Abstract
Objective
To assess the impact of a pharmacy benefit change on mail order pharmacy (MOP) uptake.
Data Sources/Study Setting
Race-stratified, random sample of diabetes patients in an integrated health care delivery system.
Study Design
In this natural experiment, we studied the impact of a pharmacy benefit change that conditionally discounted medications if patients used MOP and prepaid two copayments. We compared MOP uptake among those exposed to the benefit change (n = 2,442) and the reference group with no benefit change (n = 8,148), and estimated differential MOP uptake across social strata using a difference-in-differences framework.
Data Collection/Extraction Methods
Ascertained MOP uptake (initiation among previous nonusers).
Principal Findings
Thirty percent of patients started using MOP after receiving the benefit change versus 9 percent uptake among the reference group (p < .0001). After adjustment, there was a 26 percentage point greater MOP uptake (benefit change effect). This benefit change effect was significantly smaller among patients with inadequate health literacy (15 percent less), limited English proficiency (14 percent less), and among Latinos and Asians (24 and 16 percent less compared to Caucasians).
Conclusions
Conditionally discounting medications delivered by MOP effectively stimulated MOP uptake overall, but it unintentionally widened previously existing social gaps in MOP use because it stimulated less MOP uptake in vulnerable populations.
Keywords: Mail order pharmacy, pharmacy benefit designs, comparative effectiveness, health disparities, difference-in-differences, marginal structural model, inverse probability treatment weighting
Mail order pharmacies (MOPs) dispense medications by mail to the patient's home, offering convenience and eliminating access barriers (e.g., time, mobility, transportation), the benefits of which may be compounded for patients using multiple medications (Choudhry et al. 2011). Currently, one-third of all chronic disease prescriptions in the United States are dispensed by mail (Wroblewski et al. 2005). We have previously demonstrated better adherence (Duru et al. 2010), better LDL-C control (Schmittdiel et al. 2011), and no substantive safety concerns (Schmittdiel et al. 2013) among diabetic patients using MOPs. Better adherence among those using MOPs has been reported in other studies as well (Devine, Vlahiotis, and Sundar 2010; Zhang et al. 2011; Visaria, Frazee, and Devine 2012).
Compared to walk-in pharmacies, MOPs can also be cost-saving for the health plan, depending on differential wastage rates between the two delivery modes, the cost of increased drug utilization, and the size of any MOP incentives (Carroll et al. 2005; Carroll 2006; Valluri et al. 2007; Devine, Vlahiotis, and Sundar 2010). The World Health Organization recommends seeking effective and low-cost, structural (system-level) approaches to improving adherence as an alternative to the frequently expensive, individual-level interventions (Sabate 2003). Financial incentives for MOPs may represent such a system-level approach if they increase the use of MOPs and secondarily improve adherence and health outcomes.
However, structural changes can simultaneously improve population-level quality metrics, while also increasing social inequalities in health access and outcomes. We have previously reported lower use of MOPs among minorities and those living in deprived neighborhoods (Duru et al. 2010). While MOP use has been increasing steadily over the past two decades (Carroll et al. 2005), underuse in vulnerable groups has been observed at Kaiser Permanente Northern California (KPNC) since MOPs were introduced in 1999 (unpublished data). For example, in 2000, the prevalence of MOP use was 11 percent in Latinos, 12 percent in African Americans and Filipinos, 20 percent in Asians, and 24 percent in Caucasians. A decade later, in 2010, MOP use grew considerably, but it still lagged substantially in minorities: 37 percent in Latinos and African Americans, 46 percent in Filipinos, 63 percent in Asians, and 65 percent in Caucasians. It remains unknown whether and how financial incentives might impact disparities in MOP use (Trinacty et al. 2009).
We studied a natural experiment which included a pharmacy benefit change that increased cost sharing but promoted the use of MOPs by discounting medications (i.e., reducing the increase in out-of-pocket costs) if patients prepaid two copayments and refilled using MOPs. We evaluated the following: (1) the overall effect of rolling out the benefit change on subsequent uptake of MOPs for dispensing of cardiometabolic medications among patients with diabetes, and (2) whether the rollout's effect on MOP uptake was uniform across social strata (defined by ethnicity, educational attainment, household income, English proficiency, or health literacy).
Methods
Setting
This study was conducted in KPNC, an integrated, health care delivery system that provides medical care to ∽3 million members (∽30 percent of the population of the catchment, with ethnic and socioeconomic distributions similar to the general population, although fewer very poor or rich members) (Gordon and Kaplan 1991).
KPNC health plan pharmacy benefits are available only through KPNC's ∽120 community pharmacies or, since 1999, via MOPs. Although most new prescriptions are first dispensed at community pharmacies (Valluri et al. 2007), KPNC patients may also fill new prescriptions by mail, with telephone access to a pharmacist who can answer medication-related questions after completing a simple enrollment process (by mail, phone, or website). Unlike some MOP systems, KPNC patients must request (by mail, phone, or website) each MOP dispensing and provide payment in advance (by credit card or check) before the medication is mailed (no automatic refills). Medications usually arrive within 1 week.
Intervention
Prior to January 1, 2006, the standard KPNC drug plan for all subjects required one copayment per dispensing (regardless of days' supply or mode of delivery). Effective January 1, 2006, all individual Medicare Senior Advantage members and select commercial and employer groups were changed to a new, less generous drug benefit package (more cost sharing), which also included an incentive, in the form of a prepayment discount, to use MOPs. The change in drug benefit was not a matter of individual choice but rather based on employer group contracts. Impacted health plan members, which typically included more socially vulnerable subjects, were mailed an announcement describing the benefit changes and the MOP discount; originally in English only, translated versions of the announcement were available in the following year. The new benefit provided a 1-, 2-, or 3-month supply at community pharmacies at a charge of one, two, or three copayments, respectively. Alternatively, patients could use MOPs and receive a 1-month supply for one copayment or use the prepaid discount which incentivized use of MOPs by receiving a 3-month supply for two copayments (Figure1). Thus, a patient who was willing and able to prepay two copayments would receive a 100-day supply from the MOP compared with a 60-day supply from the walk-in pharmacy (i.e., 40 extra days' supply for using MOPs).
Figure 1.
