Abstract
Objective
Approximately 50% of Child Protective Service (CPS) referrals abuse drugs; yet, existing treatment studies in this population have been limited to case examinations. Therefore, a family-based behavioral therapy was evaluated in mothers referred from CPS for child neglect and drug abuse utilizing a controlled experimental design.
Method
72 mothers evidencing drug abuse or dependence and child neglect were randomly assigned to Family Behavior Therapy (FBT) or Treatment as Usual (TAU). Participants were assessed at baseline, 6- month-, and 10-month post-randomization.
Results
As hypothesized, intent-to-treat repeated measures analyses revealed mothers referred for child neglect not due to their children being exposed to illicit drugs demonstrated better outcomes in child maltreatment potential from baseline to 6- and 10-month post-randomization assessments when assigned to FBT, as compared with TAU mothers and FBT mothers who were referred due to child drug exposure. Similar results occurred for hard drug use from baseline to 6- and 10-month post-randomization. However, TAU mothers referred due to child drug exposure were also found to decrease their hard drug use more than TAU mothers of non-drug exposed children and FBT mothers of drug exposed children at 6- and 10-month post-randomization. Although effect sizes for mothers assigned to FBT were slightly larger for marijuana use than TAU (medium vs. large), these differences were not statistically significant. Specific to secondary outcomes, mothers in FBT, relative to TAU, increased time employed from baseline to 6- and 10-month post-randomization. Mothers in FBT, compared to TAU, also decreased HIV risk from baseline to 6-month post-randomization. There were no differences in outcome between FBT and TAU for number of days children were in CPS custody and alcohol intoxication, although FBT mothers demonstrated marginal decreases (p = .058) in incarceration from baseline to 6-month post-randomization relative to TAU mothers.
Conclusion
Family-based behavioral treatment programs offer promise in mothers who have been reported to CPS for concurrent substance abuse and child neglect of their children. However, continued intervention development in this population is very much needed.
Keywords: Drug Abuse, Child Neglect, Family Behavior Therapy, Outcome Study
More than 8 million children in the United States have at least one parent who abuses substances (Dunn et al., 2002), with the percentage of women evidencing severe levels of illicit drug abuse increasing relative to men (Dunn, Tarter, Mezzick, Vanyukok, Kirisci, & Kirillova, 2002). These changes have contributed to substantial problems within the family (Ells, 2002; Wells, 2009) as mothers who abuse substances are more likely than non-substance abusing mothers to evidence significant problems raising their children, experience separation from intimate partners, experience unemployment or underemployment (Carlson et al., 2012; Jones, 2008), experience conflict (Semidei, Radel, & Nolan, 2001), and report insecurity in home life (Brown & Hohman, 2008). Similarly, compared to children whose parents do not use substances, children of parents who use substances more often experience parental behaviors that are consistent with neglect, such as being unsupervised (Ells et al., 2002), exposure to dangerous environments, and remaining in foster home placements for extended time periods (Carlson et al., 2012).
Drug abuse is one of the chief factors influencing the development and maintenance of child maltreatment (Davis, 1990; Jones, 2008), with approximately 50 to70% of maltreated children estimated to have mothers who abuse illicit substances (Jones, 2005). Hard drug use is especially influential in the development of child neglect due to its contribution to unsafe environmental conditions (Wang & Harding, 1999). For instance, Brown and Hohman (2008) found methamphetamine use in parents was associated with unchanged diapers, dirty housing, and being without food or formula for children. Thirty eight percent of children with parents who were found to abuse cocaine experienced some form of child maltreatment in their first year of life (Wasserman & Levanthal, 1993). Sowder and Burt (1980) found 42% of three to seven year-olds born to individuals who abuse heroin suffered from mental retardation or severe emotional problems. Although it appears that marijuana use in parents may be less harmful than hard drug use (Dunn et al., 2002), poor supervision and negative health consequences due to marijuana exposure have also been identified in children (Amirav, Luder, Viner & Finkel, 2011; Appelboem & Oades, 2006; Wells, 2009).
Child neglect is the most common form of child maltreatment, and is responsible for approximately three quarters of all referrals to child protective service agencies (U.S. Department of Health and Human Services, 2010). Child neglect is the least likely type of child maltreatment to be substantiated (U.S. Department of Health and Human Services, 2003), and is relatively dangerous (Garbarino & Collins, 1999) and understudied (Erickson & Egeland, 2002). Caseworkers in child welfare protection systems have historically considered child neglect when the needs of children are insufficiently addressed, such as poor supervision, inadequate medical intervention, unsafe living environment, or lack of emotional, physical and educational care. After the Keeping Children and Families Safe Act was passed in 2003, most child welfare agencies initiated additional policies mandating health care providers to notify child protective services when infants were exposed to drugs in utero or directly affected by their parents’ illicit drug abuse. Underscoring the tension between autonomy and child protection, drug use exposure of children occurring during pregnancy (Lambert, Scheiner, & Campell, 2010; Ondersma, Halinka Malcoeb, & Simpson, 2001) and childhood (Pennar, Shapiro, & Krysik, 2011) appears to be a unique form of child neglect warranting a distinct set of consequences and intervention.
Family systems oriented behavioral therapies examined in the few randomized controlled trials that have been conducted have consistently demonstrated improved outcomes in parents referred for child physical abuse (Chaffin et al., 2004; Kolko, 1996; Swenson, Schaeffer, Henggeler, Faldowski, & Mayhew, 2010). However, treatment of child neglect is far less studied (Behl, Conyngham, & May, 2003; Chaffin, 2006). Child neglect shares many of the same antecedents as child physical abuse, but manifests itself more pervasively, leading it to be particularly dangerous (Garbarino & Collins, 1999) and difficult to treat with prescribed interventions. The pioneering contributions of John Lutzker and his colleagues in developing a comprehensive “Eco-behavioral” treatment approach for child neglect is notable (Lutzker, Wesch, & Rice, 1984). In a series of case trials, these investigators demonstrated that the implementation of behavioral interventions in the environment for which child neglect occurs facilitates development of skill sets that are incompatible with child neglect, such as personal hygiene and dental care in children, home cleanliness (Lutzker, Campbell, & Watson-Perczel, 1984), decreased home hazards (Barone, Greene, & Luzker, 1986; Watson-Perczel, Lutzker, Greene, & McGimpsey, 1988), and improved affective responses of mothers to their infants (Lutzker, Lutzker, Braunling-McMorrow, & Eddleman, 1987). SafeCare (SC; Lutzker & Edwards, 2009) has perhaps received greatest investigative attention in child neglect treatment. In this approach, home visitors teach home safety, child health, and positive parent-child/infant interaction. SC involves structured problem solving skills training exercises that are similar to the individually-based problem-solving methods developed by Dawson, de Arrnas, McGrath, and Kelly (1986) in child neglect referrals. SC was favorably evaluated in a recent highly controlled randomized clinical trial involving general referrals from child protective services (Chaffin, Hecht, Bard, Silovsky, & Beasley, 2012).
Multisystemic Therapy (MST; Henggeler, 1982) is similar to SC in its utilization of multi-component family-based interventions. Brunk, Henggeler, and Whelan (1987) conducted the first randomized controlled outcome study examining parents explicitly identified for child neglect (18 families referred for child physical abuse, 15 families referred for child neglect). Participants were randomly assigned to receive Multisytemic Therapy (MST) emphasizing strategies to manage the conduct of children, relationship enhancement, and family advocacy, or a parent training program that did not include behavioral rehearsal. Results of parent self-report inventories demonstrated that both interventions improved global psychiatric functioning and overall stress. Parents who received parent training reported greater reductions in social problems (e.g., child's problems in school, conflicts with neighbors, unemployment) than parents who received MST, and MST significantly enhanced parent-child interactions compared with parents who received parent training. Thus, results were positive for this earlier version of MST, and this study yielded findings that were consistent with other studies that have demonstrated the merits of parent training in child maltreatment.
The results of a controlled trial conducted by Chaffin and colleagues (2004) suggest behavioral rehearsal is especially warranted when implementing parenting skills training in child maltreatment. Their study involving participants evidencing child physical abuse, demonstrated that a behavioral rehearsal-based parent training program (Parent Child Interaction Therapy; PCIT) was more effective in reducing child physical abuse than a standardized didactic parenting training approach offered within the community context. Interestingly, child neglect reports were indicated at baseline as frequently as child physical abuse reports. No significant differences in re-reports of child neglect reports were found between the experimental interventions. The investigators reported that the latter finding was potentially due to the exclusion of neglect-specific components in PCIT.
Several controlled treatment outcome studies have demonstrated benefits for social skill interventions in neglected and abused children (Davis & Fantuzzo, 1989; Fantuzzo et al., 1988; Fantuzzo, Stovall, Schazhel, Goins, & Hall, 1987), and neglecting mothers (Gaudin, Wodarski, Arkinson, & Avery, 1991). Thus, the aforementioned literature indicates substance abuse occurs at a high rate in child protective service referrals and is a complicating factor when implementing interventions for child maltreatment. Additionally, in treating child neglect, comprehensive behavioral interventions (e.g., SafeCare, MST) that involve parents and include skill-based interventions (i.e., parent training, problem solving, child safety interventions, communication skills training) appear to be relatively effective in child maltreatment samples, although these programs have not addressed concurrent substance abuse.
Approximately two decades ago, investigators first emphasized the need to empirically develop behavioral treatments to concurrently address child neglect and substance abuse (e.g., Blau, 1994; Corcoran, 2000). Unfortunately, lack of integration between child welfare services and substance abuse treatment providers has restricted the development of evidence-based programming for this group (Young, Boles, & Otero, 2007). This is a significant problem (Conners, Bradley, Whiteside-Mansell, & Crone, 2001) as substance abuse programs are rarely equipped to manage child maltreatment, and persons afflicted with substance abuse are often excluded from programs specializing in the treatment of child maltreatment (see review by Donohue, Romero, & Hill, 2006). As summarized by Silovsky et al. (2011), prevention programs for child maltreatment are weak in high risk populations, such as substance abuse. To date, there have been no controlled treatment outcome studies targeting concurrent child maltreatment and drug abuse, although drug abuse treatments for mothers have indicated that child outcomes are improved when treatments are comprehensive (Niccols, Milligan, Smith, Sword, Thabane, & Henderson, 2012). Several case trials have examined the effects of Family Behavior Therapy (FBT; Donohue & Allen, 2011; Donohue & Azrin, 2012) in mothers who have been reported to Child Protective Services for child neglect and drug abuse. These case trials have demonstrated noticeable improvements in various undesired behaviors, including child abuse potential, illicit drug and alcohol use, family relationships, stress, domestic violence, and HIV risk behaviors (Donohue et al., 2010; LaPota, Donohue, Warren, & Allen, 2011; Romero, Donohue, & Allen, 2010; Romero et al., 2010). The integration of HIV prevention components in FBT is noteworthy given the high risk of HIV and AIDS in this population (see Nijhawan, Kim, & Rich, 2008).
