Abstract
Background
Although the prevalence of obesity in young children highlights the importance of early interventions to promote physical activity (PA), there are limited data on activity patterns in this age group. The purpose of this study is to describe activity patterns in preschool-aged children and explore differences by weight status.
Methods
Analyses use baseline data from Healthy Homes/Healthy Kids- Preschool, a pilot obesity prevention trial of preschool-aged children overweight or at risk for overweight. A modified parent-reported version of the previous-day PA recall was used to summarize types of activity. Accelerometry was used to summarize daily and hourly activity patterns.
Results
“Playing with toys” accounted for the largest proportion of a child’s previous day, followed by “meals and snacks”, and “chores”. Accelerometry-measured daily time spent in sedentary behavior, light PA, and moderate-to-vigorous PA (MVPA) was 412, 247, and 69 minutes, respectively. Percent of hourly time spent in MVPA ranged from 3% to 13%, peaking in the late morning and evening hours. There were no statistically significant MVPA differences by weight status.
Conclusions
This study extends our understanding of activity types, amounts, and patterns in preschool-age children and warrants further exploration of differences in physical activity patterns by weight status.
Keywords: PDPAR, accelerometer, sedentary behavior, overweight
BACKGROUND
Obesity and physical inactivity persist as major public health concerns. Twenty-seven percent of US children ages 2–5 are overweight or obese,1 highlighting the importance of early interventions to reduce obesity risk. The etiology of obesity is complex, but is broadly summarized as caloric intake and expenditure imbalance. Physical activity (PA) and sedentary behavior play a critical role in this energy balance equation. Lack of moderate-to-vigorous physical activity (MVPA) has been associated with increased risk of overweight and obesity.2,3 Decreases in total PA, or inversely, increases in sedentary behavior, also contribute to obesity prevalence.4 However, detailed information about physical activity and sedentary behaviors is only now emerging in this young population.
Activity measurement is important for informing intervention development, but presents unique challenges in this population. Because young children cannot report their activity patterns, parent-report or objective measures (e.g. accelerometry) are used, though both approaches have limitations. Because young children often spend time away from their parents in daycare and other settings, they are not always able to accurately describe their child’s activity patterns. Accelerometry presents challenges, including compliance difficulty, lack of standardized data collection protocols (e.g. monitor placement, nap-time wearing guidelines), and lack of consensus on standardized analysis (e.g. length of valid day, number of valid days needed to represent normal activity, appropriate intensity cut-points)5. Accelerometry also does not yet allow for detailed activity type information.
Along with, and likely influenced by measurement challenges, little is known about the activity patterns required to prevent unhealthy weight gain in this population. Some recent US and international physical activity and sedentary behavior guidelines have been developed for young children under the age of 5.6–9 Recommendations for young children were not included in the 2008 US’s National Physical Activity Guideline due to limited available data on which to base such guidelines. However, a recent midpoint report does highlight the importance of promoting physical activity and reducing sedentary behavior for children ages 3 to 5.10 Current preschool-age guidelines are inconsistent in the amount of activity needed to promote health, ranging from 120 to 180 minutes of physical activity per day. Guidance on how to best accumulate activity is vague. Most of these guidelines also provide recommendations for sedentary behavior, such as limiting screen time to less than 19 or 26,11 hours and limiting bouts of sedentary behavior during waking hours6–9,11 Though relatively consistent screen time recommendations exist, there are limited data on typical sedentary behavior patterns and associations with health outcomes in young children.12
The development of consistent and detailed guidelines for parents and child care providers requires further exploration of physical activity and sedentary behavior patterns. A handful of studies have looked at young children’s activity patterns beyond total daily minutes of activity. Such patterns include: seasonal variations13, daily variation (weekday vs. weekend day)13, within day variation (morning vs. evening)14,15, hourly variation16, activity location (indoor vs. outdoor)17, how activity is accumulated throughout a day (clustered vs. isolated spurts)18, and type of activity during preschool.19 Detailed information about daily patterns of activity types, prevalence of different activity types, and hourly variability in physical activity and sedentary behaviors among young children is only beginning to emerge.
Given the need for early prevention of obesity and the limited activity pattern data available for young children, the aims of this study are to 1) use a modified parent-reported version of the previous-day physical activity recall (PDPAR) to qualitatively describe activity types of preschool children, 2) conduct exploratory analyses to assess whether PDPAR-measured activity type is associated with child weight status and 3) use accelerometry to characterize daily patterns of activity amount and intensity and explore potential differences by weight status.
