Abstract
Purpose
We evaluated the safety and effectiveness of the Magnetic Resonance-guided Focused Ultrasound (MRgFUS) with the ExAblate Conformal Bone System for the palliation of painful bone metastases.
Materials and Methods
Our Institutional Review Board approved this study, and all patients gave informed consent prior to enrollment. A total of six painful metastatic bone lesions in five patients were treated using MRgFUS with the ExAblate Conformal Bone System for pain palliation. The follow-up sessions were at 3 days, 2 weeks, 1, 2, and 3 months, and 1 year after treatment. Efficacy was evaluated by the changes in visual analog scale (VAS) scores. At 3-months and 1-year follow-ups, unenhanced computed tomography and contrast-enhanced MR imaging examinations were performed. All adverse events were assessed to evaluate treatment safety.
Results
All patients showed significant pain relief within 2 weeks. Two patients experienced complete pain reduction that lasted for 1 year. Two other patients showed pain relief measured as VAS scores of 2 and 4 on their last follow-up. Although the remaining patient had experienced significant pain relief in two lesions, the VAS score re-increased on his last follow-up. The size of the enhancing soft tissue mass in metastatic lesions decreased, and new bone formation was seen on follow-up images. Although adverse events were not serious, non-specific leg pain and second degree skin burn were noted.
Conclusion
MRgFUS was demonstrated to be effective palliative treatment within 2 weeks in selected patients with painful bone metastases.
Keywords: Magnetic Resonance-guided Focused Ultrasound, bone metastases, pain palliation, high-intensity focused ultrasound
INTRODUCTION
Bone pain is the most common source of cancer-related pain in patients suffering from metastatic cancer.1,2 Current approaches to treating this condition include analgesics, chemotherapy, hormonal therapy, and bisphosphonates for systemic treatment; additionally, radiation therapy, percutaneous ablative methods, and surgical stabilization may be used for local control.3,4,5
Although treatment with external beam radiation therapy (RT) is the current standard of care for patients with painful bone metastases, RT has not been effective in 20% to 30% of patients treated with this modality, and re-treatment rates have been generally reported in the range of 10-25%.6,7,8,9 Furthermore, repeating RT treatment at a site previously irradiated may not be eligible due to limitations in normal tissue radiation intolerance.10
Magnetic Resonance-guided Focused Ultrasound (MRgFUS) is a completely noninvasive thermal ablation technique that enables physicians to perform localized ablation of intracorporeal tissue by focusing the acoustic energy precisely at the targeted volume. According to previous studies, MRgFUS used with a body system can be an effective and safe treatment option for patients suffering from painful bone metastases, especially those who fail to obtain adequate pain relief by other preceding therapies or cannot take other treatment due to poor physical and functional status.8,11
The development of MRgFUS devices for various clinical pathological conditions is still an ongoing process. One of the recently developed devices is the ExAblate 2100 Conformal Bone System (InSightec, Tirat Carmel, Israel), specifically designed for bone applications. Compared to the original fixed ExAblate 2000 Body System, where the actual transducer is embedded in the MR patient table, the transducer of ExAblate 2100 Conformal Bone System has an external connection to the MR patient table. This transducer is strapped onto the patient, who is then placed on the MRI table and moved into the MRI scanner. These new features enable easy and comfortable access to multiple anatomical locations, and the patient position is more comfortable as they can avoid lying on a painful body site, thereby decreasing pain experienced during treatment. In addition, this device is equipped with an electronically steerable transducer with a higher density (1000 elements), and an integrated built-in skin cooling system that uses a cooled porous membrane. There have been no reports on using this system for patients with bone metastasis that include a long-term follow up.
The goal of this prospective, non-randomized, single-arm study was to evaluate the safety and effectiveness of the ExAblate Conformal Bone System for the palliation of painful bone metastases.
MATERIALS AND METHODS
Study design and patient population
This study was approved by our Institutional Review Board, and informed consent was obtained from all patients prior to enrollment. The study was supported by a research grant from InSightec (Tirat Carmel, Israel); however, the authors had complete control of the data for the purpose of this study, with no influence from the company during the preparation of this manuscript.