As a methodological extension of these case studies, the proposed investigation was performed to examine the effects of FBT as compared to treatment as usual community-based services (TAU) in a randomized clinical trial. It was hypothesized that FBT would be more effective than TAU in measures consistent with the primary reason for referral (child maltreatment potential, illicit drug use), as well as secondary comorbid problem behaviors (HIV risk behavior, alcohol intoxication, unemployment, incarceration, days child victim in Department of Family Services custody). It was further hypothesized that FBT, as compared with TAU, would be particularly effective in mothers who had neglected their children for reasons other than exposure of the child victim to illicit drugs. The latter hypothesis is based on the assumption that mothers of children who have been exposed to drugs evidence characteristics and circumstances that may be inherently unique to mothers who have neglected their children for other reasons (Lambert et al., 2010; Ondersma et al., 2001; Pennar et al., 2011).
This controlled study represents a significant methodological advancement in the treatment of concurrent child neglect and drug abuse, including utilization of psychometrically validated interviews to assist in the diagnosis of participants’ substance disorders (substance abuse and dependence), inclusion of urinalysis testing to complement self-reports of substance use, formal assessment of treatment integrity, use of protocol checklists to assist in the implementation of interventions, assessment of treatment outcomes by blind technicians, and intent to treat management of missing data.
Method
Participants
Participants were 72 mothers referred for treatment of substance abuse and child neglect by the County's Department of Family Services (DFS). Study inclusion criteria were: (a) mother reported to DFS for child neglect; (b) mother living with the child victim responsible for neglect referral (or it was the intention of the Court to return the child to the mother's home upon treatment assignment); (c) identified to use illicit drugs during the 4 months prior to referral; (d) displaying symptoms consistent with illicit Drug Abuse or Dependence at the time of referral according to the results of the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Health Disorders (SCID; First, Spitzer, Gibbon, & Williams, 1996), (e) at least one adult individual willing to participate in the mother's treatment; and (f) primary reason for referral not due to sexual abuse perpetration or domestic violence. Participant demographic characteristics are presented in Table 1.
Table 1.
Demographic Characteristics of the Mothers with Numbers Shown as Frequency (%)
| Characteristic | Total (n = 72) | FBT (n = 35) | TAU (n = 37) |
|---|---|---|---|
| Age of Mother | 29.04 (8.07) | 29.63 (7.65) | 28.49 (8.51) |
| Age of Mother's Child | 3.92 (3.73) | 4.20 (4.06) | 3.65 (3.42) |
| Race | |||
| Caucasian | 34 (47.2) | 14 (40.0) | 20 (54.1) |
| Black/African American | 18 (25.0) | 10 (28.6) | 8 (21.6) |
| Hispanic/Latino | 8 (11.1) | 6 (17.1) | 2 (5.4) |
| American Indian | 3 (4.2) | 2 (5.7) | 1 (2.7) |
| Asian American | 2 (2.8) | 2 (5.7) | 0 (0.0) |
| Pacific Islander | 2 (2.8) | 1 (2.9) | 1 (2.7) |
| Other | 5 (6.9) | 0 (0.0) | 5 (13.5) |
| Marital status | |||
| Single | 33 (45.8) | 14 (40.0) | 19 (51.4) |
| Married | 14 (19.4) | 6 (17.1) | 8 (21.6) |
| Cohabitating | 25 (34.7) | 15 (42.9) | 10 (27.0) |
| Employment status | |||
| Unemployed | 63 (87.5) | 28 (80.0) | 35 (94.6) |
| Employed full time | 5 (6.9) | 3 (8.6) | 2 (5.4) |
| Employed part time | 4 (5.6) | 4 (11.4) | 0 (0.0) |
| Education | |||
| Less than high school | 36 (50.0) | 19 (54.3) | 17 (45.9) |
| High school/equivalent | 32 (44.4) | 15 (42.9) | 17 (45.9) |
| A.S./B.A./B.S. | 4 (5.6) | 1 (2.9) | 3 (8.1) |
Note. A.S. = Associate of Arts degree; B.A. = Bachelor of Arts degree; B.S. = Bachelor of Science degree
The study was approved by the appropriate institutional review board, and a federal certificate of confidentiality was obtained prior to initiating the trial. No adverse events were determined to be due to the study.
Experimental Design
A 2 (treatment type: FBT, TAU) × 2 (neglect type: neglect due to fetus/child being exposed to drugs, other child neglect) × 3 (time [assessment]: baseline, 6-month post randomization, 10-month post-randomization) mixed model experimental design with random assignment of participants to intervention conditions was utilized.
Procedure
Method of recruitment
DFS offices were informed of the study and its inclusionary criteria through email and on site presentations. Referrals were made by DFS caseworkers through telephone or fax. Upon DFS referral, an intake specialist contacted the caseworker, and separately the participant, by telephone to determine if inclusionary criteria were met. Qualifying participants were scheduled to obtain informed consent and complete the pre-treatment baseline assessment (drug abuse or dependence substantiated during baseline assessment).
Method of randomizing participants into experimental conditions
Consenting participants completed the baseline assessment specific to the reason for referral, including outcome measures and demographic and background information. The pre-treatment assessment was utilized to substantiate inclusionary criteria and establish baseline data. Upon completion of baseline assessment participants were assigned to treatment (either FBT or TAU) utilizing urn randomization to assist in maintaining treatment group equivalence in demographic and primary outcome measures (Waldron et al., 2001).
Method of collecting data
Baseline, 6-month post-randomization, and 10-month post-randomization assessments were administered in the participants’ homes by trained assessors from a neuropsychology clinic that operated independently from the treatment program. Assessors were not informed of the participants’ intervention assignment by study staff. Participants were compensated for their time with a $50 gift card for use at local store for the pre-treatment assessment, $100 for the 6-month post-randomization assessment, $100 for the 10-month post-randomization assessment, and $50 bonus if they completed both post-randomization assessments.
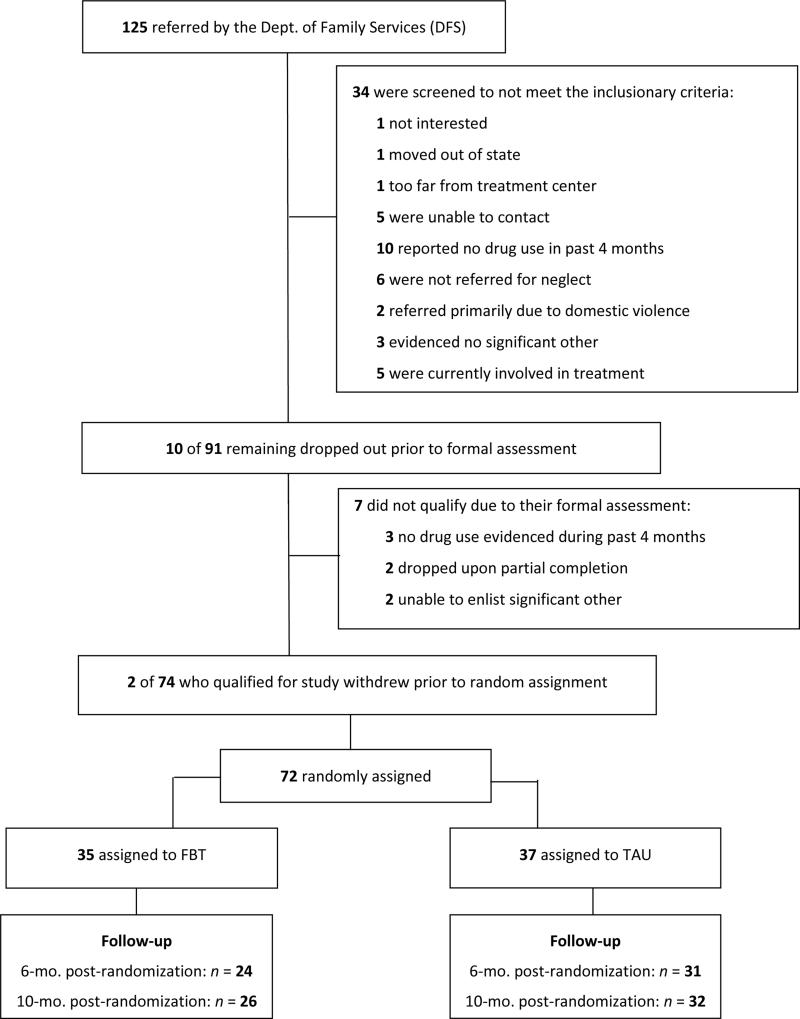
Method of retaining participants in the study
Figure 1 depicts how participants entered and were retained or exited from the study. All 72 of the qualifying participants who were interested in participating in the study were randomly assigned to treatment (35 FBT, 37 TAU) and included in the intent to treat study analyses. Seventy-four percent of participants were retained through both the 6-month and 10-month post-randomization assessments. Overall follow-up rates were 76.4% (N = 55) for 6-month post-randomization, and 80.5% (N = 58) for 10-month post-randomization assessment.
Figure 1.
Flow Chart of Participant Entry and Exit
Treatment Conditions
Family Behavior Therapy (FBT)
The experimental condition that was examined in this study was adapted from Family Behavior Therapy, which is a comprehensive outpatient substance abuse treatment (Donohue & Allen, 2011; Donohue & Azrin, 2012). In this intervention model, substance use is conceptualized as a primary reinforcer influenced by modeling, encouragement and physiological prompts, insufficient reinforcement for non-drug activities, and remoteness and uncertainty of the negative consequences of substance use. Standardized engagement procedures are used to involve family and friends of participants in treatment to support goal accomplishment (e.g., attendance, providing insightful comments, goal development and assistance, modeling pro-social behavior, assisting in child care, completion of therapeutic assignments). FBT emphasizes cognitive and behavioral skill development through behavioral role-playing, therapeutic assignments, and utilization of family support systems. Multiple intervention components are implemented sequentially and cumulatively, and include the following: (1) contingency management to assist significant others in providing family-derived rewards for pro-social target behaviors (e.g., child management) that are incompatible with substance use; (2) communication skills training to improve family relationships through expressions of appreciation and positive requests (e.g., succinct, polite directives, offers to help facilitate desired actions, offering alternatives), thereby making it reinforcing to engage in non-drug associated activities; (3) stimulus control interventions to assist family members in spending less time with individuals (and in situations) that involve substance use and other problem behaviors, and more time with individuals (and in situations) that have not involved substance use and other problem behaviors. Of course, family members are assisted in thinking and behaving in ways that promote the elimination and management of antecedent conditions that lead to substance use and problematic behaviors and enhance goal-oriented outcomes; (4) a self-control method to manage drug cravings in which participants are taught to sequentially practice a series of therapeutic thoughts and actions during imaginal practice trials (i.e., imagining early recognition of antecedents to respective problem behaviors, thought stopping to terminate urges or desires to engage in substance use or impulsive problem behavior, reviewing negative consequences of problem behavior to enhance motivation to engage in thoughts and behaviors that are consistent with goal-oriented behavior, diaphragmatic breathing to reduce stress and enhance focus on goal-oriented behavior, brainstorming potential alternatives to problematic behavior and thoughts, imagining successful implementation of chosen alternatives to problematic behavior and thoughts, imagining the receipt of rewards for having chosen to perform goal-oriented behaviors and thoughts); (5) skills training specific to attaining employment through systematic solicitation and behavioral practice regarding job interviews. These intervention components have collectively led to improvements in drug and alcohol abstinence, family functioning/satisfaction, days attending school and work, mood, and conduct in controlled trials with adults and adolescents (Azrin, Acierno et al., 1996; Azrin, Donohue et al., 2001; Azrin, Donohue et al., 1994; Azrin, McMahon et al., 1994; Donohue, Azrin et al., 1998).
