Abstract
Background
This was a prospective study of radiofrequency segmental thermal ablation (RFA) for the treatment of incompetent varicose great saphenous veins (GSVs). The present report describes long-term follow-up at 5 years.
Methods
The 5-year follow-up of this multicentre European study included assessment of the Venous Clinical Severity Score (VCSS), and GSV occlusion and reflux on duplex imaging.
Results
A total of 225 patients had 295 GSVs treated by RFA, achieving an initial vein occlusion rate of 100 per cent. With 80·0 per cent compliance, Kaplan–Meier analyses showed a GSV occlusion rate of 91·9 per cent and a reflux-free rate of 94·9 per cent at 5 years. Among the 15 GSVs noted with reflux during follow-up, only three showed full recanalization of the GSV at 1 week, 6 months and 3 years. Of the 12 legs with partial recanalization, reflux originated at the saphenofemoral junction in ten, with a mean length of the patent segment of 5·8 (range 3·2–10) cm; only six patients were symptomatic. Mean(s.d.) VCSS scores improved from 3·9(2·1) at baseline to 0·6(1·2), 0·9(1·3) and 1·3(1·7) at 1, 3 and 5 years.
Conclusion
At 5 years RFA proved to be an efficient endovenous treatment for incompetent GSVs in terms of sustained clinical and anatomical success for the vast majority of treated patients.
Introduction
Lower-limb venous insufficiency is common in adults and can manifest as a cosmetic annoyance in the early stages, but advance to a debilitating condition1. Signs and symptoms include visible varicose veins, calf pain or swelling, leg cramping or fatigue, and a sensation of heaviness1. Left untreated, skin discoloration, induration or active ulceration may ensue. Most frequently, incompetent valves in the great or small saphenous veins cause pathological venous reflux, and precipitate this condition1,2. When a refluxing saphenous vein is diagnosed, removing it from the circulation eliminates or improves the associated signs and symptoms.
Traditionally, high saphenous ligation and stripping (HLS) surgery has been used to remove the diseased great saphenous vein (GSV). Although successful, its invasive nature is associated with postoperative morbidity and delay in return to normal activities3–5. Less invasive endovascular treatments have been developed with the goal of achieving equal or better efficacy than HLS surgery, with reduced postoperative morbidity and faster recovery6,7. Radiofrequency segmental thermal ablation (RFA) is a technique used for heat-induced obliteration of incompetent truncal veins, with excellent early results, including high ablation rates, moderate side-effects and speedy return to normal activities8–10. Short- and mid-term results from prospective randomized trials11–13 and a meta-analysis14 comparing RFA with HLS, endovenous laser or ultrasound-guided foam sclerotherapy proved that RFA sets the standard in terms of efficacy and safety.
This report presents the 5-year final results of the European multicentre cohort study including first-in-human use of RFA.
Methods
This international, prospective, multicentre, cohort study was designed to evaluate the long-term effects of RFA of the GSV using a catheter with an integrated heating element, the ClosureFast™ (Venefit™; Covidien, Mansfield, Massachusetts, USA) procedure. Unselected, consecutively screened patients presenting with signs and symptoms of lower-limb venous disease in the GSV with confirmed reflux, defined as reverse flow with duration greater than 0·5 s on duplex ultrasound imaging (DUS), and eligible for endovascular treatment, were candidates for the study. Inclusion criteria also included age between 18 and 80 years at time of enrolment, physical condition allowing frequent walking after the procedure, and availability to complete study requirements. Patients who had thrombosis in the diseased vein segment to be treated, were pregnant, had a known allergic reaction to required anaesthetics, or were participating in another clinical trial were excluded from the study10.
Eight sites in Germany and France participated in the study. All investigators had experience with the previous ClosurePlus™ catheter (Covidien) and were trained on the study device before participation. The study protocol was approved by the local ethical review boards; all subjects provided written informed consent. Study visits took place at baseline, time of the procedure, and 1 week, 3 months, 6 months, 1 year, 2 years, 3 years, 4 years and 5 years after the procedure. Follow-up visits included clinical and DUS evaluations. This trial is registered at http://ClinicalTrials.gov (NCT00842296).