METHODS
Sample
Analyses use baseline data from Healthy Homes/Healthy Kids-Preschool (HHHK-Preschool), a randomized controlled obesity prevention pilot study. Children ages 2 to 4 and their parents were identified and recruited through a clinic system in the Minnesota. Eligibility criteria included 1) scheduled for an upcoming well-child visit at a participating clinic, 2) no medical conditions precluding participation, 3) English speaking, and 4) being “at-risk” for obesity, defined as either currently overweight (body mass index (BMI) between the 85th and 95th percentile as defined by the CDC growth charts), or children between the 50th and 85th BMI percentile with at least one overweight parent (BMI greater than 25 kg/m2). A total of 941 potentially eligible participants were identified through electronic medical record data. Of those, 506 were excluded before being invited to participate (primarily due to insufficient time to recruit prior to scheduled well-child visit). Of those invited, 340 were unable to be reached or uninterested in participating. An additional 35 were ineligible after further screening. In total, 60 participants enrolled in the study. Informed consent was obtained from parents; all study protocols were approved by the HealthPartners Institutional Review Board.
Previous Day Physical Activity Recall
The 24-hr Previous Day Physical Activity Recall (PDPAR)20, originally designed for older children to self-report previous day PA in a classroom setting under scripted teacher supervision, was modified to be a staff-administered, parent-completed measure to assess younger children’s previous-day PA. At the baseline visit, parents were guided by staff to recall the child’s previous-day activities in 30-min blocks between 5:00 AM and 11:59 PM. They were shown a list of age- and region-appropriate activities (e.g. coloring, tag, sledding) categorized by activity type (e.g. eating, transportation, spare time) and asked to report the primary activity their child was doing for each 30-minute block. If the parent reported two or more activities for one block, staff instructed parents to choose which activity they did most during the 30 minutes.
PDPAR activities were categorized by similarity of purpose: 1) meals and snacks, 2) nap and rest, 3) chores (e.g. cooking, laundry, shoveling), 4) motorized transportation (e.g. riding in the car), 5) non-motorized transportation (e.g. walking or biking for transportation), 6) TV, 7) computer and video games, 8) toys (e.g. coloring, puzzles, reading), 9) free play (e.g. tag, jungle gym, swimming for fun), 10) hanging around, 11) sports (e.g. soccer, tumbling, baseball), or 12) other activities (e.g. attending events, listening to music). Three additional activity types for free response were listed (“other household chores”, “other spare time/hobbies”, and “other physical activities/sports”); free-response options were re-coded into the 12 categories above. PDPAR-reported activity types are presented as the percent of parents who reported their child doing each activity type the previous day and as a proportion of the children’s previous day spent in each activity type. Activity proportions were calculated for each child by dividing the number of blocks spent in an activity type by the number of total blocks between the first non-sleep block after 5:00 AM and the last non-sleep block before 11:59 PM. Activity proportions were then averaged across all participants.
Accelerometry
Children were fitted with an ActiGraph GT3X accelerometer (ActiGraph Corporation, Pensacola, FL) at the baseline home visit and asked to wear it during waking hours for seven full days. The devices were placed on elastic belts and fitted on the right hip and initialized to record data in 5-second epochs.21 Accelerometry data were included in this analysis if there were at least four valid monitoring days, defined as 6 or more hours of wear time. The shorter 6-hour wear-time criterion was used because participants were not asked to wear the monitor during daytime naps, reducing the total amount of possible wear time. Non-wear time was defined as a string of 60 or more consecutive zero-counts, allowing for an interruption interval of 2 consecutive minutes of 100 counts or less22,23.
To estimate average time spent in sedentary, light, and moderate-to-vigorous physical activity (MVPA), data were aggregated into 15-second epochs; intensity cut-points were developed using the Pate et al. (2006) and Evenson et al (2008) equations. The cut point between sedentary and light was 25 counts/15 seconds24 and the cut point between light and MVPA was 420 counts/15 seconds.25 A calibration study comparing all available cut-points identified these cut-points as the most accurate for classifying sedentary time and MVPA.26 Data were aggregated into both average daily and hourly minutes of activity. Average hourly activity was measured by three variables (the average percent of the hour spent in sedentary, light PA, and MVPA), which were calculated for each 1-hour time period (e.g., 3 PM to 4 PM). Participants were included in each hour analysis if they had valid wear time for the entire hour on 3 or more separate days. For each 1-hour time period, the average percent of the hour spent in sedentary, light PA, and MVPA was calculated for each participant and then averaged across all participants. Due to the small sample size and wear time protocol restrictions (participants not asked to wear monitors while napping) hourly activity variability throughout the day was examined qualitatively; hourly analyses are depicted graphically by weight status.
Child Weight Status
Study staff measured child weight and height using a Seca 876 flat scale and Seca 217 stadiometer (Seca Corp., Hanover, MD). Weight and height were measured twice. If the first two measurements differed by more than 0.2 kg for weight or more than 1.0 cm for height, the process was repeated a third time. Data for the multiple assessments were averaged. BMI percentile was calculated using the CDC 2000 Growth Charts. Overweight was defined as children between the 85th and 95th BMI percentile and “at-risk” for becoming overweight was defined as children between the 50th and 85th percentile with at least one overweight parent (BMI ≥ 25kg/m2).