In this current study, FBT was adapted to accommodate the unique needs of families referred to treatment for substance abuse by child protective services. Mothers and their families were seen in their homes rather than offices of service providers, treatment sessions were increased from 60 minutes to 75 minutes, the duration of treatment was extended from 4 months to 6 months, the target number of treatment sessions was extended from 15 sessions to 20 sessions, and several intervention components were incorporated. These intervention components included (1) teaching family members to identify home hazards and generate their own strategies to making their homes safer and more stimulating for children during tours of the home; (2) improving financial management skills of mothers by reviewing sources of income and expenses, and brainstorming methods of increasing income and decreasing expenses utilizing financial management worksheets to reduce stress that often triggers substance use and neglectful behavior through distraction, irritability and avoidance of educational and caretaking responsibilities; (3) teaching mothers to differentially reinforce their children for desired behaviors while ignoring undesired behaviors (Forehand & McMahon, 1981), and to discipline undesired behaviors of children by first explaining how environmental circumstances may have led to the undesired behavior and then instructing them to practice desired behaviors several times (Azrin & Besalel-Azrin, 1980); (4) teaching mothers to react to emergent conditions that affect their families (e.g., lack of food) with the aforementioned self-control method (emergency management; Urgelles, Donohue, Wilks, Van Hasselt, & Azrin, 2012); and (5) HIV and STD prevention utilizing the aforementioned stimulus control procedures to teach mothers to recognize and effectively manage antecedents to sexually transmitted diseases (e.g., unprotected sex, intravenous drug use, promiscuity, prostitution), self-control and communication skills training to encourage assertion in requesting safe sexual activity or refusal of substance use that involve needles. This modified FBT has demonstrated preliminary efficacy in controlled and uncontrolled case trials specific to coexisting child neglect and drug abuse in home-based settings (Donohue, Romero et al., 2010; Donohue & Azrin, 2002; LaPota, Donohue, Warren, & Allen, 2011; Romero, Donohue, & Allen, 2010; Romero, Donohue et al., 2010).
Treatment as Usual (TAU)
By including a TAU comparison condition, this study was designed to examine the public health question of whether the FBT model is more effective than standard agency services in reducing maternal drug use and neglect (Swenson, Schaeffer, Henggeler, Faldowski, & Mayhew, 2010). TAU was selected because it permitted the drawing of definitive conclusions by controlling extra-treatment variables associated with the passage of time (e.g., changes in child development, parenting experience, education), and facilitated a controlled evaluation of services that are typically provided in child protective service contexts. TAU reflected a variety of services that vary according to provider qualifications, duration, intensity, and type of services offered, thus reflecting “best available options” during the designated 6-month treatment dose (Galloway et al., 2000). As customarily performed in outcome research involving drug abuse (Henggeler et al., 2002) and child maltreatment (Chaffin et al., 2004), no attempt was made to standardize or monitor fidelity of TAU to permit a valid comparison of the proposed experimental condition to “real world” service configurations that are routinely delivered (Rawson et al., 2004). There was no standard referral system, as caseworkers referred to various services according to their assessment of family needs and motivation, problem severity, availability of services, and relationship of caseworker with referral agencies. TAU services were consistent with referrals made by Child Protective Service agencies, including child placement (e.g., shelters), crisis intervention services, family services (e.g., family therapy, housing, legal services), caregiver services (e.g., individual counseling, marital counseling, inpatient and outpatient substance abuse counseling), child services (e.g., individual and group therapy), and other “miscellaneous” services (Kolko, Selelyo, & Brown, 1999).
Intervention Fidelity of FBT Providers
Eleven providers participated in the study. Two treatment providers were scheduled to implement FBT components during each home-based session. Prior to this study, the providers had no experience implementing FBT, and their professional experience varied (i.e., bachelor's level community treatment providers, master's and doctoral graduate students, post-doctoral fellow). FBT providers received approximately 16 hours of formal FBT training in workshop format utilizing behavioral role-playing prior to intervention implementation. After participating in the workshop treatment providers were required to demonstrate a minimum of 70% protocol adherence in each of the FBT intervention components with a referred pilot case from CPS prior to being permitted to counsel cases in this randomized controlled trial. Providers attended 90 to 120 minutes of weekly group supervision throughout the study. Group supervision focused on reviewing family safety, treatment planning, and maintenance of intervention adherence. Strategies were employed to ensure the integrity of treatment (Azrin, Donohue et al., 2001; Yeaton & Sechrest, 1981), including utilization of intervention manuals with protocol checklists, written documentation by the therapist of techniques used during sessions utilizing standardized forms, audio taping of sessions, ongoing clinical supervision of treatment sessions, corrective feedback to therapists, and utilization of detailed prompting lists by providers that indicated the specific tasks to be completed. Reliability and validity estimates of treatment integrity were derived from completed protocol checklists (see Intervention Fidelity in the Results section). Reliability and validity for the latter method was demonstrated in an effectiveness trial of Multisystemic Therapy involving community providers (Sheidow et al., 2008), and this method of adherence assessment and training has been successfully utilized in previous controlled trials involving FBT (Azrin, Acierno et al., 1996; Azrin, Donohue et al., 1994; Azrin, Donohue et al., 2001; Azrin, McMahon et al., 1996), including a demonstration of its acceptable reliability (Azrin, Donohue et al., 2001).
Measures
Demographic interview
A structured interview was utilized to obtain demographic and background information about the participants, including the participants’ age, age of the participant's child, ethnicity, personal income, household income, highest grade achieved, number of biological children, and employment status.
Primary outcome measures
Participants were referred to treatment for coexisting child neglect and drug abuse. To determine potential of participants to maltreat their children Abuse scores of the Child Abuse Potential Inventory were examined (CAPI; Milner, 1986). Higher scores are indicative of greater likelihood of child maltreatment potential, with scores above 215 indicating significant potential for child maltreatment. The CAPI is widely considered the most validated instrument to assess child maltreatment potential (see most recent review by Walker & Davies, 2010). Psychometric properties of the CAPI have been examined in more than 100 articles during the past 20 years. Walker and Davies (2010) review 27 studies that have demonstrated the CAPI's cross-cultural validity, internal consistency of its subscale and total scale scores across sample groups and cultures, relatively high (albeit varied) sensitivity and specificity classification rates, differential validity, and treatment sensitivity.
Frequency of days using marijuana and hard drugs (illicit drugs other than marijuana) during the four months prior to assessment was examined using the Timeline Follow-back (TLFB; Sobell & Sobell, 1992) and urinalysis testing. The TLFB utilizes a calendar to evaluate daily patterns and frequency of drug use over a specified time period (i.e., four months). Memorable events (e.g., birthdays, holidays) are marked on the calendars to facilitate recall. As in our previous controlled trials, the TLFB was administered to both study participants and their primary adult significant others separately. An 8-panel urinalysis toxicology screen (marijuana, cocaine, amphetamines, barbiturates, opiates, benzodiazepines, methadone, phencyclidine) incorporating conventional detection cut-offs was used to corroborate TLFB data. To derive a reliable estimate of the number of days participants used marijuana and hard drugs, the substance use measure (participant TLFB, significant other TLFB, urinalysis) that indicated greatest substance use during the respective 4-month assessment period was utilized. For instance, if a participant reported 3 days of marijuana use, the significant other reported 1 day of marijuana use, and urinalysis testing results indicated no marijuana use, 3 days of marijuana use was used to estimate the frequency of marijuana use. The TLFB has consistently demonstrated concurrent validity, predictive validity, inter-rater agreement, face validity, and treatment sensitivity (Carey, 1997; Donohue et al., 2004; Donohue, Hill et al., 2007; Hjorthøj, Hjorthøj, & Nordentoft, 2012; Vinson, Reidinger, & Wilcosky, 2003).
Secondary outcome measures
The 24-item Total Risk Scale of the Risk Assessment Battery (RAB; Metzger et al., 1990) was examined to assess risk of HIV transmission. Higher scores indicate greater risk of HIV transmission. The RAB has demonstrated construct validity in factor analyses, it's test-retest reliability has been shown to range from .69 to .88, its internal consistency is poor to good (Cronbach's alpha range from .42 to .82), it has demonstrated discriminant validity (differentiating between respondents engaged in different drug use patterns), and predictive validity in identifying seroconverters on the basis of higher risk scores (http://www.med.upenn.edu/hiv/rab_psychometrics.html; Metzger, Woody, & Navaline, 1993). Participant and significant other TLFB formats were utilized to assess the number of days participants’ children were reported to be in DFS custody, as well as several participant outcomes that have been examined in our previous drug abuse clinical trials (i.e., hours employed, days using alcohol, days incarcerated).
Statistical Plan
Preliminary analyses were performed to determine if FBT providers demonstrated satisfactory intervention integrity, and to determine if participants in FBT and TAU were statistically different (p < .05) on demographic and baseline measures. Intent-to-treat data analysis was performed to determine the effects of treatment and neglect type on the dependent variables. Specifically, mixed model analyses were conducted for the participants’ primary (i.e., CAPI Abuse scale, hard drug use, marijuana drug use) and secondary (RAB total scale, TLFB hours employed, days intoxicated from alcohol, days incarcerated, days child spent in DFS custody) measures, with treatment (2 levels: FBT, TAU) and neglect type (2 levels: neglect due to child being exposed to drugs, other child neglect) as the independent variables, and time (baseline/6-mo. post-randomization) as the within subject factor. A similar series of separate analyses was conducted to determine if outcomes were different between baseline and the 10-month post-randomization assessments. Effect sizes for primary and secondary outcome measures in the repeated measures models are given as η2. In those instances where specific, non-model based post-hoc examination of means was warranted, Hedges’ g statistic (Grissom & Kim, 2005; Hedges & Olkin, 1985) and 95% confidence intervals around g are provided to highlight individual differences between baseline to 6-month post-randomization and baseline to 10-month post-randomization assessments.
It was hypothesized that participants receiving FBT would demonstrate significantly better outcomes than participants in TAU from baseline to 6-month post-randomization, and from baseline to 10-month post-randomization (all ps < .05). It was further hypothesized that there would be significant 2-way interactions in all dependent measures showing greatest relative improvements in FBT mothers who were referred for child neglect not due to their child being exposed to illicit drugs, as compared with FBT mothers who were referred for child neglect due to their child being exposed to drugs and TAU participants, from baseline to 6-month post-randomization, and baseline to 10-month post-randomization.