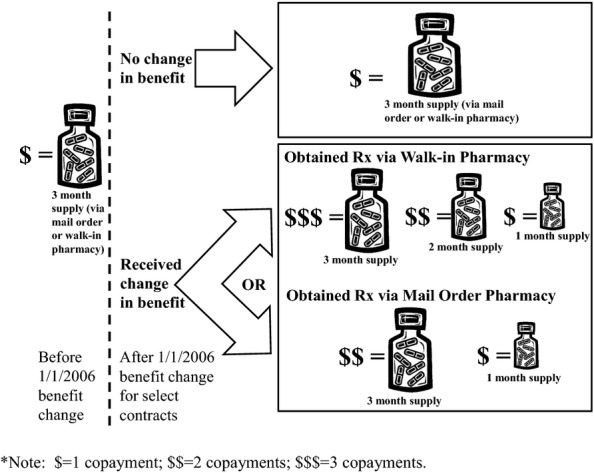
Impact of the January 1, 2006, Benefit Change for Select Patients on Their Cost Sharing and Duration of Supply Dispensed for Patients Obtaining Their Medications via Walk-in versus Mail Order Pharmacy. (Note that the copayment* per dispensing varies—typically from $5 to $15 per copayment—and depends on the individual's contract)
To illustrate, consider a scenario among patients whose benefits contract had stipulated a $10 copayment per dispensing (typically, a 3-month supply); that is, prior to the January 1, 2006 benefit change, all patients would have been charged $10 for each dispensing of a standard 3-month supply, regardless of whether they used a walk-in pharmacy or MOP. Among those patients who had no change in benefits, that copayment remained unaltered after January 1, 2006. In contrast, patients who had a benefit change would now pay $10 for each 1-month supply; however, they could get a better deal if they used the MOP and requested three 1-month supplies. That is, patients with the benefit change who obtained their medications via walk-in pharmacy would pay $10 for each 1-month supply. However, if they chose to use MOPs, they would pay $10 for each 1-month supply, or $20 for a 3-month supply. Thus, the mail order prepayment discount permitted them to pay one copayment less ($10 in this scenario) for a 3-month supply compared to using a walk-in pharmacy. Thus, their cost share for a 3-month supply changed from $10 (before the change) to $30 for medications obtained via walk-in pharmacy or $20 for medications obtained via MOPs. Therefore, the prepayment discount to use MOPs did not offset the increase in cost sharing for those switched to the new, less generous benefit.
Participants
Study subjects were drawn from a cohort of 20,188 adults who were respondents (62 percent response rate) in the Diabetes Study of Northern California (DISTANCE) Survey, an ethnically stratified, random sample of diabetes members identified prior to January 1, 2005 (Moffet et al. 2008). The DISTANCE survey was offered in English, Spanish, Mandarin, Cantonese, or Tagalog and included a wide range of social factors that we hypothesized to be associated with social disparities in health care use and outcomes. To study the effect of the pharmacy benefit change among nonusers of MOPs, we limited the study population to diabetes patients not offered incentives to use MOPs nor using MOPs prior to baseline, and dispensed at least one of the cardiometabolic medications used as primary treatment for diabetes patients (antiglycemic, antihypertensive, or lipid-lowering). Thus, we excluded the 5,216 subjects who used MOPs during the 12 months prior to baseline (January 1, 2006); we also excluded 1,131 subjects not dispensed any cardiometabolic medication during the 2 years prior to baseline (January 1, 2004–December 31, 2005) or during the year after baseline (January 1, 2006–December 31, 2006), and 3,251 who either lacked continuous Kaiser membership or a standard pharmacy benefit contract throughout the observation window. This yielded an analytic sample of 10,590 subjects, of which 2,442 (23 percent) had a benefit change and 8,148 (77 percent) had no change, serving as the reference group.
Outcomes and Follow-Up
Initiation of MOP use (“uptake”) was defined as having at least one MOP dispensing for a cardiometabolic medication in the 12 months after baseline (among previous nonusers). Our goal was to estimate the effect of the pharmacy benefit change on MOP uptake overall and across social groups defined by self-reported ethnicity, educational attainment, annual income, self-reported financial hardship (self-reported difficulties purchasing needed medications [Chien-Wen et al. 2002], medical supplies, or food [Ross and Wu 1995] due to insufficient funds), limited English proficiency (always or often having problems speaking or reading English), and a validated measure of health literacy (problems understanding health education materials or instructions; Chew, Bradley, and Boyko 2004).
Statistical Analysis
We used a difference-in-differences (DID) framework to study the impact of the benefit change on mail order uptake (“benefit change effect”). This benefit change effect was then contrasted (again using DID) across social groups by estimating the adjusted, absolute difference between the benefit change effect for any given social group and the reference social category (e.g., benefit change effects for African American minus benefit change effects for Caucasian); this estimate was called the “effect difference.” DID is a quasi-experimental approach used to study change in an outcome before and after an intervention, after “netting out” the background change in rates due to effect of secular time trends and aging on that same outcome identified in a reference group who was not affected by the intervention (Campbell and Stanley 1963; Meyer 1995). Regression to the mean is not a concern given both exposed and reference group have the identical starting point (none are MOP users at baseline). In the context of this study, the benefit change effect on mail order uptake was estimated by the uptake during the year following the benefit change after subtracting the background secular time trends estimated by MOP uptake in those not experiencing the benefit change (reference group).
DID rests on the assumption that the unobservable (i.e., counterfactual) outcome in the exposed group, if they had not been exposed to the intervention, would be qualitatively similar to the observable outcome in the unexposed reference group. That is, if the group exposed to the changes in the benefits had (counterfactually) not been exposed to those benefit changes, then we assume their MOP uptake would be similar to that observed in the reference group. We examined the validity of the DID assumption by evaluating the MOP uptake in 2005 (the year prior to the exposure) among subjects who had no MOP use as of January 1, 2006, selecting the “soon-to-be-exposed” subjects who would receive the benefit change in January 1, 2006, and comparing them to the remaining subjects (i.e., no benefit change in 2006) who made up the reference group. The 2005 rates of uptake of MOP in these two groups prior to the implementation of the new benefit design were similar, although not identical. There was a modestly larger MOP uptake among those who would later receive a change in benefits versus the reference group (1.38 vs. 1.04 percentage points per month, respectively). Although the 2005 population used for this test of assumptions was not identical to the population used for the final analysis (as we excluded those who started using MOPs during 2005 prior to the January 1, 2006 baseline), the qualitatively similar uptake suggests that the DID assumption should be reasonable. While selection into groups receiving the different benefit packages could introduce bias in the estimate of the benefit effect, this bias is assumed uniform across social groups and thus should not impact the estimate of benefit effect differences across social groups in a substantive way. However, while we present the quantitative DID results below, we will interpret those findings strictly as qualitative given this is an evaluation of a natural experiment that rests on unobservable assumptions.
