Abstract
Older adults often experience memory impairments, but can sometimes use selective processing and schematic support to remember important information. The current experiments investigate to what degree younger and healthy older adults remember medication side effects that were subjectively or objectively important to remember. Participants studied a list of common side effects, and rated how negative these effects were if they were to experience them, and were then given a free recall test. In Experiment 1, the severity of the side effects ranged from mild (e.g., itching) to severe (e.g., stroke), and in Experiment 2, certain side effects were indicated as critical to remember (i.e., “contact your doctor if you experience this”). There were no age differences in terms of free recall of the side effects, and older adults remembered more severe side effects relative to mild effects. However, older adults were less likely to recognize critical side effects on a later recognition test, relative to younger adults. The findings suggest that older adults can selectively remember medication side effects, but have difficulty identifying familiar but potentially critical side effects, and this has implications for monitoring medication use in older age.
Keywords: memory, aging, medications, side effects, older adults
When faced with large quantities of information, one often needs to be selective and prioritize the information to maximize the likelihood that important information is processed and later recalled. Older adults often take several different medications and may need to monitor all of the potential side effects of their medications. Side effect information can be quite extensive, and consists of long lists of potential side effects. Given the prevalence of medication usage in older adult populations (Qato et al., 2008), as well as college students’ increasing use of various medications for a variety of both mental and physical conditions and symptoms (White, Becker-Blease, & Grace-Bishop, 2006), it is critical to determine factors that can reduce the risks associated with the consumption of multiple medications. Thus, it is often necessary for people to accurately monitor and be aware of all of the potential side effects that are associated with a particular medication, and to know which side effects could be indicative of a serious complication. Given the fact that a majority of medications are associated with a lengthy list of potential side effects, one’s ability to remember these side effects can be paramount in monitoring one’s health.
This ability to recall important health-related information is particularly critical for older adults, who often experience memory deficits. The most pronounced age-related deficits are when remembering specific events or details (Zacks & Hasher, 2006), and associations among pairs of events or items (Chalfonte & Johnson, 1996; Naveh-Benjamin, 2000), and these deficits are often observed when older adults are presented with large amounts of to-be-remembered information, such as long lists of words (see Cohen, Sandler, & Schroeder, 1987). However, under some circumstances and conditions, older adults display preserved forms of memory (Zacks & Hasher, 2006; McDaniel, Einstein, & Jacoby, 2008), suggesting that not all memory abilities decline uniformly with age. For example, older adults can remember information that is related to previously learned semantic knowledge (e.g., Hess & Slaughter, 1990) and information that is consistent with relevant real-world conditions (Hess, 2005). That is, older adults can utilize schematic support, which is the use of prior knowledge or semantic memory to aid in the processing of new information and the facilitation of encoding and retrieval (Craik, 2002; Craik & Bosman, 1992; for a recent review see Umanath & Marsh, 2014). For example, Castel (2005) found that older adults, compared to younger adults, were equally able to remember realistic prices of grocery items (e.g., pickles $3.29) but were impaired for unrealistic pairings (e.g., ice cream $17.59), suggesting that prior knowledge, expectations, and goals may have a substantial impact on older adults’ memory. Additionally, Miller (2003) showed that older adults and younger adults with high levels of knowledge in the context of cooking recalled similar amounts of cooking-related text information, but older adults remembered less information than younger adults for domain-unrelated text passages about biology. Older adults also benefit from prior task success (Geraci & Miller, 2013), such that if older adults can succeed on certain memory tasks with relevant materials, age-related memory differences may be reduced. However, other work has shown limited or negligible effects of task experience, expertise, or schematic support, such as when older pilots were asked to remember air traffic control messages (Morrow, Menard, Stine-Morrow, Teller, & Bryant, 2001), or when prior knowledge could improve memory for prose passages or spatial layouts (Arbuckle, Cooney, Milne, & Melchior, 1994). Thus, it is unclear how and when certain forms of experience or knowledge, such as knowledge of common medication side effects, can influence older adults’ memory and potentially reduce age-related differences.
Theoretical frameworks regarding older adults’ ability to recall information deemed more important, realistic, or relevant suggests that older adults engage in “selective optimization with compensation”, allowing for the selective focus on important or goal-related information and activities, at the expense of less important or relevant information and activities (Baltes & Baltes, 1990; see also Backman & Dixon, 1992). This selectivity is particularly apparent within tasks that explicitly vary the objective value of the to-be-remembered information. According to a “value-directed remembering” framework (Castel, 2008; Castel, McGillivray, & Friedman, 2012), older adults can remember higher-value information as well as younger adults by selectively prioritizing and encoding this information over less important information (Castel, Benjamin, Craik, & Watkins, 2002; Castel et al., 2013). Furthermore, McGillivray and Castel (2011) demonstrated that both younger and older adults can learn to selectively choose to focus on and remember high value items when there are consequences associated with the failure to recall this higher value information. Thus, despite memory deficits, under some conditions older adults can efficiently learn to employ strategies that enhance recall of selected information. In the context of memory for medication side effects, the value-directed remembering framework could explain why older adults may remember some side effects better than others, in that certain specific side effects might be perceived as more subjectively valuable or important to the individual.
In prior research studies, important information was usually defined by association with objective point values that indicated higher reward values, and the point values were assigned by the experimenter. However, in many situations, the individual must decide what is important to remember. For example, when packing for a trip one needs to remember to pack certain important items, and older adults can selectively remember important items that are task relevant (McGillivray & Castel, under review). While prior research has examined how older adults can remember important information when the value is pre-assigned to items by the experimenter (see Castel, McGillivray, & Friedman, 2012, for a review), it is essential to examine situations in which participants themselves must decide what is more or less important to remember. This goal of “subjective” selectivity allows for the strategic allocation of attention towards what is deemed important by either the individual or the task setting (see also Hess, 2005; Stine-Morrow, 2007). Thus, importance can be defined objectively (generally important as stated by others or via reward) or subjectively (information that is important to the individual, specifically).