From March to September 2012, six consecutive patients with painful bone metastases were enrolled in our study. One patient was excluded during the screening period due to disease progression that caused paralysis in both legs. Ultimately, five patients were treated with MRgFUS (two females, three males; average age, 60 years; range, 51-68 years). All patients had undergone chemotherapy before the enrollment. One lesion had been treated by RT previously. However, the RT had not been effective; therefore, MRgFUS treatment was performed on the lesion. One patient was treated twice with MRgFUS for two different lesions, which were conducted about a month apart.
The main inclusion criteria were painful bone metastases with an Numerical Rating Scale pain score of 4 or higher and five or fewer distinguishable lesions, each of which were clearly visible on non-contrast MRI and accessible to the conformal bone system. The critical exclusion criteria were standard contraindications to MR imaging or gadolinium-based contrast agents, active infection or severe systemic disease (excluding the primary malignancy), and target tumors at an impending fracture site of weight-bearing bone or at a depth of less than 1 cm under the skin.
Imaging protocol
Baseline CT and MR images were obtained to identify the tumor size and location, adjacent anatomic structures, and device accessibility. Unenhanced CT imaging (100-120 kV with automated tube current modulation; kernel, B31f; window level, 570 HU; window width, 3000 HU; slice thickness, 3-5 mm; Somatom with CARE Dose4D; Siemens Medical Solutions, Forchheim, Germany) was performed if pre-screening CT images within 1 month before enrollment were not available. MR images included pre-contrast T1-weighted sequences with fat suppression [fast spoiled gradient-echo sequence, repetition time (ms)/echo time (ms), 355/2.18; field of view, 36; matrix, 256×256; band-width, 61.05; flip angle, 90°; section thickness, 4 mm] followed by gadolinium-enhanced (Gadodiamide, 10 mg; Omniscan, GE Healthcare, Mississauga, Ontario, Canada) T1-weighted images with the same sequence. T2-weighted sequences with and without fat suppression (fast spin-echo sequence, 6479/74; field of view, 36; matrix, 256×256; bandwidth, 61.05; section thickness, 5 mm) were performed before the contrast-enhanced study.
Treatment process
Before treatment, all patients underwent regional anesthesia using epidural or brachial plexus anesthesia according to the target tumor, and sedation was also administered to alleviate patients' nervousness.
MRgFUS treatments were carried out using a focused ultrasound phased array system (ExAblate 2100 System, InSightec Ltd., Tirat Carmel, Israel) integrated with a clinical 3.0-T MR Scanner (Discovery MR 750; GE Medical Systems, Milwaukee, WI, USA). This new version of the ExAblate Conformal Bone System has a flexible transducer assembly that operates at a lower frequency (550 kHz) and has an acoustic power range of up to 200 W. In addition, it is equipped with an electronically steerable 1000-element transducer (focus steering range, ±35 mm; weight, 1.5 kg with water) and a water-permeable membrane to provide effective acoustic coupling and an integrated built-in skin cooling system.
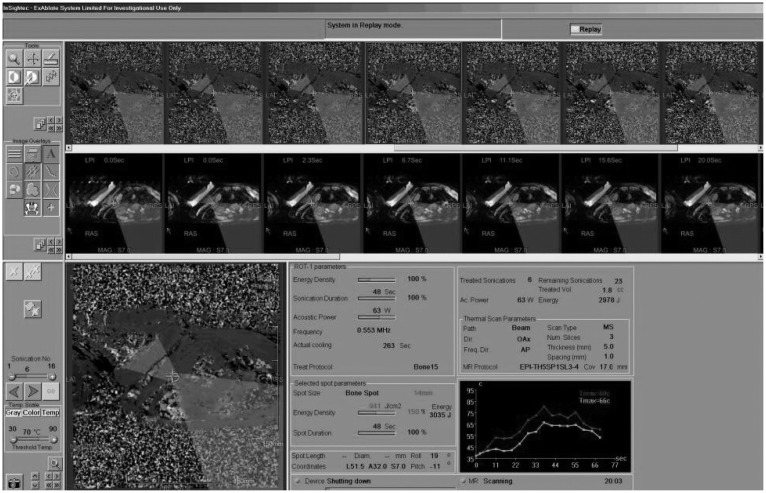
After patients were set up with the ExAblate Conformal Bone System by strapping the transducer over the targeted tumor, T2-weighted MR images in all three orientations were acquired to confirm that the transducer was in the correct location relative to the target. Upon completion of CT-MR registration, which assists bone cortex identification, treatment volume was drawn, and the number of treatment sonications that was needed to complete the desired treatment using the MRgFUS system was computed. Test sonications with a low temperature rise were performed to ensure the targeting accuracy; then, sonications at a therapeutic power level were performed. Throughout the treatment, each sonication's location and the temperature elevation in the tissue adjacent to the targeted bone were monitored in real-time (Fig. 1). Immediately after treatment, a series of MR scans including T2-weighted sequences and T1-weighted contrast enhanced sequences were performed to evaluate the general anatomy, the extent of the thermal ablation, and the possibility of eventual unexpected adverse events after the ablative process. There were no differential planning options for osteolytic or mixed lesions available in the version used for these treatments.
