Abstract
Background
The locking plates are often used for internal fixation of closed tibial fractures. The use of a locking plate as an external fixator is still controversial, particularly for closed fractures. The purpose of this study is to evaluate the results of external fixation using the femoral less invasive stabilization system (LISS) plate in proximal metaphyseal fractures of the tibia.
Methods
We prospectively evaluated 35 patients (26 males and 9 females) with a mean age of 42 years (range, 21 to 62 years) who presented with fresh tibial proximal metaphyseal fractures. According to the AO Foundation and Orthopaedic Trauma Association (AO/OTA) classification, the fractures were identified as type 41-A2 in 18 cases and type 41-A3 in 17 cases, including 25 closed fractures and 10 open fractures. The femoral LISS plate was used to fix these fractures, which was placed on the anteromedial aspect of the tibia as an external fixator. The mean follow-up period was 18 months (range, 13 to 22 months).
Results
All fractures healed in a mean time of 14 weeks (range, 10 to 20 weeks). There was no case of nonunion, deep infection, and loosening of screws and plates. One month after the appearance of cortical bridging on biplanar radiographs, the locking plate was removed within 3 minutes in the clinic without any difficulty. According to the Hospital for Special Surgery (HSS) knee scoring system and American Orthopaedic Foot & Ankle Society (AOFAS) ankle scoring system, the mean HSS score was 91 (range, 85 to 100) and 98 (range, 93 to 100), and the mean AOFAS score was 94 (range, 90 to 100) and 98 (range, 95 to 100) at 4 weeks postoperatively and final follow-up, respectively.
Conclusions
For proximal metaphyseal fracture of the tibia, external fixation using the femoral LISS plate is a safe and reliable technique with minimal complications and excellent outcomes. Its advantages include ease of performing the surgery, use of a less invasive technique, and convenience of plate removal after fracture healing.
Keywords: Tibia, Fracture, Surgery, External fixation, Locking plate
The traditional surgical treatment of proximal tibial metaphyseal fracture includes internal fixation with a plate or intramedullary nailing. Open reduction and internal fixation with a plate often requires extensive soft-tissue dissection which can increase the risk of nonunion and infection.1,2) Minimally invasive percutaneous plate osteosynthesis reduces these risks; however, complications such as infection and malalignment are not rare.3,4,5,6) Intramedullary nailing can provide rigid stability in tibial diaphyseal fractures. However, in tibial metaphyseal fracture with an hourglass shape of the intramedullary canal, nailing is a technically challenging procedure, which has a specific risk of malalignment and anterior knee pain.7,8,9)
External plate fixation is an old technique which is often used in the treatment of open tibial fractures. However, none of the papers have reported the results of external plate fixation in a large series, particularly for both closed and open fractures. The purpose of this study was to evaluate the results of external fixation using the femoral less invasive stabilization system (LISS) plate in both closed and open proximal metaphyseal fractures of the tibia.
METHODS
Patients
The study was approved by our Institutional Review Board and informed consent was given by the patients. Inclusion criteria were skeletal maturity, an isolated fracture involving the proximal one-third of the tibia. Pathological fractures, Gustilo type IIIB, type IIIC open fractures,10) tibial fractures accompanied by a soft tissue defect on the anteromedial aspect of the tibia, multiple fractures with spinal injury, and lower limbs with a pre-existing neurological deficit or vascular disease were excluded from this study.
Between July 2011 and September 2012, 35 patients with an isolated tibial proximal metaphyseal fracture underwent external fixation at our institute. There were 26 men and 9 women with a mean age of 42 years (range, 21 to 62 years). Thirteen patients sustained a fracture as a result of a fall, 7 patients sustained a fracture in a motor vehicle accident, and 15 patients sustained a fracture in an automobile-pedestrian accident. The fractures were classified according to the AO Foundation and Orthopaedic Trauma Association (AO/OTA) guidelines: type 41-A2 in 18 cases and type 41-A3 in 17 cases. There were 10 open fractur11)es, including 3 Gustilo type I, 4 Gustilo type II, and 3 Gustilo type IIIA fractures. Two patients were diabetic, and it was controlled before surgery.