The current study examines whether the perceived importance of certain medication side effects influences younger and older adults’ ability to later remember these side effects. Often times, potential side effects are presented in rapid succession or in long lists, making it difficult to focus on and remember all of the side effects. However, in many cases, it is perhaps more critical to remember certain important or severe side effects, as opposed to attempting to remember all of the side effects. Thus, goals to selectively remember subjectively and objectively important and essential information could be particularly helpful to older adults when they are presented with a long list of potential side effects. In the present experiments, we examined whether younger and older adults could selectively remember side effects of a hypothetical medication. Participants studied a list of side effects and were told to remember the side effects for a later memory test. In Experiment 1, the severity of the presented side effects was manipulated (mild: brittle nails, cough; moderate: diarrhea, rash; severe: paralysis, heart attack), with participants providing a subjective rating of severity for each side effect while it was presented. In Experiment 2, despite all of the presented side effects being relatively mild or moderate in severity, their severity was objectively manipulated such that certain side effects were marked as ones that should be reported to a doctor immediately if experienced (contact your doctor, or “CYD”).
We were interested in whether age-related differences in the recall of side effects would be present, or if they may be small or negligible as a result of older adults’ use of schematic support. Due to older adults’ experience with taking medication and learning about the associated side effects in their everyday lives (Qato et al., 2008), older adults may be able to rely on schematic support in this context (Castel, 2005; Craik, 2002; Craik & Bosman, 1992; Hess, 2005; Miller, 2003; Umanath & Marsh, 2014). However, it is unclear whether participants in this task will remember some side effects better than others, based on the subjectively assigned negativity ratings, or the objective severity. Given that older adults typically encounter more physical health issues than younger adults (cf., Wolinsky & Johnson, 1991), they may construe the severe side effects as concerning. Thus, older adults may feel it is necessary to attend to (and remember) the severe side effects when visiting/reporting to a doctor. Based on the prior research on value-directed remembering (Castel, 2008; Castel et al., 2002), and the salience of experiencing certain side effects, we expect small or negligible age-related differences in recall for the severe side effects, and larger age-difference in recall for the moderate and mild side effects.. This may be a result of older adults selectively focusing on valuable information, in this case the severe side effects, in light of being aware that due to memory impairments, not all of the side effects will be recalled. As younger adults do not face concerns regarding memory impairments, younger adults may be less selective than older adults and try to remember all of the to-be-remembered information, and not prioritize more severe side effects over less severe ones.
Experiment 1
To examine potential age-related differences in memory for side effects, younger and older adult participants studied and recalled a list of common medication side effects that could be classified into three “severity” categories: mild, moderate, and severe. By manipulating the severity of side effects in this way, participants would likely give quantitatively different ratings to each side effect category-type, providing some evidence regarding how those objective categories and subjective ratings may impact memory performance. Although younger adults typically outperform older adults on most tests of free recall, age-related differences in memory might be reduced in the present task, due to the relative prior experience or schematic support older adults have with medication side effects. Thus, Experiment 1 allowed for the investigation of potential age-related differences or similarities in the ability to remember side effects, and to what degree recall would be influenced by the subjective ratings.
Method
Participants
Twenty-four undergraduate students (5 males, average age = 20.3) from the University of California, Los Angeles and 24 older adults (11 males, average age = 73.5) from the surrounding community were recruited for this task. Older adults were living independently in the Los Angeles area, and were recruited through community flyer postings as well as through the UCLA Cognition and Aging Laboratory Participant Pool. Older adults were compensated with $10 an hour for participation, while younger adults received course credit for their participation.
Materials
The materials consisted of 21 side effects that were selected from an internet database (http://www.vaughns-1-pagers.com/medicine/prescription-drug-side-effects.htm) for medication side effects. The selected side effects were classified into three separate severity categories: mild (e.g., itching), moderate (e.g., heartburn), and severe (e.g., stroke) side effects. Each side effect was categorized a priori based on the classification of the side effects in drug advertisements approved by the Food and Drug Administration, as well as by independent raters (two undergraduate students who were not participants) and the experimenters, into one of the three groups based on its severity, such that there were seven side effects in each severity category.
Procedure
Participants were told they were going to be shown a list of side effects for a new, hypothetical medication, one at a time. As each side effect was presented, participants were asked to rate how negative or unpleasant they felt experiencing each side effect would be for them on a scale from 1 to 10, where 1 = would not be an issue (not very concerning), and 10 = would be an extremely big issue (and very concerning) if they experienced that specific side effect. The term “issue” or “concern” was used to indicate and emphasize that the participant could use the entire scale as certain side effects may be more/less concerning for specific individuals or situations. After studying the side effects, they would be asked to recall as many of the side effects as they could, in any order. Participants saw each side effect in the center of the screen in black 44-point Arial font on a white background. Participants verbally provided a rating for each side effect during the 5 s for which it was on the screen, before the next side effect was shown. Participants were randomly assigned to view the list of side effects in one of four different fixed-randomized orders. The order of the side effects was blocked randomized such that within each block of three items, one side effect from each of the severity categories was presented. The order of each block was randomized across four versions of the experiment. Although the severity of the side effects was pre-determined, the three categories (i.e., mild, moderate, severe) were never explicitly mentioned to the participants. After studying the last side effect, participants had 1 min to verbally recall as many of the studied side effects as they could. The experimenter recorded their verbal responses. After completing the free recall task, two post-test questions were asked of participants: how did they try to remember the side effects they studied, and whether they pay attention to the side effects of medication they are currently taking or have taken in the past.