Fig. 1.
Procedure image. The continuous MR imaging system allows the physician to identify and target tumors and provides temperature monitoring of the treated tissue in real time.
Assessment of treatment efficacy and safety
Patients were followed for a period of up to 1 year. The follow-up sessions were at 3 days, 2 weeks, 1, 2, and 3 months, and 1 year after treatment. To evaluate efficacy and safety of the MRgFUS treatment, each follow-up section included an evaluation of patient status, changes in pain levels by visual analog scale (VAS) pain questionnaires, changes in analgesic medication intake, and any procedure-related adverse event. Pain relief indicated by a VAS score of 2 or morewas defined as significant pain relief.
At 3-months follow-up, unenhanced CT and contrast-enhanced MR imaging examinations were performed (imaging protocols were similar to those of baseline imaging).
RESULTS
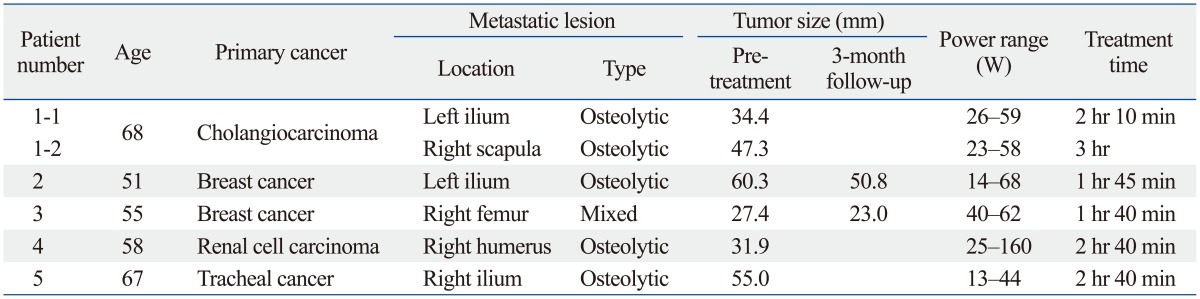
A total of six painful metastatic bone lesions in five patients were treated by MRgFUS in this study. The primary tumor origins were the breast (n=2), kidney (n=1), liver (n=1), and trachea (n=1). The locations of treated bone lesions included the ilium (n=3), scapula (n=1), femur (n=1), and humerus (n=1). Five lesions were osteolytic, and one lesion was mixed type. The number of sonications was between 15 and 20 times per treatment. The energy range of sonication was between 400 J and 4800 J, and the power range was between 13 W and 160 W. The length of treatment ranged from 100 to 180 minutes. Four treatments were conducted under epidural anesthesia, and two treatments used a brachial plexus block. Conscious sedation was sufficient for five treatments, while one treatment required deep sedation (Table 1).
Table 1.
Patient and Targeted Lesion Characteristics
Patient 1 was treated at two different sites and followed-up 60 days after treatment on the left iliac bone and 30 days after treatment on the right shoulder. Patients 2 and 3 were followed-up 1 year after treatment, while Patients 4 and 5 were followed-up 60 and 30 days after treatment, respectively. Two patients (Patient 1 and Patient 5) died before reaching the last follow-up session, and one patient (Patient 4) was unable to visit for a 3-month CT and MRI due to rapid progression of systemic neoplastic disease.