We addressed potential confounding from measured and unmeasured risk factors by using each treated group as its own control, comparing potentially confounding risk factors before versus after the benefit change use during our study, and by controlling for demographic and clinical differences between those with the benefit change versus the reference group. Those prevalent differences were accounted for using a marginal structural modeling (MSM) approach based on the counterfactual theory of causality (Robins 1999; Mortimer et al. 2005). The adjusted MSM models were weighted using a propensity score method called inverse probability of treatment weights (IPTW). The IPTW were derived from a pooled logistic regression model (R2 = 77 percent): benefit change (yes/no) was regressed on baseline age, pharmacy copay for generic and brand medications, Medicare indicator, pharmacy benefit deductible indicator, pharmacy benefit business line (e.g., large employer group, small employer group, strategic group), ethnicity, income, education, limited English proficiency, inadequate health literacy, or financial hardship. This weighting aligns the distribution in the comparison cohort of the variables used in the benefit change-probability model to match the distribution in the exposed group who experienced the benefits change. These estimates are unconfounded by the above adjustment variables under the assumption that the model is specified correctly. Models were further weighted to account for survey nonresponse (Horvitz and Source 1952) and the nonproportional sampling fractions (complex survey design). We estimated the adjusted, absolute benefit change effect (difference-in-differences) by specifying modified Poisson regression models (Zou 2004) with robust standard errors and an identity link function (Cheung 2007). Confidence intervals were estimated using bootstrapping. We also conducted sensitivity analysis after excluding the 6 percent (n = 991) of patients whose expenditures exceeded that covered by Medicare Part D (i.e., those reaching the coverage limit or “doughnut hole”) during follow-up because financial incentives to use MOPs would no longer be relevant while in the gap.
Results
Subject Characteristics
The mean age of the subjects was 60 years, 50 percent were women, 80 percent minorities, 12 percent had limited English proficiency, and 46 percent had inadequate health literacy (Table1). Twenty-one percent had annual income <$25,000 and 38 percent self-reported difficulties paying for medications. Compared to the reference group, subjects who had a pharmacy benefit change had lower educational attainment, lower income, greater financial hardships, and more likely to have limited English proficiency, inadequate health literacy, and higher out-of-pocket costs for their cardiometabolic medications in the year prior to baseline. Prior to baseline, the average daily cost for medications in the benefit change versus reference groups was $0.23 versus $0.15, and the average out-of-pocket cost per dispensing was $13.65 versus $8.42, respectively (Table2). Thus, relative to patients in the reference group, those with the benefit change were already incurring more cost sharing prior to the change. The majority of subjects were dispensed 3-month supplies at each fill before and after the rollout of the benefit change. As expected with the introduction of a less generous cost-sharing arrangement, the proportion dispensed 3-month supply at each fill dropped slightly (from 85.5 percent before the benefit change to 83.1 percent after the benefit change) among those exposed to the benefit change. For the reference group, the proportion went up slightly during the pre- versus postperiod (from 88.4 to 90.7 percent).
Table 1.
Characteristics (Unadjusted*) of the 10,590 KPNC Patients Who Had Not Used a Mail Order Pharmacy Prior to Baseline Date of Pharmacy Benefit Change (January 1, 2006)
| Pharmacy Benefit Change in 2006 | ||||
|---|---|---|---|---|
| Patient Characteristics | All (n = 10,590) | Yes (n = 2,442) | No (n = 8,148) | p-value for Unadjusted Difference† |
| Demographics | ||||
| Female | 5,332 (50.4) | 1,309 (53.6) | 4,023 (49.4) | .0002 |
| Mean age (in years) (SD) | 59.7 (10.1) | 64.8 (10.1) | 58.2 (9.6) | <.0001 |
| Race/ethnicity | ||||
| African American | 2,126 (20.1) | 345 (14.1) | 1,781 (21.9) | <.0001 |
| Asian | 1,101 (10.4) | 284 (11.6) | 817 (10.0) | |
| Caucasian | 1,955 (18.5) | 546 (22.4) | 1,409 (17.3) | |
| Filipino | 1,398 (13.2) | 232 (9.5) | 1,166 (14.3) | |
| Latino | 2,053 (19.4) | 618 (25.3) | 1,435 (17.6) | |
| Multiracial | 1,164 (11.0) | 251 (10.3) | 913 (11.2) | |
| Other/unknown | 793 (7.5) | 166 (6.8) | 627 (7.7) | |
| Education | ||||
| No degree | 1,839 (17.8) | 694 (29.5) | 1,145 (14.3) | <.0001 |
| High school/GED | 3,086 (30.0) | 730 (31.0) | 2,365 (29.5) | |
| Some college | 2,613 (25.3) | 503 (21.4) | 2,110 (26.4) | |
| College graduate | 2,808 (27.1) | 427 (18.1) | 2,381 (29.8) | |
| Annual income (in thousands) | ||||
| <$25K | 1,891 (21.4) | 906 (45.6) | 985 (14.4) | <.0001 |
| $25K–$49K | 2,709 (30.6) | 584 (29.4) | 2,125 (31.0) | |
| $50K–$79K | 2,176 (24.6) | 278 (14.0) | 1,898 (27.7) | |
| ≥$80K | 2,074 (23.4) | 219 (11.0) | 1,855 (27.0) | |
| Reported difficulties paying for medications | 661 (7.9) | 262 (14.0) | 399 (6.2) | <.0001 |
| Reported difficulties paying for food | 2,603 (26.7) | 732 (32.8) | 1,871 (24.8) | <.0001 |
| Reported difficulties paying for medical supplies | 403 (5.7) | 142 (9.2) | 261 (4.8) | <.0001 |
| Any financial hardship (for food, Rx, or med supplies) | 2,969 (38.4) | 875 (49.1) | 2,094 (35.2) | <.0001 |
| Limited English proficiency | 1,086 (12.3) | 394 (19.8) | 692 (10.1) | <.0001 |
| Inadequate health literacy | 3,297 (46.3) | 909 (57.7) | 2,388 (43.1) | <.0001 |
| Mean home to local pharmacy distance in miles (SD) | 6.5 (9.2) | 7.0 (10.7) | 6.4 (8.8) | .005 |
n (%) unless otherwise specified; column percentages shown.
p-value for chi-square test for categorical variables and t-test for continuous variables.