Results and Discussion
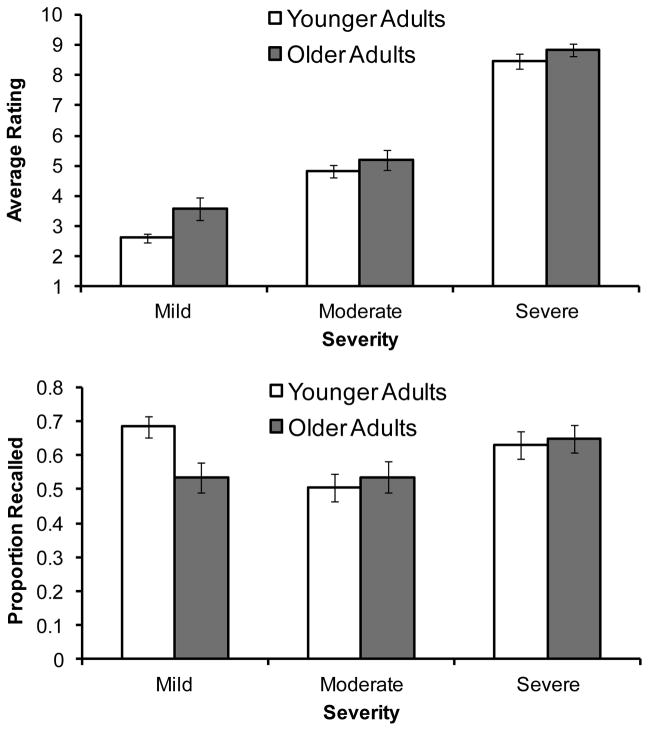
The average ratings assigned to the side effects and the proportions of side effects recalled by age group are shown in Figure 1. A 2 (Age Group: younger adults, older adults) × 3 (Severity Category: mild, moderate, severe) mixed ANOVA on ratings found a main effect of severity category, F(2, 92) = 561.45, MSE = .68, p < .001, ηG2 = .77, such that severe side effects (M = 8.65, SD = 1.07) were rated as more negative than moderate effects (M = 5.02, SD = 1.39), t(47) = 23.57, p < .001, d = 2.92, which in turn were rated as more negative than mild effects (M = 3.11, SD = 1.43), t(47) = 12.87, p < .001, d = 1.35. The effect of age group was not significant, F(1, 46) = 3.33, MSE = 3.59, p = .07, ηG2 = .05. The interaction between age groups and severity categories was non-significant, F(2, 92) = 2.09, MSE = .67, p = .13, ηG2 = .01. Given that older adults typically report more physical health issues than younger adults, and thus may construe the side effects as concerning, and necessary to attend to (and remember) when reporting to a doctor, we conducted post-hoc t-tests that indicated older adults rated mild side effects as more negative (M = 3.59, SD = 1.80) than did younger adults (M = 2.62, SD = 0.69), t(46) = 2.47, p = .02, d = .71, but the comparisons between younger and older adults’ ratings for moderate and severe side effects were similar (ts < 1.3).
Figure 1.
The mean ratings (top panel) and proportion recalled (bottom panel) of side effects in Experiment 1 based on the severity categories and age group of the participants. Error bars represent standard error of the mean.
The proportion of side effects recalled is shown in the lower portion of Figure 1. A 2 (Age Group: younger adults, older adults) × 3 (Severity Category: mild, moderate, severe) mixed ANOVA on recall found no significant effect of age group (F < 1), but an effect of severity, F(2, 92) = 4.91, MSE = .04, p < .01, ηG2 = .06, such that moderate side effects (M = .52, SD = .21) were recalled less often than mild (M = .61, SD = .20), t(47) = 2.03, p = .048, d = .43, or severe side effects (M = .64, SD = .19), t(47) = 2.84, p < .01, d = .59. Additionally, age group significantly interacted with severity category, F(2, 92) = 3.24, MSE = .04, p = .04, ηG2 = .04, such that older adults recalled a similar number of mild and moderate side effects, t(23) = 0.01, but more severe effects than mild effects, t(23) = 2.36, p < .05, d = .56, and marginally more of the moderate effects, t(23) = 2.01, p = .06, d = .54. Younger adults showed a different pattern of results, such that mild effects were recalled more often than moderate effects, t(23) = 3.36, p < .01, d = .96, while severe side effects were remembered marginally more often than moderate effects, t(23) = 1.97, p = .06, d = .62. Additionally, although a larger proportion of older adult participants (58%) reported that they pay attention to the listed side effects of medications they are currently taking relative to younger adults (38%), when we compared these two groups in terms of ratings and recall, there were no significant differences, although given the limited number of participants in each group, this type of analysis was limited by low power.
As an ancillary analysis, we further investigated the potential impact of participants’ severity ratings (i.e., subjective value) on their memory for specific side effects As subjective ratings were made on a trial-by-trial basis on a continuous scale, we conducted a trial-level mixed-effects modeling to examine the effects of subjective ratings, age group, and their interaction (Baayen, Davidson, & Bates, 2008; Murayama, Sakaki, Yan, & Smith, 2014). In this model, participants’ subjective ratings (standardized within individuals), age group, and rating by age interaction terms were included as trial-level predictors of memory performance, with participants and items being independent random effects. The model also included a quadratic effect of subjective ratings and its interaction with age group. We used a standard logit-link function to handle the dichotomous dependent variable (i.e., memory performance). The results from this analysis showed a significant positive quadratic effect, Exp (B) = 1.32, p < .01, indicating that subjective ratings have an overall nonlinear effect on memory performance. More importantly, there was a linear effect by age group interaction, Exp (B) = 1.17, p < .05, indicating that older adults had a higher linear slope, Exp (B) = 1.31, than younger adults, Exp (B) = 0.96. For reference, the exponential beta value, Exp (B), in generalized mixed-effects models can be interpreted in the same way as logistic regression analysis. Specifically, exponential beta is interpreted as the effect of the independent variable on the odds ratio of successful memory recall (i.e., the probability of recalling items divided by the probability of forgetting them). For example, Exp (B) = 1.17 means that the odds that an item is recalled is increased by 1.17 times as the standardized severity rating is increased by 1. After accounting for the overall quadratic trend, these findings suggest that older adults recalled more subjectively severe effects than moderate or mild effects whereas this trend was not observed in younger adults.
The results of this experiment illuminate an interesting relationship between subjective ratings (or value), age group, and memory. Specifically, older adults remembered more severe side effects than mild or moderate side effects. This pattern of results was found in both the ANOVA, as well as the mixed-effects modeling. However, younger adults showed a different pattern than older adults, in that they recalled as many mild side effects as they did severe side effects. This curvilinear relationship between value and memory has been found in other research (Madan & Spetch, 2012), and could be explained by two alternatives. The first explanation is that younger adults have better memory for extreme values, rather than only the high-value information (reward salience and reward value, respectively; see Madan & Spetch, 2012). The reward salience explanation is plausible, as participants were never provided with instructions to remember specific, important side effects over less important ones. The alternate explanation is one of relative experience. Namely, younger adults likely have had less experience with the moderate or severe side effects relative to the mild ones. As a result, younger adults may have elected to focus their encoding and rehearsal efforts on the side effects they had experienced in the past (i.e., the mild ones). Several participants (both younger and older) reported post-test that they tried to remember side effects they had previously experienced, giving this explanation some validity. Conversely, older adults may have relatively more experience with side effects from all three categories, simply having lived longer and having likely experienced more of these effects overall, which could explain why they selectively focused on only the severe side effects.