Table 2 shows the changes in the worst VAS scores over time. Significant pain relief was achieved within 3 days (n=3), 7days (n=2), and 14 days (n=1). The two patients with breast cancer completed the scheduled follow-up (1 year), and the worst VAS score at 1 year was 0. The three patients who could not complete the planned follow-up due to rapid progression of their primary cancer yielded the following worst VAS score changes: Patient 1 exhibited a re-exacerbation in VAS score, Patient 4's score remained at the same level as the early response, and Patient 5's score was further reduced to 1.
Table 2.
Changes in the Worst VAS Scores on Follow-Up
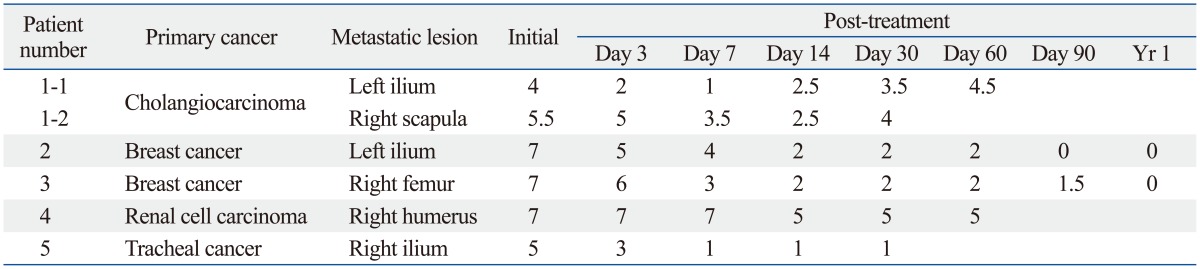
VAS, visual analog scale.
Patient 1, who had right scapular pain, had limitations in the movement of his right arm and difficulty during meals. After the treatment, he had no more difficulty in using his right arm up to death, despite the re-increase in the VAS score. Patient 2, who had a metastatic lesion on the left iliac bone due to breast cancer, had difficulty in hip joint rotation and hardly walked. After treatment, her hip joint rotation became free, and her daily average walking distance increased to 4 km. The other patients did not describe any movement limitations before or after treatment.
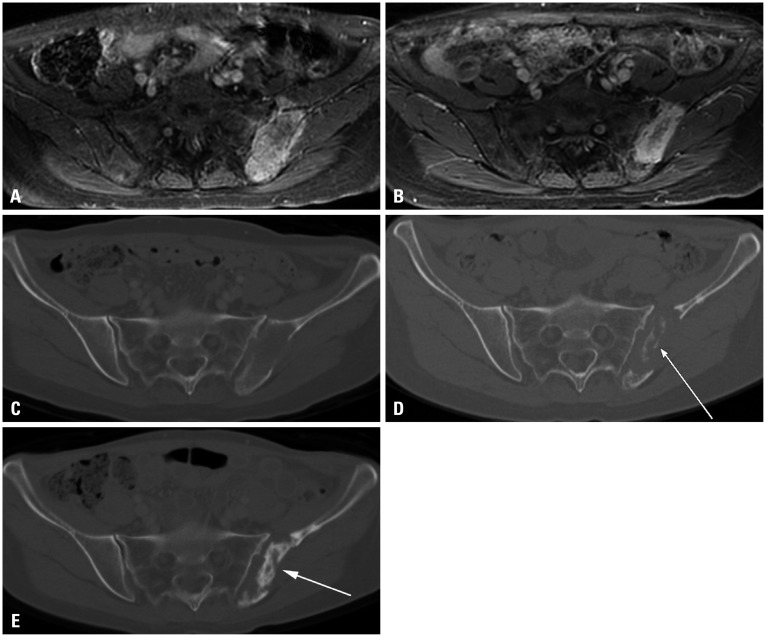
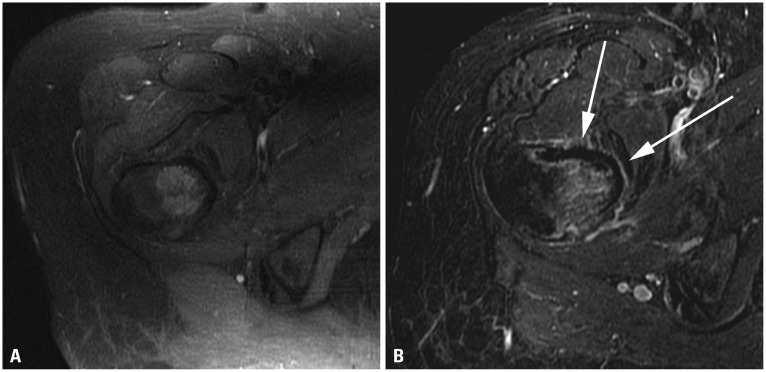
Follow-up CT and MR imaging at 90 days after treatment were obtained for the two patients who completed the schedule. In Patient 2, the size of the enhancing soft tissue mass in the metastatic lesion had decreased, and a new bone formation was seen (Fig. 2). In Patient 3, the enhancing soft tissue mass did not significantly change in size; however, a non-perfusion area was seen at the anterior periosteum of the femur (Fig. 3).
