Abstract
Objective
Interactive voice response systems (IVR) offer great advantages for data collection in large, geographically dispersed samples involving frequent contact. We assessed the quality of IVR data collected from older respondents participating in a statewide falls prevention program evaluation in Pennsylvania in 2010-12.
Method
Participants (n=1834) were followed monthly for up to 10 months to compare respondents who completed all, some, or no assessments in the IVR system. Validity was assessed by examining IVR-reported falls incidence relative to baseline in-person self-report and performance assessment of balance.
Results
While a third of the sample switched from IVR to in-person calls over follow-up, IVR interviews were successfully used to complete 68.1% of completed monthly assessments (10,511/15,430). Switching to in-person interviews was not associated with measures of participant function or cognition. Both self-reported (p < .0001) and performance assessment of balance (p = .05) at baseline were related to falls incidence.
Conclusion
IVR is a productive modality for falls research among older adults. Future research should establish what level of initial personal research contact is optimal for boosting IVR completion rates and what research domains are most appropriate for this kind of contact.
Keywords: interactive voice response, falls, aging, survey quality
Introduction
Interactive Voice Response (IVR) protocols involve automated dialing of respondents, who complete prerecorded questionnaires by pushing telephone buttons or through voice activation. IVR has become popular in research because of its ability to reach large numbers at low cost. However, the quality of data collected from older respondents using these systems is still unclear. To address this gap in research, we used an IVR protocol designed to collect monthly falls information from older adults and asked (i) if older adults who completed follow up by IVR differed from those who switched to in-person telephone follow up, and (ii) if reports of falls elicited by IVR were associated with indicators of falls risk established in in-person assessments.
In 2010-13, we developed a research study, Falls Free PA, to assess the effectiveness of a statewide falls prevention program, Healthy Steps for Older Adults. Healthy Steps is a half-day program offered by the Pennsylvania Department of Aging that involves a combination of screening for balance problems and education about falls risk, along with referral to physicians and home safety assessments (Health Research for Action, 2013; PA Department of Aging 2013).
To assess the effectiveness of Pennsylvania's Healthy Steps program in reducing the incidence of falls, we enrolled a sample of people who completed the program in 2010-11 (n=814), along with a comparison group (n=1018) recruited from the same senior centers at the same time. A full description of the design of the study is available (Albert, Edelstein, King, Lin, Boudreau, & Newman, 2014), as well as results regarding the effectiveness of the program (Albert, King, Boudreau, Prasad, Lin, & Newman, 2014).
Given the relatively large sample, its wide geographical distribution, and the proposed schedule of monthly contact, we invited respondents to complete monthly falls assessments using a telephone interactive voice response system (IVR). We adapted the approach of Wijlhuizen and colleagues (Wijlhuizen, Hopman-Rock, Knook, van der Cammen 2006; Wijlhuizen, Chorus, Hopman-Rock 2010). The system dialed respondent telephone numbers during a defined contact period each month over 10 months; administered a brief human-voice questionnaire on falls, activity, and health care utilization; and logged data and daily completion rates.
While the quality of data collected from older respondents using these systems is still unclear, prior research suggests reliability relative to in-person calls covering the same time period (Albert, et al., 2014a). To assess the quality of IVR data collection, we first examined completion rates for monthly interviews, the proportion switching to in-person telephone interviews during follow-up, and features of older adults that might be associated with switching from the IVR format. Second, we examined the validity of IVR data by comparing the incidence of falls over follow-up, elicited in the IVR interview, relative to risk factors for falls identified in the baseline telephone in-person assessment. These risk factors included self-reported balance and performance on a test of balance and lower extremity strength. High quality according to these indicators would suggest the value of IVR for large health surveys, especially for eliciting recurrent outcomes such as falls.