Table 2.
Out-of-Pocket Costs and Utilization before and after Pharmacy Benefit Change among 10,590 KPNC Patients Who Had Not Used Mail Order Pharmacy Prior to Baseline Date of Pharmacy Benefit Change (January 1, 2006)
| Pharmacy Benefit Change (before Weighting) | ||||
|---|---|---|---|---|
| Patient Characteristics | All (n = 10,590) | Yes (n = 2,442) | No (n = 8,148) | p-value for Unadjusted Difference§ |
| 12 months prior to baseline† | ||||
| Per day per medication cost,‡ for community pharmacy fills, mean (SD) | $0.17 ($0.38) | $0.23 (0.36) | $0.15 ($0.38) | <.0001 |
| Total incurred cost per refill, for community fills, mean (SD) | $9.62 ($8.53) | $13.65 ($13.04) | $8.42 ($6.11) | <.0001 |
| Days' supply dispensed, for community fills, mean (SD) | 89 (16) | 87 (18) | 89 (15) | <.0001 |
| 1-month supply dispensed | 784 (7.4) | 251 (10.3) | 533 (6.5) | <.0001 |
| 2-month supply dispensed | 347 (3.3) | 69 (2.8) | 278 (3.4) | .15 |
| 3-month supply dispensed | 9,293 (87.8) | 2,087 (85.5) | 7,206 (88.4) | <.0001 |
| Total dispensings, for community fills, mean (SD) | 14.3 (7.8) | 15.0 (7.8) | 14.1 (7.8) | <.0001 |
| Cost sharing 12 months after baseline† | ||||
| Per day per medication cost,‡ for community pharmacy fills, mean (SD) | $0.20 ($0.39) | $0.35 ($0.48) | $0.16 ($0.35) | <.0001 |
| Per day per medication cost,‡ for mail order pharmacy fills, mean (SD) | $0.18 ($0.22) | $0.28 ($0.26) | $0.09 ($0.12) | <.0001 |
| Total incurred cost per refill, for community fills, mean (SD) | $11.64 ($10.62) | $21.33 ($15.27) | $8.78 ($6.21) | <.0001 |
| Total incurred cost per refill, for mail order pharmacy fills, mean (SD) | $15.97 ($16.93) | $24.23 ($18.26) | $7.77 ($10.27) | <.0001 |
| Days supply dispensed, for | ||||
| Community pharmacy fills, mean (SD) | 88 (16) | 83 (20) | 90 (15) | <.0001 |
| Mail order pharmacy fills, mean (SD) | 91 (18) | 95 (13) | 87 (22) | <.0001 |
| 1-month supply dispensed | 801 (7.6) | 336 (13.8) | 465 (5.7) | <.0001 |
| 2-month supply dispensed | 246 (2.3) | 48 (2.0) | 198 (2.4) | .18 |
| 3-month supply dispensed | 9,417 (88.9) | 2,030 (83.1) | 7,387 (90.7) | <.0001 |
| Total dispensings, for | ||||
| Community pharmacy fills, mean (SD) | 14.7 (8.1) | 14.0 (8.8) | 14.9 (7.9) | <.0001 |
| Mail order pharmacy fills, mean (SD) | 5.6 (5.5) | 8.0 (6.3) | 3.2 (3.3) | <.0001 |
| Insurance type | ||||
| Part D group coverage (%) | 1,454 (13.7) | 22 (0.9) | 1,432 (17.6) | <.0001 |
| Part D individual coverage (%) | 1,814 (17.1) | 1,817 (74.3) | 0 | |
| Non-Medicare coverage (%) | 7,322 (69.1) | 606 (24.8) | 6,716 (82.4) | |
n (%) unless otherwise specified; column percentages shown.
2005 versus 2006 used for pre-post comparison of those not receiving the benefit.
Per day medication cost equals the patient out-of-pocket cost divided by the days supply dispensed.
p-value for chi-square test for categorical variables and t-test for continuous variables.
MOP Uptake and Benefit Change Effect
Among those who did not previously use MOP, 30 percent of diabetes patients with the pharmacy benefit change initiated use of MOP in the year after the benefit change, as compared to 9 percent of patients not receiving the benefit change (Table3). The benefit change effect was quantified by the absolute difference in uptake between the benefit change and reference groups, which was a difference of 21 percentage points (95 percent CI: 19–23 percent) in the crude model and 26 percentage points (CI: 22–30 percent) in the adjusted model.
Table 3.
Uptake of Mail Order Pharmacy Use (MOP) Following Baseline Date of Pharmacy Benefit Change, Benefit Change Effect, and Effect Difference (Difference in Benefit Change Effect Across Social Groups) in a Cohort of 10,590 Diabetes Patients
| MOP Uptake | Benefit Change Effect* | Effect Difference§ (95% CI) | |||
|---|---|---|---|---|---|
| Pharmacy Benefit Changed | No Benefit Change | Unadjusted (95% CI) | Adjusted‡ (95% CI) | ||
| All subjects | 0.30 | 0.09 | 0.21 (0.19, 0.23) | 0.26 (0.22,0.30) | — |
| Income | |||||
| <$25K (ref) | 0.25 | 0.08 | 0.18 (0.14, 0.21) | 0.26 (0.19, 0.32) | — |
| $25K–$49K | 0.32 | 0.08 | 0.24 (0.20, 0.28)† | 0.21 (0.14, 0.29) | −0.05 (−0.15, 0.05) |
| $50K–$79K | 0.34 | 0.08 | 0.25 (0.20, 0.31)† | 0.34 (0.23, 0.46) | 0.08 (−0.05, 0.22) |
| $80K+ | 0.37 | 0.12 | 0.26 (0.19, 0.32)† | 0.27 (0.14, 0.40) | 0.02 (−0.13, 0.16) |
| Race | |||||
| Caucasian (ref) | 0.44 | 0.12 | 0.32 (0.28, 0.37) | 0.37 (0.31, 0.44) | — |
| African Am. | 0.21 | 0.08 | 0.13 (0.09, 0.18)† | 0.25 (0.14, 0.38) | −0.12 (−0.25, 0.04) |
| Asian | 0.39 | 0.11 | 0.28 (0.22, 0.34) | 0.21 (0.10, 0.34)† | −0.16 (−0.30, −0.001)† |
| Filipino | 0.25 | 0.08 | 0.17 (0.11, 0.23)† | 0.22 (0.10, 0.37) | −0.15 (−0.29, 0.02) |
| Latino | 0.21 | 0.06 | 0.15 (0.12, 0.19)† | 0.14 (0.07, 0.20)† | −0.24 (−0.33, −0.14)† |
| Education | |||||
| No degree (ref) | 0.25 | 0.07 | 0.18 (0.14, 0.22) | 0.22 (0.15, 0.30) | — |
| HS/GED | 0.29 | 0.09 | 0.20 (0.16, 0.24) | 0.26 (0.19, 0.33) | 0.04 (−0.07, 0.14) |
| Some college | 0.33 | 0.09 | 0.25 (0.20, 0.29)† | 0.23 (0.16, 0.32) | 0.01 (−0.10, 0.13) |
| College+ | 0.38 | 0.10 | 0.29 (0.24, 0.34)† | 0.31 (0.21, 0.41) | 0.09 (−0.05, 0.21) |
| Limited English proficiency | |||||
| No (ref) | 0.33 | 0.09 | 0.24 (0.21, 0.27) | 0.27 (0.23, 0.32) | — |
| Yes | 0.21 | 0.06 | 0.15 (0.10, 0.20)† | 0.13 (0.06, 0.21)† | −0.14 (−0.22, −0.05)† |
| Inadequate health literacy | |||||
| No (ref) | 0.40 | 0.09 | 0.31 (0.27, 0.35) | 0.35 (0.27, 0.42) | — |
| Yes | 0.26 | 0.08 | 0.18 (0.15, 0.21)† | 0.20 (0.14, 0.26)† | −0.15 (−0.24, −0.05)† |
| Financial hardship | |||||
| No (ref) | 0.36 | 0.09 | 0.27 (0.23, 0.30) | 0.31 (0.24, 0.37) | — |
| Yes | 0.26 | 0.09 | 0.19 (0.16, 0.22)† | 0.24 (0.17, 0.31) | −0.07 (−0.16, 0.02) |