Demographic Characteristics
Demographic characteristics were collected via parent survey (age, gender, race, and ethnicity). Child care attendance was derived from proportion of meals eaten at preschool as reported by parents during previous-day dietary recalls (NDSR, Nutrition Coordinating Center, NCC, University of Minnesota, Minneapolis, MN)27 in which parents were asked to recall foods and beverages their child consumed on the previous day, specifying meal time and location.
Statistical Analyses
All analyses were completed using SAS version 9.2. For baseline descriptive characteristics, means and standard deviations are reported for all continuous variables and frequencies are reported for categorical variables. Independent sample t-tests were used to compare continuous variables by weight-status. Sample size limitations precluded exploration of covariates such as age or sex in these analyses. Chi-square tests compared categorical variables by weight-status. Fisher’s Exact tests were used if any cell size was less than five.
RESULTS
Demographic Characteristics
Baseline characteristics for participants with valid PDPAR data (n=59) are shown in Table 1. Children’s mean age (SD) was 2.8 (0.8) years and the mean BMI percentile (SD) was 81 (11). About half (45%) of children were female, and most were non-Hispanic (95%) and white (80%). Sixty percent of parents reported that their child had eaten no meals at preschool on the previous day. Of the 40% who reported that their child had one or more meals at daycare, only 14 reported that more than half of their meals were consumed in preschool. There were no significant differences by weight status in any of the baseline demographics other than the expected BMI percentile difference (p<.01).
Table 1.
Demographic characteristics overall and by weight status.
| Overall (N=59) |
At-Risk (n=34) |
Overweight (n=25) |
p-value | |
|---|---|---|---|---|
| Child Age, M (SD) | 2.8 (0.8) | 2.7 (0.8) | 2.9 (0.8) | 0.34 |
| Child Gender, % Female | 46 | 44 | 48 | 0.77 |
| Child Race, % White | 80 | 82 | 76 | 0.55 |
| Child Ethnicity, % Non-Hispanic | 95 | 94 | 96 | 0.73 |
| Child BMI Percentile, M (SD) | 80.7 (10.7) | 73.8 (9.0) | 90.0 (3.1) | <.01 |
| Child Care | ||||
| % no meals at preschool | 60 | 54 | 68 | |
| % < half of meals at preschool | 17 | 23 | 8 | |
| % ≥ half of meals at preschool | 23 | 23 | 24 | 0.30 |
| Parent Age, M (SD) | 33.9 (4.7) | 34.3 (4.6) | 33.3 (4.8) | 0.40 |
| Parent Gender, % Female | 93 | 90 | 96 | 0.45 |
PDPAR-Measured Activity Types and Patterns
Of the 60 participants, all but one had complete PDPAR data and 81% of the recalls were weekdays. The percent of parents who reported that their child participated in each activity type on the previous day are shown in Table 2. The most commonly reported activity types were “meals and snacks” and “playing with toys”; 100% of parents reporting that their child did these activities for at least one 30-minute block of time. The next most frequently reported activities were “chores,” “free play,” and “motorized transportation,” with 97% (n=56), 88% (n=51), and 79% (n=46) of parents reporting these activities, respectively. Two thirds of parents reported their child watched TV the previous day (n=38). Relatively few parents reported that their child spent time playing sports (n=14), computer or video games (n=6), or walking or biking for transportation (n=3) on the previous day.
Table 2.
Percent of children doing different activity types overall and by weight status.
| Overall (N=59) |
At-Risk (n=34) |
Overweight (n=25) |
p-value | |
|---|---|---|---|---|
| Meals/Snacks | 100 | 100 | 100 | - |
| Nap/Rest | 33 | 30 | 36 | 0.65 |
| Chores | 97 | 97 | 96 | 1.00 |
| Motorized Transportation | 79 | 82 | 76 | 0.59 |
| Non-motorized Transportation | 5 | 3 | 8 | 0.57 |
| TV | 66 | 67 | 64 | 0.83 |
| Computer/Video Games | 10 | 3 | 20 | 0.08 |
| Toys | 100 | 100 | 100 | - |
| Free Play | 88 | 91 | 84 | 0.45 |
| Hanging Around | 21 | 9 | 36 | 0.02 |
| Sports | 24 | 21 | 28 | 0.55 |
| Other Activities | 17 | 18 | 16 | 0.83 |
Table 2 shows comparisons of percent of children doing different activity types by weight status (overweight vs. at-risk for becoming overweight). Thirty-six percent of overweight participants spent some of their previous day “hanging around”, compared to 9% of at-risk participant (p=0.02). Twenty percent of overweight participants spent some time in “computers and video games” compared to 3% of at-risk participants (p=0.08).