Consistent with the value-directed remembering framework (Castel, 2008), it may be that older adults elected to focus on the severe side effects because they could not remember everything that was studied, so they chose to focus on the side effects they felt were most important or were more harmful. Older adults may have also found the severe side effects to be more emotionally arousing than the mild or moderate side effects, thus leading to enhanced recall for these items, as such arousing information may garner additional attention and processing for older adults (Mather & Carstensen, 2003). Although this is typically found for emotionally-positive information for older adults, medication side effects may be viewed as more salient and emotional for older adults, due to any potential changes in health and/or more experience visiting doctors, possibly leading to enhanced elaborative processing or greater self-reference to one’s own experience with these symptoms.
Experiment 2
Experiment 2 was designed to investigate the extent to which younger and older adults could both recall and recognize objectively important side effect information. In Experiment 2, all of the side effects were relatively mild or moderate. However, within the instructions, participants were encouraged to selectivity attend to and remember specific side effects. Many contemporary medication advertisements come with warnings that certain mild side effects may be indicative of a severe complication. This warning, in effect, makes typically low-value information suddenly important to remember. Thus, some relatively mild side effects (e.g., sore throat) may be critical to remember, as they are indicative of a potentially life-threatening condition. Within Experiment 2, a subset of the side effects presented were labeled as important and should be immediately reported to a doctor if experienced (“contact-your-doctor” side effects, or “CYDs”). Memory for the side effects was assessed using a free recall test and was then followed by a recognition source memory task, in which participants had to identify which of the side effects were indicative of the severe complications (i.e., the CYD, contact-your-doctor effects). We refer to this as a source recognition task, as participants were NOT asked to identify all of the previously presented side effects (as might be the case in a typical recognition task), but rather to identify only the five CYD side effects among the group of 20 previously presented side effects.
While schematic support may facilitate recall, it is possible that older adults will have greater difficulty with the source recognition task compared with younger adults. Specifically, a lifetime of experience with the mild to-be-remembered side effects likely will lead to a greater degree of proactive interference when identifying the CYD effects. After all, why should a side effect like a cough, which an older adult has viewed their entire life as common and usually not important, suddenly become more important to remember than back pain? Such a finding may illustrate one potential cost of schematic support, in that older adults may be able to recall as much information as younger adults, yet may also have an inability to update the value of information in memory due to extensive proactive interference (cf. Friedman & Castel, 2013). In addition, work by Jacoby and colleagues has shown that older adults have relatively higher false alarm rates than younger adults due to a reliance on familiarity and not recollection (e.g., Jacoby, 1991; Jacoby, Bishara, Hessels, & Toth, 2005; Jacoby, Walheim, Rhodes, Daniels, & Rogers, 2010; Jones & Jacoby, 2005; Rhodes, Castel, & Jacoby, 2008). Thus, the use of familiarity on the source recognition test could lead to higher rates of false alarms for older adults.
Method
Participants
Twenty-four undergraduates (10 males, average age = 21.5) from the University of California, Los Angeles and 24 older adults (11 males, average age = 71.2) from the surrounding community were recruited for this task, and none of the participants had participated in Experiment 1. Older and younger adults were recruited and compensated in the same manner described in Experiment 1.
Materials
The materials were similar to those in Experiment 1 with the following exceptions: Twenty mild and moderate medication side effects (e.g., nausea, sweating, headache, etc.) were presented, such that all of the side effects selected for this experiment were temporary in their duration (although the selected side effects could occur chronically as well), such that they could be counterbalanced to be either CYD or non-CYD side effects.
Procedure
The procedure was similar to Experiment 1, in that side effects were studied and rated, followed by a free recall test. However, participants were instructed that a subset of the side effects that they studied, if experienced, were indicative of a serious complication, and that they would need to contact their doctor immediately if they experienced any of those specific symptoms (contact-your-doctor side effects, CYDs). That is, some of the to-be-remembered side effects were objectively made more valuable and important for the participant to remember relative to others, despite the fact that they could be mild or moderate in nature. Those objectively severe, or CYD, side effects were a subset of five of the 20 side effects, randomly selected across the entire list and counterbalanced across participants. The CYD side effects were shown in red font rather than black font to indicate that they were important for the participants to identify and later report. The order of the side effects studied was blocked randomized such that within each block of 4 side effects, one side effect was identified as a CYD effect.
Following the 1 min free recall test, participants engaged in a recognition source memory test to identify the five CYD side effects out of the 20 side effects initially studied. The experimenter read aloud the name of each side effect to the participant in the order in which they were presented during the learning portion of the experiment. As each side effect was read aloud, the participant had to respond by saying “yes” or “no” as to whether that specific side effect was one of the CYD side effects. After the participant made their judgment on the last side effect, he or she proceeded to answer the post-test questions used in Experiment 1 before being debriefed.
Results and Discussion
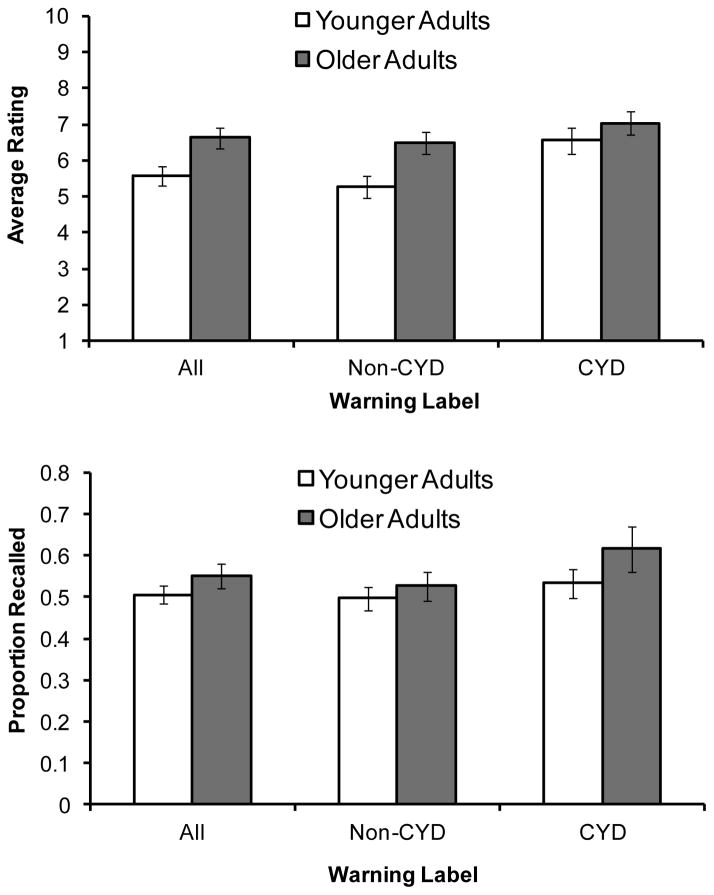
The mean proportion of recalled side effects and the average ratings assigned to the side effects based on age group and severity category are shown in Figure 2. A 2 (Age Group: younger adults, older adults) × 2 (Warning Category: non-CYD, CYD) mixed ANOVA on ratings found an effect of age group, F(1, 46) = 4.85, MSE = 3.63, p = .03, ηG2 = .07, such that older adults (M = 6.76, SD = 1.38) gave higher ratings to the side effects than younger adults (M = 5.91, SD = 1.32). There was a main effect of warning category, F(1, 46) = 13.12, MSE = 1.52, p = .001, ηG2 = .08, such that CYD side effects were rated more negatively (M = 6.79, SD = 1.21) than non-CYD side effects (M = 5.88, SD = 1.06). The interaction between age group and warning category was not significant, F(1, 46) = 2.20, p = .14.
