Abstract
Background
There are few studies about risk factors for poor outcomes from multi-level lumbar posterolateral fusion limited to three or four level lumbar posterolateral fusions. The purpose of this study was to analyze the outcomes of multi-level lumbar posterolateral fusion and to search for possible risk factors for poor surgical outcomes.
Methods
We retrospectively analyzed 37 consecutive patients who underwent multi-level lumbar or lumbosacral posterolateral fusion with posterior instrumentation. The outcomes were deemed either 'good' or 'bad' based on clinical and radiological results. Many demographic and radiological factors were analyzed to examine potential risk factors for poor outcomes. Student t-test, Fisher exact test, and the chi-square test were used based on the nature of the variables. Multiple logistic regression analysis was used to exclude confounding factors.
Results
Twenty cases showed a good outcome (group A, 54.1%) and 17 cases showed a bad outcome (group B, 45.9%). The overall fusion rate was 70.3%. The revision procedures (group A: 1/20, 5.0%; group B: 4/17, 23.5%), proximal fusion to L2 (group A: 5/20, 25.0%; group B: 10/17, 58.8%), and severity of stenosis (group A: 12/19, 63.3%; group B: 3/11, 27.3%) were adopted as possible related factors to the outcome in univariate analysis. Multiple logistic regression analysis revealed that only the proximal fusion level (superior instrumented vertebra, SIV) was a significant risk factor. The cases in which SIV was L2 showed inferior outcomes than those in which SIV was L3. The odds ratio was 6.562 (95% confidence interval, 1.259 to 34.203).
Conclusions
The overall outcome of multi-level lumbar or lumbosacral posterolateral fusion was not as high as we had hoped it would be. Whether the SIV was L2 or L3 was the only significant risk factor identified for poor outcomes in multi-level lumbar or lumbosacral posterolateral fusion in the current study. Thus, the authors recommend that proximal fusion levels be carefully determined when multi-level lumbar fusions are considered.
Keywords: Lumbar vertebrae, Spinal stenosis, Spinal fusion, Risk factors
Multi-level spinal stenosis is a commonly encountered disease in clinical situations. Posterolateral fusions (PLF) after wide decompression for multi-level spinal stenosis are also commonly performed for treatment. PLFs are a well-established method for treatment, due to their usefulness and demerits. Many studies have researched fusion rates, functional outcomes, and adjacent segment degeneration, which is a main problems of fusion surgeries.1,2,3,4) The fusion rate of PLF is known to decrease as the number of fusion levels increases.5) It has also been reported that the fusion rate of PLF is lower than that of posterior lumbar interbody fusion.6,7) However, functional outcomes of the procedure have been reported to be good, though relatively lower fusion rates were found in the case of short level fusions.2,4,7,8,9) Although the studies about risk factors for poor outcomes in one or two level PLFs have been widely researched, the studies which were limited to three or four level lumbar or lumbosacral PLFs are relatively rare. The authors have encountered poor outcomes including adjacent segment degeneration by proximal fusion level from three or four level lumbar or lumbosacral PLF. We hypothesized that the level of proximal fusion would be a meaningful risk factor for poor outcomes of multi-level lumbar PLF empirically. The purpose of this study was to analyze surgical outcomes of three or four level lumbar or lumbosacral PLF for multi-level spinal stenosis and to determine risk factors for poor outcomes.
METHODS
This study was a retrospective case series and was approved by Institutional Review Board of Kangwon Natioanl University Hospital. The eligible cases were the patients who underwent posterior decompression and three or four level lumbar or lumbosacral PLFs with wide decompression for 3 or 4 level spinal stenosis with or without spondylolisthesis or scoliosis between January 1, 2004 and February 29, 2012 at Kangwon Natioanl University Hospital. The cases which showed a grade two or more spondylolisthesis or over 20° of degenerative scoliosis were excluded. The cases of infection, tumor, trauma, and the cases with follow-up periods less than 1 year were also excluded. Ultimately, 37 cases were included in the current study.