Fig. 2.
Patient 2 with breast cancer. Comparison of (A) contrast-enhanced T1-weighted MR image before treatment, (B) contrast-enhanced T1-weighted MR image at 90 days after treatment; note the decrease in size of the enhancing mass, especially right to left diameter. Comparison of (C) CT before treatment, (D) CT at 90 days after treatment; note the new bone formation (arrow). Further new bone formation (arrow) was seen on (E) CT at 1 year after treatment.
Fig. 3.
Patient 3 with breast cancer. Comparison of (A) contrast-enhanced T1-weighted MR image before treatment, (B) contrast-enhanced T1-weighted MR image at 90 days after treatment; note the newly-developed linear, non-perfused area (arrows) at the anterior periosteum of the femur.
Due to the anesthesia administered before the beginning of each treatment, all patients did not complain of any pain during the treatment. Although there were no severe adverse events related to the ExAblate Conformal Bone System treatment, two minor adverse events were noted in this study. Patient 3 complained of sonication-related leg pain one day after MRgFUS treatment; however, this symptom resolved spontaneously within 2 weeks without any specific treatment. On the MRIs taken immediately and 90 days after treatment, there were no abnormalities in the adjacent nerves, including the sciatic nerve. Another adverse event was a skin burn on Patient 4, who had right humerus bone metastasis from renal cell carcinoma. One day after the treatment, there were second degree skin burns on the right humerus and chest wall, the side opposite to where the transducer was placed. These burns resolved spontaneously within 1 week.
DISCUSSION
Our preliminary study suggests that MRgFUS using the ExAblate Conformal Bone System seems to be an effective palliative treatment in selected patients with painful bone metastases, without serious adverse events.
The two patients with breast cancer showed complete response lasting more than 1 year, despite the progression of the tumor burden at primary and other metastatic sites. Considering that there were no adverse events observed at 1 year and that the procedure could be repeated as necessary, MRgFUS using the ExAblate Conformal Bone System can be a good treatment option, especially for patients with a long life expectancy.
Several previous studies reported the use of MRgFUS for pain palliation therapy performed on patients with bone metastases. These studies reported that MRgFUS can be an effective palliative treatment for selected patients with painful bone metastases without device-related serious adverse events. In previous body system studies, however, occasional difficulties were reported in positioning the patient over the water bath when bone lesions were in areas where placement in contact with the treatment transducer was difficult. Moreover, previous treatments performed using fixed position transducers could provoke pain during treatment by requiring patients to lie on a painful body site.8,11 The ExAblate Conformal Bone System used in the present study overcame these limitations by using a flexible transducer assembly, thereby enabling easy and comfortable access to multiple anatomical locations and reducing positioning-related pain in patients.
The mechanism of the analgesic effect on bone metastasis is assumed to be mainly periosteal denervation induced by high ultrasound energy absorption of the bone cortex. Another possible mechanism could be a reduced mass effect by thermal ablation of the tumor. The acoustic absorption of bone tissue is higher than that of soft tissue, and the penetration of ultrasonic energy into the bone can be minimal. Due to the low thermal conductivity and high acoustic absorption rate of the bone cortex, MRgFUS for bone metastases can be conducted using lower energy levels than MRgFUS for soft tissue tumors. This feature minimizes the thermal damage around the treated bone site while still achieving a localized heating effect.