Results
Preliminary Analyses
FBT intervention fidelity
The method of determining protocol adherence has been utilized in our previous NIDA- and NIMH-funded clinical trials, and has been formally demonstrated to be a reliable and valid method (Azrin et al., 2001; Sheidow, Donohue, Hill, Henggeler, & Ford, 2008). Protocol checklists include each of the critical steps required to implement each intervention and are used by therapists during treatment to guide the intervention. Protocol adherence of FBT providers was determined by computing the number of protocol instructions reported to have been implemented by providers, and dividing this number by the total number of prescribed protocol instructions. Results indicated that 95% of the protocol instructions were implemented by providers, suggesting providers achieved high adherence to FBT protocols. Adherence to individual interventions ranged from 81% (Self-Control) to 99% (Child Management). Approximately 10% of sessions were randomly coded by independent reviewers who were blind to the provider assessments of protocol. The providers’ and independent raters’ lists were compared, and a reliability estimate was computed to estimate inter-rater reliability. The intra-class correlation coefficient was 96.4%, suggesting the providers’ estimates of protocol adherence were reliable.
FBT session attendance
The average number of FBT sessions attended by mothers was 14.9 meetings (sd = 7.2), whereas the average number of sessions attended by their adult significant others was 10.0 (sd = 6.9) meetings.
Comparison of experimental conditions at baseline
Potential pre-treatment differences between experimental conditions were examined utilizing Chi-square analyses on baseline categorical demographic and outcome variables, and one-way ANOVAs on continuous demographic and outcome variables utilizing assigned experimental condition (FBT, TAU) as the independent variable. These results indicated that there were no significant baseline differences between participants in the respective intervention conditions on the examined demographic and outcome measures at baseline (all p-values > .05). Table 1 presents demographic data.
Comparison of experimental conditions in treatment retention
The proportions of participants completing 6- and 10-month post-randomization assessment do not significantly differ between FBT and TAU (χ2 = .016, p = .899). Odds ratios and associated phi coefficients indicated small and non-significant effects between groups at the 6-month (OR = 2.368, 95% CI = 0.76 - 7.32, phi = .18, Fishers exact probability = .17) and 10-month (OR = 2.215, 95% CI = 0.66 - 7.42, phi = .20, Fishers exact probability = .24) post randomization assessments.
Examination of Primary Outcomes
Means and standard deviations for the primary measures for FBT and TAU participants by referral status across time are presented in Table 2. The effect of intervention and neglect type on child maltreatment potential was analyzed utilizing repeated measures analyses of variance (ANOVAs). There was a significant main effect for time from baseline to 6-month post-randomization, F(1, 68) = 15.820, p < .001, partial η2 = .189 and baseline to 10-month post randomization, F(1, 68) = 12.156, p < .001, partial η2 = .152, indicating that CAPI Abuse scores were significantly reduced across time. There was a significant Time × Neglect Type interaction from baseline to 6-month post-randomization, F(1, 68) = 6.037, p = .009, partial η2 = .082, indicating mothers of children who were referred for child neglect other than substance exposure demonstrated greater improvements in reducing their child maltreatment potential than mothers referred for neglect due to exposing their child to drugs. As hypothesized, there was a significant Time × Treatment × Neglect Type interaction from baseline to 6-month post-randomization, F(1, 68) = 5.977, p = .009, partial η2 = .081, and baseline to 10-month post-randomization, F(1, 68) = 3.329, p = .04, partial η2 = .047. Post-hoc analyses indicated that FBT mothers of non-drug exposed children reduced their child maltreatment potential more than FBT mothers of drug-exposed children, and TAU mothers (p < .05).
Table 2.
Means and Standard Deviations of Primary Outcome Measures at Baseline, 6- and 10-Mo. Post-Randomization (N = 72)
| Measure | FBT |
TAU |
||||
|---|---|---|---|---|---|---|
| All Participants M(SD) | Drug Exposed M(SD) | Other Neglect M(SD) | All Participants M(SD) | Drug Exposed M(SD) | Other Neglect M(SD) | |
| CAPI Abuse Scale | ||||||
| Baseline | 176.4 (107.4) | 130.1 (88.8) | 238.3 (100.7) | 168.7 (103.8) | 128.2 (90.4) | 199.6 (104.6) |
| 6-mo. post- | 135.4 (86.0) | 121.8 (85.3) | 153.5 (86.5) | 144.2 (113.1) | 97.0 (106.8) | 180.1 (106.5) |
| 10- mo. post- | 135.6 (89.7) | 128.8 (97.9) | 144.7 (79.7) | 140.0 (112.0) | 107.3 (108.1) | 165.0 (110.8) |
| Hard Drug Use | ||||||
| Baseline | 16.2 (26) | 6.1 (8.4) | 29.7 (34.7) | 17.3 (25.4) | 22.8 (33.1) | 13.2 (17.3) |
| 6-mo. post- | 6.4 (20.0) | 3.9 (5.1) | 9.7 (30.2) | 10.0 (20.3) | 12.8 (27.4) | 7.9 (12.9) |
| 10--mo. post- | 7.0 (20.1) | 5.1 (6.8) | 9.5 (30.2) | 7.5 (16.3) | 4.0 (10.3) | 10.1 (19.6) |
| Marijuana Use | ||||||
| Baseline | 30.0 (38.3) | 11.9 (28.7) | 30.0 (38.3) | 28.0 (43.6) | 23.9 (39.0) | 31.1 (47.6) |
| 6-mo. post- | 6.2 (19.0) | 1.4 (3.1) | 12.6 (27.9) | 7.4 (27.4) | .4 (1.1) | 12.6 (35.9) |
| 10-mo. post- | 8.8 (25.8) | 2.9 (8.0) | 16.7 (37.6) | 8.2 (28.0) | 3.1 (10.3) | 12.1 (36.0) |
Note. CAPI = Child Abuse Potential Inventory; Drug Exposed = mothers whose children were exposed to drugs; Other Neglect = Mothers founded for neglect of children other than drug exposure.
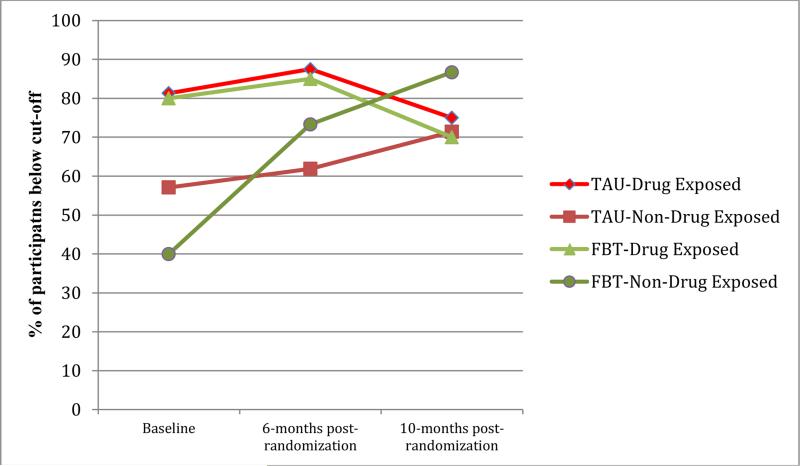
In determining the clinical meaningfulness of these results, CAPI Abuse scale scores were examined based on clinical cut-off scores that indicate risk for child maltreatment potential (i.e., scores above 215 indicate significant risk) at baseline, 6-mo. post-randomization, and 10-mo. post-randomization across intervention condition and neglect type. As can be seen in Figure 1, these results corroborate that FBT was particularly meaningful in mothers of non-drug exposed children.
Table 3 shows effect sizes and corresponding 95% confidence intervals for FBT and TAU from baseline to 6- and 10-month post-randomization. In reducing child maltreatment potential from baseline to 6-month post-randomization and from baseline to 10-month post-randomization FBT demonstrated medium effects, whereas TAU demonstrated small effects.
Table 3.
Overall Effect Sizes (Hedges’ g) and 95% Confidence Intervals for Secondary Measures (N = 72)
| Measure | FBT | TAU |
|---|---|---|
| Primary Measures | ||
| CAPI Abuse Scale | ||
| 6-mo. post- | .41 (−.11, .94) | .23 (−.25, .70) |
| 10-mo. post- | .41 (−.10, .92) | .27 (−.21, .74) |
| TLFB Hard Drug Use | ||
| 6-mo. post- | .41 (−.11, .93) | .31 (−.16, .79) |
| 10-mo. post- | .39 (−.12, .90) | .45 (−.02, .93) |
| TLFB Marijuana Use | ||
| 6-mo. post- | .74 (.22, 1.27) | .55 (.07, 1.04) |
| 10-mo. post- | .63 (.12, 1.15) | .53 (.06, 1.01) |
| Secondary Measures | ||
| HIV RAB Total | ||
| Baseline-to-post | .33 (−.19, .85) | .00 (−.48, .48) |
| Baseline-to-follow-up | .33 (−.18, .84) | .24 (−.24, .71) |
| Hours Worked | ||
| 6-mo. post- | −.18 (−.70, .34) | .23 (−.25, .71) |
| 10-mo. post- | −.30 (−.80, .21) | .04 (−.43, .52) |
| Alcohol Intoxication | ||
| 6-mo. post- | .31 (−.21, .83) | .11 (−.37, .59) |
| 10-mo. post- | .37 (−.14, .88) | .33 (−.14, .81) |
| Incarceration | ||
| 6-mo. post- | .02 (−.50, .54) | −.40 (−.88, .08) |
| 10-mo. post- | .03 (−.48, .54) | −.35 (−.83, .12) |
| Child In DFS Custody | ||
| 6-mo. post- | −.24 (−.76, .28) | −.28 (−.76, .19) |
| 10-mo. post- | −.04 (−.55, .47) | −.12 (−.59, .36) |
Note. CAPI = Child Abuse Potential Inventory. In the interpretation of Hedges’ g absolute magnitude from zero demonstrates larger effect sizes: small = ±.2, medium = ±.5, and large = ±.8 (Cohen, 1988).
For hard drug use, the repeated measures analyses of variance indicated that there was a significant main effect for time from baseline to 6-month post-randomization, F(1, 68) = 15.424, p < .001, partial η2 = .185, and baseline to 10-month post-randomization, F(1, 68) = 12.484, p < .001, partial η2 = .155, indicating that hard drug use was significantly reduced across time. As hypothesized, hard drug use revealed a significant Time × Treatment × Neglect Type interaction from baseline to 6-month post-randomization, F(1, 68) = 5.577, p = .015, partial η2 = .076, and from baseline to 10-month post-randomization, F(1, 68) = 8.148, p = .003, partial η2 = .107. Post-hoc analysis of these interaction effects indicated that mothers of non-drug exposed children in FBT demonstrated significant decreases in hard drug use, as compared with mothers of drug exposed children in FBT and mothers of non-drug exposed children in TAU (p <.05). Mothers of drug exposed children in TAU demonstrated significant decreases in hard drug use, as compared with mothers of drug exposed children in FBT and mothers of non-drug exposed children in TAU. Consistent with these results, Table 3 indicates that effect sizes for hard drug use were small to medium for both FBT and TAU from baseline to 6-month post-randomization, and from baseline to 10-month post-randomization assessment. When examining reductions in marijuana use, there was a significant main effect for time from baseline to 6-month post-randomization, F(1, 68) = 19.346, p < .001, partial η2 = .221, and baseline to 10-month post-randomization, F(1, 68) = 17.327, p < .001, partial η2 = .203, indicating that marijuana use decreased across time. Although hypothesized, there were no significant interactions for marijuana use (all ps > .05). Examination of effect sizes in Table 3 shows that FBT and TAU participants demonstrated medium to large effect sizes from baseline to both 6- and 10-month post-randomization.