Methods
Older adults aged 50+ attending PA Department of Aging programs in senior centers and venues offering Healthy Steps (for example, senior residential sites and churches) were eligible to participate in the Falls Free PA program evaluation. Exclusion criteria included inability to provide informed consent, language other than English or Spanish, residence in a skilled nursing facility, and inability to participate in telephone follow-up. The University of Pittsburgh Institutional Review Board approved the research.
Recruitment and Follow-Up of the Falls Free PA Cohort
Falls Free PA enrolled participants in 19 counties through presentations made at venues offering Healthy Steps. Potential respondents were invited to participate in the research, provided contact information, and completed signed informed consent. In total, 74.6% of people contacted (1834/2459) at senior center sites signed consent, completed the baseline assessment, and were eligible for follow-up. Ninety-seven percent (1772/1834) of participants completing the baseline provided one or more monthly follow-up assessments (Albert et al., 2014a).
Identifying Falls: IVR Monthly Telephone Assessments
The research used IVR technology provided by Plum Voice (www.plumvoice.com). The IVR technology uses VoiceXML, which interprets and executes a script generated by a web server. Our IVR System integrated the Plum Voice telephony services with a local web server, locally hosted VoiceXML scripts, and a powerful local database. The interaction between these systems allowed for seamless data collection from the moment the automated phone call was placed (or received) until the call was ended. Call data were instantly stored on the local database and immediately made available to researchers in real time. The IVR system left messages on voicemail if no one answered, which included a telephone number for respondents to initiate the IVR interview call, if they wished.
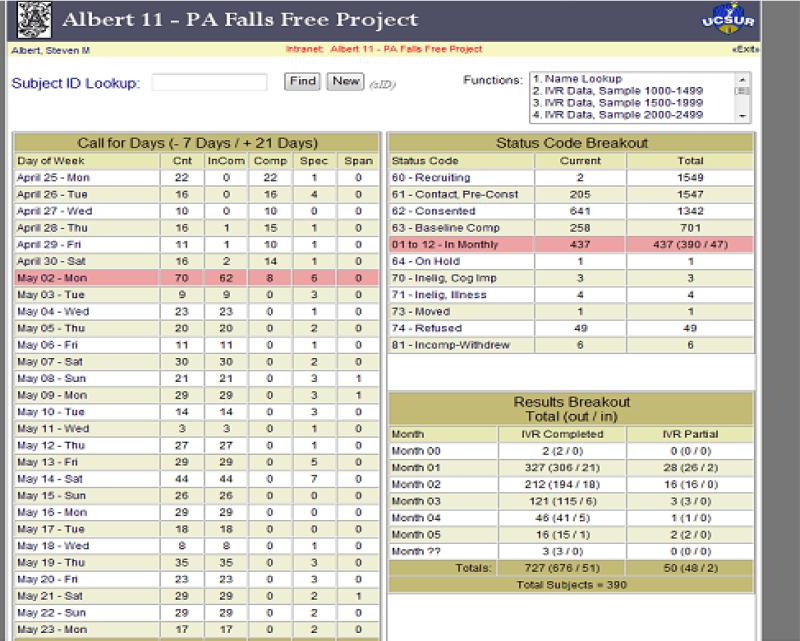
Participants were scheduled for a call each month, every 30 days, beginning 30 days after the baseline interview. The automated system generated two random calls each day (one morning, one evening) for up to 8 days until the person answered and the monthly interview was completed. If a respondent did not complete the follow-up interview in the 8-day window, the follow-up was considered missing and a call was attempted in the next month. Respondents missing IVR calls for two consecutive months were called by research interviewers for an in-person telephone monthly assessment. A screenshot of the system user interface is shown in Figure 1.
Figure 1.
Screenshot from Interactive Voice Recognition System
To ensure that only consented research participants completed the call, the IVR call began with the following message, which inserted the first name of the research participant: “Hello! This is the University of Pittsburgh calling regarding the Falls Free PA research project. We are using an automated system today and I am calling for {FIRST_NAME} who has agreed to participate in a short 5-minute questionnaire. If this is {FIRST_NAME}, press 1. If not press 2.” If someone else answered the telephone, the system allowed the person time to get the respondent or reschedule the call. If no one answered the call, the system left a message and a number that respondents could call to complete the interview.