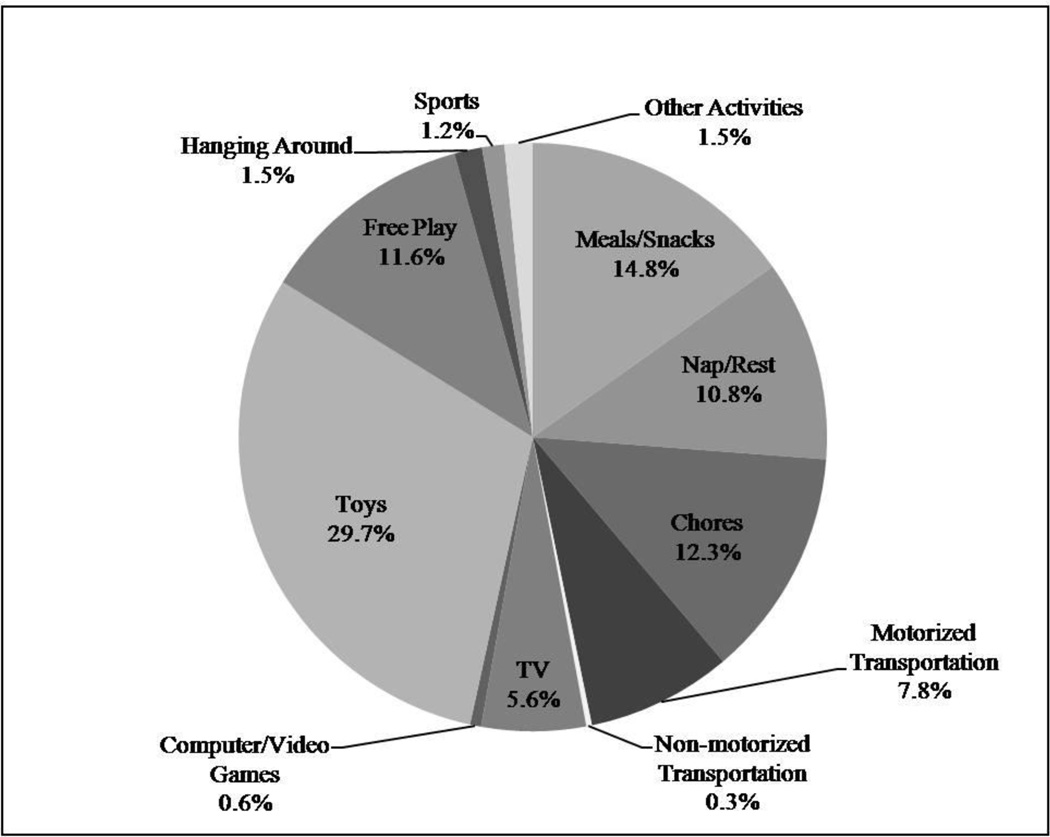
To examine activity patterns, we calculated the average proportion of the previous day spent in each type of activity across all participants (Figure 1). On average, “playing with toys” represented the largest proportion of a child’s previous day, followed by “meals and snacks” and “chores.” These activity types accounted for about 60% of an average child’s day. Parent-reported “free play” and “napping or resting” accounted for another approximately 20% of the average day. “Television” and “computer or video game” use accounted for about 6% of an average day. Motorized transportation accounted for about 8% of the previous day, compared to less than 1% of non-motorized transportation. “Hanging around”, “playing sports”, and “other activities” made up the remainder of an average day.
Figure 1.
Average proportion of previous day spent in different activity types, N=59.
The proportion of the day spent in different activity types did not differ markedly between at-risk and overweight children. As above, the only statistically significant differences were in average time spent “hanging around” (0.3% of the day in at-risk children and 2.9% of the day in overweight children, p<0.01) and “playing computer/video games” (on average 0.1% of the day in at-risk children and 1.1% of the day in overweight children).