The demographic data including age, gender, history of prior surgery, follow-up period, patient's symptoms and complications were assessed by medical chart reviews. The bone mineral density scores were assessed in L1-4 lumbar spines by using dual energy X-ray absorptiometry (DEXA, Lunar Prodigy Advance, GE Healthcare, Pollards Wood, UK). The measurements of radiographic data were performed by using a picture archiving communication system (PACS, PiViewStar, INFINITT Co., Seoul, Korea).
The PLF was done between decorticated transverse processes with mixtures of local bones and 10 mL per level of synthetic hydroxyapatite (Bongros HA, Bioalpha, Seongnam, Korea) in a routine manner. Posterior instrumentation with pedicle screws (GSS Pedicle Screw System, GS Medical, Soquel, CA, US; LnK Spinal Fixation System, L&K Biomed, Seoul, Korea) was done in all fusion levels.
Plain Radiography Protocol
The radiographic data were obtained from lumbar spine anteroposterior (AP) and lateral neutral views in upright standing positions with arms folded. Routine check-ups were scheduled during the preoperative period and included postoperative 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and annually after the 1-year follow-up. The data about spondylolisthesis, lumbar lordosis, disc heights, and segmental angles of just above level of superior instrumented vertebra (SIV) were acquired on lumbar lateral views and those about scoliosis over 10° and horizontal tilts of SIV were acquired on lumbar AP views.
Lumbar lordosis was derived by the Cobb's angle between upper endplate of L1 and that of S1 in lateral views. The disc heights and segmental angles of just above level of SIV were derived by the distances and Cobb's angles between upper and lower margin of disc space, respectively. Horizontal tilts of SIV were derived by Cobb's angles between upper endplates of SIV and the lines linking top of both iliac crest. The measurement methods are demonstrated in Fig. 1. The bone fusion status was assessed by the radiographic fusion grades by Lenke et al.10) at postoperative 1-year follow-up. Lenke grades A and B were judged as unions; grades C and D were judged as nonunions.
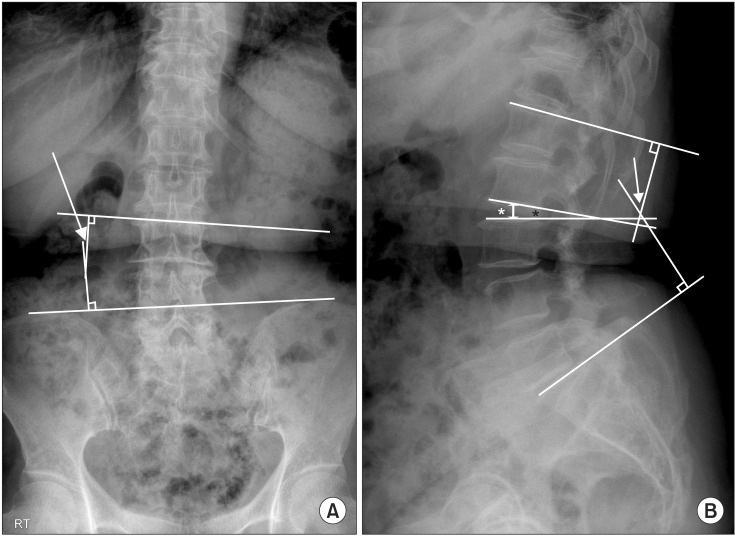
Fig. 1.
Measurements of radiological parameters. (A) The horizontal tilt was measured as the angle between the upper end plates of the superior instrumented vertebra (SIV) and the lines linking the top of both iliac crests on the lumbar standing anteroposterior radiograph (arrow). (B) Lumbar lordosis was measured as the angle between the superior endplates of L1 and S1 (arrow). The disc height and segmental angle directly above the level of SIV are illustrated as a white asterisk and a black asterisk, respectively.
Magnetic Resonance Imaging Protocol
The magnetic resonance images (MRI) were obtained preoperatively by a 1.5T scanner (Intera Achieva, Philips, Amsterdam, The Netherlands). The degrees of spinal stenosis, the degrees of lumbar back muscle degeneration and the degrees of disc degeneration in just above level of SIV were assessed. The degrees of spinal stenosis were assessed in the most severely compressed level by Schizas' method.11) They were categorized as 'mild' in case of Schizas grade A or B, and as 'severe' in case of Schizas grade C or D. The lumbar back muscle degenerations were assessed in L3-4 disc level qualitatively.12) They were categorized as 'mild' and 'moderate to severe.' The degrees of disc degeneration at the level just above the SIV were assessed by the Pfirrmann grade.13) They were categorized as 'mild' in cases of Pfirrmann grade I, II or III and as 'severe' in case of grades IV or V.