Benefit change effect is estimated by the MOP uptake among those with a benefit change after subtracting the uptake in those without a benefit change (to “net out” the MOP uptake due to secular time trends among those not affected by the benefit change). All risk differences in table were significant at the <.05 level for H0: RD = 0.
Indicates statistical significance at the ≤.05 level for H0: RD(level) = RD(reference).
Poisson model with identity link function, models weighted for inverse probability of treatment weights (IPTW), expansion weights for race-stratified sampling design, and survey nonresponse (Horvitz–Thompson weighting). The IPTW model included baseline age, out-of-pocket drug copay, benefits based copay for brand drugs, Medicare indicator, deductible drug plan indicator, drug benefit business line (e.g., large employer group, small employer group, strategic group), and our socioeconomic indicators (ethnicity, income, education, limited English proficiency, inadequate health literacy, or financial hardship); weights were truncated at the 99th percentile. Confidence intervals calculated using 1,000 bootstrap samples in the adjusted models.
Effect difference is the absolute difference in the adjusted benefit change effect between a given social strata and the reference social strata.
Vulnerable social groups had a substantially smaller MOP uptake overall and were less responsive to the discount. Among those with the benefit change, the benefit change effect was higher among those with adequate health literacy (35 percent percentage point greater uptake [95 percent CI: 27–42 percent]) compared to those with inadequate health literacy (20 percent percentage point greater uptake [CI: 14–26 percent]), representing 15 percentage points (CI: 5 percent, 24 percent) effect difference. Similarly, the benefit change effect was 27 percent percentage point greater uptake (CI: 23–32 percent) among English-speaking patients, while among those with limited English proficiency only 13 percent (CI: 6–21 percent), representing a 14 percent (CI: 5 percent, 22 percent) point effect difference. There were also significant race-ethnic effect differences relative to Caucasians; Latinos and Asians had a 24 percent (CI: 14–33 percent) and 16 percent (CI: 0.1–30 percent) smaller benefit change effect. A smaller benefit change effect was also observed among those with lower annual income, self-reported financial hardship, and fewer years of education, albeit not statistically significant after adjustment. There were no substantive differences in our findings when rerunning the above analyses after excluding the 991 members who lost Part D Medicare pharmacy coverage during the observation window, and in separate models for Medicare and non-Medicare subjects.
Sensitivity Analysis
To disentangle the effect of the financial incentive for MOPs from a patient's choice of length of supply, we conducted a subanalysis in the 8,860 patients who would benefit from the incentive because they consistently filled 3-month supply in the periods before and after the benefit change. The adjusted MOP uptake was 28 percentage points greater in those who received the benefit change compared to those with no change in benefit (33 percent vs. 9 percent uptake) (p < .0001). Thus, restricting to people who could benefit from the incentive because they always filled a 3-month supply yielded essentially the same answer as the main analysis (which estimated a 26 percent increase in MOP uptake). We then repeated that sensitivity analysis in the 741 patients who would not benefit from the incentive because they consistently filled less than a 3-month supply during pre- and postperiods and detected no significant difference in uptake among those who did versus did not receive the benefit change.
Discussion
We examined MOP uptake after a pharmacy benefit change which included a prepayment discount for use of MOP, while offering a less generous (more cost sharing) pharmacy benefit package. We observed a substantial stimulating effect on MOPs uptake. In the year following the benefit change, the MOP uptake among previous MOP nonusers offered the prepayment discount to use MOPs was a 26 percent points greater compared to those not offered the discount. Given existing disparities in MOP use and the potential for MOPs to improve convenience, medication adherence, and risk factor control, it is important to understand the effects of benefit changes and incentives on vulnerable populations. In general, patients behaved as price-sensitive consumers and the discount greatly stimulated MOP uptake population-wide. However, the effect of the benefit change on MOPs was substantially smaller among minorities, those with inadequate health literacy or limited English proficiency.
Since the introduction of MOPs at KPNC in 1999, minorities have consistently lagged behind Caucasians in the uptake of MOPs and the reduced minority response to the MOP discount perpetuated the disparities. Similar patterns were observed in a recent study reporting that minorities or patients with inadequate health literacy or lower educational attainment were less likely to initiate use of a widely offered Internet-based patient portal even if they had access to a computer (Sarkar et al. 2010, 2011). The disparities in MOP use may have downstream impacts on disparities in medication adherence and clinical outcomes. We have previously reported better adherence (Duru et al. 2010) and better LDL-C control (Schmittdiel et al. 2011) among diabetic patients using MOPs. Better adherence among those using MOPs has been demonstrated in other studies (Devine, Vlahiotis, and Sundar 2010; Zhang et al. 2011; Visaria, Frazee, and Devine 2012), although one study (Khandelwal et al. 2011) had a null finding.
