Abstract
Generally, giant cell tumors are rare and their localization in the spine is even more so. They are locally aggressive leading to spine instability and neurologic deficits. Radical excision is highly advocated. A role of radiotherapy in these tumors is controversial. We report the case of a giant cell tumor localized in D1 and D2 on a 39-year-old patient, presented with interscapular back pain, paraparesis grade 3/5 and sphincter dysfunction. Thoracic spine computed tomogarphy and magnetic resonance imaging showed a vertebral body tumor in D1 and D2, compressing the spinal cord at the same level. The patient initially underwent decompressive laminectomy of affected levels and stabilized with laminar hooks and rods. Second surgery performed through an anterior approach whereby tumor excision together with corpectomy of D1 and D2 carried out, autograft was placed and plate applied. Three weeks postoperatively, the patient's neurologic deficit recovered fully and back pain subsided.
INTRODUCTION
Spine giant cell tumors are rare, and if occurs commonly are located on the sacrum [1]. Although they are benign, their prognosis is dominated by their aggressiveness and neuronal structures involvement, recurrence and the risk of malignant transformation [2]. Their surgical management should be radical excision whenever possible, accompanied by stabilization of the spine [2]. We report the case of a patient with uncommon spinal location of giant cell tumor.
CASE REPORT
A thirty-nine-year-old patient with no history of trauma or constitutional symptoms who reported upper thoracic back pain lasting for 8 months before seeking medical attention. The pain was dull in nature to begin with, gradually progressive in intensity and not posture related. Initially, the pain was responding to conventional non steroidol anti-inflammatory drugs (NSAIDs). There was a marked increase in pain intensity in last 4 days before admission, and this was accompanied by inability to walk due to lower limb weakness and urinary incontinence. The neurologic examination revealed power grade 3/5 in all lower limb muscle groups, hypesthesia to the level of nipples and locally there was tenderness on D1–D2 level. The rest of his physical examination found no other abnormalities.
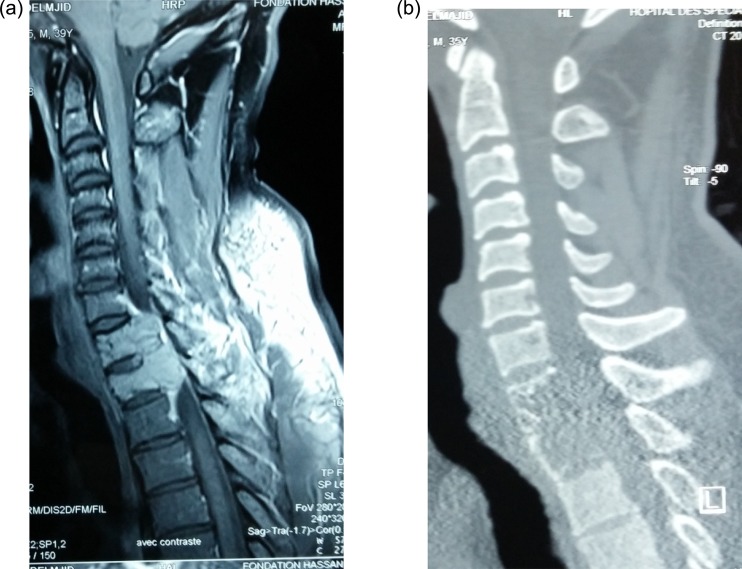
The thoracic spine computed tomography (CT) and magnetic resonance imaging (MRI) showed a tumor involving D1 and D2 vertebral bodies. The lesions are osteolytic eroding the two vertebrae with extension into the spinal canal and enhancing with gadolinium. The patient underwent emergency decompressive laminectomy of D1 and D2 together with stabilization by laminar hooks and rods through C7–D3 (Figs 1 and 2). The biopsy histology revealed to be in favor of a giant cell tumor.
Figure 1:
Preoperative gadolinium-enhanced MRI (a) and CT (b) showing expansile lytic tumor at D1 and D2 and compression of the cord at these levels.