Outcome Measurements and Statistical Analysis
The data acquisition was done by two spine surgeons in the same department who did not participate in surgeries. The means were adopted as data for analysis in case of continuous variables and agreements between two surgeons were adopted in case of categorical variables.
Clinical outcomes were assessed by numeric rating scales (NRS) preoperatively and in every routine postoperative visit. The NRS were obtained about low back pain and radiating pain separately.
Surgical outcomes were categorized as the 'good' or the 'bad' based on changes of NRS and radiological assessment. The category 'good' included the cases which satisfied the following criteria: (1) the patients who showed improved symptoms which were defined as 3 or more decrease of NRS about radiating pain postoperatively and maintained that level for at least 1 year without recurrence of symptoms; and (2) the changes of radiographic findings were minimal between immediate postoperative period and final visits. The category 'bad' included the cases which satisfied the following criteria: (1) the patients who showed persistent or relapsed symptoms within postoperative 1 year; and (2) the changes of radiographic findings were definite and concordant with symptoms. The decision of the outcome category was determined by two reviewers independently. If the case did not reach a consensus, then the Delphi method was used.
The data were analyzed by a statistical software PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA). Student t-test, Fisher exact test, and a chi-square test were used by nature of variables to search possible factors which showed the differences according to surgical outcome category. A paired t-test was used to assess changes of NRS between each follow-up period. Factors associated with surgical outcomes with p-value of less than 0.20 in univariate analysis were analyzed with multiple logistic regression analysis to exclude confounding factors. Statistical significance in multivariate analysis was defined as a p-value of less than 0.05.
RESULTS
Demographic Data
Ten male and 27 female patients were analyzed and their mean age was 65.6 ± 7.4 years old. Spondylolisthesis existed in 13 patients (35.1%) and scoliosis over 10° existed in 17 of 37 patients (45.9%). The mean bone marrow density of 37 patients was -1.29 ± 1.17. The average follow-up period was 29.7 months (range, 12 to 102 months). There were 32 primary cases and 5 revision cases. The revision cases were 2 open discectomies and 3 fusion surgeries. The levels of operation were 8 cases of L2-3-4-5, 7 cases of L2-3-4-5-S1, and 22 cases of L3-4-5-S1. None of the cases included an L1 fusion level.
Surgical Outcomes
Good outcomes were shown in 20 patients (54.1%) and bad outcomes were shown in 17 patients (45.9%). Both low back pain and radiating pain showed significant improvement within postoperative 3 months in the 'good' group. On the contrary, this improvement in the 'bad' group was not as dramatic as in a 'good' group. The mean NRS regarding low back pain and radiating pain in each period are described in Fig. 2. The overall fusion rate was 70.3% (26/37). Thirteen cases were Lenke grade A (35.1%), 13 cases were grade B (35.1%), 7 cases were grade C (18.9%), and 4 cases were grade D (10.8%). There were 2 postoperative infections (2/37, 5.4%). The one was immediate postoperative superficial infection, which was controlled by debridement and antibiotic treatment. The other was infectious spondylitis at L5-S1 disc level, which was found at the 20-month postoperative appointment. This case was controlled by additional anterior lumbar interbody fusion. Five patients underwent revision operations for poor clinical and radiological outcomes during their follow-up periods (5/37, 13.5%). The clinical backgrounds and courses of 5 revision cases are described in Table 1 and one example case is described in Fig. 3.
Fig. 2.
Comparisons of numeric rating scales (NRS) between 'good' group and 'bad' group in each period. (A) The NRS regarding radiating pain. (B) The NRS regarding low back pain. Preop: preoperative, PO: postoperative.
Table 1.