There are several possible explanations for these disparities in the effect of benefit changes. While one may expect greater price sensitivity in vulnerable patients, the prepayment of the additional copayment required to receive the incentive was possibly more of a barrier for the vulnerable groups. The prepayment discount may have failed as an incentive if it was inadequately communicated to or understood by patients. We observed significantly lower uptake in those with inadequate health literacy, limited English proficiency, and among the two ethnic groups (Latinos and Asians) with the greatest number of non-English-speaking patients compared to their respective reference groups (i.e., those with adequate health literacy and proficient in English, Caucasians). The reduced effect among patients with limited English proficiency is not unexpected. The health plan mailed a written notice of the benefit change (in English) to all the beneficiaries in advance of benefit design change but did not distribute a Spanish version of the notice until the year after the study. No other form of communication from the health plan was provided uniformly. We should expect that some patients would have additional information provided via discussion with the pharmacist when patients inquired about charges at the walk-in pharmacies. However, no subject-level data are available regarding those discussions.
The lower effect among those with inadequate health literacy may be attributable to difficulties navigating the complexities of the health system (i.e., understanding the steps needed to initiate a mail order refill); some patients may prefer the regular face-to-face interactions with pharmacists if they struggle with understanding written labels and medication instructions. Poor literacy is often accompanied by poor numeracy (i.e., the inability to understand and use numbers in daily life) which, though we did not assess this, may make it difficult for patients to weigh relative costs and benefits of the incentive (Cavanaugh et al. 2008; Rothman et al. 2008). Lower income individuals may lack a credit card and be unaware that MOPs can be requested via a mail-in form with a check or be concerned about using a telephone or Internet for credit card transactions. Some patients may be concerned about having medications sent to a mailbox that may be vulnerable to theft.
The benefit change offered a prepayment discount for MOPs such that patients had a larger initial, out-of-pocket cost to obtain the discount (“pay to play” design), representing a larger burden for vulnerable patients with limited financial resources, a barrier compounded for patients taking multiple medications. After the benefit change, those receiving the less generous benefit had a substantial increase in cost sharing (e.g., $21.33 per refill paid by those receiving the new benefit vs. $8.78 in the reference group). Thus, the prepayment burden was increased by the greater cost sharing. More price-sensitive patients may simply have had insufficient discretionary money or liquidity and were limited by the two copayments needed to benefit discount offer, or simply preferred “money in hand” over future savings provided by the incentive.
While the majority of subjects were dispensed 3-month supplies at each fill before and after the rollout of the benefit change, the change to a less generous cost-sharing arrangement also resulted in a slight decrease (2.4 percentage points) in the proportion dispensed a 3-month supply at each fill (from 85.5 percent before the benefit change to 83.1 percent after the benefit change) among those exposed to the benefit change. Our sensitivity analysis suggests there was an incentive effect in members who were dispensed a 3-month supply before and after the benefit rollout. Among the remaining minority of subjects who filled less than a 3-month supply during pre- and postperiods, we detected no significant incentive effect; there was no significant difference in MOP uptake among those who did versus did not receive the benefit change. This sensitivity analysis suggests that the offered incentive will likely not stimulate MOP uptake among patients whose usual level of dispensing is less than a 3-month supply. It is important to note that 80–90 percent of health plan members fill a 3-month supply at each dispensing and stand to benefit from the incentive.
Some limitations and strengths should be noted. This is a study of a nonrandomized exposure (benefit changes), and although we used a rigorous causal modeling approach (DID framework with marginal structural models) to handle biases associated with observational studies, residual confounding by measured or unmeasured variables is still a threat to validity. To isolate the effect of the benefit change on MOPs from expected secular changes in MOPs, we netted out the MOP uptake among those who had no change in benefits (i.e., the reference group). A limitation of this analytic approach is that there is no way to prove the validity of the DID assumption that the MOP uptake in the reference group serves as a reasonable model for the unobservable “background rates” of MOP uptake in the exposed group if they were actually not exposed. Thus, we exercise caution when interpreting the quantitative findings. Because we studied a cohort of nonusers, there were no prior trends in uptake to guide our predictions of future changes in utilization. However, given the magnitude of the quantitative differences in MOP uptake (i.e., >3-fold greater MOP uptake in 2006 among those exposed to the new benefit vs. those not exposed) and the substantially smaller benefit-related uptake in socially vulnerable populations, we believe that the qualitative interpretation of our findings regarding the uptake that is above and beyond background is reasonable; the benefit change with a prepayment discount for MOP-stimulated MOP uptake, but less so in vulnerable populations. The stark differences in MOP uptake in patients receiving the pharmacy benefit change (vs. not) will likely diminish over time with growing acceptance for this new mode of medication delivery and as the number of remaining nonusers decreases. Because this is observational research, interpreting the social differences in the impact of the benefit change is complicated given the exposed and reference groups differed on baseline social characteristics, although the final models adjusted for observed confounders. The ideal reference group would have been patients who were switched to a pharmacy benefit offering a 1-month supply (rather than remaining on the 3-month supply plan) without MOP incentives. No such benefit structure existed. Concerns of endogeneity arise if subjects can choose which level of benefits they were exposed to. However, during the time of this study, while the generosity of benefit coverage varied across employer group or Medicare, patients receiving benefits through any one of these contractors did not have a choice of level of benefit plan. All but 3 percent (n = 351) of our study subjects acquired health plan coverage via employment or Medicare and thus had no choice about the level of coverage. The adjusted model accounts for differences in the generosity of benefits by weighting for pharmacy benefit deductibles and pharmacy benefit business line.
To simply report the MOP uptake in those experiencing the benefit change would overestimate the effect of the benefit change given the secular trends. We reduced that MOP uptake resulting from the benefit change by the background expected uptake observed in the reference group, after adjusting for case mix differences. That said, the variation in uptake among different social groups receiving the benefit change (i.e., exposed) conveys the same take home message; vulnerable subjects receiving the incentive were less likely to initiate MOPs. For example, among those who did not use MOPs prior to the benefit change, 44 percent of Caucasians versus 21 percent of Latino and African Americans initiated MOPs after receiving the benefit change. Although some of this MOP uptake would be expected due to secular trends and thus not due to the benefit change, the differential between social groups is consistent with a benefit change effect that differs is size across social strata.