The mean time between injury and operation was 3 days (range, 2 to 7 days) in closed fractures. For open fractures, external plating was performed after debridement during the emergency operation.
Surgical Technique
Three surgeons who had 15 years of experience in orthopaedic surgery performed the operations. The patient was placed supine on the operating table. Under general or spinal anesthesia, the affected lower limb was prepared and draped in a standard sterile fashion. No tourniquet was used. The femoral LISS plates were provided by many companies, such as Synthes (Oberdorf, Switzerland), Smith & Nephew (Memphis, TN, USA), DePuy (Warsaw, IN, USA), Zimmer (Warsaw, IN, USA), and Kanghui (Changzhou, China). The shape of all femoral LISS plates was similar.
The ipsilateral femoral LISS plate was used, i.e., the right femoral LISS plate was used to fix the right proximal tibial fracture and the left femoral LISS plate was used to fix the left proximal tibial fracture. The broad end of the plate was placed close to the knee joint since it can allow insertion of more screws for stabilization of the short proximal segment.
For closed oblique and spiral fractures, a small incision (3 to 5 cm) was made to expose and clean the fracture gap. The fracture was anatomically reduced. A clamp or two K-wires were used to temporarily fix and maintain the anatomic reduction. Definitive external fixation was achieved with a femoral LISS plate (9 or 11 holes). The plate was placed on the anteromedial aspect of the tibia as close to the skin as possible. A stack of evenly folded towels (1 to 2 cm in thickness) was placed under the plate to keep the plate away from the skin, preventing impingement between the plate and the skin. Successive holes were drilled over locking drill-guides through stab incisions where the overlying soft tissue envelope was intact. The depth of the drilled holes was gauged. Locking screws of the corresponding length were inserted. All screws were bicortical. At each end of the fracture, four to five bicortical locking screws were inserted. The position and orientation of the screws were checked with fluoroscopy.
For closed comminuted fractures, under live C-arm fluoroscopy, restoration of length and alignment was achieved by manual traction and percutaneous manipulation using Schanz pins. Two K-wires were used to percutaneously fix and maintain the reduction. The steps for placement of screws and plate were the same as those mentioned above. For open fractures, after excisional debridement, external plating was performed during the emergency operation. The steps for placement of screws and plate were the same as those mentioned above.
The patients were allowed to walk with partial weight-bearing from the second postoperative day. The screws were cleaned twice a day using Betadine. Patients were instructed to visit the clinic for examination every 4 weeks. At each follow-up, radiographs of the tibia were taken and the patients were evaluated using the Hospital for Special Surgery (HSS) knee scoring system and American Orthopaedic Foot & Ankle Society (AOFAS) ankle scoring system.12) Fracture healing was defined as the presence of cortical bridging on biplanar radiographs. Complications were defined by fixation failure, infection, and nonunion. Once cortical bridging was observed on biplanar radiographs, the patients were allowed to walk with full weight-bearing for one month before removing the plate in the clinic. The time to fracture healing and postoperative complications were observed and documented.
RESULTS
All patients were followed up for a mean period of 18 months (range, 13 to 22 months). The mean duration of surgery for closed fractures was 32 minutes (range, 20 to 65 minutes).
All fractures healed without any complications. The mean time to fracture healing was 14 weeks (range, 10 to 20 weeks). After walking with full weight-bearing for one month, the patients underwent uneventful plate removal in the clinic within 3 minutes. The pain during plate removal was assessed by visual analogue score (VAS). The average VAS score was 3.5 points (range, 1 to 5 points).
According to the HSS knee scoring system and AOFAS ankle scoring system, the mean HSS score was 91 (range, 85 to 100) and 98 (range, 93 to 100), and the mean AOFAS score was 94 (range, 90 to 100) and 98 (range, 95 to 100) at 4 weeks postoperatively and final follow-up (Table 1).
Table 1.