Accelerometer-Measured Activity Amount and Intensity
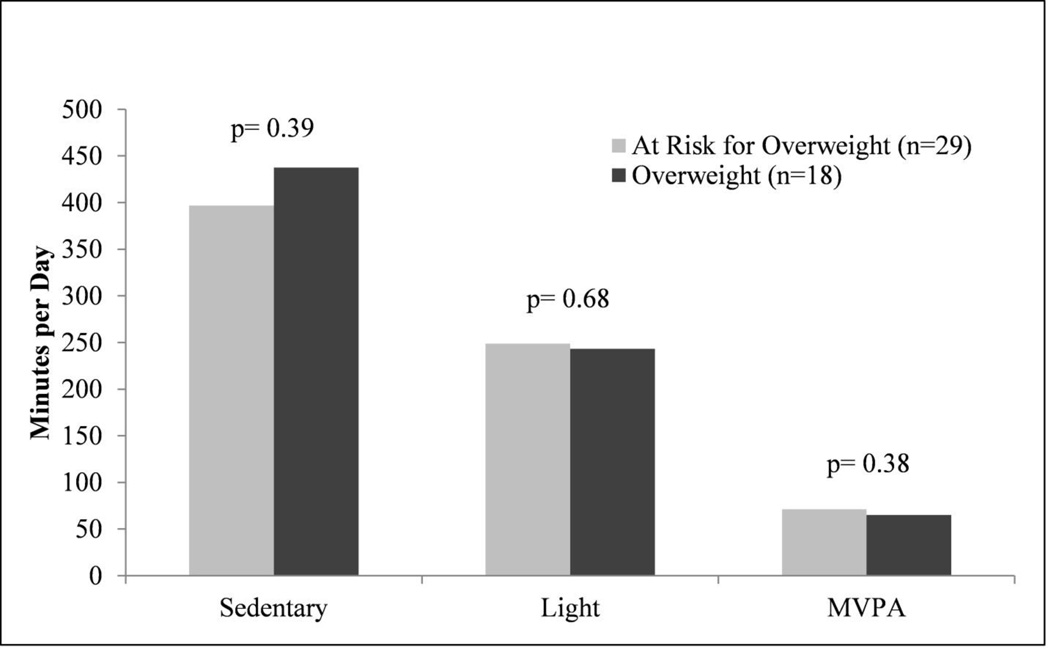
Of the enrolled children, 78% had valid accelerometry data at baseline (N=47). Seven participants had incomplete data due to device failure and six were lost due to participant non-compliance (e.g. failed to meet wear time criteria, device water damage). There were no statistically significant differences in gender (p= 0.92), age (p=0.77), or BMI percentile (p=0.97) by accelerometry compliance. Mean minutes of daily wear time (SD) for those successfully meeting criteria was 728 (185) with an average (SD) of 5.9 (1.0) valid days. Average minutes of daily time (SD) spent in sedentary behavior, light PA, and MVPA measured was 412 (155), 247 (43), and 69 (23) minutes, respectively. There were no statistically significant differences in daily activity levels between children who were overweight and those at risk for becoming overweight (Figure 2).
Figure 2.
Average daily minutes of activity intensity by weight status.
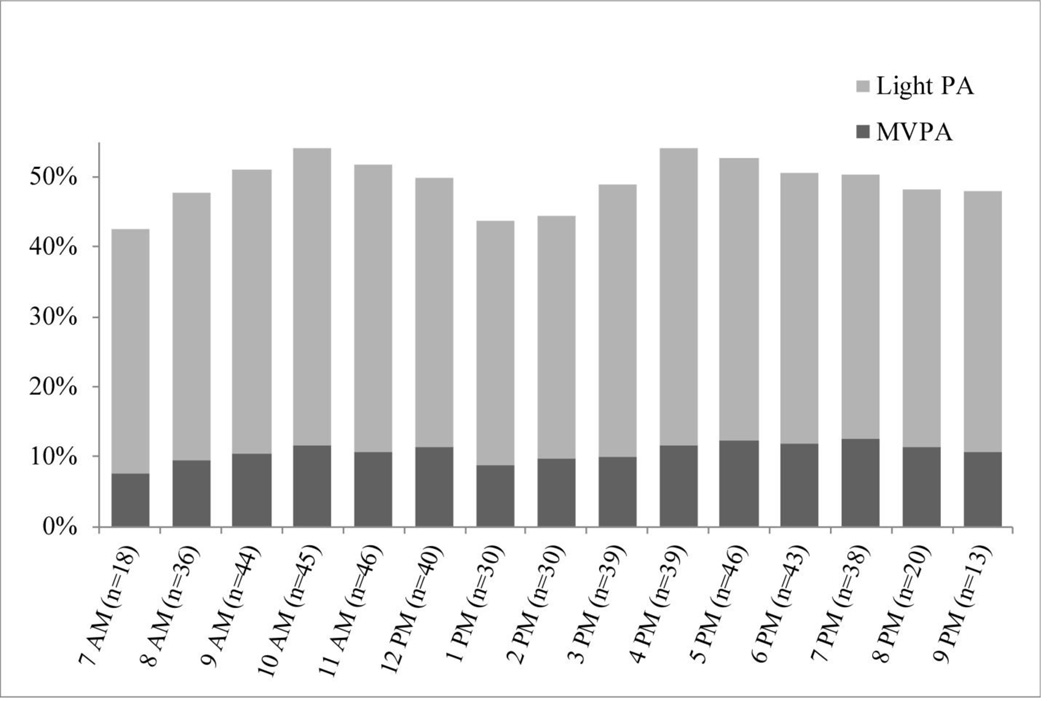
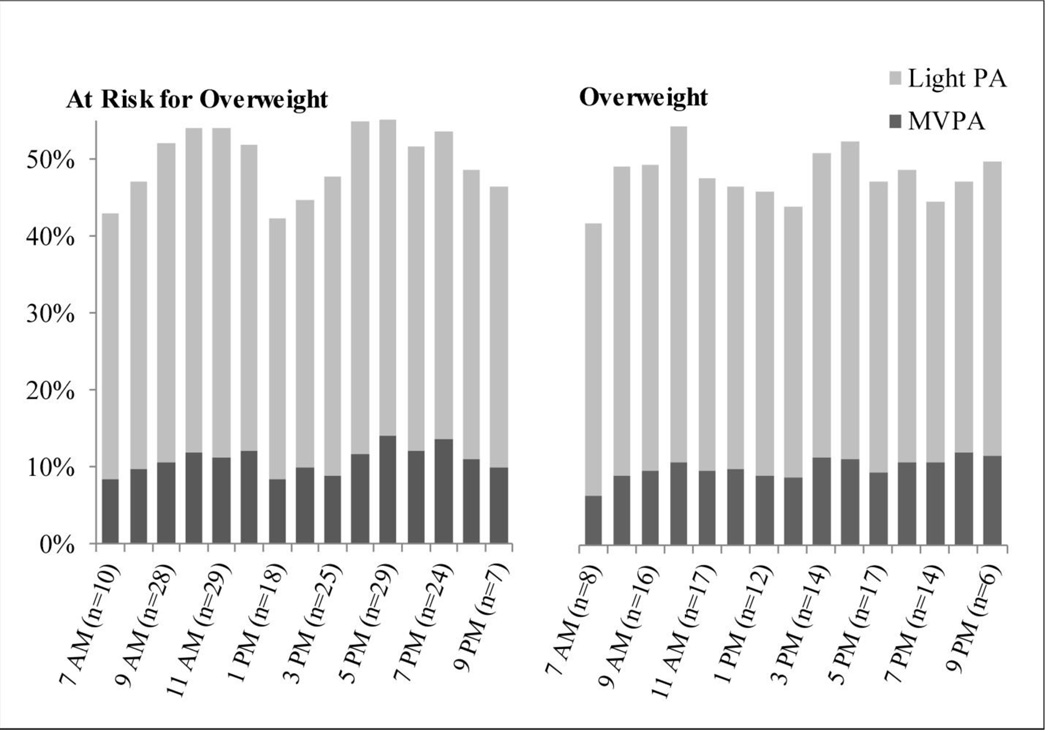
Hourly PA data are presented in Figures 3 and 4. Percent of each hour spent in MVPA ranged from 3% (about 2 minutes per hour) to 13% (about 8 minutes per hour). The highest levels of MVPA were in the late morning and late evening hours, with a dip in activity in the early afternoon hours. Similar patterns were observed for total PA (light and MVPA combined). Inversely, sedentary behavior levels were highest in the early morning and early afternoon. Percent of each hour spent in sedentary time ranged from 46% to 58%. When comparing this pattern qualitatively by weight status, the early afternoon activity dip appeared more pronounced in the at-risk group than the overweight group.
Figure 3.
Average percent of hour spent in physical activity intensities
Figure 4.
Average percent of hour spent in MVPA by weight status.
CONCLUSIONS
Physical inactivity is a long-standing public health concern for US children.28 Though there have been recent improvements in physical activity guidelines for young children, information about current activity patterns remains largely unexplored. Importantly, it also remains unclear which patterns of activity (e.g. types of activity, timing of activity throughout the day) are associated with better health. The current study explored such activity patterns and associations with weight status in a group of young children at risk for obesity. In order to identify opportunities for a more active lifestyle, it is important to understand how children spend their time.