Procedures
A detailed description of the study protocol was published previously10. Briefly, the study device, the ClosureFast™ catheter, is a 7-Fr catheter with an integrated heating element and handle with an attached cable for connection to the radiofrequency generator. The catheter is compatible with 0·025-inch guidewires, and available in lengths of 60 and 100 cm. The distal heating element is 7 cm long. It comprises a fixed-diameter heating coil element that transfers heat to the vessel wall by contact and conduction with the vessel wall tissue. The heating element is activated with radiofrequency energy to 120°C for 20-s heating cycles. For study procedures, the vein was accessed at the distal point of reflux, and the catheter tip was advanced towards the epigastric vein connection and placed 1–2 cm below the saphenofemoral junction (SFJ). Energy was delivered after injection of perivenous tumescent local anaesthesia, as described previously10. External compression was achieved during treatment either manually or by using the ultrasound probe. If applicable, patients were offered treatment of tributaries by either phlebectomy or sclerotherapy at the discretion of the treating physician.
At each follow-up visit, DUS was completed to assess vein occlusion, reflux status (if flow was present) and compressibility of the treated segment, and for measurement of the diameters of the treated vein segment. Ultrasound examinations were performed by a physician familiar with the procedure to obtain ultrasound information on the treated leg at the same level. Follow-up clinical evaluation included assessment of venous signs and symptoms, return to normal activity, walking status and adverse events.
Endpoints
The primary study endpoints were vein occlusion and absence of reflux, as determined by DUS. Vein occlusion was defined as absence of flow in the treated vein using distal augmentation. Flow in the stump of the GSV up to 3 cm below the SFJ was considered normal. Secondary endpoints were evaluated using standard scales, including the Clinical Etiologic Anatomic Pathophysiologic (CEAP) classification15,16, the Venous Clinical Severity Score (VCSS)17,18, and a visual analogue scale for pain, to assess clinical signs and symptoms of lower-limb venous disease, and patient interviews for presence of complications and side-effects.
Statistical analysis
All legs of enrolled patients with available data were considered analysable. The primary endpoints are presented over 5 years using Kaplan–Meier estimates. CEAP was analysed as an ordinal variable, VCSS as a continuous variable using both parametric and non-parametric tests, and pain as a continuous variable using parametric tests. All statistical analyses were performed using SAS® (SAS Institute, Cary, North Carolina, USA).
Results
Between April 2006 and March 2007, 225 subjects were enrolled and 295 legs (bilateral disease in 70 patients) were treated at eight centres in Germany and France. At 5 years, 177 subjects with 236 treated limbs had completed the follow-up examinations; the study completion rate was 78·7 per cent. Baseline characteristics of the study subjects and procedural data have been published in detail elsewhere9.
The mean(s.d.) preoperative diameter of all study-treated GSVs 3 cm distal to the SFJ (GSV-3 cm) was 5·8(2·2) (range 2·0–18·0) mm. The majority of vein diameters were measured in the supine position (222, 75·3 per cent), based on the guidance provided in the initial version of the study protocol, with a mean baseline diameter of 5·5(2·3) (2·0–18·0) mm. In comparison, the GSV-3 cm diameters measured in the standing position (73 legs) were significantly larger: mean 6·9(1·8) (2·5–11·8) mm (P < 0·001). Previous venous procedures on the treated leg included sclerotherapy (5·4 per cent), phlebectomy (2·7 per cent), stripping (1·0 per cent), VNUS ClosurePlus™ catheter (0·7 per cent), endovascular laser (0·3 per cent), ligation (0·3 per cent) and other (0·3 per cent).
Early results
Technical success was achieved in all legs (295, 100 per cent). The mean GSV-3 cm diameter immediately after the procedure as measured by DUS (291 legs) was 3·3(1·5) (0·8–9·2) mm, in comparison with 5·8(2·2) (2·0–18·0) mm before the procedure. Vein wall thickening was visible in the treated segment in 293 (99·7 per cent) of 294 legs. Vein occlusion immediately after segmental thermal ablation was achieved in 294 legs (99·7 per cent), with a mean distance from the SFJ to the occlusion of 1·1(0·5) (0–2·9) cm. The remaining leg had delayed GSV occlusion, shown at 1 week after study treatment.