Figure 2.
The mean ratings (top panel) and proportion recalled (bottom panel) of side effects in Experiment 2 based on the assigned warning categories and the age group of the participants. CYD refers to “Contact Your Doctor” if the participant were to experience these side effects. Since there were three times as many non-CYD side effects as there were CYD side effects, separate bars are shown to depict overall performance (“All”, shown on the left side of each graph) as well as the non-CYD and CYD side effects. Error bars represent standard error.
The proportions of side effects recalled based on age group and warning category is shown in the lower portion of Figure 2. Older adults remembered as many side effects as younger adults, while warning category only had a minor influence on recall. A 2 (Age Group: younger adults, older adults) × 2 (Warning Category: non-CYD, CYD) mixed ANOVA on recall found a non-significant effect of warning category, F(1, 46) = 2.51, MSE = .04, p = .12, ηG2 = .03, such that side effects that were categorized as CYD appeared to be recalled slightly more often than side effects not categorized as CYD, although the difference did not reach statistical significance. Both the main effect of age group and the interaction between age group and warning category were non-significant (ps > 0.15). One reason for the lack of an effect of warning label may be that items were intentionally counterbalanced in these conditions, thus controlling for item type, and making the only distinction being if the item was presented in red or black color. This would make the differentiation between CYD and non-CYD purely a feature binding task, and perhaps participants did not engage in processing that allowed for later retrieval of this information during recall.
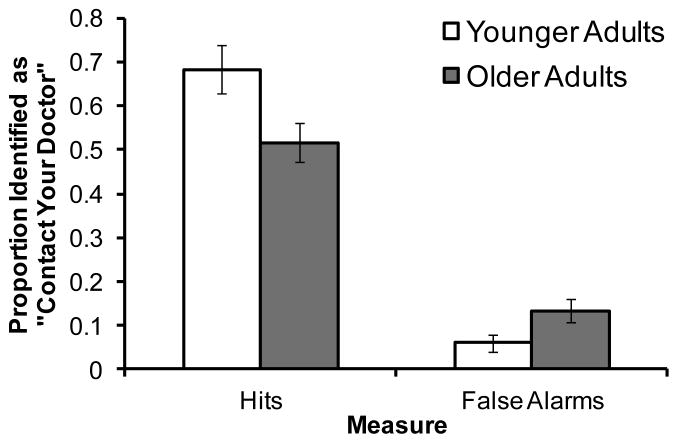
Mean proportions of side effects identified as “CYD” on the source recognition test are shown in Figure 3. A 2 (Age Group: younger adults, older adults) × 2 (Measure: hits, false alarms) mixed ANOVA revealed a main effect of measure, F(1, 46) = 152.07, MSE = .04, p < .001, ηG2 = .64, such that participants overall had more hits (M = .60, SD = .26) than false alarms (M = .10, SD = .12). Critically, age group interacted with measure, F(1, 46) = 8.58, MSE = .04, p < .01, ηG2 = .09. Older adults (M = .52, SD = .22) had significantly fewer hits than younger adults (M = .68, SD = .27), t(46) = 2.35, p = .02, d = .65, whereas the opposite pattern was found for false alarms, t(46) = 2.22, p = .03, d = .63, such that older adults (M = .13, SD = .13) misidentified more side effects as CYD than younger adults (M = .06, SD = .09). The above age group by measure interaction supports the claim that older adults may be more reliant on familiarity and not recollection when recognizing important information (e.g., Jacoby, 1991). Additionally the interaction illustrates that, while older adults are sensitive to remembering information based on its value (in free recall), they may also have difficulty binding that importance to specific side effect items. Consistent with the associative deficit hypothesis (see Naveh-Benjamin, 2000), the only feature that distinguished CYD and non-CYD items in the source recognition task were the color they were presented in at encoding, but the CYD items were not necessarily more severe. Lastly, although more older adults reported paying attention to the listed side effects of medications they are currently taking (67%) compared with younger adults (33%), this factor did not influence performance on either dependent measure of ratings or recall, nor performance on the source recognition test.
Figure 3.
The mean proportion of items identified as “CYD” (contact your doctor if you experience these side effects) in the source recognition task that followed the recall test in Experiment 2. Error bars represent standard error.
The results of Experiment 2 bear some similarities and some differences with the findings from Experiment 1. Importantly, there was no effect of age group on recall of the side effects, suggesting that older adults can remember side effects as well as younger adults, perhaps due to schematic support. However, there were differences between objective (i.e., CYD warnings) and subjective value (i.e., participants’ negativity ratings), and the degree to which this influenced recall. In the later source recognition test, hit and false alarm performance provides further evidence for gist-based memory in older adults (Koutstaal & Schacter, 1997) and also the use of familiarity contributing to false recognition in older adults (Jacoby, 1991; Rhodes et al., 2008). Younger adults were able to correctly identify more CYD side effects than older adults (i.e., hits), while older adults incorrectly identified more non-CYD side effects as CYD compared to younger adults (i.e., false alarms). This result is surprising given that older adults recalled as many CYD severe side effects as younger adults during the free recall test that occurred immediately prior to the source recognition test. Taken together, these findings may represent both the benefits (enhance free recall) and costs (greater false alarm rates) of schematic support for older adults when recalling and recognizing important side effect information.