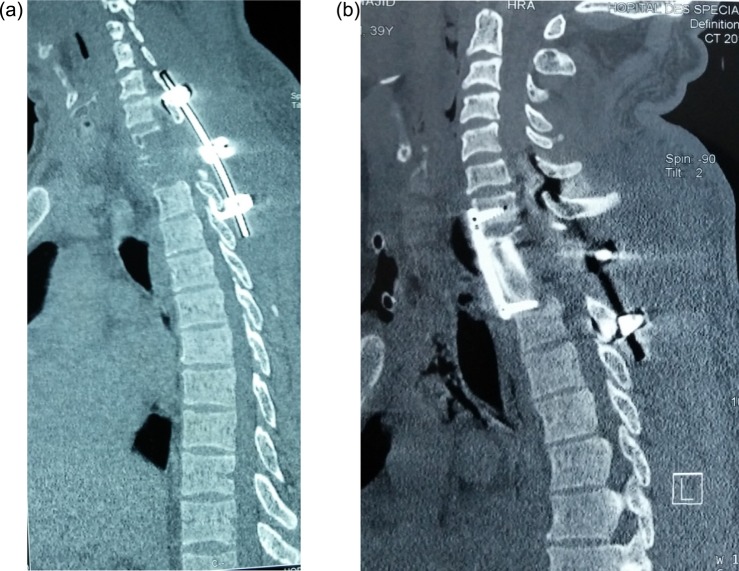
Figure 2:
Postoperative sagittal CT showing (a) hook and rod stabilization posteriorly, and (b) bone graft and plate fixation anteriorly after corporectomy of D1 and D2.
Given this diagnosis, a second-stage surgery was performed 2 weeks later. This was performed by an anterior approach whereby cervicothoracic incision extending from lower cervical (C6) to upper thoracic (D3) was performed. It involved detachment of two heads of sternocleidomastoid muscles on the right side, and medial third of right clavicle was excised. The innominate artery and superior vena cava were identified and retracted exposing pathological vertebrae. Corpectomies of D1–D2 carried out, and residual tumor on posterior longitudinal ligament (PLL) and other surrounding structure was excised. Strut graft from the clavicle was placed to bridge the defect and stabilized by anterior plate bridging between C7 and D3.
He fared well postsurgery, at 4 weeks, the neurological deficit improved and the power was grade 4/5. At 6 weeks, he had fully recovery of sensorimotor functions on lower limbs and trunk. The control CT scan showed a good restoration of the spinal canal dimensions. At 3 months, the patient has no back pain. He did not receive radiation therapy as it has been found to be controversial interims of recurrence.
DISCUSSION
Giant cell tumors are classified benign, but can be very aggressive locally with a risk of malignant transformation in 10% of cases [3]. Their spinal localization is rare outside the sacrum or they are the third most common type of tumor after plasmacytoma and chordoma [3]. They occur between the second and fourth decade of life with a female predominance of up to 70% for spinal locations [1]. These tumors have predilection to vertebral bodies and spares the posterior arch in majority of cases.
Clinically, the patient experiences constant back pain which increases as tumor expands and destroys the architecture of involved vertebra [4]. The radicular and myelopathic symptoms and signs appear later, as in the case of our patient [1, 2]. Giant cell tumors are radiologically destructive lesions, lytic and expansile with irregular edges, sometimes condensing with surrounding tissues. A CT scan allows proper assessment of the cortical involvement and extension into the soft tissues. The MRI shows the tumor in several planes and the details of soft tissue involvement [4]. The main radiological differential diagnoses are spine aneurysmal bone cyst and osteoblastoma mostly found in the posterior arch. Others are plasmacytoma, chordoma and lytic metastasis [5].
The histological examination of giant cell tumor can be difficult since giant cells are present in several bone tumors. Presence of multiple multinucleated giant cells within a stroma of mononuclear cells, hemorrhagic foci, telangiectasia entholialized and no evidence of ossification points to giant cell tumors [5].
Three histological grades of aggressiveness (I–III) have been described: mild aggressive (benign), moderate aggressive (borderline) and malignant [6].