Ultrasound follow-up
DUS was performed during follow-up visits to measure vein diameters following segmental thermal ablation therapy. Compliance with the DUS follow-up was 98·3 per cent at 3 months, 98·0 per cent at 6 months, 99·0 per cent at 1 year, 94·6 per cent at 2 years, 88·1 per cent at 3 years, 86·1 per cent at 4 years and 80·0 per cent at 5 years. Mean diameters of the GSV-derived fibrotic cord 3 cm distal to the SFJ decreased from 5·8(2·2) mm before treatment to 4·6(1·7) mm at 1 week after treatment (295 legs) and 2·0(1·0) mm at 5 years (110 legs; 126 veins (53·4 per cent) not visible on DUS) (Fig. 1). Mean stump lengths at the SFJ remained stable over time: 1·0(0·7) cm at 1 week (289 legs), 1·2(0·7) cm at 3 months (289 legs) and 1·4(1·5) cm at 5 years (233 legs) after treatment.
Figure 1.
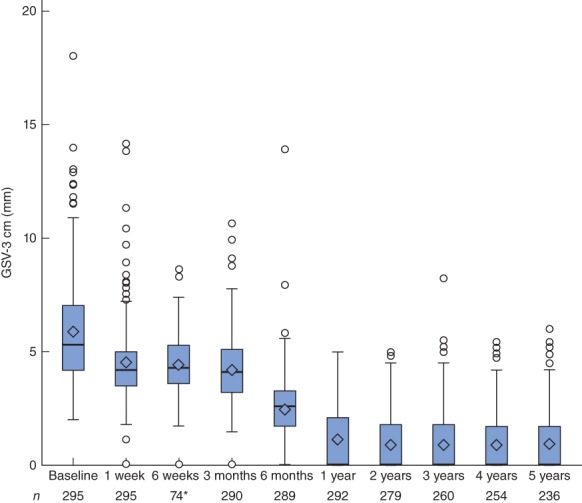
Great saphenous vein diameter 3 cm below the saphenofemoral junction (GSV-3 cm) after radiofrequency ablation treatment. Mean (diamond), median (line within box), i.q.r. (box), and range (error bar) excluding outliers (circles) are shown. *Six-week follow-up only for initially enrolled subjects
Blood flow in any part of the treated GSV from 3 cm below the SFJ and distally was observed in 25 different GSVs during follow-up. Of these, 15 legs had GSV reflux, which, remarkably, was not necessarily linked to clinical symptoms. Of the 15 legs, clinically significant total recanalization of the treated GSV was observed in three (at 1 week, 6 months and 3 years). Segmental recanalization was noted in the other 12 legs, with reflux originating at the SFJ in ten (1 at 3 months, 2 at 1 year, 3 at 2 years, 2 at 3 years, 2 at 4 years) and reflux not connected to the SFJ in two legs (1 at 2 years, 1 at 3 years). For the ten legs with reflux originating at the SFJ, the mean length of the patent segment was only 5·8 (3·2–10) cm. Four of the ten legs were completely asymptomatic; the other six had recurrent varicose veins.
For the two legs with reflux not originating at the SFJ, reflux was observed in the distal third of the GSV, originating from a tributary in one patient, and at mid-GSV with reflux originating from a perforating vein in the second patient. Both legs had multiple varicose veins above and below the knee.
Among the 15 legs with documented reflux during follow-up, two had a patent segment at 1 and 2 years, and presented with reflux 1 year later. In contrast, the reflux observed in one leg at 3 months and in two legs at 2 years was no longer present at 1 and 5 years respectively.
Ten other legs developed a patent segment of the treated GSV without reflux on DUS. In nine, the patent segment originated from the SFJ with a mean length of only 4·1 (3·3–6·5) cm, and had no clinical relevance. In one leg, the patent segment free from reflux was located below the knee.
Using Kaplan–Meier estimates, the GSV occlusion rate was 91·9 per cent at 5 years (Fig. 2). The Kaplan–Meier estimate of reflux-free GSV was 94·9 per cent at 5 years (Fig. S1, supporting information). The standard errors for all estimates were below 2 per cent.
Figure 2.