The Clinical Backgrounds and Courses of Patients Who Underwent Revision Surgeries during the Follow-up Periods

No.: case number, BMD: bone marrow density, Op.: operation, SIV: superior instrumented vertebra, ASP: adjacent segment pathology, PLF: posterolateral fusion, ALIF: anterior lumbar interbody fusion.
*The fusion status was checked by using Lenke classification at postoperative 1 year follow-up. However, radiographs of final follow-up before revision surgery were used for case number 35.
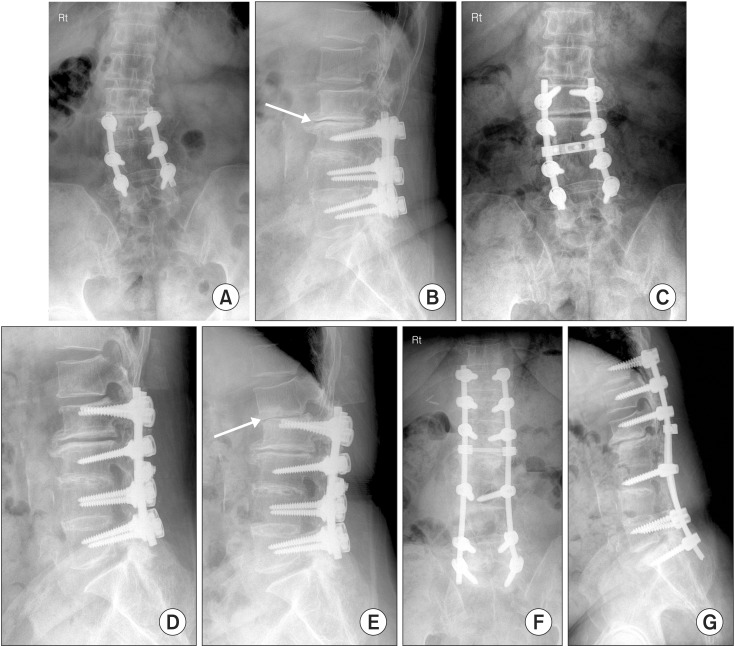
Fig. 3.
A 70-year-old female patient who suffered from severe back pain and radiating pain after lumbar posterolateral fusion from L3 to L5 level at another hospital. Preoperative anteroposterior (A) and lateral (B) radiographs showed disc space narrowing (arrow) just above the level of superior instrumented vertebra. Postoperative anteroposterior (C) and lateral (D) radiographs. (E) The lateral radiograph at 9 months postoperative revealed progression of disc space narrowing at the L1-2 level (arrow). (F,G) Revision operation was performed to relieve severe back pain and radiating pain.
Factors Associated with Surgical Outcomes of Multi-Level Lumbar PLF
The age, sex, follow-up periods, and preoperative radiological parameters including lumbar lordosis, disc heights, disc wedge angles, horizontal tilts were not different between the 'good' group and the 'bad' group. The degree of back muscle degenerations and disc degenerations in MRIs were also not different between groups. Only 3 possible associated factors for poor outcomes were found by univariate analysis. The proportion of prior surgery in the 'bad' group (4/17, 23.5%) was higher than that in the 'good' group (1/20, 5.0%). The SIVs were also different between both groups. Ten of 17 'bad' group patients underwent proximal fusion to L2 (58.8%), while 5 of the 20 'good' group patients underwent proximal fusion to L2 (5/20, 25.0%). The degrees of spinal stenosis also proved to be a possible factor. Three of 11 'bad' group patients showed severe stenosis (27%), while 12 of 19 'good' group patients showed severe stenosis (63%). However, the fusion status at the 1-year follow-up did not relate to the surgical outcomes (p = 0.495). The overall results of univariate analysis are summarized in Table 2.
Table 2.
The Differences between the Good Group and the Bad Group and Results of Univariate Analysis to Search for Factors Associated with Surgical Outcomes of Multi-Level Lumbar Posterolateral Fusions

Values are presented as mean ± standard deviation or number (%).
*p-values were obtained by a Student t-test (continuous variables), a chisquare test, and Fisher exact test (categorical variables). †Negative value means lordotic.
The above-mentioned three factors were entered in multivariate analysis. After adjustment, the SIV was the only factor related to surgical outcomes in the current study. The odds ratio was 6.562 (95% confidence interval, 1.259 to 34.203).