The Demographic Data of 35 Patients
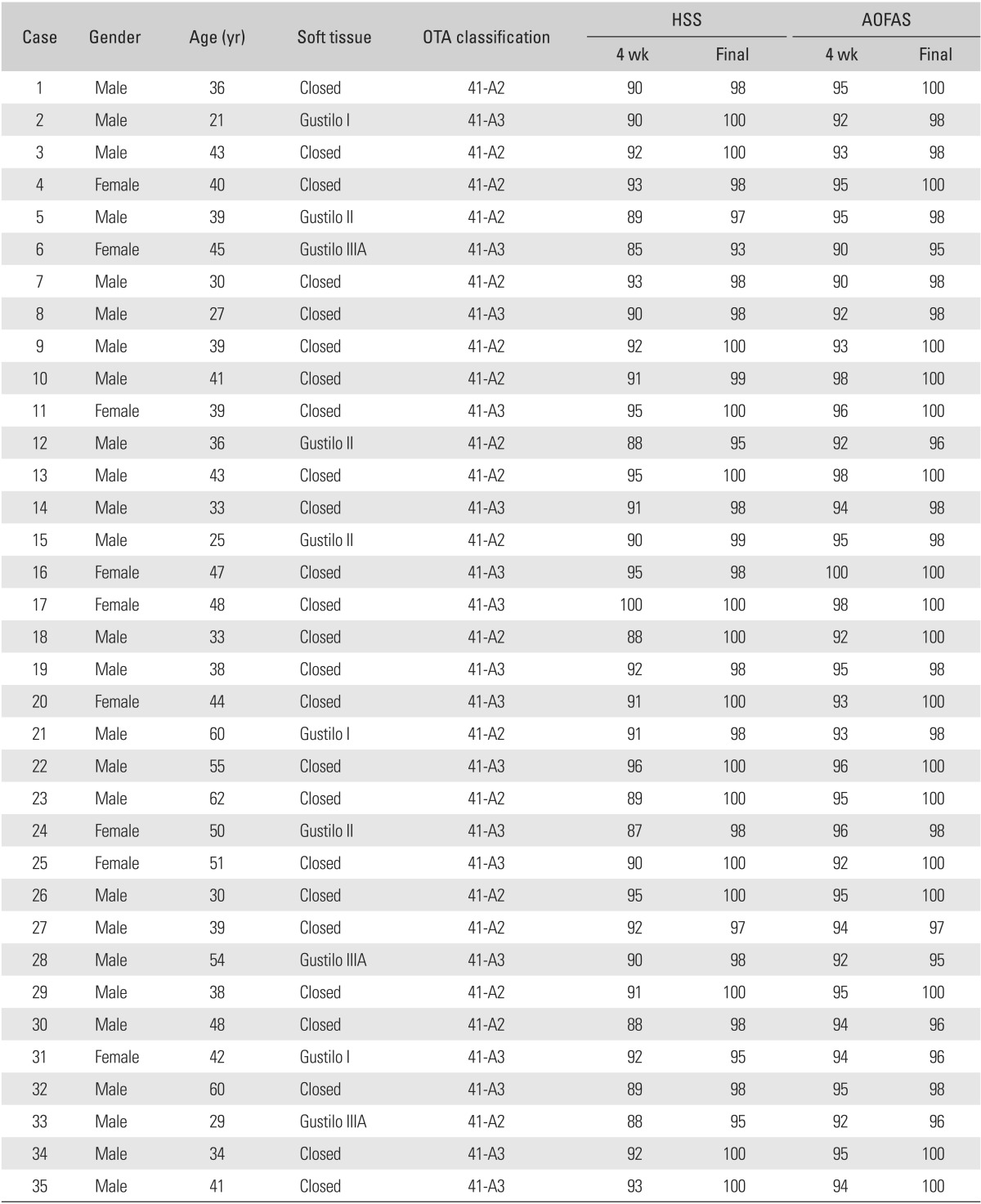
OTA: Orthopaedic Trauma Association, HSS: Hospital for Special Surgery, AOFAS: American Orthopaedic Foot & Ankle Society.