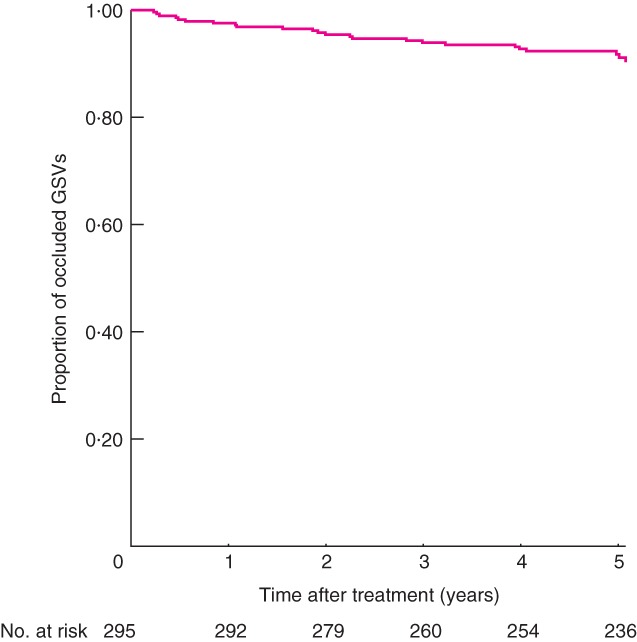
Great saphenous vein occlusion rate after radiofrequency ablation treatment
Clinical results
At baseline, the mean VCSS for the 295 legs was 3·9(2·1), ranging from 1, representing uncomplicated varicose veins or venous oedema with ankle swelling in the evening, to 11, in a patient with ankle ulceration. The VCSS improved over time starting 3 months after RFA, reaching a value of 1·3(1·7) for 236 treated legs at the 5-year follow-up (Fig. 3).
Figure 3.
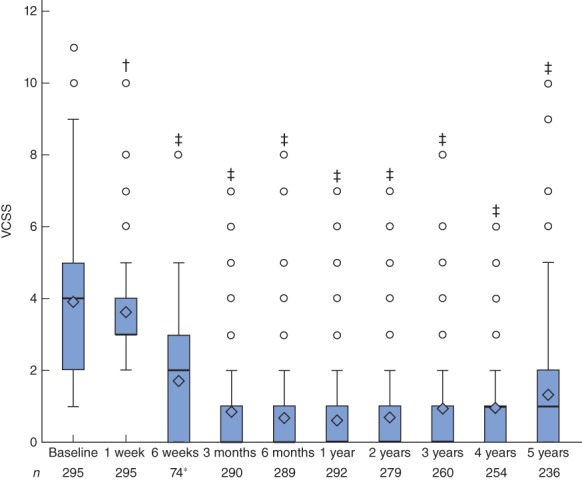
Venous Clinical Severity Score (VCSS; range 0–30) before and after radiofrequency ablation for great saphenous vein reflux. Mean (diamond), median (line within box), i.q.r. (box), and range (error bar) excluding outliers (circles) are shown. *Six-week follow-up only for initially enrolled subjects. †P = 0·012, ‡P < 0·001 versus baseline (paired t test)
Varicose veins were present in 98·6 per cent of legs at baseline, with 52·2 originating from the GSV (VCSS domain score 2). At 3 months after treatment, only 15·2 per cent of the treated limbs had varicose veins present, according to the VCSS assessment. The proportion of legs with varicose veins (VCSS domain score 1) increased over time to 40·7 per cent at 5 years. However, at the same time, only 5·9 per cent of the treated legs had multiple varicose veins originating from the GSV (VCSS domain score 2) (Fig. S2, supporting information).
Similarly, 52·9 per cent of diseased limbs had oedema at baseline. By 3 months after treatment, only 8·6 per cent of the treated legs had residual oedema, but this increased to 23·7 per cent by 5 years, according to the VCSS assessment. At 5 years, most of the reported residual oedema was at the ankles and visible only in the evenings (19·1 per cent; VCSS domain score 1). A few patients also had oedema below the knee visible in the afternoon (VCSS domain score 2; 1·7 per cent at 1 year, 2·7 per cent at 3 years, 4·2 per cent at 5 years) (Fig. S3, supporting information).
Significant pain was present in the legs at baseline in 58·6 per cent of the legs, according to the VCSS pain domain: occasional (39·0 per cent), daily (17·3 per cent) or activity-limiting (2·4 per cent). By 3 months after treatment, this had decreased to 6·9 per cent of legs: occasional (5·5 per cent) or daily (1·4 per cent). According to the VCSS assessment, 92·4 per cent of the treated limbs were pain-free at the 5-year follow-up visit (Fig. S4, supporting information).