DISCUSSION
The current study showed relatively bad outcomes of three or four level lumbar or lumbosacral PLFs. The proximal fusion level (SIV) was shown to be related to surgical outcomes, as expected. Although the revision procedures and severity of stenosis did not show statistical significance in the multivariate model, they might be important factors, if the number of cases were sufficient. However, the fusion status did not have any relation with outcome, as many other studies had proposed.
Many studies have researched the ideal proximal fusion level in multi-level lumbar or thoracolumbar fusions.14,15,16,17,18) One study did not find a difference in adjacent segment degenerations from T10 to T12 as a proximal fusion level in degenerative scoliosis.14) Another study proposed that there were no differences in proximal junctional kyphosis or revision rates when proximal fusion levels were chosen as T9, T11, and L1, respectively.14) However, other researchers have reached a different conclusion. Upper instrumented vertebra of L1 or L2 showed higher rates of failure than that of T10, T11, or T12 in 4 level minimum fusions.18) However, these studies focused on adult lumbar deformity instrumented fusions. Clinically, three or four level lumbar or lumbosacral instrumented fusions have been performed in numerous cases without such deformities. The reasons of the high failure rate in the SIV of L2 in current study was thought to be because the disc space between L1 and L2 is in the transitional zone from kyphosis to lordosis, so mechanical stress may be locally concentrated. In addition, because the L3 vertebra is the apex of lumbar lordosis, the anteroposterior translational force to disc space would be higher in the L1-2 disc space than in the L2-3 disc space. This translational force could influence the acceleration of disc degeneration, such as in retrolisthesis. This theory is described in Fig. 4. For the same reason, if SIV is L1, the outcomes might not be as good as in cases of L3, although this is not supported by the current study.
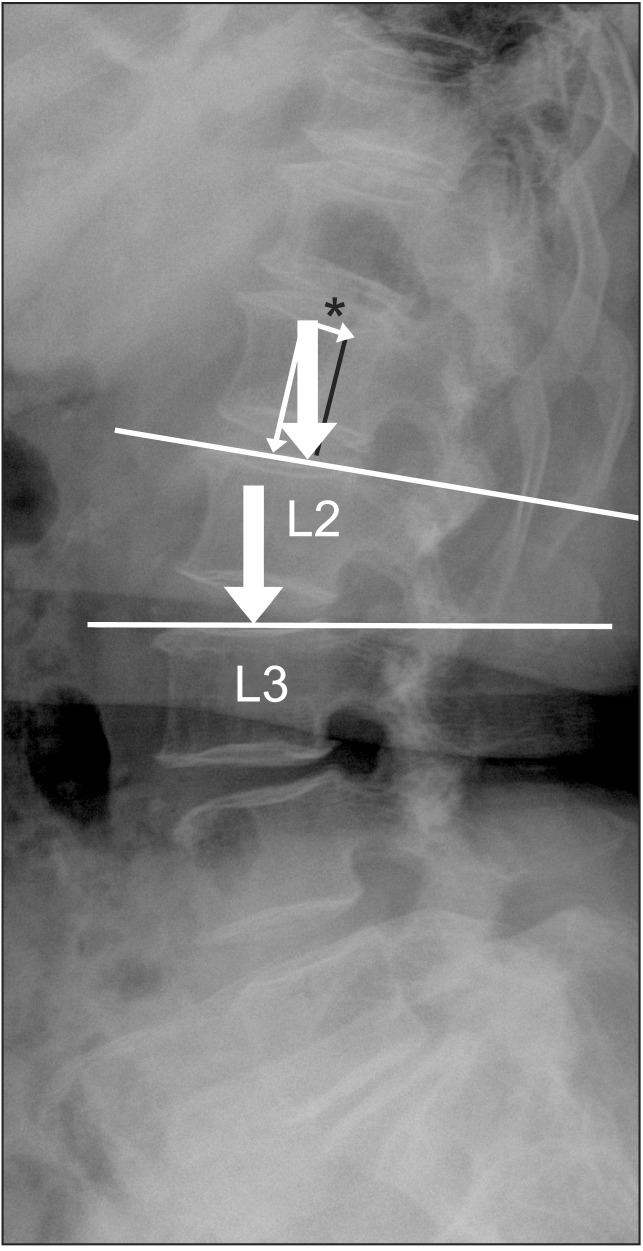
Fig. 4.