The IVR call, consisting of six questions, took a mean of 2.5 minutes to complete. To ascertain falls, respondents were asked, “Think about the last 30 days. Did you fall in the last 30 days, that is, end up on the floor or ground because you were unable to stop yourself? Press 1 for yes, 2 for no.” When participants reported a fall, the system generated an email message to the research team, who followed up with an in-person telephone interview to collect information about the fall.
Participants could opt out of the automated IVR system at any point over follow-up by contacting the research team, in which case they were switched to in-person telephone follow-up. In-person telephone calls were reserved from the start for people with hearing impairment, Spanish speakers, people lacking touchtone telephones, people who indicated a preference for in-person contact, or people who interviewers thought might have difficulty with the IVR format. The in-person monthly interview was identical to the IVR interview.
The study began before the IVR system was fully implemented. The first 160 respondents began follow-up with in-person calls and were later switched to the IVR system.
Assessments
Baseline assessments used to examine features of respondents completing or not completing IVR assessments included sociodemographics; health-related quality of life and functional status (EQ-5D; Kind et al., 1998; Shaw et al., 2005); self-rated balance; memory performance (Memory Impairment Screen-Telephone: Buschke et al., 1999; Lipton et al., 2003); and Timed Up and Go, a performance test of balance and lower extremity strength (PA Department on Aging 2007). The Timed Up and Go was only conducted in people attending the Healthy Steps program.
Analyses
Frequencies of monthly interviews were tabulated to identify respondents who completed all, some, or no assessments in the IVR system. Key quality indicators included the proportion of completed interviews by IVR, the proportion of IVR interviews with missing data, and the proportion of respondents switching from IVR to in-person telephone interviews over follow-up.
We could not observe falls and did not have access to hospital admissions or emergency department claims related to falls, ruling out a true test of validity. Instead, we opted for a measure of convergent validity, seeking to determine if reports of falls elicited in the monthly IVR interviews were related to (i) self-reports of balance elicited at baseline, since self-reported balance is a strong predictor of incident falls (Tinetti, Richman, Powell 1990; Rubenstein, Vivrette, Harker, Stevens, Kramer 2013), and (ii) lower extremity strength and balance performance, which are also a strong predictor of falls (Fukagawa, Wolfson, Judge, Whipple, King 1995; Smee, Anson, Waddington, Berry 2012; Karlsson et al., 2012).
Falls were tracked as the number of months in which respondents reported a fall. Incidence was expressed as the number of months with a fall per 100 person-months of follow-up. Differences in incidence rate ratios were compared using Poisson regression models. Analyses were conducted in SPSS (20.0) and SAS (9.3).
Results
Features of the Sample
The majority of Falls Free PA participants was female (79.1%) and white (87.6%), with a mean age of 75.6 (s.d., 8.5) years. While nearly half of the sample reported education after high school, less than 20% had completed college. Participants with (n=1772) and without (n=62) follow-up did not differ in sociodemographic indicators, self-reported health, or falls risk indicators at baseline.
Participation Rate and Quality of IVR Protocol
Over the follow-up period, 10,903 IVR interviews were recorded by the web-based system, in which 10,511 (96.4%) had complete data. IVR interviews were completed by 1434 respondents. Respondents initiated the IVR call (leaving a voicemail message) in 10.1% of interviews. The cohort completed 4919 in-person monthly telephone interviews, which involved 984 people.
Combining the two types of interviews showed that 803 (45.2%) completed all monthly follow-up assessments by IVR, 344 (19.3%) completed all follow-up assessments by in-person calls; and 631 completed follow-up with a mix of the two modalities. As mentioned earlier, 160 participants began the study before the IVR system was introduced and were switched to IVR, and so by design completed interviews with mixed modes. The proportion of respondents beginning with IVR and switching to in-person contact was (631-160)/(1772-344), or 33.0%. These respondents requested the switch to in-person follow-up or required interviewer-initiated calls to complete follow-up. Among people switching out of IVR follow-up, 53% of total assessments were completed by IVR.
