects for B0 inhomogeneity-induced geometric distortions. In terms of the sample, the groups were not large, had different statistical power due to uneven sample sizes and included smaller numbers of males than females. Within the LLD group a heterogeneous sample of late-onset and early onset patients was included and due to sample size, differences between age-of-onset groups could not be explored.
To conclude, in this preliminary study we demonstrate a seemingly preserved global network in LLD, but with local network susceptibilities that differ between LLD and HOA. Furthermore, widespread age associations were noted in the HOA group, as opposed to more localized age-related changes in the LLD group. Future applications of this method to larger samples and incorporating cognitive function may clarify whether results reflect successful adaptation in LLD patients or altered structural brain networks that are not functionally beneficial.
Supplementary Material
Acknowledgments
We wish to acknowledge the assistance of the Mood Disorders Team for participant screening and assessment.
Source of Funding: Funding for this study was provided by NIMH 7RO1 MH073989-04 (AK).
Footnotes
Conflicts of Interest: No Disclosures to Report
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ballmaier M, Narr KL, Toga AW, et al. Hippocampal Morphology and Distinguishing Late-Onset From Early-Onset Elderly Depression. Am J Psychiatry. 2008;165(2):229–237. doi: 10.1176/appi.ajp.2007.07030506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lamar M, Charlton RA, Zhang A, Kumar A. Differential associations between types of verbal memory and prefrontal brain structure in healthy aging and late life depression. Neuropsychologia. 2012;50(8):1823–1829. doi: 10.1016/j.neuropsychologia.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang A, Leow A, Ajilore O, et al. Quantitative Tract-Specific Measures of Uncinate and Cingulum in Major Depression Using Diffusion Tensor Imaging. Neuropsychopharmacology. 2012;37(4):959–967. doi: 10.1038/npp.2011.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Charlton RA, Schiavone F, Barrick TR, Morris RG, Markus HS. Diffusion Tensor Imaging detects age-related white matter change over a two-year follow-up which is associated with working memory decline. Journal of Neurology, Neurosurgery & Psychiatry. 2010;81:13–19. doi: 10.1136/jnnp.2008.167288. [DOI] [PubMed] [Google Scholar]
- 5.Gunning-Dixon FM, Raz N. Neuroanatomical correlates of selected executive functions in middle-aged and older adults: a prospective MRI study. Neuropsychologia. 2003;41(14):1929–1941. doi: 10.1016/s0028-3932(03)00129-5. [DOI] [PubMed] [Google Scholar]
- 6.Bullmore E, Sporns O. Complex brain networks: graph theoretical analysis of structural and functional systems. Nat Rev Neurosci. 2009;10(4):312. doi: 10.1038/nrn2575. [DOI] [PubMed] [Google Scholar]
- 7.Rubinov M, Sporns O. Complex network measures of brain connectivity: uses and interpretations. NeuroImage. 2010;52(3):1059–1069. doi: 10.1016/j.neuroimage.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Guye M, Bettus G, Bartolomei F, Cozzone P. Graph theoretical analysis of structural and functional connectivity MRI in normal and pathological brain networks. Magnetic Resonance Materials in Physics, Biology and Medicine. 2010;23(5):409–421. doi: 10.1007/s10334-010-0205-z. [DOI] [PubMed] [Google Scholar]
- 9.Wu K, Taki Y, Sato K, et al. Age-related changes in topological organization of structural brain networks in healthy individuals. Hum Brain Mapp. 2012;33(3):552–568. doi: 10.1002/hbm.21232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu W, Wen W, He Y, Xia A, Anstey KJ, Sachdev P. Changing topological patterns in normal aging using large-scale structural networks. Neurobiol Aging. 2012;33:899–913. doi: 10.1016/j.neurobiolaging.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 11.Wen W, Zhu W, He Y, et al. Discrete Neuroanatomical Networks Are Associated with Specific Cognitive Abilities in Old Age. The Journal of Neuroscience. 