Comparison of the direction of vertical forces by weight between the cases where superior instrumented vertebra (SIV) is L2 and L3. If SIV is L3, the translational force will be minimal because the upper end plates of L3 are nearly parallel to the ground in standing positions. If SIV is L2, the translational force (*) will be increased because the vector of the vertical force is divided by the vector which is perpendicular and parallel to the upper end plates of L2 by lumbar lordosis (arrow means gravity force to each disc level).
The revision procedure itself can be a possible risk factor for bad outcomes. Many clinical studies have shown the trend of inferior outcomes with revision surgeries. The visual analog scale and Oswestry Disability Index (ODI) have both shown lower outcomes in revision lumbar surgeries.15,17) In another study, social functioning including activities of daily living or anxiety/depression showed inferior outcomes though fusion rates were similar in one or two level lumbar fusion surgeries.19) The infection risk was also increased in revision surgeries.20)
Age is another controversial factor. Many studies did not find a relationship between age and surgical outcomes. However, the protective effect of the aging process on the development of adjacent segment degeneration has also proposed.21)
Although many authors have studied the relationship between various factors and the clinical or radiological outcomes in lumbar fusion surgeries, localized studies in three or four level lumbar fusions are relatively rare. In addition, they have mainly concentrated on adjacent segment degeneration, which was considered as one factor for poor outcomes. However, surgical outcomes could not be determined by only one factor. That is the reason why we considered both the clinical and radiological aspects in our evaluatation of surgical outcomes.
There are some limitations to the current study. Firstly, this study was retrospective, so some MRI data could not be obtained because computed tomography (CT) was performed instead. The power of the test was weakened by the reason above as well as the relatively small sample size. Secondly, the assessment method for fusion rates was another limitation. The assessment of fusion rates could be stronger with CT scans. Thirdly, specific clinical outcome assessment tools such as the ODI or the Short-Form 36 Questionnaire were not used.
In conclusion, overall surgical outcomes of multilevel PLF were not as good as expected in our study. Although many limitations, including small sample size and insufficient clinical data, existed, several possible risk factors were found. Whether the proximal fusion level was L2 or L3 was revealed to be an important risk factor for poor outcomes. Thus, the authors recommend that proximal fusion levels are carefully determined when multi-level lumbar fusions are considered.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Aiki H, Ohwada O, Kobayashi H, et al. Adjacent segment stenosis after lumbar fusion requiring second operation. J Orthop Sci. 2005;10(5):490–495. doi: 10.1007/s00776-005-0919-3. [DOI] [PubMed] [Google Scholar]
- 2.Ekman P, Moller H, Hedlund R. The long-term effect of posterolateral fusion in adult isthmic spondylolisthesis: a randomized controlled study. Spine J. 2005;5(1):36–44. doi: 10.1016/j.spinee.2004.05.249. [DOI] [PubMed] [Google Scholar]
- 3.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 2004;29(17):1938–1944. doi: 10.1097/01.brs.0000137069.88904.03. [DOI] [PubMed] [Google Scholar]
- 4.Turunen V, Nyyssonen T, Miettinen H, et al. Lumbar instrumented posterolateral fusion in spondylolisthetic and failed back patients: a long-term follow-up study spanning 11-13 years. Eur Spine J. 2012;21(11):2140–2148. doi: 10.1007/s00586-012-2320-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Inage K, Ohtori S, Koshi T, et al. One, two-, and three-level instrumented posterolateral fusion of the lumbar spine with a local bone graft: a prospective study with a 2-year follow-up. Spine (Phila Pa 1976) 2011;36(17):1392–1396. doi: 10.1097/BRS.0b013e3181f40e69. [DOI] [PubMed] [Google Scholar]