In two patients, effusion from one or two screw sites was observed. One effusion was under control with one week of daily cleaning with Betadine. The other effusion persisted even after one week of cleaning with Betadine, and the screws involved in the effusion were removed. There was no case of deep infection, malaligned union, nonunion, and loosening or breakage of plates and screws. All patients were satisfied with the outcome. The photographs of the representative cases are shown in Figs. 1, 2, 3, 4, 5.
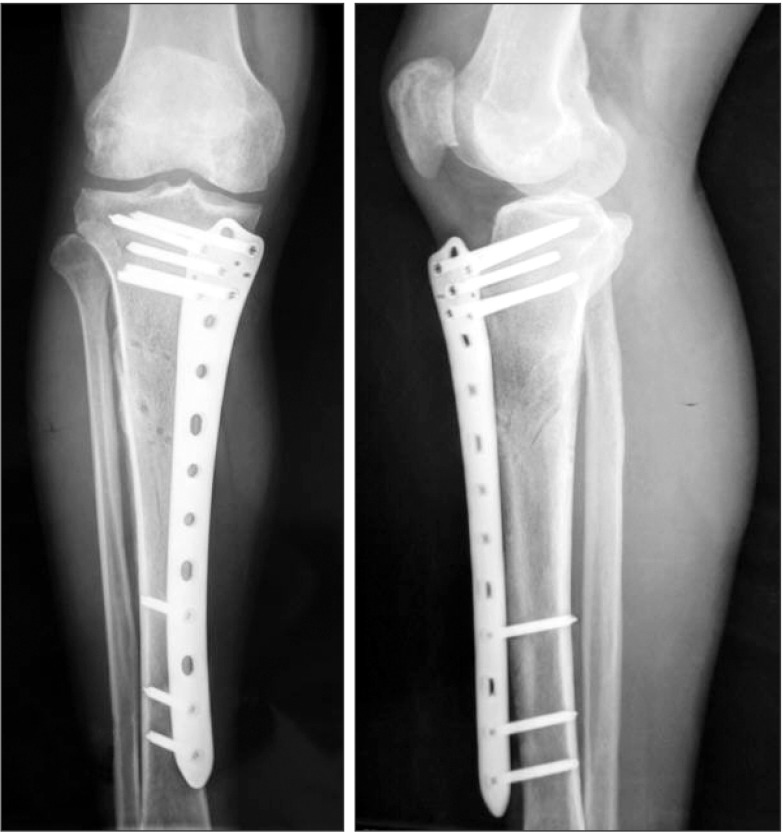
Fig. 1.
Preoperative X-ray showing the tibial proximal metaphyseal fracture.
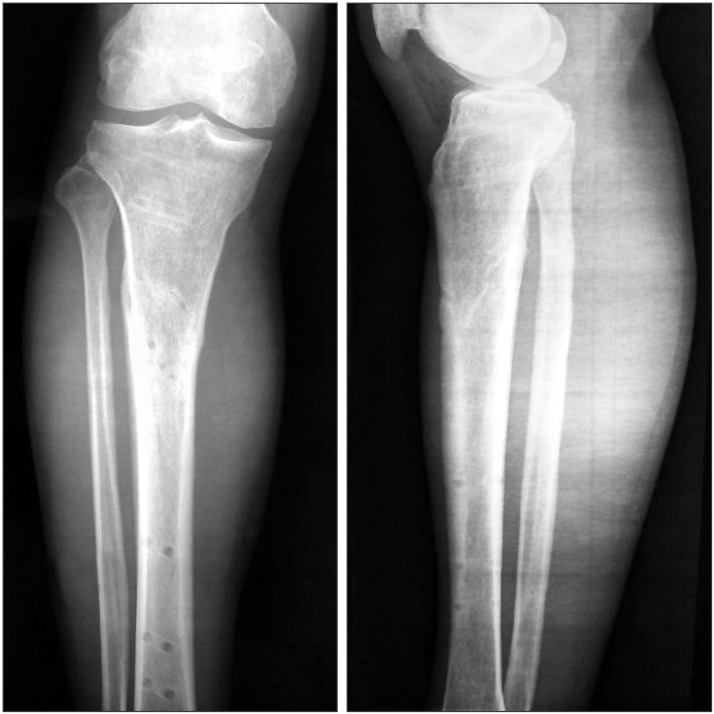
Fig. 2.