In addition to volume reduction, new bone formation has been reported in several patients with osteolytic bone metastasis treated with MRgFUS.8,11,12 A possible explanation for this observation is that thermal ablation by MRgFUS could lead to accelerated bone healing with subsequent sclerosis at the osteolytic lesion. In our study, one patient with osteolytic metastasis demonstrated new bone formation on 3-month follow-up CT and progressive formation on 1-year follow-up CT.
The thermal effect of high-energy focused ultrasound induces cell death and tissue coagulation necrosis. MR thermometry based on the shift in proton resonance frequency caused by temperature rise makes real-time thermal mapping possible.13,14,15 The integration of focused ultrasound with MR thermometry enables the system operator to target and treat metastatic bone lesions accurately and safely, avoiding destruction of surrounding normal tissue by using the real-time closed loop control.
The device has a relatively high safety profile compared with alternatives. In our study, however, there were two adverse events, though not serious. One patient with sonication-related leg pain was clinically suspected to have a transient sciatic nerve injury. One of the known complications of MRgFUS is nerve injury due to the lower tolerance of nerves to the high temperature.16 The other adverse event in our study was a second degree skin burn on the side of the body opposite to where the transducer was positioned. There have been several reports of skin burns on the same side as the transducer due to entrapped air between the body and the transducer.17,18 However, our case shows a skin burn on the side opposite the transducer. This skin burn on the anterior arm might be related to energetic sonications that were not fully intersecting the body tissue, causing far field heating due to reflection from the skin-air interface. Due to the relatively low frequency of the conformal bone transducer, there is a deeper penetration of the energy. There is no upper limit to the accumulated acoustic energy as the energy is nonionizing. Therefore, the treatment can be repeated as long as tissue temperature is kept at a safe level. This feature makes MRgFUS more effective and useful than external-beam radiation therapy, which is currently considered as the standard treatment of bone metastases. Furthermore, MRgFUS does not require the insertion of any probe or needle into the patient, making the procedure completely noninvasive.
In conclusion, MRgFUS was shown to be a long-lasting, effective palliative treatment in selected patients with painful bone metastases. In addition to pain palliation, our results suggest MRgFUS as a potential treatment option for long-lasting local tumor control.
ACKNOWLEDGEMENTS
This study was sponsored by InSightec, titled "A Study to Evaluate the Safety and Initial Effectiveness of ExAblate MR Guided Focused Ultrasound Surgery in the Treatment of Pain Resulting from Metastatic Bone Tumors with the ExAblate 2100 Conformal System (Protocol BM012)".
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Roodman GD. Mechanisms of bone metastasis. N Engl J Med. 2004;350:1655–1664. doi: 10.1056/NEJMra030831. [DOI] [PubMed] [Google Scholar]
- 2.Mercadante S. Malignant bone pain: pathophysiology and treatment. Pain. 1997;69:1–18. doi: 10.1016/s0304-3959(96)03267-8. [DOI] [PubMed] [Google Scholar]
- 3.Rades D, Schild SE, Abrahm JL. Treatment of painful bone metastases. Nat Rev Clin Oncol. 2010;7:220–229. doi: 10.1038/nrclinonc.2010.17. [DOI] [PubMed] [Google Scholar]
- 4.Sze WM, Shelley MD, Held I, Wilt TJ, Mason MD. Palliation of metastatic bone pain: single fraction versus multifraction radiotherapy--a systematic review of randomised trials. Clin Oncol (R Coll Radiol) 2003;15:345–352. doi: 10.1016/s0936-6555(03)00113-4. [DOI] [PubMed] [Google Scholar]