Because of the lack of objective measures to assess the types of activities in which children participate, we used a parent-reported measure to describe child activity types and patterns. In our sample of at-risk and overweight preschool-aged children, the majority of parents reported activities usually classified as sedentary or light intensity such as playing with toys, napping or resting, riding in a car, and watching TV. These results are in line with findings from Brown and colleagues who found children in child care settings spent a large portion of their day napping or snacking. Our findings together suggest the need to promote higher intensity activity as a routine part of the day.19
Almost all parents reported that their children engaged in some free play activities, typically considered higher intensity. Very few parents reported that their child participated in non-motorized transportation (e.g. walking to a nearby park or store). In a sample of Australian 5–6 year olds, almost 50% of parents reported their child walking or cycling to school.29 This may be a key place for intervention in younger US populations; parents can teach children from a young age to use walking or biking as a means of transportation. It is important to note that although the afore-mentioned activities are typically thought of as either sedentary or active, this may not be the case in this young population. For example, time spent eating a snack or watching TV may be interspersed with short bouts of activity. Conversely, activities normally thought of as highly active, such as sports, may be less active due to young children’s limited attention spans or motor skills. Finally, although a number of parents reported that their children spent time doing household chores (e.g. laundry, yard work), the energy expenditure associated with participation in these activities likely varies as children’s involvement is limited to the developmentally appropriate portions of the activity.