Examination of Secondary Outcomes
Similar intent to treat repeated measures analyses were conducted for secondary dependent measures (RAB total scale, TLFB hours employed, days intoxicated from alcohol, days incarcerated, days child spent in DFS custody). Means and standard deviations of these outcome measures are presented in Table 4. Specific to the RAB total scale, there was a significant main effect for time from baseline to 6-month post randomization, F(1, 68) = 6.010, p = .008, partial η2 = .081 and baseline to 10-month post-randomization, F(1, 68) = 8.480, p = .003, partial η2 = .111, demonstrating that HIV risk behaviors were significantly reduced across time. As hypothesized, there was a significant Time × Treatment interaction from baseline to 6-month post-randomization, F(1, 68) = 4.014, p = .03, partial η2 = .056, suggesting that participants in FBT demonstrated relatively greater improvements in HIV risk behavior from baseline to 6-month post-randomization as compared with TAU participants. The hypothesized Time × Treatment and Time by Neglect Type by Treatment interactions were not significant from baseline to 10-month post-randomization (ps > .05). These results are consistent with the effect sizes indicated in Table 3. Participants in FBT evidenced a small to medium effect size from baseline to 6-month post-randomization, whereas TAU participants essentially demonstrated no effect during this time. At 10-month post-randomization both FBT and TAU participants demonstrated a small effect.
Table 4.
Means and Standard Deviations of Secondary Outcome Measures at Baseline, 6- and 10-Month Post-randomization (N= 72)
| Measure | FBT | TAU | ||||
|---|---|---|---|---|---|---|
| All Participants M(SD) | Drug Exposed M(SD) | Other Neglect M(SD) | All Participants M(SD) | Drug Exposed M(SD) | Other Neglect M(SD) | |
| HIV RAB Total | ||||||
| Baseline | .12 (.06) | .13 (.07) | .12 (.05) | .13 (.08) | .11 (.04) | .14 (.10) |
| 6-mo. post- | .10 (.06) | .12 (.06) | .09 (.05) | .13 (.08) | .11 (.05) | .14(.10) |
| 10-mo. post- | .10 (.06) | .11 (.07) | .09 (.05) | .11 (.09) | .08(.05) | .14 (.10) |
| Hours Worked | ||||||
| Baseline | 47.2 (138.0) | 50.48 (121.96) | 42.87 (161.38) | 31.2 (121.3) | 5.00 (20.00) | 51.10 (158.80) |
| 6-mo. post- | 72.1 (146.8) | 66.00 (147.25) | 80.27 (151.03) | 9.2 (44.5) | 5.00 (20.00) | 12.43 (56.95) |
| 10-mo. post- | 91.0 (160.9) | 103.13 (176.83) | 74.87 (141.12) | 25.9 (124.4) | 0 (0) | 45.67 (164.04) |
| Alcohol Intoxication | ||||||
| Baseline | 6.5 (18.9) | 0.10 (0.31) | 15.13 (27.00) | 6.8 (21.8) | 1.06(2.74) | 11.10 (28.42) |
| 6-mo. post- | 1.9 (4.3) | 0.40 (0.94) | 3.80 (6.13) | 4.5 (20.1) | 0.25 (0.58) | 7.76 (26.53) |
| 10-mo. post- | 1.2 (2.9) | 0.21 (0.54) | 2.40 (4.14) | 1.4 (4.9) | 0.44 (0.63) | 2.14 (6.51) |
| Incarceration | ||||||
| Baseline | 2.9 (11.7) | 4.55 (15.31) | 0.60 (1.68) | 2.0 (5.0) | 0.63 (1.41) | 3.10 (6.37) |
| 6-mo. post- | 2.7 (11.6) | 4.25 (15.29) | 0.60 (1.68) | 5.4 (11.8) | 3.50 (11.77) | 6.86 (11.93) |
| 10-mo. post- | 2.6 (7.5) | 2.35 (7.68) | 3.00 (7.56) | 7.2 (20.9) | 0.44 (1.75) | 12.38 (26.81) |
| Child In DFS Custody | ||||||
| Baseline | 29.7 (42.7) | 24.10 (40.19) | 37.13 (46.06) | 38.4 (46.2) | 24.75 (37.64) | 48.76 (50.18) |
| 6-mo. post- | 41.2 (55.0) | 25.70 (48.70) | 61.87 (57.76) | 52.9 (56.3) | 35.06 (54.27) | 66.48 (55.28) |
| 10-mo. post- | 31.5 (47.4) | 29.85 (50.27) | 33.80 (44.80) | 44.2 (54.6) | 45.13 (59.90) | 43.52 (51.73) |
Note. DFS = Department of Family Services; HIV = human immunodeficiency virus; RAB = Risk Assessment Battery; Drug Exposed = mothers whose children were exposed to drugs in utero; Other Neglect = Mothers founded for neglect of children living in the home.
There were no significant effects in time for baseline to 6- and 10-month post-randomization in hours of employment. As hypothesized, however, there was a significant Time × Treatment interaction in the number of hours employed from baseline to 6-month post-randomization, F(1, 68) = 3.868, p = .027, partial η2 = .054, and baseline to 10-month post-randomization, F(1, 68) = 3.549, p = .032, partial η2 = .05. Thus, FBT participants worked significantly more hours compared with TAU participants across time. No other significant interaction effects for hours employed were found. Examination of Table 3 shows FBT and TAU participants both evidence small effects from baseline to 6-month post-randomization (FBT increasing employment, TAU decreasing days worked), whereas effects get somewhat larger for FBT and disappear for TAU from baseline to 10-month post-randomization.
Specific to alcohol intoxication, results revealed a significant main effect from baseline to 6-month randomization, F(1, 68) = 6.008, p = .009, partial η2 = .081, and baseline to 10-month post-randomization, F(1, 68) = 6.082, p = .006, partial η2 = .092, indicating that alcohol intoxication was significantly reduced across time. A significant Time × Neglect Type interaction was observed from baseline to 6-month post-randomization, F(1, 68) = 5.224, p = .01, partial η2 = .071, indicating mothers of non-drug exposed children, as compared with mothers of drug exposed children, demonstrated greatest reductions in alcohol intoxication. No other significant differences were found for alcohol intoxication. With the exception of baseline to 6-month post-randomization for TAU (no effect), these results are consistent with small to medium effect sizes reported in Table 3.
Regarding incarceration, results revealed a marginally significant main effect from baseline to 6-month randomization, F(1, 68) = 2.554, p = .058, partial η2 = .036. There was a significant Time × Neglect interaction from baseline to 6-month post-randomization, F(1, 68) = 3.395, p = .04, partial η2 = .048. As hypothesized, there was a significant Time × Treatment interaction from baseline to 6-month post randomization, F(1, 68) = 3.061, p = .04, partial η2 = .043, showing FBT participants spent significantly fewer days incarcerated as compared with TAU participants from baseline to 6-month post-randomization. This finding was not maintained 10-months after randomization (p >.05). No other significant differences between experimental conditions were found. Examination of Table 3 shows no effect for FBT from baseline to 6- and 10-month post-randomization, whereas there are medium effects specific to TAU during this same time period. In understanding these effects it is important to consider that examination of means in Table 4 shows TAU participants increased their incarceration. Thus, FBT to some extent may have assisted in preventing future incarceration.
Lastly, when examining effects of intervention and neglect type on the number of days children were in DFS custody, a significant main effect for time from baseline to 6-month post-randomization was observed, F(1, 68) = 7.625, p = .004, partial η2 = .101. Thus, children were significantly more likely to spend more time in DFS custody from baseline to 6-month post-randomization. This result was not found pre- to 10-month post-randomization (p >.05). No other significant differences were found. Examination of Table 3 shows there was a small effect for both FBT and TAU from baseline to 6-month post-randomization, indicating the children of participants increased their time in DFS custody during this time. These effects were diminished from baseline to 10-month post-randomization, particularly in FBT participants.
Discussion
The very few controlled treatment outcome studies that have been conducted in child neglect samples indicate in-situ delivered family-supported treatment programs are relatively efficacious, although results are not universally positive. We are unaware of controlled trials that have demonstrated positive outcomes in parents who have been referred to treatment for concurrent child neglect and drug abuse. However, in uncontrolled trials, Family Behavior Therapy (FBT) has shown promise in this population. Therefore, the current randomized controlled trial is a methodological advancement in the treatment in coexisting child neglect and drug abuse. It was hypothesized that FBT, relative to TAU, would result in improved outcomes from baseline to 6- and 10-month post-randomization assessments, and that FBT would be particularly efficacious with mothers of non-drug exposed children relative to mothers of children exposed to drugs who report relatively less severe behavior problems.
Results indicated that within-subject improvements were found from baseline to 6- and 10-month post-randomization for most measures and many of the hypothesized interaction effects were significant. Specific to the primary measures, FBT was more effective than TAU in reducing child maltreatment potential in mothers of non-drug exposed children from baseline to 6- and 10-month post-randomization. For instance, more FBT mothers of non-drug exposed children were below the clinical cut-off score for child maltreatment potential at 10-month post-randomization than all other mothers (i.e., 47% improvement as compared with 14% improvement for TAU mothers of non-drug exposed children and 10% and 6% decrease, respectively, for FBT mothers of drug exposed children and TAU mothers of non--drug exposed children. FBT was also more efficacious than TAU in hard drug use in mothers of non-drug exposed children from baseline to both 6- and 10-month post-randomization. However, from baseline to 6- and 10-month post-randomization, TAU mothers of drug exposed children demonstrated a greater decrease in hard drug use than TAU mothers of non-drug exposed children and FBT mothers of drug exposed children. Mothers demonstrated medium (TAU) to large (FBT) effects in significantly decreasing marijuana use. These differences, however, were not significantly discrepant.
In trying to understand these findings it is important to indicate that the mothers who were found to neglect their children for reasons other than illicit drug exposure in this study were older than mothers who were found to expose their children to illicit drugs, and given their older age may have been particularly motivated to participate in behavioral treatment (Choi & Ryan, 2011). Mothers of non-drug exposed children also had relatively older children who were in the age range typically targeted in parent training child management programs for physical abuse (Chaffin et al., 2004; Kolko, 1996; Swenson, Schaeffer, Henggeler, Faldowski, & Mayhew, 2010). Moreover, the families of these mothers appeared to be more intact and less transient than mothers who had exposed their children to drugs, permitting FBT providers to encourage family support and facilitate family activities, home safety tours, and in vivo child management practice opportunities (e.g., descriptively praising their children, positive practice) that were incompatible with substance use, and compatible with family cohesion. Therefore, in treating child maltreatment potential and hard drug use in mothers who have been indicated to neglect their children and abuse drugs, the results of this study suggest recommendations for treatment may need to be based on the type of child neglect evidenced. The FBT intervention components examined in this study are probably more in line with mothers who are referred for non-drug exposed types of neglect (e.g., lack of supervision, emotional, medical, environmental, physical neglect) that appear to be associated with relatively higher risk for future child maltreatment. However, in treating hard drug use and child maltreatment in mothers who have been found to expose their children to drugs and evidence relatively low risk for child maltreatment, TAU community services appear to be supported over FBT. In treating marijuana use, it appears that TAU and FBT are equally justified, although FBT demonstrated larger, albeit non-significant, effect sizes.