Discussion
Here, the 5-year results of the first-in-human use of segmental thermal ablation for incompetent GSVs are reported. The strength of this prospective multicentre cohort study arises from the high compliance rate of 80·0 per cent for DUS after 5 years19. Meanwhile, studies on RFA with shorter follow-up have already proven the high efficacy, safety and speed of the procedure8,9,12,13. Its favourable side-effect profile, in conjunction with a high rate of maintained GSV occlusion in the mid-term9, have been corroborated by prospective multicentre comparisons with endovenous laser and surgery13. Other studies11,12 have confirmed the favourable side-effect profile of RFA in comparison with endovenous laser ablation (EVLA). Pain, tenderness and bruising were less frequent after RFA during the first 2 weeks after the procedure11, and patients who received RFA returned to work 4 days earlier than those who received EVLA12. Looking at other relevant side-effects, the rate of paraesthesia of 0·4 per cent in the present study9 compared favourably with a rate of 7·6 per cent 12 months after EVLA, performed with a more recently used wavelength of 1470 nm20. Comparing RFA with the new technique of mechanochemical ablation (MOCA), it seems that MOCA is less painful with a quicker return to work; however, MOCA has not yet proven equal to RFA for clinical and anatomical outcomes at 1-year follow-up21.
RFA maintains occlusion rates of more than 90 per cent and freedom from reflux in 95 per cent of legs after 5 years. This is reassuring with such a favourable side-effect profile. Currently, the focus of most new treatments for saphenous vein reflux is directed towards a minimal side-effect profile and high periprocedural quality of life. However, the primary intention of reliable and durable abolition of vein reflux must not be sacrificed. Foam sclerotherapy of saphenous veins, which initially looks attractive because of its easy and quick delivery and its minimal impairment of quality of life, serves as an example. With a side-effect and quality-of-life profile comparable to RFA13, 1-year anatomical success rates of between 70 per cent22 and 75 per cent23 after foam sclerotherapy are lower than those obtained with endothermal technology. Foam sclerotherapy should be questioned as a first-line therapy for refluxing saphenous veins, especially for large veins, as the risk of failure increases when the diameter of the vein is 6 mm or more24,25. In this context, anatomical long-term results of MOCA are still lacking. Similarly, adapted protocols for delivery of endovenous laser with lowered energy doses have to be examined critically. With a reduction in laser energy dose, side-effect profiles can be ameliorated, but anatomical success rates may drop below the standard benchmarks26.
The definition of occlusion in the present study was very restrictive: complete occlusion with absence of any reflux along the treated vein up to 3 cm below the SFJ. Even in 14 of 25 non-occluded veins, the patent part of the GSV was 5 cm or less. In such instances true failure of the treatment is questionable because the distribution of the venous tributaries can influence the final length of the patent GSV27.
Although quality of life was not assessed in the present study, the VCSS and some of its subdomains clearly indicated the achievement of durable clinical success after RFA. Throughout the 5-year follow-up, the VCSS remained significantly improved, with maintenance of low scores. According to the VCSS assessment, presence of varicose veins (component score 1–3) dropped to a minimum of less than 5 per cent at 6-week follow-up, but constantly increased thereafter to 47·4 per cent at 5 years, reflecting the natural course of venous disease. Most dramatically, the VCSS pain domain improved in a durable way; at baseline only 41·4 per cent of the affected legs were free from pain, whereas this proportion stayed above 90 per cent throughout 5-year follow-up.
RFA is an effective and durable treatment for great saphenous varicose veins. Comprehensive follow-up for other methods to 5 years is required to establish the optimal treatment for varicose veins.
Acknowledgments
The study was funded by VNUS and Covidien. The study was designed by the sponsor (Covidien) and physician advisors. Data were monitored, collected and managed by the sponsor. Study sponsors had no influence on patient selection. The data analyses were performed by a professional statistician. Investigators had access to source data and evaluations as requested. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication. T.M.P. and T.N. also received funding from VNUS and Covidien for consultancy and attending conferences.
Disclosure: The authors declare no other conflict of interest.