As no known criterion measures exist to test the validity of the PDPAR in measuring activity types, we conducted exploratory analyses to examine differences in activity-type participation by child weight status. The only statistically significant difference was that a higher percent of overweight children spent any time “hanging around” than children at-risk for becoming overweight. A higher proportion of overweight children in our sample spent some of their day using computers or video games compared to children at-risk for becoming overweight, but this difference was driven by the small number of participants reporting this activity and was not significantly significant. However, media use in this young population is growing rapidly,30 suggesting sedentary behavior reduction interventions are important.
Describing the overall amount of activity and the patterns through which young children accumulate this activity is also important for informing physical activity guidelines and obesity prevention intervention development. Children in this sample had more minutes of MVPA on average than the current 60-minute guidelines (mean MVPA = 69 ± 23 minutes) and they accumulated approximately 250 minutes of light physical activity throughout the day. Currently, there are no clear guidelines regarding recommended daily amounts of light physical activity for preschool-age children. MVPA and light PA appeared to be spread throughout the day with a dip in the early afternoon, presumably during nap time. Van Cauwenberghe and colleagues (2012) reported similar hourly patterns in a group of preschool children in Melbourne.16 However, they showed MVPA started out low and progressively increased throughout the day with no decline during early afternoon hours. When examining hourly patterns stratified by child weight status, children at-risk for becoming overweight appeared to have a slightly more exaggerated dip in activity during the early afternoon hours. Looking for differences in activity patterns across a range of BMI percentiles may lead to valuable insights for activity guideline and intervention development.
This study had limitations that could be addressed in future work. First, parents reporting on the PDPAR may not have spent the majority of the previous day with their child. Protocol modifications could improve the validity of the measure (e.g. administering multiple previous day recalls, changing the sensitivity of the measure by changing the 30-minute block reporting, developing tools for other caregivers to report child activity, and allowing for more detailed reporting of activity type). Another limitation was our relatively small sample size (N=59) which was relatively homogeneous with regards to weight status, given the recruitment criteria of the HHHK-Preschool RCT. Additional studies with larger, more diverse sample populations would improve generalizability and provide increased power to identify weight status differences in activity patterns.
Research in the area of physical activity measurement in preschool-aged children is necessary given the prevalence of childhood obesity and potential for improved activity patterns. Our findings highlight opportunities for increasing physical activity, such as active transportation, limiting sedentary activities such as TV and video games, and increasing the intensity and duration of free play opportunities. Our preliminary findings suggest that the relationship between activity patterns and weight status should be investigated further.
Acknowledgments
FUNDING SOURCE
This work was supported by the following grants funded by the National Institute of Diabetes and Digestive and Kidney Diseases, R21DK078239, P30DK050456 and P30DK092924.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012 Feb 1;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bauman AE. Updating the evidence that physical activity is good for health: an epidemiological review 2000–2003. Journal of Science and Medicine in Sport. 2004;7(1):6–19. doi: 10.1016/s1440-2440(04)80273-1. [DOI] [PubMed] [Google Scholar]
- 3.Timmons BW, Leblanc AG, Carson V, et al. Systematic review of physical activity and health in the early years (aged 0–4 years) Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. 2012 Aug;37(4):773–792. doi: 10.1139/h2012-070. [DOI] [PubMed] [Google Scholar]
- 4.Duncan MJ, Vandelanotte C, Caperchione C, Hanley C, Mummery WK. Temporal trends in and relationships between screen time, physical activity, overweight and obesity. BMC Public Health. 2012;12(1):1060. doi: 10.1186/1471-2458-12-1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cain KL, Sallis JF, Conway TL, Van Dyck D, Calhoon L. Using accelerometers in youth physical activity studies: a review of methods. Journal of physical activity & health. 2013 Mar;10(3):437–450. doi: 10.1123/jpah.10.3.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGuire S. Adv Nutr. 1. Vol. 3. Washington, DC: The National Academies Press; 2012. Jan, Institute of Medicine (IOM) Early Childhood Obesity Prevention Policies; pp. 56–57. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Association for Sport and Physical Education. Active Start: A Statement of Physical Activity Guidelines for Children from Birth to Age 5. 2nd ed. Sewickley, PA: American Alliance for Health, Physical Education, Recreation, and Dance; 2009. [Google Scholar]