Specific to secondary measures, no differences between TAU and FBT were found for the number of days of alcohol intoxication, and days children were in DFS custody. FBT was more effective than TAU from baseline to 6-month post-randomization in decreasing HIV risk behaviors and hours employed, with marginal improvements (p = .058) in days mothers were incarcerated. FBT was also shown to be more effective than TAU from baseline to 10-month post-randomization in the improvement of days employed. Improvements in secondary outcomes did not appear to be influenced by child neglect type, as hypothesized. Along these lines, intervention implementation for some of the secondary measures (i.e., HIV risk behaviors, days employed, days incarcerated) appeared to be relatively less dependent on the influence or presence of family members. Indeed, mothers often preferred to discuss these problem areas privately, leading FBT providers to emphasize treatment components to address these target goals when children were removed from the home by CPS and/or significant others were absent.
Although the reduction of HIV risk behaviors in FBT, compared to TAU, was relatively short-lived, the integration of an HIV prevention program within family-based treatment is an important first step in treatment research involving this highly susceptible population. Indeed, HIV/STD risk behaviors were explicitly addressed in treatment planning, behavioral goals, contingency management, stimulus control, and self-control, which are hallmark behavioral interventions. Given the substantial risk in this population for contracting HIV/STD, and the resulting challenges this poses for treatment (and in parenting in particular), future studies of evidence-based approaches to high-risk populations such as the one examined here, would do well to target these problem behaviors. Indeed, complicating factors in preventing HIV infection have been noted in populations with substance use disorders, with a call for comprehensive and integrated care (Nijhawan, Kim, & Rich, 2008). While our focus was specifically on behaviors that place mothers at risk for HIV, future studies are needed to determine whether there are corresponding decreases in HIV seroconversion associated with integrated HIV prevention implementation in this population, including concomitant decreases in other infectious diseases.
Employment is a critical factor in community re-integration among persons suffering from substance disorders, and assisting women in this population to meet financial obligations is necessary to ensure adequate housing and nutrition of their children. Therefore, FBT providers spent considerable time teaching mothers in this condition to develop career interests, prepare resumes, solicit job interviews, develop job interview and financial management skills, and retain employment. Mothers and their significant others were generally very motivated to participate in these activities, and we believe there may be long-term beneficial effects in training mothers in this population to gain and retain employment, such as financial independence from federal and state resources and abusive intimate partners.
The current trial suggests FBT may be beneficial in mothers who have been referred by CPS for child neglect and drug abuse, particularly in mothers of children referred for non-drug exposed child neglect types that are likely to evidence high risk potential for future child maltreatment. Indeed, the results indicate an incremental improvement associated with FBT over TAU, suggesting FBT is generally preferred over TAU. However, it is important to emphasize that TAU mothers showed improvements on a number of treatment outcome measures, and that mothers of drug exposed children with less risk for future child maltreatment victimization demonstrated greater reductions in hard drug use and child maltreatment potential when compared with FBT mothers who were referred due to having exposed their children to drugs. Although it is difficult to determine the change agents in TAU, these results should be anticipated given that both specific and non-specific treatment factors play an important role in treatment effectiveness, and these factors positively influence intervention programs typically provided in TAU (e.g., drug court, psychiatric hospitalization, family reunification). Future studies are needed to identify and integrate TAU community services, including the development of psychometrically validated measures of TAU implementation, to better understand the merits of TAU conditions.
Given that this was the first clinical trial to concurrently address substance abuse and child neglect, despite its extremely high comorbidity, there are a number of issues that are worthy of consideration when conducting family-based treatment in this population. First, it was originally proposed to exclude mothers from the study if they did not have an adult significant other living in the home and willing to participate in their treatment. This criterion is hypothesized to assist in providing opportunities to implement prescribed family supported interventions, including home practice of parenting techniques and drug relapse prevention strategies, with adult significant others who are likely to monitor children in the homes of participating mothers. However, in our pilot trials for this study we discovered that many of the referred women did not have supportive significant others who were stable, positive influences permanently living in their homes. Many of the available significant others transitioned in and out of the mother's residence. Therefore, to enhance generalizability and assist in recruitment of participants, we relaxed this criterion at the onset of the study to specify that adult significant others were not required as residents in the mothers’ homes. This change probably resulted in the inclusion of mothers with a higher proportion of troublesome or superficial relationships. For example, some mothers were financially and emotionally dependent on significant others who were abusive to them or abused substances. Therefore, many of the FBT sessions were focused on assisting mothers in achieving employment or learning self-protection strategies, which took therapy session time away from other target problem areas, but improved sustainable employment and personal independence. Therefore, methods of engaging appropriate significant others within the context of family-based treatment for concurrent child neglect and substance abuse is warranted.
Consistent with the U.S. Department of Health and Human Services, Administration on Children, Youth and Families (2009) guidelines for family preservation, it was originally proposed that the neglected child would need to be living in the residence of the mother to qualify for the study. However, as Table 4 indicates, a high percentage of neglected children were removed from the homes of their mothers throughout the study, which often decreased motivation of mothers to participate in treatment, and decreased opportunities to apply or practice parenting skills learned in FBT with their children. Therefore, this study inclusion criterion was modified prior to this study to permit mothers to be enrolled in the study if it was the intention of CPS to work with the Court to return the child to the mother after appropriate services were established. Despite assurances from CPS caseworkers, and often inconsistent with the progress of mothers in therapy, children were often not returned into the homes of their mothers in a timely manner, and sometimes were not returned. Of course, this decreased motivation of the mothers to actively participate in treatment and made it difficult to practice behavioral parenting strategies in vivo with their children, which as indicated previously is important in the treatment of child neglect (Hurley et al., 2012). Along this vein, an examination of child protection cases in the County for which this study was conducted revealed that homelessness, methamphetamine use, and lack of resources regularly prompted placement of children into CPS custody, with many cases showing drug use as the exclusive reason for separation (Pelton, 2008). Moreover, many of the separated children experienced instability in their living arrangements and emotional problems. Managing home adjustment issues is certainly appropriate within FBT, which incorporates specific intervention techniques to address common crisis situations and family emergencies as they arise (Urgelles, Donohue, Wilks, Van Hasselt, & Azrin, 2012). However, many of the emergency outcomes (e.g., domestic violence, eviction, financial need, no food) were not formally assessed in this study, supporting the need to develop outcome measures with real-world application. Lastly, time spent in crisis management competed with the implementation of prescribed treatments aimed at addressing underlying issues perpetuating child neglect and drug abuse.
It is important to emphasize that FBT does not include prescribed intervention components designed to assist caseworkers in managing positive consequences for successful treatment participation and outcomes. For instance, in this study, team meetings between participants, caseworkers, FBT providers and others were attempted to assist treatment planning. However, case management follow through was sometimes missing, limited or inconsistent. Some caseworkers closed their cases with CPS immediately after the referral to FBT or made non-contingent recommendations to separate children from the homes of their mothers. In these situations, motivation of mothers to complete treatment was compromised and parenting practice opportunities at home were limited. We believe a formalized incentive program to assist mothers in treatment completion may have been helpful along these lines (Ledgerwood, Alessi, Hanson, Godley, & Petry, 2008).
Study Strengths, Limitations and Future Directions
Overall, this study represents a significant advancement in child welfare treatment, both in terms of its methodology and scope of practice implications. It is the first controlled outcome study to incorporate psychometrically validated clinical interviews, self-report measures, and biological testing to assist in formally examining and diagnosing substance use disorders in child maltreatment, and adheres to rigorous experimental methods (e.g., blind assessment technicians, intent to treat management of missing data, treatment integrity checks). Specific to practice implications, the results of this study suggest family-based behavioral treatments are justified for use in this very difficult to treat population. However, as in most studies, there were limitations in the methodology of this study, including the lack of outcome measures specific to the direct assessment of behaviors, home conditions, attitudes, and underlying belief systems of participants. Along these lines, the psychometric development of innovative outcome measures are desperately needed in child neglect and drug abuse, including the development of measures to assess quality in the relationship between perpetrators of child neglect and their significant others, role-play performance that is specific to preventing dangerous and inappropriate scenarios, and measures of service utilization in TAU conditions. In this regard, we are currently attempting to validate a measure aimed at detecting home hazards through behavioral observation occurring during home tours.
It should be mentioned that the average number of sessions attended by participants in the Family Behavior Therapy condition was 15, whereas they were scheduled to receive up to 20 sessions. Fifteen sessions is comparable or more than the number of sessions attended by participants receiving behavioral interventions in outcome studies specific to child maltreatment and substance abuse. However, the severity of behavior problems evidenced by parents in this study suggests research in the development of engagement and retention interventions in this population is warranted. The examined FBT in this study incorporated empirically-supported methods of engagement and retention, including orientation and detailed session reminder telephone calls, consumer selection of intervention components, and integrated significant other support (Donohue, Azrin et al., 1998) that probably assisted in maintaining a relatively high number of sessions. Although these methods were not formally examined in the current study, our investigative team is attempting to empirically examine the effects of meal and cell phone provision contingent on therapy attendance in this population. Future studies will need to empirically develop and assess similar innovative methods of treatment retention and engagement utilizing controlled methodology.
In conclusion, this investigation suggests there is much work to be done in child neglect and drug abuse treatment outcome research. Our results support family-based treatment in mothers who have been found to neglect their children and abuse drugs, and to an incrementally lesser extent TAU. Additional controlled trials in child neglect and drug abuse are desperately needed, particularly with large sample sizes to assist in understanding heterogeneity within this population. Although intent to treat analysis in the current study assisted in minimizing the influence of attrition, it also decreased power, thus limiting the number and type of analyses that could be reliably performed.
Figure 2.
Percentage of mothers below CAPI Abuse scale clinical cut-off scores (< 215)at baseline, 6- and 10-month-post randomization across treatment condition and neglect type (N=72)
Acknowledgements
This study was supported with a grant awarded to Brad Donohue from the National Institute on Drug Abuse (1R01DA20548-01A1).
Personal acknowledgment from primary author: With the passing of Nathan H. Azrin, I am honored to be included in his last of many outcome studies. He was always the consummate pioneer driving innovation while making his research team members foolishly believe they came up with the ideas. Given his tremendous contributions to the treatment of human suffering, it is soothing for me to know he was interested in concluding his prodigious career developing treatments for children most in need of positive reinforcement.