Supporting Information
Additional supporting information may be found in the online version of this article:
Reflux-free rate after radiofrequency ablation treatment for great saphenous vein reflux (Word document)
Distribution of Venous Clinical Severity Score varicose vein domain values (Word document)
Distribution of Venous Clinical Severity Score oedema domain values (Word document)
Distribution of Venous Clinical Severity Score pain domain values (Word document)
References
- 1.Tran NT, Meissner MH. The epidemiology, pathophysiology, and natural history of chronic venous disease. Semin Vasc Surg. 2002;15:5–12. [PubMed] [Google Scholar]
- 2.Meissner MH. Lower extremity venous anatomy. Sem Interv Radiol. 2005;22:147–156. doi: 10.1055/s-2005-921948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mackay DC, Summerton DJ, Walker AJ. The early morbidity of varicose vein surgery. J R Nav Med Serv. 1995;81:42–46. [PubMed] [Google Scholar]
- 4.Miller GV, Lewis WG, Sainsbury JR, Macdonald RC. Morbidity of varicose vein surgery: auditing the benefit of changing clinical practice. Ann R Coll Surg Engl. 1996;78:345–349. [PMC free article] [PubMed] [Google Scholar]
- 5.Baker DM, Turnbull NB, Pearson JC, Makin GS. How successful is varicose vein surgery? A patient outcome study following varicose vein surgery using the SF-36 Health Assessment Questionnaire. Eur J Vasc Endovasc Surg. 1995;9:299–304. doi: 10.1016/s1078-5884(05)80134-0. [DOI] [PubMed] [Google Scholar]
- 6.Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomized study of endovenous radiofrequency obliteration (closure procedure) versus ligation and stripping in a selected patient population (EVOLVeS Study) J Vasc Surg. 2003;38:207–214. doi: 10.1016/s0741-5214(03)00228-3. [DOI] [PubMed] [Google Scholar]
- 7.Rautio T, Ohinmaa A, Perala J, Ohtonen P, Heikkinen T, Wiik H, et al. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: a randomized controlled trial with comparison of the costs. J Vasc Surg. 2002;35:958–965. doi: 10.1067/mva.2002.123096. [DOI] [PubMed] [Google Scholar]
- 8.Creton D, Pichot O, Sessa C, Proebstle TM. ClosureFast EuropeG. Radiofrequency-powered segmental thermal obliteration carried out with the ClosureFast procedure: results at 1 year. Ann Vasc Surg. 2010;24:360–366. doi: 10.1016/j.avsg.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 9.Proebstle TM, Alm J, Göckeritz O, Wenzel C, Noppeney T, Lebard C, et al. Three-year European follow-up of endovenous radiofrequency-powered segmental thermal ablation of the great saphenous vein with or without treatment of calf varicosities. J Vasc Surg. 2011;54:146–152. doi: 10.1016/j.jvs.2010.12.051. [DOI] [PubMed] [Google Scholar]
- 10.Proebstle TM, Vago B, Alm J, Gockeritz O, Lebard C, Pichot O. Treatment of the incompetent great saphenous vein by endovenous radiofrequency powered segmental thermal ablation: first clinical experience. J Vasc Surg. 2008;47:151–156. doi: 10.1016/j.jvs.2007.08.056. [DOI] [PubMed] [Google Scholar]
- 11.Almeida JI, Kaufman J, Gockeritz O, Chopra P, Evans MT, Hoheim DF, et al. Radiofrequency endovenous ClosureFAST versus laser ablation for the treatment of great saphenous reflux: a multicenter, single-blinded, randomized study (RECOVERY study) J Vasc Interv Radiol. 2009;20:752–759. doi: 10.1016/j.jvir.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Shepherd AC, Gohel MS, Brown LC, Metcalfe MJ, Hamish M, Davies AH. Randomized clinical trial of VNUS ClosureFAST radiofrequency ablation versus laser for varicose veins. Br J Surg. 2010;97:810–818. doi: 10.1002/bjs.7091. [DOI] [PubMed] [Google Scholar]
- 13.Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011;98:1079–1087. doi: 10.1002/bjs.7555. [DOI] [PubMed] [Google Scholar]
- 14.Siribumrungwong B, Noorit P, Wilasrusmee C, Attia J, Thakkinstian A. A systematic review and meta-analysis of randomised controlled trials comparing endovenous ablation and surgical intervention in patients with varicose vein. Eur J Vasc Endovasc Surg. 2012;44:214–223. doi: 10.1016/j.ejvs.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 15.Porter JM, Moneta GL. Reporting standards in venous disease: an update. International Consensus Committee on Chronic Venous Disease. J Vasc Surg. 1995;21:635–645. doi: 10.1016/s0741-5214(95)70195-8. [DOI] [PubMed] [Google Scholar]