- 6.Dehoux E, Fourati E, Madi K, Reddy B, Segal P. Posterolateral versus interbody fusion in isthmic spondylolisthesis: functional results in 52 cases with a minimum follow-up of 6 years. Acta Orthop Belg. 2004;70(6):578–582. [PubMed] [Google Scholar]
- 7.Madan S, Boeree NR. Outcome of posterior lumbar interbody fusion versus posterolateral fusion for spondylolytic spondylolisthesis. Spine (Phila Pa 1976) 2002;27(14):1536–1542. doi: 10.1097/00007632-200207150-00011. [DOI] [PubMed] [Google Scholar]
- 8.Farrokhi MR, Rahmanian A, Masoudi MS. Posterolateral versus posterior interbody fusion in isthmic spondylolisthesis. J Neurotrauma. 2012;29(8):1567–1573. doi: 10.1089/neu.2011.2167. [DOI] [PubMed] [Google Scholar]
- 9.Gehrchen PM, Dahl B, Katonis P, Blyme P, Tondevold E, Kiaer T. No difference in clinical outcome after posterolateral lumbar fusion between patients with isthmic spondylolisthesis and those with degenerative disc disease using pedicle screw instrumentation: a comparative study of 112 patients with 4 years of follow-up. Eur Spine J. 2002;11(5):423–427. doi: 10.1007/s00586-002-0401-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lenke LG, Bridwell KH, Bullis D, Betz RR, Baldus C, Schoenecker PL. Results of in situ fusion for isthmic spondylolisthesis. J Spinal Disord. 1992;5(4):433–442. doi: 10.1097/00002517-199212000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Schizas C, Theumann N, Burn A, et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976) 2010;35(21):1919–1924. doi: 10.1097/BRS.0b013e3181d359bd. [DOI] [PubMed] [Google Scholar]
- 12.Lee CS, Hwang CJ, Lee SW, et al. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J. 2009;18(11):1637–1643. doi: 10.1007/s00586-009-1060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001;26(17):1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Cho KJ, Suk SI, Park SR, Kim JH, Jung JH. Selection of proximal fusion level for adult degenerative lumbar scoliosis. Eur Spine J. 2013;22(2):394–401. doi: 10.1007/s00586-012-2527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geisler FH, Guyer RD, Blumenthal SL, et al. Patient selection for lumbar arthroplasty and arthrodesis: the effect of revision surgery in a controlled, multicenter, randomized study. J Neurosurg Spine. 2008;8(1):13–16. doi: 10.3171/SPI-08/01/013. [DOI] [PubMed] [Google Scholar]
- 16.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Kim YW. Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine (Phila Pa 1976) 2007;32(24):2653–2661. doi: 10.1097/BRS.0b013e31815a5a9d. [DOI] [PubMed] [Google Scholar]
- 17.Lee JC, Kim MS, Shin BJ. An analysis of the prognostic factors affecing the clinical outcomes of conventional lumbar open discectomy: clinical and radiological prognostic factors. Asian Spine J. 2010;4(1):23–31. doi: 10.4184/asj.2010.4.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis SJ, Abbas H, Chua S, et al. Upper instrumented vertebral fractures in long lumbar fusions: what are the associated risk factors? Spine (Phila Pa 1976) 2012;37(16):1407–1414. doi: 10.1097/BRS.0b013e31824fffb9. [DOI] [PubMed] [Google Scholar]
- 19.Christensen FB, Thomsen K, Eiskjaer SP, Gelinick J, Bunger CE. Functional outcome after posterolateral spinal fusion using pedicle screws: comparison between primary and salvage procedure. Eur Spine J. 1998;7(4):321–327. doi: 10.1007/s005860050082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kurtz SM, Lau E, Ong KL, et al. Infection risk for primary and revision instrumented lumbar spine fusion in the Medicare population. J Neurosurg Spine. 2012;17(4):342–347. doi: 10.3171/2012.7.SPINE12203. [DOI] [PubMed] [Google Scholar]
- 21.Min JH, Jang JS, Jung BJ, et al. The clinical characteristics and risk factors for the adjacent segment degeneration in instrumented lumbar fusion. J Spinal Disord Tech. 2008;21(5):305–309. doi: 10.1097/BSD.0b013e318142b960. [DOI] [PubMed] [Google Scholar]