The pharmacy benefit change combined the offer of a financial incentive, in the form of a prepayment discount, with a less generous pharmacy benefit plan. Those exposed to the benefit change were switched from a more generous baseline benefit to a much less generous benefit, and that may have impacted the magnitude of the incentive effect on MOP uptake. The financial incentive is the most plausible explanation for the increased MOP uptake. There is no obvious reason why charging patients more per pill (due to the increased cost sharing imposed by the benefit change) would induce the large increase in use of MOPs that we observed overall or induce vulnerable patients to be less likely to take advantage of the MOP incentive that reduces the cost per pill. On the contrary, to the extent that vulnerable populations are more price sensitive, they might be expected to be more likely to take advantage of the discount. Admittedly, we have no data available to explain why subjects made their choices regarding whether to initiate MOPs. Substantive changes in adherence could change the motivation to use MOPs or sample composition. One of the strengths of this study is that it was a natural experiment; the benefit change was not subject to patient choice or self-selection but was dependent on group contract negotiations. Reverse causality is precluded also by the design's temporal ordering (i.e., pretest-posttest with controls), and regression to the mean is not a concern given both exposed and reference group have the identical starting point (none are MOP users at baseline).
This study suggests some policy-related lessons. Benefit change announcements using plain language in English and other languages should be sent out prior to initiating the change. When both modes of medication delivery are supported by a health delivery system, pharmacists and pharmacy staff could verbally encourage the use of MOPs and explain any potential cost savings associated with the MOPs to patients currently using community pharmacies. Rather than requiring prepayment of an extra copayment to receive the discount, a more uniform effect may be achievable by restructuring the discount so that patients using MOPs receive a set number of free days' supply for each copayment. “Pay to play” designs such as this may in the end act as a disincentive that overrides the benefit of any potential discounts for the patient in a way that differentially impacts vulnerable populations. While largely dictated by external forces (e.g., competitive health plan markets, group purchaser and federal insurer demands, rising cost of pharmaceuticals, and provision of health care), benefit changes present a difficult policy dilemma for health care delivery systems given the often competing economic and quality implications. In this case, the health plan benefit change simultaneously supported one quality improvement goal (e.g., increase use of MOP) and potentially reduced the cost of pharmacy operations, while competing with another (e.g., elimination of health disparities). These findings further demonstrate the hazard of assuming uniform effects of innovations, interventions, or structural changes across patient groups. While we expect that inequalities in use of MOP will shrink as advantaged groups approach a ceiling and the disadvantaged groups catch up, the pattern needs to be viewed in the larger context. Even if the inequalities resulting from any given structural change eventually dissipate, the constant stream of new structural changes can perpetuate or exacerbate existing inequalities if even small and temporary differences in health system access are progressively introduced (see Phelan and Link's theory of “fundamental causes” [Phelan and Link 2005; Phelan et al. 2004]). To avoid increasing existing social differences in utilization, early testing for heterogeneity in treatment effectiveness provides an important opportunity to proactively design and tailor innovations, whether they be new benefit models, translation of interventions, or quality improvement efforts (Frohlich and Potvin 2008; Varadhan et al. 2012).
Acknowledgments
Joint Acknowledgment/Disclosure Statement: National Institute of Diabetes, Digestive and Kidney Diseases (R01DK081796, RC1 DK086178, R01DK080726, R01DK65664, P30 DK092924), National Institute on Aging (R01AG032249), the Patient-Centered Outcomes Research Institute (CE-1304-7250), and the Division of Diabetes Translation, Centers for Disease Control and Prevention (U58 DP002641, U58 DP002721).
Disclosures: None.
Disclaimers: None.
Supporting Information
Appendix SA1: Author Matrix.
Figure S1. Directed Acyclic Graph (DAG) Used to Guide Our Development of the Model of the Impact of Mail Order Incentives (MOIs) on Mail Order Pharmacy (MOP) Use.
References
- Campbell DT. Stanley JC. Experimental and Quasi-Experimental Designs for Research. Boston: Houghton Mifflin; 1963. [Google Scholar]
- Carroll NV. Mail-Service Pharmacy Savings: A Conclusion in Search of Evidence. Journal of Managed Care Pharmacy. 2006;12(2):164–7. doi: 10.18553/jmcp.2006.12.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll NV, Brusilovsky I, York B. Oscar R. Comparison of Costs of Community and Mail Service Pharmacy. Journal of American Pharmacists Association. 2005;45(3):336–43. doi: 10.1331/1544345054003796. [DOI] [PubMed] [Google Scholar]
- Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, Gregory RP, Fuchs L, Malone R, Cherrington A, Pignone M, DeWalt DA, Elasy TA. Rothman RL. Association of Numeracy and Diabetes Control. Annals of Internal Medicine. 2008;148(10):737–46. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- Cheung YB. A Modified Least-Squares Regression Approach to the Estimation of Risk Difference. American Journal of Epidemiology. 2007;166(11):1337–44. doi: 10.1093/aje/kwm223. [DOI] [PubMed] [Google Scholar]
- Chew LD, Bradley KA. Boyko EJ. Brief Questions to Identify Patients with Inadequate Health Literacy. Family Medicine. 2004;36(8):588–94. [PubMed] [Google Scholar]
- Chien-Wen T, Phillips RL, Green LA, Fryer GE. Dovey SM. What Physicians Need to Know about Seniors and Limited Prescription Benefits, and Why. American Family Physician. 2002;66(2):212. [PubMed] [Google Scholar]
- Choudhry NK, Fischer MA, Avorn J, Liberman JN, Schneeweiss S, Pakes J, Brennan TA. Shrank WH. The Implications of Therapeutic Complexity on Adherence to Cardiovascular Medications. Archives of Internal Medicine. 2011;171(9):814–22. doi: 10.1001/archinternmed.2010.495. [DOI] [PubMed] [Google Scholar]