All told, the 1834 respondents could have completed a maximum of 10 monthly follow-up interviews, or 18,340 assessments. Between the 10,511 completed in the IVR system and 4919 completed with in-person telephone assessments, 84.1% (15,430/18,340) of potential follow-up assessments were obtained. 68.1% (10,511/15,430) of the follow-up was completed by IVR.
Comparison of Participants Completing Follow-Up by IVR and In-Person Telephone Interviews
As shown in Table 1 (right panel), participants who completed all follow up by IVR and those who switched to in-person telephone follow-up did not differ in any indicator except race-ethnicity. Non-white participants were more likely to switch to in-person telephone follow-up. Switching from the IVR protocol was not associated with any falls risk indicator or poorer functional status, including cognitive status as assessed by the Memory Impairment Screen.
Table 1.
Features of Respondents according to Use of Interactive Voice Response (IVR) System over Follow-Up
| Use of IVR System vs. No Use over Follow-Up, n=1778 | Maintain IVR Follow-Up vs. Switch n=1274 (Excludes n=160 who began study before start of IVR interviews) | |||
|---|---|---|---|---|
| Any IVR over Follow-Up, n=1434 | Only In-Person Follow-Up, n=344 | All Follow-Up by IVR, n=803 | Switch to In-Person Follow-Up, n=471 | |
| Demographics | ||||
| Age, mean (sd) | 74.9 (8.2) | 77.4 (8.9)*** | 75.0 (8.1) | 74.8 (8.5) |
| Female, % | 80.1 | 75.5 | 80.3 | 79.6 |
| Married, % | 36.5 | 26.8*** | 38.0 | 35.9 |
| Non-White, % | 9.6 | 23.5*** | 6.6 | 10.7** |
| College grad, % | 16.8 | 11.7*** | 17.2 | 15.5 |
| Baseline Health Status | ||||
| Mobility disability, % | 36.1 | 44.9*** | 34.4 | 37.8 |
| IADL disability, % | 25.7 | 37.3*** | 24.4 | 26.5 |
| ADL disability, % | 4.7 | 9.9*** | 5.2 | 3.6 |
| Pain, % | 61.2 | 59.1 | 61.8 | 60.1 |
| Anxiety-depression, % | 28.5 | 31.7 | 28.4 | 28.7 |
| Global health, mean (sd) | 80.4 (15.8) | 76.4 (18.3)*** | 80.4 (15.9) | 80.8 (14.9) |
| 3+ Rx meds, % | 62.5 | 50.0*** | 63.5 | 61.0 |
| Memory impairment, % | 7.1 | 19 0*** | 6.1 | 7.9 |
| Fair-poor balance, % | 24.7 | 32.4*** | 24.5 | 24.8 |
p < .01
p < .001 by t-test or X2
Mobility, IADL, ADL, pain, and anxiety-depression symptoms were self-reported using the EQ-5D and indicate “some” or “a lot” of difficulty in the domain. IADL, instrumental activities of daily living; ADL, activities of daily living
By contrast, people who completed all follow up with in-person telephone calls differed from IVR participants in nearly every indicator assessed at baseline. These differences were expected, given that IVR follow-up was not offered to people who interviewers thought might have difficulty with the IVR format.
Convergent Validity of Reported Falls Elicited in IVR Interview
As a measure of validity, we examined the cumulative incidence of people reporting a fall over follow-up in the IVR system. Over 10 months of follow-up, 30.7% reported a fall, very similar to the yearly incidence reported for other cohorts of older adults.