Three months postoperative X-ray showing fracture healing.
Fig. 3.

The wound and the plate in situ after the emergency operation.
Fig. 4.

(A-C) Joint with full range of motion and wound after plate removal at 3 months postoperative.
Fig. 5.
X-ray showing fracture healing at 6 months after plate removal.
DISCUSSION
The technique of external fixation using a plate is not new. The early design of an external plate such as the Zespol implant coupled with multiple nuts and washers13) may have dissuaded surgeons who may have been otherwise more receptive to this technique.14) With the advent of locking plates with fewer moving parts, this technique was used in the management of open fractures, septic arthritis, and was called the 'supercutaneous plating technique.'15,16,17) However, in most of the previously reported studies, only a small number of patients and open fractures were included, and the tibial fracture was fixed with a tibial locking plate which was thinner than the femoral LISS plate.
In our study, the femoral LISS plate was used as an external fixator to fix both closed and open proximal tibial metaphyseal fractures. The plate was placed on the anteromedial aspect of the tibia, with its broad end close to the knee joint, because we found that the contour of the femoral LISS plate matched the anteromedial aspect of the lower leg. The broad end of the femoral LISS plate offers greater versatility for inserting the screws as it has 7 holes that allow more precise modulation to obtain the greatest bone purchase in the proximal segment. In contrast to the tibial locking plate, the femoral LISS plate is thicker and the diameter of screws in the femoral LISS plate is larger than that of the screws in the tibial plate, which can increase the stability of fixation. The anteromedial aspect of the tibia is not covered by bulky muscles and important neurovascular structures, and hence, the surface can be clearly palpated; thus, facilitating fast and accurate insertion of screws with less risk of neurovascular injuries. In our study, the mean surgical duration was 32 minutes.
The plate-bone distance was 20 to 30 mm, which can increase the stability of fixation. According to the report by Stoffel et al.18) on the biomechanics of a locking plate, the axial stiffness and torsional rigidity were mainly influenced by the working length. The number of screws also significantly affected the stability. In our study, a long femoral LISS plate with 9 to 11 holes was used. All screws were bicortical. All these features can increase both the axial and torsional stability.19) All fractures healed without any complications in a mean time of 14 weeks.
The plate was placed on the anteromedial aspect of the tibia. Therefore, the motility of muscles was intact, which ensured a good range of motion. Because of its low profile, the femoral LISS plate can be easily concealed under the stockings. The patients could walk wearing normal trousers and there was much less tendency for the locking plate to strike the contralateral lower leg in the swing-through phase of either leg during ambulation.20) In our study, all of the patients were allowed to walk with partial weight-bearing from the second postoperative day. None of the patients complained of pain caused by the screws. The mean HSS score was 91 (range, 85 to 100) and 98 (range, 93 to 100), and the mean AOFAS score was 94 (range, 90 to 100) and 98 (range, 95 to 100) at 4 weeks postoperatively and final follow-up, respectively. The functional recovery of adjacent joint was satisfactory. In the other report by the authors,21) the tibial LISS plates were placed on the lateral aspect of the tibia and staged operations were performed for internal fixation. The laterally placed plate had many disadvantages. The large distance between the plate and the bone resulted in a large offset. The screws were unicortical. These factors decreased the stability of fixation. At the same time, the laterally placed screws passed through the muscles on the anterolateral aspect of the tibia which would compromise the motility of muscles and cause an uncomfortable feeling, pin-site effusion, and even neurovascular injuries.
The conventional surgical treatment for tibial fractures includes nailing and plating. It is not easy to achieve rigid stability using nailing in a metaphyseal fracture. Although some techniques have been reported to augment the fixation with nailing, such as a blocking screw,22,23) the placement of a blocking screw is not always easy and would increase the time of surgery. Another common complication of nailing is anterior knee pain, regardless of whether a transtendinous or peritendinous procedure is used.24,25) The clinical series with the use of an internal locking plate demonstrated favorable results;26,27,28) however, complications such as malunion and infection are not rare.