- 16.Kistner RL, Eklof B, Masuda EM. Diagnosis of chronic venous disease of the lower extremities: the ‘CEAP’ classification. Mayo Clin Proc. 1996;71:338–345. doi: 10.4065/71.4.338. [DOI] [PubMed] [Google Scholar]
- 17.Rutherford RB, Padberg FT, Jr, Comerota AJ, Kistner RL, Meissner MH, Moneta GL. Venous severity scoring: an adjunct to venous outcome assessment. J Vasc Surg. 2000;31:1307–1312. doi: 10.1067/mva.2000.107094. [DOI] [PubMed] [Google Scholar]
- 18.Passman MA, McLafferty RB, Lentz MF, Nagre SB, Iafrati MD, Bohannon WT, et al. Validation of Venous Clinical Severity Score (VCSS) with other venous severity assessment tools from the American Venous Forum, National Venous Screening Program. J Vasc Surg. 2011;54(Suppl):2S–9S. doi: 10.1016/j.jvs.2011.05.117. [DOI] [PubMed] [Google Scholar]
- 19.De Maeseneer M, Pichot O, Cavezzi A, Earnshaw J, van Rij A, Lurie F, et al. Union Internationale de Phlebologie. Duplex ultrasound investigation of the veins of the lower limbs after treatment for varicose veins – UIP consensus document. Eur J Vasc Endovasc Surg. 2011;42:89–102. doi: 10.1016/j.ejvs.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 20.Pannier F, Rabe E, Maurins U. First results with a new 1470-nm diode laser for endovenous ablation of incompetent saphenous veins. Phlebology. 2009;24:26–30. doi: 10.1258/phleb.2008.008038. [DOI] [PubMed] [Google Scholar]
- 21.van Eekeren RR, Boersma D, Konijn V, de Vries JP, Reijnen MM. Postoperative pain and early quality of life after radiofrequency ablation and mechanochemical endovenous ablation of incompetent great saphenous veins. J Vasc Surg. 2013;57:445–450. doi: 10.1016/j.jvs.2012.07.049. [DOI] [PubMed] [Google Scholar]
- 22.Biemans AA, Kockaert M, Akkersdijk GP, van den Bos RR, de Maeseneer MG, Cuypers P, et al. Comparing endovenous laser ablation, foam sclerotherapy, and conventional surgery for great saphenous varicose veins. J Vasc Surg. 2013;58:727–734.e1. doi: 10.1016/j.jvs.2012.12.074. [DOI] [PubMed] [Google Scholar]
- 23.Devereux N, Recke AL, Westermann L, Recke A, Kahle B. Catheter-directed foam sclerotherapy of great saphenous veins in combination with pre-treatment reduction of the diameter employing the principals of perivenous tumescent local anesthesia. Eur J Vasc Endovasc Surg. 2014;47:187–195. doi: 10.1016/j.ejvs.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 24.Myers KA, Jolley D, Clough A, Kirwan J. Outcome of ultrasound-guided sclerotherapy for varicose veins: medium-term results assessed by ultrasound surveillance. Eur J Vasc Endovasc Surg. 2007;33:116–121. doi: 10.1016/j.ejvs.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Shadid N, Nelemans P, Lawson J, Sommer A. Predictors of recurrence of great saphenous vein reflux following treatment with ultrasound-guided foam sclerotherapy. Phlebology. 2014 doi: 10.1177/0268355514521183. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 26.Vuylsteke ME, Vandekerckhove PJ, De Bo T, Moons P, Mordon S. Use of a new endovenous laser device: results of the 1500 nm laser. Ann Vasc Surg. 2010;24:205–211. doi: 10.1016/j.avsg.2009.06.024. [DOI] [PubMed] [Google Scholar]
- 27.Khilnani NM, Grassi CJ, Kundu S, D'Agostino HR, Khan AA, McGraw JK, et al. Cardiovascular Interventional Radiological Society of Europe, American College of Phlebology, and Society of Interventional Radiology Standards of Practice Committees. Multi-society consensus quality improvement guidelines for the treatment of lower-extremity superficial venous insufficiency with endovenous thermal ablation from the Society of Interventional Radiology, Cardiovascular Interventional Radiological Society of Europe, American College of Phlebology and Canadian Interventional Radiology Association. J Vasc Interv Radiol. 2010;21:14–31. doi: 10.1016/j.jvir.2009.01.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Reflux-free rate after radiofrequency ablation treatment for great saphenous vein reflux (Word document)
Distribution of Venous Clinical Severity Score varicose vein domain values (Word document)
Distribution of Venous Clinical Severity Score oedema domain values (Word document)
Distribution of Venous Clinical Severity Score pain domain values (Word document)