General Discussion
The overall goal of the current studies was to explore the impact of different value types (i.e., objective and subjective) and the occurrence of value-directed remembering in the ecologically valid context of memory for medication side effects in younger and older adults. Across both experiments there was no effect of age on recall, a somewhat striking observation given that age-related effects on most other tests of free recall are usually quite pronounced. Importantly, in some cases, participants were sensitive to value in their memory for the side effects, but in other cases both young and older adults’ recall did not differentiate between side effect that that should be reported to a doctor (Contact Your Doctor, or CYD), and those that do not, when this information was demarked using a perceptual cue during encoding (red font). In addition in Experiment 2, identification of the “Contact Your Doctor” items in the source recognition test showed that older adults had a greater frequency of false alarms and fewer hits relative to younger adults.
The lack of age-related differences in free recall of side effect information may be due to older adults’ utilization of schematic support, or their relatively greater experience with medication and associated side effects, which could have assisted in their ability to recall the side effect information (Castel, 2005; 2007; Castel et al., 2013; Miller, 2003; Morrow, Leirer, Altieri, & Fitzsimmons, 1994; Umanath & Marsh, 2014). While there were no significant differences between those who reported usually attending to side effects when taking medication in real life and those who did not, it may be that side effects are more important in general for older adults to attend to, combined with greater experience with these effects, and this could lead to memory benefits via a survival (cf. Kang et al., 2012), or self-reference effect (cf. Gutchess, Kensinger, & Schacter, 2007). Older adults may also consider potential severe side effects as more life-threatening, and this could lead to an emotional component in terms of remembering this important information. In Experiment 2, older adults rated the side effects as more severe or negative overall compared to younger adults. Based on these relatively higher ratings, it stands to reason that older adults could have found the to-be-learned material to be more valuable, emotional, or important than younger adults did, which could have contributed to the negligible effects of age.
Older adults may have benefitted from contextual support in the present task (see also Hess, 2005), as well as the use of schematic support based on prior experience (e.g., Craik & Bosman, 1992; Castel, 2005). The results from the present study indicate that memory for medication side effects appears to be one domain in which older adults do not show large age-related declines, at least when tested immediately and when focusing on a single hypothetical medication. However, older adults do show a cost in terms of inaccurately recognizing certain side effects (as evidenced by greater false alarms relative to younger adults). Since the prevalence of medication usage increases in later adulthood, the need for additional awareness of medication-related issues such as memory for potential side effects is critical (Hines & Murphy, 2011; Moore, Whiteman, & Ward, 2007; Qato et al., 2008). Practically, this work may help doctors and medical providers better inform their patients about their prescribed medications, and help to organize treatment plans based on what symptoms or side effects the patient views are more severe or adverse (as side effects people perceive as more negative appear to be better remembered).
The results from the recognition source memory test in Experiment 2 provide support for the idea that older adults may rely more heavily on familiarity compared with younger adults when retrieving information (Jacoby 1991; Jacoby et al., 2005; 2010), in that they incorrectly identified significantly more side effects as the critical CYD effects compared to younger adults, illustrating one potential cost of schematic support. While prior research has shown that age-related differences in recognition are smaller than in recall (e.g., Craik & McDowd, 1987), older adults may be strategically recalling important side effects in the present task, and then relying on familiarity of the side effects on the later recognition test. Specifically, older adults may have greater difficulty updating the value or importance of to-be-remembered information (Friedman & Castel, 2013), and creating new associations with that information (Naveh-Benjamin, 2000), especially if competing yet irrelevant information has to be suppressed (inhibitory deficits; Hasher & Zacks, 1988; Lustig, Hasher, & Zacks, 2007).
It is possible that the source recognition test used in Experiment 2 may have been too difficult, in that older adults had to specifically remember which of these typically mild side effects were categorized as especially important and severe. Additionally, if all of the side effects were presented simultaneously during the test, then older adults may be able to use relative familiarity to identify the critical side effects, despite the side effects not usually being life-threatening. The “incongruency” between those two types of value cues (i.e., the side effect is usually not serious, but in this instance it is) may illustrate a potential cost of schematic support, as it creates interference when updating critical information that is typically considered less important. This finding is crucial when one considers the potential dangers associated with taking medications. It would also be important to assess confidence both during encoding and at test, when participants recall and recognize potentially life-threatening side effects. Older adults, in particular, may have difficulty recognizing that they are experiencing a potentially life-threating side effect that is typically considered or thought to be subjectively mild, or could misidentify the symptoms of a less serious side effect as something requiring immediate medical attention.
In the present study, both younger and older adults were able to effectively remember important side effect information. We note that the current work examined relatively short-term memory for side effects; future research could examine these issues using longer delays (days or weeks), or use side effects that could vary in terms of frequency or duration. Also, it maybe that if given more time to recall all items (without attention to value), then older adults would recall some of the lower value items, or perhaps be able to recognize them on a later recognition test. Further examination of the specific role of emotion or anxiety associated with remembering side effects would be informative, to determine how emotional value might be related to later recall. Future research could also include a stronger cue or event-based prospective memory component (use of multiple drugs and various combinations of side effects) to better reflect real-world medication use. The investigation of prospective memory may be especially critical as it is often necessary for one to later report experienced (and either subjectively or objectively important) side effects to their physician (see Einstein & McDaniel, 1990; Henry, MacLeod, Phillips, & Crawford, 2004; Liu & Park, 2004; McDaniel & Einstein, 2007; Scullin, Bugg, & McDaniel, 2012; Webb et al., 2008; Zogg et al., 2012). This area of research has the potential to benefit both younger and older adults, and to provide practical and theoretical insight regarding how people can selectively remember important medication-related information.
Acknowledgments
We thank Monika Holser, Stephanie Knipprath, and Angel Wu for help with data collection, and Barbara Knowlton, Douglas Bell, and Robert Bjork for helpful comments. This research was conducted in partial fulfillment of a doctoral dissertation by Michael C. Friedman at the University of California, Los Angeles. This research was supported in part by the National Institutes of Health (National Institute on Aging), Award Number R01AG044335.
Footnotes
This research was presented at the 15th Biennial Cognitive Aging Conference, Atlanta, GA.