- 5.Callstrom MR, Charboneau JW, Goetz MP, Rubin J, Atwell TD, Farrell MA, et al. Image-guided ablation of painful metastatic bone tumors: a new and effective approach to a difficult problem. Skeletal Radiol. 2006;35:1–15. doi: 10.1007/s00256-005-0003-2. [DOI] [PubMed] [Google Scholar]
- 6.Cole DJ. A randomized trial of a single treatment versus conventional fractionation in the palliative radiotherapy of painful bone metastases. Clin Oncol (R Coll Radiol) 1989;1:59–62. doi: 10.1016/s0936-6555(89)80035-4. [DOI] [PubMed] [Google Scholar]
- 7.8 Gy single fraction radiotherapy for the treatment of metastatic skeletal pain: randomised comparison with a multifraction schedule over 12 months of patient follow-up. Bone Pain Trial Working Party. Radiother Oncol. 1999;52:111–121. [PubMed] [Google Scholar]
- 8.Gianfelice D, Gupta C, Kucharczyk W, Bret P, Havill D, Clemons M. Palliative treatment of painful bone metastases with MR imaging--guided focused ultrasound. Radiology. 2008;249:355–363. doi: 10.1148/radiol.2491071523. [DOI] [PubMed] [Google Scholar]
- 9.Saarto T, Janes R, Tenhunen M, Kouri M. Palliative radiotherapy in the treatment of skeletal metastases. Eur J Pain. 2002;6:323–330. doi: 10.1016/s1090-3801(02)00028-9. [DOI] [PubMed] [Google Scholar]
- 10.Goetz MP, Callstrom MR, Charboneau JW, Farrell MA, Maus TP, Welch TJ, et al. Percutaneous image-guided radiofrequency ablation of painful metastases involving bone: a multicenter study. J Clin Oncol. 2004;22:300–306. doi: 10.1200/JCO.2004.03.097. [DOI] [PubMed] [Google Scholar]
- 11.Liberman B, Gianfelice D, Inbar Y, Beck A, Rabin T, Shabshin N, et al. Pain palliation in patients with bone metastases using MR-guided focused ultrasound surgery: a multicenter study. Ann Surg Oncol. 2009;16:140–146. doi: 10.1245/s10434-008-0011-2. [DOI] [PubMed] [Google Scholar]
- 12.Napoli A, Anzidei M, Marincola BC, Brachetti G, Ciolina F, Cartocci G, et al. Primary pain palliation and local tumor control in bone metastases treated with magnetic resonance-guided focused ultrasound. Invest Radiol. 2013;48:351–358. doi: 10.1097/RLI.0b013e318285bbab. [DOI] [PubMed] [Google Scholar]
- 13.Ishihara Y, Calderon A, Watanabe H, Okamoto K, Suzuki Y, Kuroda K, et al. A precise and fast temperature mapping using water proton chemical shift. Magn Reson Med. 1995;34:814–823. doi: 10.1002/mrm.1910340606. [DOI] [PubMed] [Google Scholar]
- 14.Chung AH, Jolesz FA, Hynynen K. Thermal dosimetry of a focused ultrasound beam in vivo by magnetic resonance imaging. Med Phys. 1999;26:2017–2026. doi: 10.1118/1.598707. [DOI] [PubMed] [Google Scholar]
- 15.McDannold N, King RL, Jolesz FA, Hynynen K. The use of quantitative temperature images to predict the optimal power for focused ultrasound surgery: in vivo verification in rabbit muscle and brain. Med Phys. 2002;29:356–365. doi: 10.1118/1.1449495. [DOI] [PubMed] [Google Scholar]
- 16.Hindley J, Gedroyc WM, Regan L, Stewart E, Tempany C, Hynyen K, et al. MRI guidance of focused ultrasound therapy of uterine fibroids: early results. AJR Am J Roentgenol. 2004;183:1713–1719. doi: 10.2214/ajr.183.6.01831713. [DOI] [PubMed] [Google Scholar]
- 17.Leon-Villapalos J, Kaniorou-Larai M, Dziewulski P. Full thickness abdominal burn following magnetic resonance guided focused ultrasound therapy. Burns. 2005;31:1054–1055. doi: 10.1016/j.burns.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 18.Stewart EA, Gedroyc WM, Tempany CM, Quade BJ, Inbar Y, Ehrenstein T, et al. Focused ultrasound treatment of uterine fibroid tumors: safety and feasibility of a noninvasive thermoablative technique. Am J Obstet Gynecol. 2003;189:48–54. doi: 10.1067/mob.2003.345. [DOI] [PubMed] [Google Scholar]