With external plate fixation, it is not necessary to make two incisions to create a tunnel under the skin, which can provide better protection of the blood supply, decrease the postoperative pain and risk of infection. After fracture healing, the external plate was removed easily. In our study, all of the patients underwent uneventful plate removal in the clinic within 3 minutes. The average VAS score was 3.5 (range, 1 to 5). In contrast, the operation for removal of nails and internal locking plate could be troublesome in some cases. In the report by Raja et al.29) on plate removal, the rate of complications was as high as 47%.
With respect to the rate of infections, it was reported to be approximately 1% in closed tibial shaft fractures, 5% for Gustilo type I, 10% for type II, and > 15% for type III.30) In our study, all of the 10 open fractures underwent external fixation using the femoral LISS plate during the emergency operation. None of the fractures developed infections. There were 2 cases of superficial pin-site infections which were under control. There was no case of deep infection, nonunion, and loosening or breakage of plates and screws. All of the patients were satisfied with the outcome.
Our study has several limitations, including a relatively short follow-up and lack of a control group. The use of the femoral LISS plate, which was originally designed for internal fixation of the femur, as an external fixator to fix a tibial fracture is also controversial.
In conclusion, for most proximal metaphyseal fractures of the tibia, external fixation using the femoral LISS plate is a safe and reliable technique with minimal complications and excellent outcomes. The low profile plate can be concealed under stockings and it is aesthetically acceptable. It is easy to remove the hardware after fracture healing. The traditional and classic surgical treatment of a closed tibial fracture is internal fixation. In our study, the indication for external plate fixation was expanded to include both closed and open fractures. Although the results of external plate fixation are very good, its use is still controversial. More studies are needed to definitely confirm the result of this technique.
ACKNOWLEDGEMENTS
The operations were carried out in Ningbo Sixth Hospital.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Dillin L, Slabaugh P. Delayed wound healing, infection, and nonunion following open reduction and internal fixation of tibial plafond fractures. J Trauma. 1986;26(12):1116–1119. doi: 10.1097/00005373-198612000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84(8):1093–1110. doi: 10.1302/0301-620x.84b8.13752. [DOI] [PubMed] [Google Scholar]
- 3.Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008;32(5):697–703. doi: 10.1007/s00264-007-0384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McFerran MA, Smith SW, Boulas HJ, Schwartz HS. Complications encountered in the treatment of pilon fractures. J Orthop Trauma. 1992;6(2):195–200. doi: 10.1097/00005131-199206000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Pai V, Coulter G, Pai V. Minimally invasive plate fixation of the tibia. Int Orthop. 2007;31(4):491–496. doi: 10.1007/s00264-006-0228-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wagner M. General principles for the clinical use of the LCP. Injury. 2003;34(Suppl 2):B31–B42. doi: 10.1016/j.injury.2003.09.023. [DOI] [PubMed] [Google Scholar]
- 7.Katsoulis E, Court-Brown C, Giannoudis PV. Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg Br. 2006;88(5):576–580. [Google Scholar]
- 8.Keating JF, Orfaly R, O'Brien PJ. Knee pain after tibial nailing. J Orthop Trauma. 1997;11(1):10–13. doi: 10.1097/00005131-199701000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Lefaivre KA, Guy P, Chan H, Blachut PA. Long-term follow-up of tibial shaft fractures treated with intramedullary nail ing. J Orthop Trauma. 2008;22(8):525–529. doi: 10.1097/BOT.0b013e318180e646. [DOI] [PubMed] [Google Scholar]
- 10.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58(4):453–458. [PubMed] [Google Scholar]
- 11.Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma. 1996;10(Suppl 1):v–ix. 1–154. [PubMed] [Google Scholar]