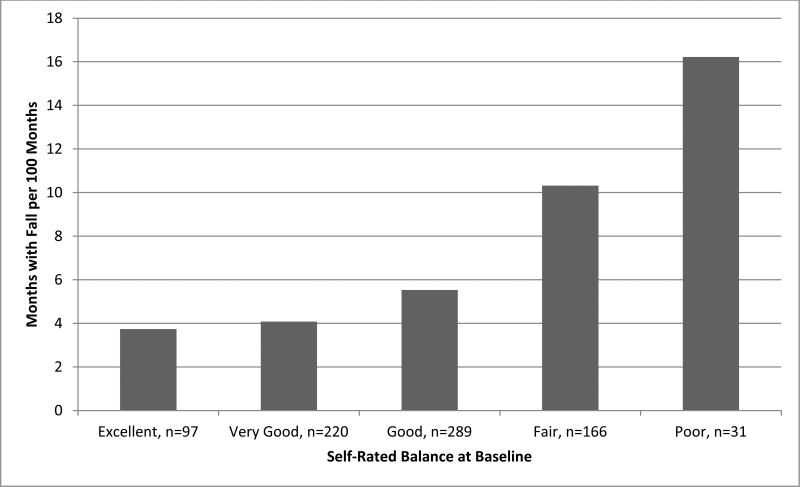
Falls incidence captured in the IVR system was highly associated with baseline self-reported balance. As shown in Figure 2, self-reports of poorer balance at baseline were associated with increased incidence of falls elicited in IVR follow-up. The incidence of falls (measured by number of months with a fall per 100 months of follow-up) ranged from 3.7 among people reporting excellent balance to 16.2 among those reporting poor balance. This difference in incidence rate ratios was highly significant (p < .0001).
Figure 2.
Falls Incidence by Self-Rated Balance at Baseline, IVR Follow-Up
Falls incidence also tracked well with lower extremity performance, as assessed with the Timed Up and Go Test. As shown in Figure 3, participants with the poorest performance experienced 7.3 months with a fall per 100 months of follow-up, compared to a rate of 6.1 in the moderate risk group and 5.3 in the lowest risk group. The difference in incidence rate ratios differed significantly between the lowest and highest risk groups (p= .05).
Figure 3.
Falls Incidence by Performance on Timed Up and Go Task at Baseline
Discussion
This research demonstrates the value of IVR automated telephone calls to collect information on recurrent health outcomes in older respondents. In this statewide sample of nearly 2000 older adults, over two-thirds of monthly assessments were successfully completed using an IVR protocol. While a third of respondents switched to in-person follow-up (either because they requested the switch or because they did not respond to IVR calls), switching from the IVR protocol was not associated with poorer functional status or any falls risk indicator, suggesting that the IVR protocol was no more demanding than personal calls.
Acceptability of the IVR protocol can be seen in the high completion rate (nearly half of respondents completed all follow up by IVR, with little missing data). By contrast, IVR follow up may not be appropriate for more frail older adults. We excluded about 20% of the sample from IVR follow up based on appraisal of their ability to complete the baseline in-person assessment.
Falls incidence based on IVR ascertainment was significantly associated with self-report and performance assessment of balance at baseline. Thus, the IVR protocol demonstrated adequate convergent validity.
IVR protocols have become more common in research because of their convenience and ability to reach large numbers but also because of their advantage for meeting certain research challenges. For example, IVR protocols are useful for collecting information on illicit or stigmatizing behavior (Burge, Becho, Ferrer, Wood, Talamantes, Katerndahl 2014; Piette et al., 2013; Possemato et al., 2012). IVR systems have also been used successfully to deliver health promotion interventions, such as weight loss programs (Steinberg et al., 2014), cancer screening (Cohen-Cline, Wernli, Bradford, Boles-Hall, Grossman 2014; Grearey et al., 2014), and chronic disease management (Heyworth et al., 2014; Piette et al., 2013). The greater reach of IVR contact does not appear to come at the expense of fidelity to standard research measures. For example, IVR assessments demonstrate adequate reliability and construct validity relative to in-person assessments even for complex health-related quality of life (Lundy, Coons, Aaronson 2014; Bjorner, Rose, Gandek, Junghaenel, Ware 2014) and mental health (Turvey, Sheeran, Dindo, Wakefield, Klein 2012) measures.
