A substantial proportion of individuals infected with the human immunodeficiency virus (HIV) in the United States enter a correctional facility annually.1,2 Therefore, incarceration presents an opportunity for HIV detection. Even though many states have adopted policies of mass HIV screening of inmates,2–4 the extent to which HIV testing on prison entry detects new infections is unclear.
We examined HIV prevalence among inmates entering a state prison system and the proportion known to state public health authorities as having previously tested HIV seropositive.
Methods
We evaluated individuals entering the North Carolina Department of Public Safety (NC DPS) between June 2008 and April 2009. Testing entering inmates for HIV in North Carolina was voluntary; however, a state statute mandated screening for syphilis. Excess blood was batch tested for HIV antibodies (Labcorp Inc). Before removing links to the inmate’s HIV test result, identifiers were used to merge prison test results with the North Carolina Department of Health and Human Services (NCDHHS) HIV testing database. The University of North Carolina biomedical institutional review board, the NCDPS human subjects review committee, and the US Office of Human Research Protections approved the study. A waiver of informed consent was provided.
Results
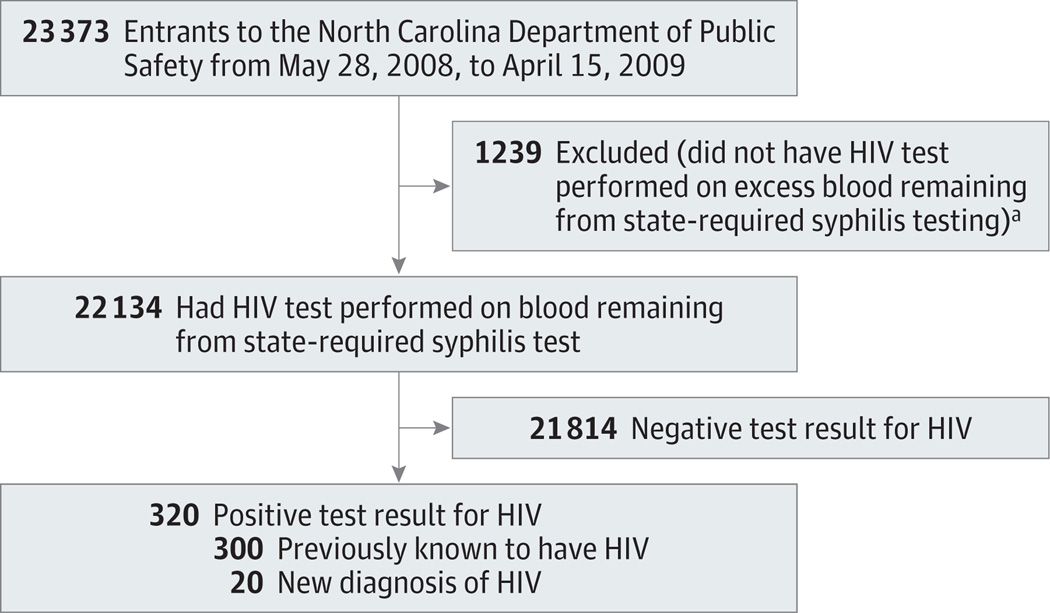
During the study period, 23 373 inmates entered the NC DPS (Table); most were black men and more than half had a prior incarceration. Of these 23 373 inmates, 22 134 (94.7%) had HIV testing performed on blood remaining after syphilis testing (Figure). Reasons for not having an HIV test included no blood drawn, insufficient quantity, or lost specimen. Testing of excess blood revealed 320 inmates (1.45%) to be HIV seropositive. Of those who tested HIV seropositive, 300 (93.8%) were known by the NC DHHS to be infected with HIV prior to incarceration. Therefore, 20 of 22 134, or 0.09% (95%CI, 0.06%–0.14%) of tested inmates were infected and not known to be previously.
Table.
Characteristics of Inmates Entering Prison in North Carolina
| No. (%) of Inmates | |||
|---|---|---|---|
| New to NC DPS (n = 23 373) |
HIV Test of Excess Blooda | ||
| Yes (n = 22 134) |
No (n = 1239) |
||
| Sex | |||
| Female | 2657 (11.4) | 2499 (11.3) | 158 (12.8) |
| Male | 20 701 (88.6) | 19 620 (88.7) | 1081 (87.3) |
| Missing | 15 (<1) | 15 (<1) | 0 |
| Raceb | |||
| White | 9311 (39.84) | 8844 (39.96) | 467 (37.69) |
| Black | 12 570 (53.78) | 11 860 (53.58) | 710 (57.30) |
| Native American | 366 (1.57) | 352 (1.59) | 14 (1.13) |
| Asian | 47 (0.20) | 44 (0.20) | 3 (0.24) |
| Otherc | 934 (4.00) | 899 (4.06) | 35 (2.82) |
| Unknown | 145 (0.62) | 135 (0.61) | 10 (0.81) |
| Prior incarceration | |||
| Yes | 12 184 (52.1) | 11 585 (52.3) | 599 (48.4) |
| No | 11 188 (47.9) | 10 548 (47.7) | 640 (51.7) |
| Missing | 1 (<1) | 1 (<1) | 0 |
Abbreviations: HIV, human immunodeficiency virus; NC DPS, North Carolina Department of Public Safety.
None of the distributions of the characteristics were significantly different among inmates with a study HIV test vs those without.
Self-reported.
Other included inmates who identified as having mixed race.
Figure 1.