Footnotes
The first and last author would like to report that they have received financial compensation to conduct research involving FBT funded by the National Institutes of Health (including the current study), book royalties specific to FBT, and have conducted both pro bono and financially compensated training in FBT. These efforts have been disclosed to their governing institution and determined by this institution not to be a conflict of interest.
References
- Amirav I, Luder A, Viner Y, Finkel M. Decriminalization of cannabis-Potential risks for children? Acta Paediatrica. 2010;100(4):618–619. doi: 10.1111/j.1651-2227.2010.02081.x. doi:10.1111/j.1651-2227.2010.02081.x. [DOI] [PubMed] [Google Scholar]
- Appelboam A, Oades PJ. Coma due to cannabis toxicity in an infant. European Journal of Emergency Medicine. 2006;13(3):177–179. doi: 10.1097/01.mej.0000194405.38206.f2. [DOI] [PubMed] [Google Scholar]
- Azrin NH, Acierno R, Kogan ES, Donohue B, Besalel V, McMahon PT. Follow-up results of Supportive versus Behavioral Therapy for illicit drug use. Behaviour Research and Therapy. 1996;34:41–46. doi: 10.1016/0005-7967(95)00049-4. [DOI] [PubMed] [Google Scholar]
- Azrin NH, Besalel-Azrin VA. How to Use Positive. The University of Virginia; H & H Enterprises, Inc.; 1981. [Google Scholar]
- Azrin NH, Donohue B, Besalel V, Kogan E, Acierno R. Youth drug abuse treatment: A controlled outcome study. Journal of Child and Adolescent Substance Abuse. 1994;3:1–16. [Google Scholar]
- Azrin NH, Donohue B, Teichner G, Crum T, Howell J, DeCato L. A controlled evaluation and description of Individual-Cognitive Problem Solving and Family-Behavioral therapies in Conduct-Disordered and Substance Dependent youth. Journal of Child and Adolescent Substance Abuse. 2001;11:1–43. [Google Scholar]
- Azrin NH, McMahon P, Donohue B, Besalel V, Lapinski K, Kogan E, Acierno R, Galloway E. Behavior therapy of drug abuse: A controlled outcome study. Behaviour Research and Therapy. 1994;32:857–866. doi: 10.1016/0005-7967(94)90166-x. [DOI] [PubMed] [Google Scholar]
- Barone VJ, Greene BF, Lutzer JR. Home safety with families being treated for child abuse and neglect. Behavior Modification. 1986;10:93–114. doi: 10.1177/01454455860101006. [DOI] [PubMed] [Google Scholar]
- Behl LE, Conyngham HA, May PF. Trends in child maltreatment literature. Child Abuse and Neglect. 2003;27(2):215–229. doi: 10.1016/s0145-2134(02)00535-5. [DOI] [PubMed] [Google Scholar]
- Blau GM, Whewell MC, Gullotta TP, Bloom M. The prevention and treatment of child abuse in households of substance abusers: A research demonstration report. Child Welfare League of America. 1994:83–94. [PubMed] [Google Scholar]
- Brown JA, Hohman M. The impact of methamphetamine use on parenting. Journal of Social Work Practice in the Addictions. 2008;6:63–88. [Google Scholar]
- Brunk MA, Henggeler SW, Whelan JP. Comparison of multi systemic therapy and parent training in the brief treatment of child abuse and neglect. Journal of Consulting and Clinical Psychology. 1987;55:171–178. doi: 10.1037//0022-006x.55.2.171. [DOI] [PubMed] [Google Scholar]
- Carey KB. Reliability and validity of the Timeline Follow-Back Interview among psychiatric outpatients: A preliminary report. Psychology of Addictive Behaviors. 1997;11:26–33. [Google Scholar]
- Carlson BE, Williams LR, Shafer MS. Methamphetamine-involved parents in the child welfare system: Are they more challenging than other substance involved parents? Journal of Public Child Welfare. 2012;6(3):280–295. [Google Scholar]
- Chaffin M. The changing focus of child maltreatment research and practice within psychology. J Soc Issues. 2006;62(4):663–684. [Google Scholar]
- Chaffin M, Hecht D, Bard D, Silovsky JF, Beasley WH. A Statewide Trial of the SafeCare Home-based Services Model With Parents in Child Protective Services. Pediatrics. 2012;129:509–515. doi: 10.1542/peds.2011-1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaffin M, Silovsky JF, Funderburk B, Valle LA, Brestan EV, Balachova T, et al. Parent–child interaction therapy with physically-abusive parents: Efficacy for reducing future abuse reports. Journal of Consulting and Clinical Psychology. 2004;72:500–510. doi: 10.1037/0022-006X.72.3.500. [DOI] [PubMed] [Google Scholar]
- Choi S, Ryan JP. Completing substance abuse treatment in child welfare: The role of co-occurring problems and primary drug of choice. Child Maltreatment. 2011;11:313–325. doi: 10.1177/1077559506292607. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Conners NA, Bradley RH, Whiteside-Mansell LC, Crone C. A comprehensive substance abuse treatment program for women and their children: An initial evaluation. Journal of Substance Abuse Treatment. 2001;21:67–75. doi: 10.1016/s0740-5472(01)00186-6. [DOI] [PubMed] [Google Scholar]
- Corcoran J. Family interventions with child physical abuse and neglect: A critical review. Children and Services Review. 2000;22:2000. [Google Scholar]
- Davis SK. Chemical dependency in women: A description of its effects and outcome on adequate parenting. Journal of Substance Abuse Treatment. 1990;7:225–232. doi: 10.1016/0740-5472(90)90045-r. [DOI] [PubMed] [Google Scholar]
- Davis SP, Fantuzzo JW. The effects of adult and peer social initiations on the social behavior of withdrawn and aggressive maltreated preschool children. Journal of Family Violence. 1989;4:227–248. doi: 10.1037//0022-006x.56.1.34. [DOI] [PubMed] [Google Scholar]
- Dawson B, de Armas A, McGrath ML, Kelly JA. Cognitive problem solving training to improve the child-care judgment of child neglectful parents. Journal of Family Violence. 1986;1:209–221. [Google Scholar]
- Donohue B, Allen DA. Family Behavior Therapy: A Step-By-Step Approach to Adult Substance Abuse. John Wiley & Sons, Inc.; Hoboken, NJ: 2012. [Google Scholar]
- Donohue B, Azrin NH. Family Behavior Therapy: A Step-By-Step Approach to Adolescent Substance Abuse. John Wiley & Sons, Inc.; Hoboken, NJ: 2011. [Google Scholar]
- Donohue B, Azrin NH. Family behavior therapy. In: Wagner E, Waldron H, editors. Innovations in adolescent substance abuse intervention. NY7 Pergamon Press; Tarrytown: 2001. [Google Scholar]
- Donohue B, Azrin NH, Lawson H, Friedlander J, Teichner G, Rindsberg J. Improving initial session attendance in conduct disordered and substance abusing adolescents: A controlled study. Journal of Child and Adolescent Drug Abuse. 1998;8:1–13. [Google Scholar]
- Donohue B, Azrin NH, Strada MJ, Silver NC, Teichner G, Murphy H. Psychometric evaluation of self and collateral Timeline Follow-Back reports of drug and alcohol use in a sample of drug abusing and conduct disordered adolescents and their parents. Psychology of Addictive Behaviors. 2004;18:184–189. doi: 10.1037/0893-164X.18.2.184. [DOI] [PubMed] [Google Scholar]
- Donohue B, Hill H, Azrin NH, Cross C, Strada M. Psychometric support for contemporaneous and retrospective youth and parent reports of adolescent marijuana use frequency in an adolescent outpatient treatment population. Addictive Behaviors. 2007;32:1787–1797. doi: 10.1016/j.addbeh.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Donohue B, Romero V, Herdzik K, Lapota H, Abdel Al, R., Allen DA, Azrin NH, Van Hasselt VB. Concurrent treatment of substance abuse, child neglect, Bipolar Disorder, Post-Traumatic Stress Disorder, and domestic violence: A case Examination involving Family Behavior Therapy. Clinical Case Studies. 2010;9:106–124. doi: 10.1177/1534650109351928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohue B, Romero V, Hill H. Treatment of co-occurring child maltreatment and substance-abuse. Aggression and Violent Behavior: A Review Journal. 2006;11:626–640. [Google Scholar]
- Dunn MG, Tarter RE, Mezzich AC, Vanyukov M, Kirisci L, Kirillova G. Origins and consequences of child neglect in substance abuse families. Clinical Psychology Review. 2002;22:1063–1090. doi: 10.1016/s0272-7358(02)00132-0. [DOI] [PubMed] [Google Scholar]
- Ells M, Sturgis B, Wright G. Behind the drug: The child victims of meth labs. National Center for Prosecution of Child Abuse. 2002;15(2):1–4. [Google Scholar]
- Erickson MF, Egeland B. Child neglect. In: Myers JEB, Berliner L, Briere J, Hendrix CT, Jenny C, Reid TA, editors. The APSAC handbook on child maltreatment. 2nd ed. Sage; Thousand Oaks, CA: 2002. pp. 3–20. [Google Scholar]
- Fantuzzo JW, Jurecic L, Stovall A, Hightower AD, Goins C, Schachtel D. Effects of adult and peer social initiations on the social behavior of withdrawn, maltreated, preschool children. Journal of Consulting and Clinical Psychology. 1988;56:34–39. doi: 10.1037//0022-006x.56.1.34. [DOI] [PubMed] [Google Scholar]
- Fantuzzo JW, Stovall A, Schachtel D, Goins C, Hall R. The effects of peer social initiations on the social behavior of withdrawn maltreated preschool children. Journal of Behaviour Therapy and Experimental Psychiatry. 1987;18:357–363. doi: 10.1016/0005-7916(87)90050-4. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version (SCID-I) Biometrics Research, New York State Psychiatric Institute; New York, NY: 1996. [Google Scholar]
- Forehand RL, McMahon RJ. Helping the Noncompliant Child: A Clinician's Guide to Parent Training. Guilford Press; New York, NY: 1981. [Google Scholar]
- Garbarino J, Collins CC. Child neglect: The family with a hole in the middle. In: Dubowitz H, editor. Neglected children: Research, practice, and policy. Sage; Thousand Oaks, CA: 1999. pp. 1–23. [Google Scholar]
- Galloway GP, Marinelli-Casey P, Stalcup J, Lord RH, Christian D, Cohen J, Reiber C, Vandersloot D. Treatment as usual in the Methamphetamine Treatment Project. Journal of Psychoactive Drugs. 2000;32:165–175. doi: 10.1080/02791072.2000.10400225. [DOI] [PubMed] [Google Scholar]
- Gaudin JM, Wodarski JS, Arkinson MK, Avery LS. Remedying child neglect: Effectiveness of social network intervention. Journal of Applied Social Sciences. 1991;15:97–123. [Google Scholar]
- Grissom RJ, Kim JJ. Effect sizes for research: A broad practical approach. Lawrence Erlbaum Associates; Mahwah, NJ: 2005. [Google Scholar]
- Hedges LV, Olkin I. Statistical methods for meta-analysis. Academic Press; San Diego, CA: 1985. [Google Scholar]
- Henggeler SW. Delinquency and Adolescent Psychopathology: A Family-Ecological Systems Approach. Wright-PSG; Littleton, MA: 1982. [Google Scholar]
- HIV/AIDS Prevention Research Division, Department of Psychiatry Penn Behavioral Health Psychometrics. Risk Assessment Battery (RAB) Retrieved from http://www.med.upenn.edu/hiv/rab_psychometrics.html.