Consistent with our research, other studies using IVR with older people also report high quality data collection. In these studies older adults completed over 80% of IVR assessments (Piette et al., 2013; Aikens, Zivin, Trivedi, Piette 2014). Older adults report favorable attitudes to IVR interviews even when they have difficulty using such systems (Miller, Aube, Talbot, Gagnon, Messier 2014). Overall compliance with IVR assessment may be higher among older participants than in younger samples and is preferred over Internet follow-up (Verma, et al., 2014).
Limitations of this research include absence of a true criterion measure for assessing the validity of IVR-reported falls. Access to hospital and emergency room information over the same time period would be useful but would only capture more severe injurious falls, not the full experience of falls assessed in the IVR protocol. Use of concurrent monthly falls diaries might be useful, but completion rates for diaries are low. A new and promising modality is use of sensors to detect falls in homes, but we are unaware of studies that have assessed self-reports relative to sensor indicators. Still another approach is to determine if IVR reports of falls track with improvements in balance established in interventional settings. Each of these approaches would shed additional light on the value of IVR for tracking falls in community settings. Adequate assessment of falls may require a combination of such approaches.
This research suggests that IVR is a productive modality for falls research among older adults. Future research should establish what level of initial personal research contact is optimal for boosting IVR completion rates and what research domains are most appropriate for this kind of contact. Likewise, it will be useful to know what features of older adults, such as level of cognitive performance, make IVR approaches less reliable than in-person contact.
Highlights.
Interactive voice response (IVR) calls were used to track falls in older adults.
People completing IVR and switching to in-person follow up were similar.
Falls incidence elicited by IVR was associated with baseline falls risk.
Acknowledgments
Research supported by Cooperative Agreement Number DP002657 from the Centers for Disease Control and Prevention, Prevention Research Centers program, and by NIH AG024827, Pittsburgh Older Americans Independence Center. The findings and conclusions in this presentation are those of the author and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosure
The authors report no conflict of interest.
References
- Aikens JE, Zivin K, Trivedi R, Piette JD. Diabetes self-management support using mHealth and enhanced informal caregiving. J Diabetes Complications. 2014;28:171–176. doi: 10.1016/j.jdiacomp.2013.11.008. doi: 10.1016/j.jdiacomp.2013.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert SM, Edelstein O, King J, Lin CJ, Boudreau R, Newman AB. Assessing the Quality of a Non-randomized Pragmatic Trial for Primary Prevention of Falls among Older Adults. Prevention Science. 2014a doi: 10.1007/s11121-014-0466-2. Epub ahead of print Feb. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert SM, King J, Boudreau R, Prasad T, Lin CJ, Newman AB. Primary Prevention of Falls: Effectiveness of a Statewide Program. Am J Public Health. 2014b;104(5):e77–84. doi: 10.2105/AJPH.2013.301829. doi: 10.2105/AJPH.2013.301829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorner JB, Rose M, Gandek B, Junghaenel DU, Ware JE. Difference in method of administration did not significantly impact item response: An IRT-based analysis from the Patient-Reported Outcomes Measurement Information System (PROMIS) initiative. Qual Life Res. 2014;23:217–27. doi: 10.1007/s11136-013-0451-4. doi: 10.1007/s11136-013-0451-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burge SK, Becho J, Ferrer RL, Wood RC, Talamantes M, Katerndahl DA. Safely examining complex dynamics of intimate partner violence. Family Systems Health. 2014 doi: 10.1037/fsh0000013. EPub ahead of print June 9. [DOI] [PubMed] [Google Scholar]