- 12.Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg. 2007;46(2):65–74. doi: 10.1053/j.jfas.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Ramotowski W, Granowski R. Zespol: an original method of stable osteosynthesis. Clin Orthop Relat Res. 1991;(272):67–75. [PubMed] [Google Scholar]
- 14.Woon CY, Wong MK, Howe TS. LCP external fixation--external application of an internal fixator: two cases and a review of the literature. J Orthop Surg Res. 2010;5(1):19. doi: 10.1186/1749-799X-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kerkhoffs GM, Kuipers MM, Marti RK, Van der Werken C. External fixation with standard AO-plates: technique, indications, and results in 31 cases. J Orthop Trauma. 2003;17(1):61–64. doi: 10.1097/00005131-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Kloen P. Supercutaneous plating: use of a locking compression plate as an external fixator. J Orthop Trauma. 2009;23(1):72–75. doi: 10.1097/BOT.0b013e31818f8de4. [DOI] [PubMed] [Google Scholar]
- 17.Marti RK, van der Werken C. The AO-plate for external fixation in 12 cases. Acta Orthop Scand. 1991;62(1):60–62. doi: 10.3109/17453679108993094. [DOI] [PubMed] [Google Scholar]
- 18.Stoffel K, Dieter U, Stachowiak G, Gachter A, Kuster MS. Biomechanical testing of the LCP: how can stability in locked internal fixators be controlled? Injury. 2003;34(Suppl 2):B11–B19. doi: 10.1016/j.injury.2003.09.021. [DOI] [PubMed] [Google Scholar]
- 19.Dougherty PJ, Kim DG, Meisterling S, Wybo C, Yeni Y. Biomechanical comparison of bicortical versus unicortical screw placement of proximal tibia locking plates: a cadaveric model. J Orthop Trauma. 2008;22(6):399–403. doi: 10.1097/BOT.0b013e318178417e. [DOI] [PubMed] [Google Scholar]
- 20.Tulner SA, Strackee SD, Kloen P. Metaphyseal locking compression plate as an external fixator for the distal tibia. Int Orthop. 2012;36(9):1923–1927. doi: 10.1007/s00264-012-1585-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma CH, Tu YK, Yeh JH, Yang SC, Wu CH. Using external and internal locking plates in a two-stage protocol for treatment of segmental tibial fractures. J Trauma. 2011;71(3):614–619. doi: 10.1097/TA.0b013e3182041175. [DOI] [PubMed] [Google Scholar]
- 22.Buehler KC, Green J, Woll TS, Duwelius PJ. A technique for intramedullary nailing of proximal third tibia fractures. J Orthop Trauma. 1997;11(3):218–223. doi: 10.1097/00005131-199704000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Ricci WM, OBoyle M, Borrelli J, Bellabarba C, Sanders R. Fractures of the proximal third of the tibial shaft treated with intramedullary nails and blocking screws. J Orthop Trauma. 2001;15(4):264–270. doi: 10.1097/00005131-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Toivanen JA, Vaisto O, Kannus P, Latvala K, Honkonen SE, Jarvinen MJ. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft: a prospective, randomized study comparing two different nail-insertion techniques. J Bone Joint Surg Am. 2002;84(4):580–585. doi: 10.2106/00004623-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Vaisto O, Toivanen J, Kannus P, Jarvinen M. Anterior knee pain and thigh muscle strength after intramedullary nailing of tibial shaft fractures: a report of 40 consecutive cases. J Orthop Trauma. 2004;18(1):18–23. doi: 10.1097/00005131-200401000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003;34(Suppl 2):B63–B76. doi: 10.1016/j.injury.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 27.Namazi H, Mozaffarian K. Awful considerations with LCP instrumentation: a new pitfall. Arch Orthop Trauma Surg. 2007;127(7):573–575. doi: 10.1007/s00402-007-0343-6. [DOI] [PubMed] [Google Scholar]
- 28.Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma. 2007;21(2):83–91. doi: 10.1097/BOT.0b013e318030df96. [DOI] [PubMed] [Google Scholar]
- 29.Raja S, Imbuldeniya AM, Garg S, Groom G. Difficulties encountered removing locked plates. Ann R Coll Surg Engl. 2012;94(7):502–505. doi: 10.1308/10.1308/003588412X13373405386411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shuler FD, Obremskey WT. Tibial shaft fractures. In: Stannard JP, Schmidt AH, Kregor PJ, editors. Surgical treatment of orthopaedic trauma. New York: Thieme; 2007. pp. 742–766. [Google Scholar]