- 8.United Kingdom Department of Health. New physical activity guidelines. 2011 [Google Scholar]
- 9.Department of Health and Ageing. Australian Government; 2010. National physical activity recommendations for children 0–5 years old. [Google Scholar]
- 10.US Department of Health and Human Services. Physical Activity Guidelines for Americans Midcourse Report: Strategies to Increase Physical Activity Among Youth. 2012 [Google Scholar]
- 11.Council on Communications and Media. Children, adolescents, and the media. Pediatrics. 2013;132(5):958. doi: 10.1542/peds.2013-2656. [DOI] [PubMed] [Google Scholar]
- 12.Mendoza JA, Zimmerman FJ, Christakis DA. Television viewing, computer use, obesity, and adiposity in US preschool children. The international journal of behavioral nutrition and physical activity. 2007;4:44. doi: 10.1186/1479-5868-4-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Soini A, Tammelin T, Sääkslahti A, et al. Seasonal and daily variation in physical activity among three-year-old Finnish preschool children. Early Child Development and Care. 2014;184(4):589–601. [Google Scholar]
- 14.Baranowski T, Thompson WO, Durant RH, Baranowski J, Puhl J. Observations on Physical Activity in Physical Locations: Ager Gender, Ethnicity, and Month Effects. Research quarterly for exercise and sport. 1993;64(2):127–133. doi: 10.1080/02701367.1993.10608789. [DOI] [PubMed] [Google Scholar]
- 15.Jackson DM, Reilly JJ, Kelly LA, Montgomery C, Grant S, Paton JY. Objectively Measured Physical Activity in a Representative Sample of 3-to 4-Year-Old Children. Obesity research. 2003;11(3):420–425. doi: 10.1038/oby.2003.57. [DOI] [PubMed] [Google Scholar]
- 16.Van Cauwenberghe E, Jones RA, Hinkley T, Crawford D, Okely AD. Patterns of physical activity and sedentary behaviour in preschool children. The international journal of behavioral nutrition and physical activity. 2012;9:138. doi: 10.1186/1479-5868-9-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benham-Deal T. Preschool children's accumulated and sustained physical activity. Perceptual and motor skills. 2005;100(2):443–450. doi: 10.2466/pms.100.2.443-450. [DOI] [PubMed] [Google Scholar]
- 18.Ruiz RM, Tracy D, Sommer EC, Barkin SL. A novel approach to characterize physical activity patterns in preschool-aged children. Obesity. 2013;21(11):2197–2203. doi: 10.1002/oby.20560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown WH, Pfeiffer KA, McIver KL, Dowda M, Almeida JM, Pate RR. Assessing preschool children's physical activity: the Observational System for Recording Physical Activity in children-preschool version. Research quarterly for exercise and sport. 2006;77(2):167–176. doi: 10.1080/02701367.2006.10599351. [DOI] [PubMed] [Google Scholar]
- 20.Trost SG, Marshall AL, Miller R, Hurley JT, Hunt JA. Validation of a 24-h physical activity recall in indigenous and non-indigenous Australian adolescents. Journal of science and medicine in sport / Sports Medicine Australia. 2007 Dec;10(6):428–435. doi: 10.1016/j.jsams.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 21.Vale S, Santos R, Silva P, Soares-Miranda L, Mota J. Preschool children physical activity measurement: importance of epoch length choice. Pediatric exercise science. 2009 Nov;21(4):413–420. doi: 10.1123/pes.21.4.413. [DOI] [PubMed] [Google Scholar]
- 22.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine and science in sports and exercise. 2008;40(1):181. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 23.Sherar LB, Griew P, Esliger DW, et al. International children's accelerometry database (ICAD): design and methods. BMC Public Health. 2011;11(1):485. doi: 10.1186/1471-2458-11-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. Journal of sports sciences. 2008;26(14):1557–1565. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- 25.Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring) 2006 Nov;14(11):2000–2006. doi: 10.1038/oby.2006.234. [DOI] [PubMed] [Google Scholar]
- 26.Janssen X, Cliff DP, Reilly JJ, et al. Predictive validity and classification accuracy of ActiGraph energy expenditure equations and cut-points in young children. PLoS One. 2013;8(11):e79124. doi: 10.1371/journal.pone.0079124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schakel SF, Sievert YA, Buzzard IM. Sources of data for developing and maintaining a nutrient database. Journal of the American Dietetic Association. 1988 Oct;88(10):1268–1271. [PubMed] [Google Scholar]
- 28.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012 Jul 21;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 29.Timperio A, Ball K, Salmon J, et al. Personal, family, social, and environmental correlates of active commuting to school. American journal of preventive medicine. 2006;30(1):45–51. doi: 10.1016/j.amepre.2005.08.047. [DOI] [PubMed] [Google Scholar]
- 30.Media CS. Zero to eight: Children's media use in America, 2013. Common Sense Media; 2013. [Google Scholar]