2011;31(4):1204–1212. doi: 10.1523/JNEUROSCI.4085-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gong G, Rosa-Neto P, Carbonell F, Chen ZJ, He Y, Evans AC. Age- and Gender-Related Differences in the Cortical Anatomical Network. The Journal of Neuroscience. 2009;29(50):15684–15693. doi: 10.1523/JNEUROSCI.2308-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bai F, Shu N, Yuan Y, et al. Topologically Convergent and Divergent Structural Connectivity Patterns between Patients with Remitted Geriatric Depression and Amnestic Mild Cognitive Impairment. The Journal of Neuroscience. 2012;32(12):4307–4318. doi: 10.1523/JNEUROSCI.5061-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ajilore O, Lamar M, Leow A, Zhang A, Kumar A. Graph theory analysis of cortical-subcortical networks in late-life depression. Am J Geriatr Psychiatry. 2014;22(2):195–206. doi: 10.1016/j.jagp.2013.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bae JN, MacFall JR, Krishnan KR, Payne ME, Steffens DC, Taylor WD. Dorsolateral Prefrontal Cortex and Anterior Cingulate Cortex White Matter Alterations in Late-Life Depression. Biol Psychiatry. 2006;60(12):1356–1363. doi: 10.1016/j.biopsych.2006.03.052. [DOI] [PubMed] [Google Scholar]
- 16.Herrmann LL, Le Masurier M, Ebmeier KP. White matter hyperintensities in late life depression: a systematic review. Journal of Neurology, Neurosurgery & Psychiatry. 2008;79(6):619–624. doi: 10.1136/jnnp.2007.124651. [DOI] [PubMed] [Google Scholar]
- 17.Kumar A, Mintz J, Bilker W, Gottlieb G. Autonomous neurobiological pathways to late-life major depressive disorder: clinical and pathophysiological implications. Neuropsychopharmacology. 2002;26(2):229–236. doi: 10.1016/S0893-133X(01)00331-1. [DOI] [PubMed] [Google Scholar]
- 18.Taylor WD, MacFall JR, Steffens DC, Payne ME, Provenzale JM, Krishnan KRR. Localization of age-associated white matter hyperintensities in late-life depression. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(3):539–544. doi: 10.1016/S0278-5846(02)00358-5. [DOI] [PubMed] [Google Scholar]
- 19.Taylor WD, MacFall JR, Payne ME, et al. Late-life depression and microstructural abnormalities in dorsolateral prefrontal cortex white matter. The American Journal of Psychiatry. 2004;161(7):1293–1296. doi: 10.1176/appi.ajp.161.7.1293. [DOI] [PubMed] [Google Scholar]
- 20.Charlton RA, Lamar M, Zhang A, Yang S, Ajilore O, Kumar A. White-matter tract integrity in late-life depression: associations with severity and cognition. Psychol Med. 2014;44(07):1427–1437. doi: 10.1017/S0033291713001980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pujol J, Bello J, Deus J, Mart+¡-Vilalta JL, Capdevila A. Lesions in the left arcuate fasciculus region an depressive symptoms in multiple sclerosis. Neurology. 1997;49(4):1105–1110. doi: 10.1212/wnl.49.4.1105. [DOI] [PubMed] [Google Scholar]
- 22.Zou K, Huang X, Li T, et al. Alterations of white matter integrity in adults with major depressive disorder a magnetic resonance imaging study. J Psychiatry Neurosci. 2008;33(6):525–530. [PMC free article] [PubMed] [Google Scholar]
- 23.Greicius MD, Flores BH, Menon V, et al. Resting-State Functional Connectivity in Major Depression: Abnormally Increased Contributions from Subgenual Cingulate Cortex and Thalamus. Biol Psychiatry. 2007;62(5):429–437. doi: 10.1016/j.biopsych.2006.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rive MM, van Rooijen G, Veltman DJ, Phillips ML, Schene AH, Ruh+® HG. Neural correlates of dysfunctional emotion regulation in major depressive disorder. A systematic review of neuroimaging studies. Neuroscience & Biobehavioral Reviews. 2013 doi: 10.1016/j.neubiorev.2013.07.018. In press. [DOI] [PubMed] [Google Scholar]