The therapeutic management of spinal giant cells tumors is surgical. The resection should be radical whenever it is possible because of local aggressiveness, frequent recurrence and the risk of malignant transformation [1–4]. Giant cell tumors are chemoresistant and the place of radiation therapy is controversial [5]. Indeed, many authors have questioned its effectiveness, neurological risks and the potential for sarcomatous transformation. It is reserved only for cases where the location or extension makes it impossible surgery [7]. Giant cell tumors are often very vascular requiring vertebrobasilar spinal arteriography and preoperative selective embolization to limit bleeding intraoperatively [8]. Radical resection appears to be the best treatment for giant cell tumors. Indeed, Dahlin [9] in his study reported 75% of good results at 5 years and above, following local wide resection (normal clinical findings and no tumor recurrence). If tumor involves the posterior arch as well, corpectomy and excision of posterior arch components should be performed; as in the case of our patient with a posterior arch involvement, the first stage surgery was excision of tumor extension to posterior arch elements together with freeing the cord and stabilization. Second-stage surgery was aimed at removal of primary tumor and cord decompression anteriorly, grafting and stabilization with plate. Additional treatment was not considered necessary in our patient given the radical nature of our surgery.
The prognosis is determined by the risk of recurrence of up to 25% for the spine in a period of 2 years and malignant transformation. There are no real predictive factors of possible radiological or histological recurrence. Only a radical resection reduces this risk [5]. For our patient's outcome was favorable with complete recovery of his neurological deficit and the disappearance of pain till the end of first 6-month follow-up. Spinal locations of giant cell tumors require radical treatment whenever possible to improve survival and prevent early recurrence.
CONFLICT OF INTEREST STATEMENT
The authors have no personal financial or institutional interest in any of the drugs, materials or devices described in this article.
REFERENCES
- 1.Laffargue PH, Cotten A, Cortet B, Leconte Houcke M, Decoulx J. Giant cell tumors of spine: a case report and literature review. Acta Orthop Belg. 1997;63:28–34. [PubMed] [Google Scholar]
- 2.Yoichi S, Michio H, Naohisa M, Yuji K, Shigeru A, Eiji I, Eiji A. Giant cell tumor of fifth lumbar vertebrae: two case reports and review of the literature. Spine J. 2007;7:499–505. doi: 10.1016/j.spinee.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 3.Diabira SM, Riffaud L, Haegelen C, Hamlat A, Hénaux PL, Brassier G, et al. Intraspinal and spine tumors. EMC Neurol. 2011;11:1–22. [Google Scholar]
- 4.Turcotte RE, Isler M, Doyon J. Giant cell tumors. Orthop Clin North Am. 2006;37:35–51. doi: 10.1016/j.ocl.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 5.Bergamasco P, Rousiere M, Manet MP, Plantin P, Monteiro L, Le Parc JM. Giant cell tumor of lumbar spine: a case report and review of the literature. Rachis J. 1999;11:229–32. [Google Scholar]
- 6.Noël G, Benjelloun H, Feuvret L, Calugaru V, Mazeron JJ, Habrand J-L. Two cases of giant cell tumors of the skull base: review of literature. Cancer Radiother. 2006;10:175. doi: 10.1016/j.canrad.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Chekrine T, Tawfiq N, Bourhaleb Z, Benchakroun N, Jouhadi H, Sahraoui S, et al. Two cases of bone giant cell tumors of the spine and review of the literature. Cancer Radiother. 2009;13:451–4. doi: 10.1016/j.canrad.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Prando A, De Santos LA, Wallace S, Murray JA. Angiography in giant cell tumors. Radiology. 1979;130:323–31. doi: 10.1148/130.2.323. [DOI] [PubMed] [Google Scholar]
- 9.Dahlin DC. Giant cell tumor of vertebrae above the sacrum. A review of 31 cases. Cancer. 1977;39:1350–6. doi: 10.1002/1097-0142(197703)39:3<1350::aid-cncr2820390351>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]