- Buschke H, Kuslansky G, Katz M, Stewart WF, Sliwinski MJ, Eckholdt HM, Lipton RB. Screening for dementia with the Memory Impairment Screen. Neurology. 1999;52:231–238. doi: 10.1212/wnl.52.2.231. [DOI] [PubMed] [Google Scholar]
- Cohen-Cline H, Wernli KJ, Bradford SC, Boles-Hall M, Grossman DC. Use of interactive voice response to improve colorectal cancer screening. Med Care. 2014;52:496–499. doi: 10.1097/MLR.0000000000000116. doi: 10.1097/MLR.0000000000000116. [DOI] [PubMed] [Google Scholar]
- D'Arcy S, Rapcan V, Gali A, Burke N, O'Connell GC, Robertson IH, Reilly RB. A study into the automation of cognitive assessment tasks or delivery via the telephone: Lessons for developing remote monitoring applications for the elderly. Technol Health Care. 2013;21:387–396. doi: 10.3233/THC-130740. doi: 10.3233/THC-130740. [DOI] [PubMed] [Google Scholar]
- Fukagawa NK, Wolfson L, Judge J, Whipple R, King M. Strength Is a Major Factor in Balance, Gait, and the Occurrence of Falls. J Gerontol A Biol Sci Med Sci. 1995;50A(Special Issue):64–67. doi: 10.1093/gerona/50a.special_issue.64. doi:10.1093/gerona/50A.Special_Issue.6. [DOI] [PubMed] [Google Scholar]
- Grearey ML, De Jesus M, Sprunck-Harrild KM, Tellez T, Bastani R, Battaglia TA, Michelson JS, Emmons KM. Designing audience-centered interactive voice response messages to promote cancer screening among low-income Latinas. Prev Chronic Dis. 2014;11:e40. doi: 10.5888/pcd11.130213. doi: 10.5888/pcd11.130213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyworth L, Kleinman K, Oddeifson S, Bernstein L, Frampton J, Lehrer M, Salvato K, Weiss TW, Simon SR, Connelly M. Comparison of interactive voice response, patient mailing, and mailed registry to encourage screening for osteoporosis: A randomized controlled trial. Osteoporosis Int. 2014;25:1519–1526. doi: 10.1007/s00198-014-2629-1. doi: 10.1007/s00198-014-2629-1. [DOI] [PubMed] [Google Scholar]
- Karlsson MK, Ribom E, Nilsson JÅ, Ljunggren Ö , Ohlsson C, Mellström D, Lorentzon M, Mallmin H, Stefanick M, Lapidus J, Leung PC, Kwok A, Barrett-Connor E, Orwoll E, Rosengren BE. Inferior physical performance tests in 10,998 men in the MrOS study is associated with recurrent falls. Age Ageing. 2012 Nov;41(6):740–6. doi: 10.1093/ageing/afs104. doi: 10.1093/ageing/afs104. Epub 2012 Aug 24. doi: 10.1093/ageing/afs104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ. 1998;316:736–741. doi: 10.1136/bmj.316.7133.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipton RB, Katz MJ, Kuslansky G, Sliwinski MJ, Stewart WF, Verghese J, Crystal HA, Buschke H. Screening for Dementia by Telephone Using the Memory Impairment Screen. J Am Geriatr Soc. 2003;51:1382–1390. doi: 10.1046/j.1532-5415.2003.51455.x. [DOI] [PubMed] [Google Scholar]
- Lundy JJ, Coons SJ, Aaronson NK. Test-retest reliability of an interactive voice response (IVR) version of the EORTC QLC-C30. Patient. 2014 doi: 10.1007/s40271-014-0071-2. EPub ahead of print June 24. [DOI] [PubMed] [Google Scholar]