- 25.Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental State’ A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer RL, Williams JBW, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID) History, Rationale, and Description. Arch Gen Psychiatry. 1992;49(8):624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 27.Hamilton MA. A rating scale for depression. Journal of Neurology Neurosurgery and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang H, van Zijl PC, Kim J, Pearlson GD, Mori S. DtiStudio: resource program for diffusion tensor computation and fiber bundle tracking. Comput Methods Programs Biomed. 2006;81(2):106–116. doi: 10.1016/j.cmpb.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Desikan RS, Ségonne F, Fischl B, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31(3):968–980. doi: 10.1016/j.neuroimage.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 30.Destrieux C, Fischl B, Dale A, Halgren E. Automatic parcellation of human cortical gyri and sulci using standard anatomical nomenclature. Neuroimage. 2010;53(1):1–15. doi: 10.1016/j.neuroimage.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fischl B, van der Kouwe A, Destrieux C, et al. Automatically Parcellating the Human Cerebral Cortex. Cereb Cortex. 2004;14(1):11–22. doi: 10.1093/cercor/bhg087. [DOI] [PubMed] [Google Scholar]
- 32.Benjamini Y, Hochberg Y. Controlling the FDR: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B Statistical Methodology. 1995;57(1):289–300. [Google Scholar]
- 33.Bhaumik DK, Roy A, Lazar NA, et al. Hypothesis testing, power and sample size determination for between group comparisons in fMRI experiments. Stat Methodol. 2009;6(2):133–146. doi: 10.1016/j.stamet.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bremner JD, Narayan M, Anderson ER, Staib LH, Miller HL, Charney DS. Hippocampal Volume Reduction in Major Depression. Am J Psychiatry. 2000;157(1):115–118. doi: 10.1176/ajp.157.1.115. [DOI] [PubMed] [Google Scholar]
- 35.Drevets W, Price J, Furey M. Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Structure and Function. 2008;213(1):93–118. doi: 10.1007/s00429-008-0189-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Charlton RA, Barrick TR, McIntyre DJO, et al. White matter damage on diffusion tensor imaging correlates with age related cognitive decline. Neurology. 2006;66(2):217–222. doi: 10.1212/01.wnl.0000194256.15247.83. [DOI] [PubMed] [Google Scholar]
- 37.Metzler-Baddeley C, Jones DK, Belaroussi B, Aggleton JP, O'Sullivan MJ. Frontotemporal Connections in Episodic Memory and Aging: A Diffusion MRI Tractography Study. The Journal of Neuroscience. 2011;31(37):13236–13245. doi: 10.1523/JNEUROSCI.2317-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O'Sullivan M, Jones DK, Summers PE, Morris RG, Williams SCR, Markus HS. Evidence for cortical “disconnection” as a mechanism of age-related cognitive decline. Neurology. 2001;57(4):632–638. doi: 10.1212/wnl.57.4.632. [DOI] [PubMed] [Google Scholar]
- 39.Biver F, Goldman S, Delvenne V, et al. Frontal and parietal metabolic disturbances in unipolar depression. Biol Psychiatry. 1994;36(6):381–388. doi: 10.1016/0006-3223(94)91213-0. [DOI] [PubMed] [Google Scholar]
- 40.Surguladze SA, El-Hage W, Dalgleish T, Radua J, Gohier B, Phillips ML. Depression is associated with increased sensitivity to signals of disgust: A functional magnetic resonance imaging study. Journal of Psychiatric Research. 2010;44(14):894–902. doi: 10.1016/j.jpsychires.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ishizaki J, Yamamoto H, Takahashi T, Takeda M, Yano M, Mimura M. Changes in regional cerebral blood flow following antidepressant treatment in late-life depression. Int J Geriatr Psychiatry. 2008;23(8):805–811. doi: 10.1002/gps.1980. [DOI] [PubMed] [Google Scholar]
- 42.Li L, Rilling JK, Preuss TM, Glasser MF, Hu X. The effects of connection reconstruction method on the interregional connectivity of brain networks via diffusion tractography. Hum Brain Mapp. 2012;33(8):1894–1913. doi: 10.1002/hbm.21332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zalesky A, Fornito A, Harding IH, et al. Whole-brain anatomical networks: Does the choice of nodes matter? NeuroImage. 2010;50(3):970–983. doi: 10.1016/j.neuroimage.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 44.van den Heuvel MP, Sporns O. Rich-Club Organization of the Human Connectome. The Journal of Neuroscience. 2011;31(44):15775–15786. doi: 10.1523/JNEUROSCI.3539-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.