References
- Arbuckle TY, Cooney R, Milne J, Melchior A. Memory for spatial layouts in relation to age and schema typicality. Psychology and Aging. 1994;9:467–480. doi: 10.1037//0882-7974.9.3.467. [DOI] [PubMed] [Google Scholar]
- Backman L, Dixon RA. Psychological compensation: A theoretical framework. Psychological Bulletin. 1992;112:259–283. doi: 10.1037/0033-2909.112.2.259. [DOI] [PubMed] [Google Scholar]
- Baltes PB, Baltes MM. Psychological perspectives on successful aging: The model of selective optimization with compensation. In: Baltes PB, Baltes MM, editors. Successful aging: Perspectives from the behavioral sciences. New York, NY: Cambridge University Press; 1990. pp. 1–34. [Google Scholar]
- Baayen RH, Davidson DJ, Bates DM. Mixed-effects modeling with crossed random effects for subjects and items. Journal of Memory and Language. 2008;59:390–412. [Google Scholar]
- Castel AD. Memory for grocery prices in younger and older adults: The role of schematic support. Psychology and Aging. 2005;20:718–721. doi: 10.1037/0882-7974.20.4.718. [DOI] [PubMed] [Google Scholar]
- Castel AD. Aging and memory for numerical information: The role of specificity and expertise in associative memory. Journal of Gerontology: Psychological Sciences. 2007;62:194–196. doi: 10.1093/geronb/62.3.p194. [DOI] [PubMed] [Google Scholar]
- Castel AD. The adaptive and strategic use of memory by older adults: Evaluative processing and value-directed remembering. In: Benjamin AS, Ross BH, editors. The psychology of learning and motivation. Vol. 48. London: Academic Press; 2008. pp. 225–270. [Google Scholar]
- Castel AD, Benjamin AS, Craik FIM, Watkins MJ. The effects of aging on selectivity and control in short-term recall. Memory & Cognition. 2002;30:1078–1085. doi: 10.3758/bf03194325. [DOI] [PubMed] [Google Scholar]
- Castel AD, Murayama K, Friedman MC, McGillivray S, Link I. Selecting valuable information to remember: Age-related differences and similarities in self-regulated learning. Psychology and Aging. 2013;28:232–242. doi: 10.1037/a0030678. [DOI] [PubMed] [Google Scholar]
- Castel AD, McGillivray S, Friedman MC. Metamemory and memory efficiency in older adults: Learning about the benefits of priority processing and value-directed remembering. In: Naveh-Benjamin M, Ohta N, editors. Memory and aging: Current issues and future directions. New York: Psychology Press; 2012. pp. 245–270. [Google Scholar]
- Chalfonte BL, Johnson MK. Feature memory and binding in young and older adults. Memory & Cognition. 1996;24:403–416. doi: 10.3758/bf03200930. [DOI] [PubMed] [Google Scholar]
- Cohen RL, Sandler SP, Schroeder K. Aging and memory for words and action events: effects of item repetition and list length. Psychology and Aging. 1987;2:280–285. doi: 10.1037//0882-7974.2.3.280. [DOI] [PubMed] [Google Scholar]
- Craik FIM. Human memory and aging. In: Backman L, von Hofsten C, editors. Psychology at the turn of the millennium. Hove, UK: Psychology Press; 2002. pp. 261–280. [Google Scholar]
- Craik FIM, Bosman BA. Age-related changes in memory and learning. In: Bouma H, Graafmans JAM, editors. Gerontechnology. Amsterdam: IOS Press; 1992. pp. 79–92. [Google Scholar]
- Craik FIM, McDowd JM. Age differences in recall and recognition. Journal of Experimental Psychology: Learning, Memory, and Cognition. 1987;13:474. [Google Scholar]
- Einstein GO, McDaniel MA. Normal aging and prospective memory. Journal of Experimental Psychology: Learning, Memory, and Cognition. 1990;16:717–726. doi: 10.1037//0278-7393.16.4.717. [DOI] [PubMed] [Google Scholar]
- Friedman MC, Castel AD. Memory, priority encoding, and overcoming high-value proactive interference in younger and older adults. Aging, Neuropsychology, and Cognition. 2013;20:660–683. doi: 10.1080/13825585.2012.762083. [DOI] [PubMed] [Google Scholar]
- Geraci L, Miller TM. Improving older adults’ memory performance using prior task success. Psychology and Aging. 2013;28:340. doi: 10.1037/a0030332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutchess AH, Kensinger EA, Schacter DL. Aging, self-referencing, and medial prefrontal cortex. Social Neuroscience. 2007;2:117–133. doi: 10.1080/17470910701399029. [DOI] [PubMed] [Google Scholar]
- Hasher L, Zacks RT. Working memory, comprehension, and aging: A review and a new view. In: Bower GH, editor. The psychology of learning and motivation. Vol. 22. New York, NY: Academic Press; 1988. pp. 193–225. [Google Scholar]
- Henry JD, MacLeod MS, Phillips LH, Crawford JR. A meta-analytic review of prospective memory and aging. Psychology and Aging. 2004;19:27–39. doi: 10.1037/0882-7974.19.1.27. [DOI] [PubMed] [Google Scholar]
- Hess TM. Memory and aging in context. Psychological Bulletin. 2005;131:383–406. doi: 10.1037/0033-2909.131.3.383. [DOI] [PubMed] [Google Scholar]
- Hess TM, Slaughter SJ. Schematic knowledge influences on memory scene information in young and older adults. Developmental Psychology. 1990;26:855–865. [Google Scholar]
- Hines LE, Murphy JE. Potentially harmful drug drug interactions in the elderly: A review. American Journal of Geriatric Pharmacotherapy. 2011;9:364–377. doi: 10.1016/j.amjopharm.2011.10.004. [DOI] [PubMed] [Google Scholar]
- Jacoby LL. A process dissociation framework: Separating automatic from intentional uses of memory. Journal of Memory and Language. 1991;30:513–541. [Google Scholar]
- Jacoby LL, Bishara AJ, Hessels S, Toth JP. Aging, subjective experience, and cognitive control: Dramatic false remembering by older adults. Journal of Experimental Psychology: General. 2005;134:131–148. doi: 10.1037/0096-3445.134.2.131. [DOI] [PubMed] [Google Scholar]