- Hjorthøj C, Hjorthøj A, Nordentoft M. Validity of Timeline Follow-Back for self- reported use of cannabis and other illicit substances; Systematic review and meta-analysis. Addictive Behaviors. 2012;37:225–233. doi: 10.1016/j.addbeh.2011.11.025. doi:10.1016/j.addbeh.2011.11.025. [DOI] [PubMed] [Google Scholar]
- Hohman MM, Shillington AM, Baxter H. A comparison of pregnant women presenting for alcohol and other drug treatment by CPS status. Child Abuse & Neglect. 2003;27(3):303–317. doi: 10.1016/s0145-2134(03)00008-5. doi:10.1016/S0145-2134(03)00008-5. [DOI] [PubMed] [Google Scholar]
- Hurley K, Griffith A, Ingram S, Bolivar C, Mason W, Trout A. An approach to examining the proximal and intermediate outcomes of an intensive family preservation program. Journal of Child and Family Studies. 2012;21(6):1003–1017. doi:10.1007/s10826-011-9563-z. [Google Scholar]
- Jones L. The prevalence and characteristics of substance abusers in a child protective service sample. Journal of Social Work Practice in the Addictions. 2008;42(2):33–50. [Google Scholar]
- Jones L. The prevalence and characteristics of substance abusers in a child protective service sample. Journal of Social Work Practice in Addictions. 2005;4:33–50. [Google Scholar]
- Kolko DJ. Individual cognitive behavioral treatment and family therapy for physically abused children and their offending parents: A comparison of clinical outcomes. Child Maltreatment. 1996;1:322–342. [Google Scholar]
- Kolko DJ, Selelyo J, Brown EJ. The treatment histories and service involvement of physically and sexually abusive families: description, correspondence, and clinical correlates. Child Abuse and Neglect. 1999;23:459–476. doi: 10.1016/s0145-2134(99)00022-8. [DOI] [PubMed] [Google Scholar]
- Lambert B, Scheiner M, Campbell D. Ethical Issues and Addiction. Journal of Addictive Diseases. 2010;29:2, 164–174. doi: 10.1080/10550881003684673. [DOI] [PubMed] [Google Scholar]
- LaPota HB, Donohue B, Warren CS, Allen DN. Integration of a Healthy Living curriculum within Family Behavior Therapy: A clinical case example in a woman with a history of domestic violence, child neglect, drug abuse, and obesity. Journal of Family Violence. 2011;26:227–234. doi: 10.1007/s10896-011-9358-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledgerwood DM, Alessi SM, Hanson T, Godley MD, Petry NM. Contingency management for attendance to group substance abuse treatment administered by clinicians in community clinics. Journal of Applied Behavior Analysis. 2008;41:517–526. doi: 10.1901/jaba.2008.41-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutzker JR, Campbell RV, Watson-Perczel M. Using the case study method to treat several problems in a family indicated for child neglect. Education and Treatment of Children. 1984;7:315–333. [Google Scholar]
- Lutzker JR, Edwards A. SafeCare®: Towards wide-scale implementation of a child maltreatment prevention program. International Journal Of Child Health And Human Development. 2009;2(1):7–15. [Google Scholar]
- Lutzker SZ, Lutzker JR, Braunling-McMorrow D, Eddleman J. Prompting to increase mother–baby stimulation with single mothers. Journal of Child and Adolescent Psychotherapy. 1987;4:3–12. [Google Scholar]
- Lutzker JR, Wesch D, Rice JM. A review of project “12-Ways”: an ecobehavioral approach to the treatment and prevention of child abuse and neglect. Adv Behav Res Ther. 1984;6(1):63–73. [Google Scholar]
- Metzger DS, Woody GE, Druley P, DePhillipis D, Navaline H, McLellan AT, O'Brien CP. Psychiatric symptoms, high risk behaviors and HIV positivity among methadone patients. NIDA Research Monograph. 1990;105:490–491. [PubMed] [Google Scholar]
- Metzger D, Woody G, Navaline H. The Risk Assessment Battery: Validity and Reliability.. Presented at the 6th Annual Meeting of the National Cooperative Vaccine Development Group for AIDS; Alexandria, Virginia. 1993. [Google Scholar]
- Milner JS. The child abuse potential inventory: Manual. 2nd ed. Psytec. Inc.; DeKalb: 1986. [Google Scholar]
- Nijhawan A, Kim S, Rich JD. Current Infectious Disease Report. Management of HIV Infection in Patients With Substance Use Problems. 2008;10(5):432–438. doi: 10.1007/s11908-008-0068-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niccols A, Milligan K, Smith A, Sword W, Thabane L, Henderson J. Integrated programs for mothers with substance abuse issues and their children: A systematic review of studies reporting on child outcomes. Child Abuse & Neglect. 2012;36(4):308–322. doi: 10.1016/j.chiabu.2011.10.007. doi:10.1016/j.chiabu.2011.10.007. [DOI] [PubMed] [Google Scholar]
- Ondersma SJ, Halinka Malcoeb, L., Simpson SM. Child protective services’ response to prenatal drug exposure: results from a nationwide survey. Child Abuse & Neglect. 2001:657–658. doi: 10.1016/s0145-2134(01)00235-6. [DOI] [PubMed] [Google Scholar]
- Ondersma S, Rawson RA, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamirie dependence. Addiction. 2004;99:708–718. doi: 10.1111/j.1360-0443.2004.00707.x. [DOI] [PubMed] [Google Scholar]
- Pelton LH. An examination of the reasons for child removal in Clark County, Nevada. Children And Youth Services Review. 2008;30(7):787–799. doi:10.1016/j.childyouth.2007.12.007. [Google Scholar]
- Pennar AL, Shapiro AF, Krysik J. Drug endangered children: Examining children removed from methamphetamine laboratoriesChildren and Youth Services Review. 2012;34:1777–1785. [Google Scholar]
- Romero V, Donohue B, Allen DN. Treatment of Substance Dependence, child neglect, and domestic violence: A single case examination utilizing Family Behavior Therapy. Journal of Family Violence. 2010;25:287–295. doi: 10.1007/s10896-009-9291-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero V, Donohue B, Hill HH, Powell S, Van Hasselt V, Azrin NH, Allen DN. Family Behavior Therapy for use in child welfare: Results of a case study involving an abused woman formally diagnosed with Alcohol Dependence, Bipolar Disorder, and several anxiety disorders. Clinical Case Studies. 2010;9:353–358. doi: 10.1177/1534650110383306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semidei J, Radel LF, Nolan C. Substance abuse and child welfare: Clear linkages and promising responses. Child Welfare. 2001;LXXX(2):109–128. [PubMed] [Google Scholar]
- Sheidow AJ, Donohue B, Hill HH, Henggeler SW, Ford JD. Development of an audio-tape review system for supporting adherence to an evidence-based practice. Professional Psychology Research & Practice. 2008;39:553–560. doi: 10.1037/0735-7028.39.5.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silovsky JF, Bard D, Chaffin M, Hecht D, Burris L, Owora A, Beasley L, Doughty D, Lutzker J. Prevention of child maltreatment in high-risk rural families: A randomized clinical trial with child welfare outcomes. Children and Youth Services Review. 2011;33:1435–1444. [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Humana Press; New Jersey: 1992. pp. 41–72. [Google Scholar]
- Sowder B, Burt M. Children of Heroin Addicts. Praeger; New York: 1980. [Google Scholar]
- Swenson C, Schaeffer CM, Henggeler SW, Faldowski R, Mayhew A. Multisystemic therapy for child abuse and neglect: A randomized effectiveness trial. Journal Of Family Psychology. 2010;24(4):497–507. doi: 10.1037/a0020324. doi:10.1037/a0020324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services . Administration on Children, Youth and Families, Children's Bureau. Child Maltreatment 2009. US Department of Health and Human Services; Washington, DC: 2010. [Google Scholar]
- U.S. Department of Health. Human Services ACF. Research to practice: Reducing re-referral in unsubstantiated child protective services cases. 2003 Retrieved from: http://www.childwelfare.gov/pubs/focus/researchtopractice.
- Urgelles J, Donohue B, Wilks C, Van Hasselt VB, Azrin NH. A Standardized Method of Preventing & Managing Emergencies in Child Welfare within the Context of Evidenced-Based Therapy. Behavior Modification. 2012;36:558–579. doi: 10.1177/0145445512448192. [DOI] [PubMed] [Google Scholar]
- Vinson DC, Reidinger C, Wilcosky T. Factors Affecting the Validity of a Timeline Follow-Back Interview. Journal Of Studies On Alcohol. 2003;64(5):733–740. doi: 10.15288/jsa.2003.64.733. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Slesnick N, Turner CW, Turner Brody JL, Peterson TR. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. Journal of Consulting and Clinical Psychology. 2001;5:802–813. [PubMed] [Google Scholar]
- Walker CA, Davies J. A critical review of the psychometric evidence base of the Child Abuse Potential Inventory. Journal of Family Violence. 2010;25:215–227. doi:10.1007/s10896-009-9285-9. [Google Scholar]
- Wang CT, Harding K. Current trends in child abuse reporting and fatalities the results of the 1998 annual fifty state survey. National Committee to Prevent Child Abuse; Chicago: 1999. [Google Scholar]
- Wasserman DR, Leventhal JM. Maltreatment of children born to cocaine-dependent mothers. American Journal of Diseases of Children. 1993;147(12):1324–1328. doi: 10.1001/archpedi.1993.02160360066021. [DOI] [PubMed] [Google Scholar]
- Watson-Perczel M, Lutzker JR, Greene BF, McGimpsey BJ. Assessment and modification of home cleanliness among families adjudicated for child neglect. Behavior Modification. 1988;12:57–81. doi: 10.1177/01454455880121003. [DOI] [PubMed] [Google Scholar]
- Wells K. Substance abuse and child maltreatment. Pediatrics Clinic of North America. 2009;56:345–362. doi: 10.1016/j.pcl.2009.01.006. [DOI] [PubMed] [Google Scholar]
- Yeaton WH, Schrest L. Critical dimensions in the choice and maintenance of successful treatments: Strength, integrity, and effectiveness. Journal of Consulting and Clinical Psychology. 1981;49:156–167. doi: 10.1037//0022-006x.49.2.156. [DOI] [PubMed] [Google Scholar]
- Young N, Boles S, Otero C. Parental Substance Use Disorders and Child Maltreatment: Overlap, Gaps, and Opportunities. Child Maltreatment. 2007;12:137–149. doi: 10.1177/1077559507300322. [DOI] [PubMed] [Google Scholar]