Testing of Inmates Entering the North Carolina Prison System for Human Immunodeficiency Virus (HIV)
aThere were 1066 inmates who did not have HIV test performed on excess blood remaining from state-required syphilis testing but who were tested for HIV by the prison system. Of these, 36 tested positive for HIV and all were previously known by the North Carolina Department of Health and Human Services to be infected with HIV.
Among the 1239 entering inmates without HIV testing of excess blood, 1066 underwent voluntary HIV testing by the prison, 36 of whom (4.8%) were HIV seropositive. All 36 were previously known by the NC DHHS to be infected with HIV.
Discussion
Although the overall prevalence of HIV infection was high at 1.45%, the prevalence of undiagnosed infection was 0.09% and the yield of screening of individuals entering prison in North Carolina was low, with more than 93% of infected inmates previously known by health authorities to be infected. Therefore, in contrast to the perception that undiagnosed HIV infection is prevalent among incarcerated individuals, our results indicate that few new cases of HIV enter prison. The confidence interval around the prevalence of undiagnosed infection included 0.1%, the threshold above which the US Centers for Disease Control and Prevention recommends routine HIV screening in health care settings.5 Other at-risk populations with higher levels of undiagnosed HIV infection may constitute a higher priority for screening for HIV than prisoners. Of all new HIV diagnoses in North Carolina in 2008–2009, less than 2% were prison entrants.6
There are limitations to our study. Prior HIV testing may have occurred as a consequence of screening during a previous incarceration, although almost half of the inmates with known HIV infection had no history of incarceration. Additionally, some with a prior positive HIV test may not have received their results and without screening upon incarceration would remain unaware of their HIV status. However, according to the NCDHHS, 90% of those testing HIV seropositive in North Carolina in 2008–2009 were notified of their results. Furthermore, although North Carolina has the eighth highest prevalence of HIV in the United States, these results may not generalize to other states. In addition, the few cases of previously unknown HIV coupled with limited available inmate data precluded analyses to identify prisoner characteristics that could be used to enhance detection of undiagnosed HIV infection.
Acknowledgment
Funding/Support: This research was supported by grant R01 MH079720-01A1 from the National Institute of Mental Health and grant AI 50410-04 from the University of North Carolina Center for AIDS Research.
Role of the Sponsor: The National Institute of Mental Health and the University of North Carolina Center for AIDS Research had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We acknowledge the contributions of the following co-investigators who assisted in study design and analysis: Andrew Kaplan, MD, J. Michael Bowling, PhD, Peter Leone, MD, and Robert Devellis, PhD (all with the University of North Carolina, Chapel Hill); Paula Smith, MD (North Carolina Department of Public Safety [NC DPS]); and Rebecca Ochtera, PhD (Kaiser-Permanente). We also acknowledge the University of North Carolina, Chapel Hill, research staff: Kelly Green, MPH, Monique Williams, Dani Strauss, Makisha Ruffin, and Catherine Grodensky, MPH. The NC DPS facility nurses and administrators and the North Carolina Department of Health and Human Services Communicable Disease Branch provided access and constructive advice to the research team. Drs Bowling, Devellis, and Leone and Mss Green, Williams, Strauss, and Ruffin received salary support from the National Institutes of Health grant supporting the study. Drs Kaplan, Smith, and Ochtera and Ms Grodensky did not receive compensation for their contributions.
Footnotes
Author Contributions: Dr Wohl had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Wohl, Golin, Rosen, White.
Acquisition of data: Wohl, White.
Analysis and interpretation of data: Wohl, Golin, Rosen, May, White.
Drafting of the manuscript: Wohl, May, White.
Critical revision of the manuscript for important intellectual content: Wohl, Golin, Rosen, White.
Statistical analysis: Wohl, Rosen, May.
Obtained funding: Wohl, Golin, Rosen.
Administrative, technical, or material support: Wohl, White.
Study supervision: Wohl, Golin, White.
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Wohl reported serving as a consultant to Janssen and Gilead; and receiving grant funding from Merck, GlaxoSmithKline, Gilead, and ViiV. Dr White reported receiving payment for lectures from Gilead Sciences. No other disclosures were reported.
Contributor Information
David Alain Wohl, University of North Carolina, Chapel Hill.
Carol Golin, Sheps Center for Health Services Research, University of North Carolina, Chapel Hill.
David L. Rosen, Center for Infectious Diseases, University of North Carolina, Chapel Hill.
Jeanine M. May, Sheps Center for Health Services Research, University of North Carolina, Chapel Hill.
Becky L. White, Sheps Center for Health Services Research, University of North Carolina, Chapel Hill.
References
- 1.Maruschak LM, Beavers R. HIV in prisons, 2007–08. [Accessibility verified October 31, 2013]; http://bjs.ojp.usdoj.gov/content/pub/pdf/hivp08.pdf.
- 2.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altice FL, Mostashari F, Selwyn PA, et al. Predictors of HIV infection among newly sentenced male prisoners. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18(5):444–453. doi: 10.1097/00042560-199808150-00005. [DOI] [PubMed] [Google Scholar]
- 4.Braithwaite RL, Arriola KR. Male prisoners and HIV prevention: a call for action ignored. Am J Public Health. 2003;93(5):759–763. doi: 10.2105/ajph.93.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Branson BM, Handsfield HH, Lampe MA, et al. Centers for Disease Control and Prevention (CDC) Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 6.North Carolina Department of Health and Human Services Communicable Disease Branch. 2008 HIV/STD surveillance report. [Accessed January 30, 2013]; http://epi.publichealth.nc.gov/cd/stds/figures/std08rpt.pdf.