- Devine S, Vlahiotis A. Sundar H. A Comparison of Diabetes Medication Adherence and Healthcare Costs in Patients Using Mail Order Pharmacy and Retail Pharmacy. Journal of Medical Economics. 2010;13(2):203–11. doi: 10.3111/13696991003741801. [DOI] [PubMed] [Google Scholar]
- Duru OK, Schmittdiel JA, Dyer WT, Parker MM, Uratsu CS, Chan J. Karter AJ. Mail-Order Pharmacy Use and Adherence to Diabetes-Related Medications. American Journal of Managed Care. 2010;16(1):33–40. [PMC free article] [PubMed] [Google Scholar]
- Frohlich KL. Potvin L. Transcending the Known in Public Health Practice: The Inequality Paradox: The Population Approach and Vulnerable Populations. American Journal of Public Health. 2008;98(2):216–21. doi: 10.2105/AJPH.2007.114777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon NP. Kaplan GA. Some Evidence Refuting the HMO “Favorable Selection” Hypothesis: The Case of Kaiser Permanente. Advances in Health Economics and Health Services Research. 1991;12:19–39. [PubMed] [Google Scholar]
- Horvitz DG. Source DJT. A Generalization of Sampling without Replacement from a Finite Universe. American Statistical Association Stable. 1952;47:663–85. [Google Scholar]
- Khandelwal N, Duncan I, Rubinstein E, Ahmed T, Pegus C, Murphy P. Kudrak KE. Medication Adherence for 90-Day Quantities of Medication Dispensed through Retail and Mail Order Pharmacies. American Journal of Managed Care. 2011;17(11):e427–34. [PubMed] [Google Scholar]
- Meyer BD. Natural and Quasi-Experiments in Economics. Journal of Business and Economic Statistics. 1995;13(2):151–61. [Google Scholar]
- Moffet HH, Adler N, Schillinger D, Ahmed AT, Laraia B, Selby JV, Neugebauer R, Liu JY, Parker MM, Warton M. Karter AJ. Cohort Profile: The Diabetes Study of Northern California (DISTANCE)–Objectives and Design of a Survey Follow-Up Study of Social Health Disparities in a Managed Care Population. International Journal of Epidemiology. 2008;38(1):38–47. doi: 10.1093/ije/dyn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortimer KM, Neugebauer R, van der LM. Tager IB. An Application of Model-Fitting Procedures for Marginal Structural Models. American Journal of Epidemiology. 2005;162(4):382–8. doi: 10.1093/aje/kwi208. [DOI] [PubMed] [Google Scholar]
- Phelan JC. Link BG. Controlling Disease and Creating Disparities: A Fundamental Cause Perspective. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2005;60(60 Spec No 2):27–33. doi: 10.1093/geronb/60.special_issue_2.s27. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Ez-Roux A, Kawachi I. Levin B. ‘Fundamental Causes’ of Social Inequalities in Mortality: A Test of the Theory. Journal of Health and Social Behavior. 2004;45(3):265–85. doi: 10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- Robins JM. Association, Causation, and Marginal Structural Models. Synthese. 1999;121:151–79. [Google Scholar]
- Ross CE. Wu CL. The Links between Education and Health. American Sociological Review. 1995;60:719–45. [Google Scholar]
- Rothman RL, Montori VM, Cherrington A. Pignone MP. Perspective: The Role of Numeracy in Health Care. Journal of Health Communication. 2008;13(6):583–95. doi: 10.1080/10810730802281791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabate E. Adherence to Long-Term Therapies: Evidence for Action. Switzerland: World Health Organization; 2003. pp. 1–196. [Google Scholar]
- Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, Lopez A. Schillinger D. The Literacy Divide: Health Literacy and the Use of an Internet-Based Patient Portal in an Integrated Health System-Results from the Diabetes Study of Northern California (DISTANCE) Journal of Health Communication. 2010;15(Suppl 2):183–96. doi: 10.1080/10810730.2010.499988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, Lopez A. Schillinger D. Social Disparities in Internet Patient Portal Use in Diabetes: Evidence that the Digital Divide Extends Beyond Access. Journal of the American Medical Informatics Association. 2011;18(3):318–21. doi: 10.1136/jamia.2010.006015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittdiel JA, Karter AJ, Dyer W, Parker M, Uratsu C, Chan J. Duru OK. The Comparative Effectiveness of Mail Order Pharmacy Use vs. Local Pharmacy Use on LDL-C Control in New Statin Users. Journal of General Internal Medicine. 2011;26(12):1396–402. doi: 10.1007/s11606-011-1805-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittdiel JA, Karter AJ, Dyer WT, Chan J. Duru OK. Safety and Effectiveness of Mail Order Pharmacy Use in Diabetes. The American Journal of Managed Care. 2013;19(11):882–7. [PMC free article] [PubMed] [Google Scholar]
- Trinacty CM, Adams AS, Soumerai SB, Zhang F, Meigs JB, Piette JD. Ross-Degnan D. Racial Differences in Long-Term Adherence to Oral Antidiabetic Drug Therapy: A Longitudinal Cohort Study. BMC Health Services Research. 2009;9(1):24. doi: 10.1186/1472-6963-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valluri S, Seoane-Vazquez E, Rodriguez-Monguio R. Szeinbach SL. Drug Utilization and Cost in a Medicaid Population: A Simulation Study of Community vs. Mail Order Pharmacy. BMC Health Services Research. 2007;7:122. doi: 10.1186/1472-6963-7-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varadhan R, Stuart EA, Louis TA, Segal JB. Weiss CO. Standards in Addressing Heterogeneity of Treatment Effectiveness in Observational and Experimental Patient Centered Outcomes Research. Washington, DC: 2012. [Google Scholar]
- Visaria J, Frazee SG. Devine ST. Asthma Controller Adherence in Mail Order Pharmacy Compared to Retail Pharmacy. American Journal of Pharmacy Benefits. 2012;4(3):e73–80. [Google Scholar]
- Wroblewski, Michael S, Schmidt DavidR, Schultheiss Patricia, Goldman KarenA, Marks Randall, DeSanti Susan, Mathias SarahM, Argeris ElizabethJ, Shonka Natalie. Wigton Mahlon. Pharmacy Benefit Managers: Ownership of Mail-Order Pharmacies. Washington, DC: Federal Trade Commission; 2005. Rep. Web. 24 July 2014. [Google Scholar]
- Zhang L, Zakharyan A, Stockl KM, Harada AS, Curtis BS. Solow BK. Mail-Order Pharmacy Use and Medication Adherence among Medicare Part D Beneficiaries with Diabetes. Journal of Medical Economics. 2011;14(5):562–7. doi: 10.3111/13696998.2011.598200. [DOI] [PubMed] [Google Scholar]
- Zou G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. American Journal of Epidemiology. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Figure S1. Directed Acyclic Graph (DAG) Used to Guide Our Development of the Model of the Impact of Mail Order Incentives (MOIs) on Mail Order Pharmacy (MOP) Use.