- Miller DI, Aube F, Talbot V, Gagnon M, Messier C. Older people's attitudes toward interactive voice response systems. Telemed J E Health. 2014;20:152–156. doi: 10.1089/tmj.2013.0028. doi: 10.1089/tmj.2013.0028. [DOI] [PubMed] [Google Scholar]
- PA Department of Aging . Train-the-Trainer Session for Healthy Steps for Older Adults. Dering Consulting Group; 2007. [Google Scholar]
- Piette JD, Aikens JE, Trivedi R, Parrish D, Standiford C, Marinec NS, Striplin D, Bernstein SJ. Depression self-management assistance using automated telephonic assessments and social support. Am J Managed Care. 2013;19:892–900. [PubMed] [Google Scholar]
- Piette JD, Rosland AM, Marinec NS, Striplin D, Bernstein SJ, Silveira MJ. Engagement with automated patient monitoring and self-management support calls: Experience with a thousand chronically ill patients. Med Care. 2013;51:216–223. doi: 10.1097/MLR.0b013e318277ebf8. doi: 10.1097/MLR.0b013e318277ebf8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Possemato K, Kaier E, Wade M, Lantinga LJ, Maisto SA, Ouimette P. Assessing daily fluctuations in posttraumatic stress disorder symptoms and substance use with Interactive Voice Response technology: Protocol compliance and reactions. Psychol Serv. 2012;9:185–96. doi: 10.1037/a0027144. doi: 10.1037/a0027144. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Vivrette R, Harker JO, Stevens JA, Kramer BJ. Validating an evidence-based, self-rated fall risk questionnaire (FRQ) for older adults. J Safety Res. 2011 Dec;42(6):493–9. doi: 10.1016/j.jsr.2011.08.006. doi: 10.1016/j.jsr.2011.08.006. Epub 2011 Nov 17. [DOI] [PubMed] [Google Scholar]
- Smee DJ, Anson JM, Waddington GS, Berry HL. Association between Physical Functionality and Falls Risk in Community-Living Older Adults. Curr Gerontol Geriatr Res. 2012;2012:864516. doi: 10.1155/2012/864516. doi: 10.1155/2012/864516. Epub 2012 Dec 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg DM, Levine EL, Lane I, Askew S, Foley PB, Puleo E, Bennett GG. Adherence to self-monitoring via interactive voice response technology in a eHealth intervention targeting weight gain prevention among Black women: Randomized controlled trial. J Med Internet Res. 2014;16:e114. doi: 10.2196/jmir.2996. Doi 10.2196/jmir.2996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. Journal of Gerontology. 1990;45:239–243. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- Turvey C, Sheeran T, Dindo L, Wakefield B, Klein D. Validity of the Patient Health Questionnaire, PHQ-9, administered through interactive-voice response technology. J Telemed Telecare. 2012;18:348–351. doi: 10.1258/jtt.2012.120220. doi: 10.1258/jtt.2012.120220. [DOI] [PubMed] [Google Scholar]
- Verma SK, Courtney TK, Lombardi DA, Chang WR, Huang YH, Brennan MJ, Perry MJ. Internet and telephonic IVR mixed-mode survey for longitudinal studies: Choice, retention, and data equivalency. Ann Epidemiol. 2014;24:72–74. doi: 10.1016/j.annepidem.2013.10.004. doi: 10.1016/j.annepidem.2013.10.004. [DOI] [PubMed] [Google Scholar]
- Wijlhuizen GJ, Chorus AMJ, Hopman-Rock M. The FARE: A new way to express falls risk among older persons including physical activity as a measure of exposure. Prev Med. 2010;50:143–147. doi: 10.1016/j.ypmed.2009.12.014. doi: 10.1016/j.ypmed.2009. [DOI] [PubMed] [Google Scholar]
- Wijlhuizen GJ, Hopman-Rock M, Knook DL, van der Cammen TJ. Automatic registration of falls and other accidents among community-dwelling older people: Feasibility and reliability of the telephone inquiry system. Int J Inj Contr Saf Promot. 2006;13:58–60. doi: 10.1080/15660970500036937. [DOI] [PubMed] [Google Scholar]