- Jacoby LL, Wahlheim CN, Rhodes MG, Daniels KA, Rogers CS. Learning to diminish the effects of proactive interference: Reducing false memory for young and older adults. Memory & Cognition. 2010;38:820–829. doi: 10.3758/MC.38.6.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones TC, Jacoby LL. Conjunction errors in recognition memory: Modality-free errors for older adults but not for young adults. Acta Psychologica. 2005;120:55–73. doi: 10.1016/j.actpsy.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Kang SHK, McDermott KB, Cohen SM. The mnemonic advantage of processing fitness-relevant information. Memory & Cognition. 2008;36:1151–1156. doi: 10.3758/MC.36.6.1151. [DOI] [PubMed] [Google Scholar]
- Koutstaal W, Schacter DL. Gist-based false recognition of pictures in older and younger adults. Journal of Memory and Language. 1997;37(4):555–583. [Google Scholar]
- Liu LL, Park DC. Aging and medical adherence: The use of automatic processes to achieve effortful things. Psychology and Aging. 2004;19:318–325. doi: 10.1037/0882-7974.19.2.318. [DOI] [PubMed] [Google Scholar]
- Lustig C, Hasher L, Zacks RT. Inhibitory deficit theory: Recent developments in a “new view”. American Psychological Association; Washington, DC: 2007. pp. 145–162. [Google Scholar]
- Madan CR, Spetch ML. Is the enhancement of memory due to reward driven by value or salience? Acta Psychologica. 2012;139:343–349. doi: 10.1016/j.actpsy.2011.12.010. [DOI] [PubMed] [Google Scholar]
- Mather M, Carstensen LL. Aging and attentional biases for emotional faces. Psychological Science. 2003;14:409–415. doi: 10.1111/1467-9280.01455. [DOI] [PubMed] [Google Scholar]
- McDaniel MA, Einstein GO. Prospective memory components most at risk for older adults and implications for medication adherence. American Psychological Association; Washington, DC: 2007. pp. 49–75. [Google Scholar]
- McDaniel MA, Einstein GO, Jacoby LL. New considerations in aging and memory: The glass may be half full. In: Craik FIM, Salthouse T, editors. The Handbook of Aging and Cognition. 3. Hove: Psychology Press; 2008. pp. 255–310. [Google Scholar]
- McGillivray S, Castel AD. Betting on memory leads to metacognitive improvement in younger and older adults. Psychology and Aging. 2011;26:137–142. doi: 10.1037/a0022681. [DOI] [PubMed] [Google Scholar]
- McGillivray S, Castel AD. Older and younger adults’ strategic control of metacognitive monitoring: The role of consequences, task experience, and prior knowledge. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LMS. The effects of age and domain knowledge on text processing. Journals of Gerontology: Psychological Sciences. 2003;58:217–222. doi: 10.1093/geronb/58.4.p217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AA, Whiteman EJ, Ward KT. Risks of combined alcohol/medication use in older adults. American Journal of Geriatric Pharmacotherapy. 2007;5:64–74. doi: 10.1016/j.amjopharm.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow DG, Leirer VO, Altieri PA, Fitzsimmons C. When expertise reduces age differences in performance. Psychology and Aging. 1994;9:134–148. doi: 10.1037//0882-7974.9.1.134. [DOI] [PubMed] [Google Scholar]
- Morrow DG, Menard WE, Stine-Morrow EAL, Teller T, Bryant D. The influence of expertise and task factors on age-differences in pilot communication. Psychology and Aging. 2001;16:31–46. doi: 10.1037/0882-7974.16.1.31. [DOI] [PubMed] [Google Scholar]
- Murayama K, Sakaki M, Yan VX, Smith GM. Type-1 error inflation in the traditional by-participant analysis to metamemory accuracy: A generalized mixed-effects model perspective. Journal of Experimental Psychology: Learning, Memory, & Cognition. 2014;40:1287–1306. doi: 10.1037/a0036914. [DOI] [PubMed] [Google Scholar]
- Naveh-Benjamin M. Adult-age differences in memory performance: Tests of an associative deficit hypothesis. Journal of Experimental Psychology: Learning, Memory and Cognition. 2000;26:1170–1187. doi: 10.1037//0278-7393.26.5.1170. [DOI] [PubMed] [Google Scholar]
- Qato DM, Alexander GC, Conti RM, Johnson M, Schumm P, Lindau ST. Use of prescription and over-the-counter medications and dietary supplements among older adults in the united states. JAMA: Journal of the American Medical Association. 2008;300:2867–2878. doi: 10.1001/jama.2008.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes MG, Castel AD, Jacoby LL. Associative recognition of face pairs by younger and older adults: The role of familiarity-based processing. Psychology and Aging. 2008;23:239–249. doi: 10.1037/0882-7974.23.2.239. [DOI] [PubMed] [Google Scholar]
- Scullin MK, Bugg JM, McDaniel MA. Whoops, I did it again: Commission errors in prospective memory. Psychology and Aging. 2012;27:46–53. doi: 10.1037/a0026112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stine-Morrow EA. The Dumbledore hypothesis of cognitive aging. Current Directions in Psychological Science. 2007;16:295–299. [Google Scholar]
- Umanath S, Marsh EJ. Understanding how prior knowledge influences memory in older adults. Perspectives on Psychological Science. 2014;9:408–426. doi: 10.1177/1745691614535933. [DOI] [PubMed] [Google Scholar]
- Webb J, Davis TC, Bernadella P, Clayman ML, Parker RM, Adler D, Wolf MS. Patient-centered approach for improving prescription drug warning labels. Patient Education and Counseling. 2008;72:443–449. doi: 10.1016/j.pec.2008.05.019. [DOI] [PubMed] [Google Scholar]
- White BP, Becker-Blease KA, Grace-Bishop K. Stimulant medication use, misuse, and abuse in an undergraduate and graduate student sample. Journal of American College Health. 2006;54:261–268. doi: 10.3200/JACH.54.5.261-268. [DOI] [PubMed] [Google Scholar]
- Wolinsky FD, Johnson RJ. The use of health services by older adults. Journal of Gerontology. 1991;46:S345–S357. doi: 10.1093/geronj/46.6.s345. [DOI] [PubMed] [Google Scholar]
- Zacks RT, Hasher L. Aging and long-term memory: Deficits are not inevitable. In: Bialystok E, Craik FIM, editors. Lifespan cognition: Mechanisms of change. New York, NY: Oxford University Press; 2006. pp. 162–177. [Google Scholar]
- Zogg JB, Woods SP, Sauceda JA, Wiebe JS, Simoni JM. The role of prospective memory in medication adherence: A review of an emerging literature. Journal of Behavioral Medicine. 2012;35:47–62. doi: 10.1007/s10865-011-9341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]