Abstract
Patients with obstructed defecation syndrome (ODS) form an important subset of patients with chronic constipation. Evaluation and treatment of these patients has traditionally been difficult. Magnetic resonance defecography (MRD) is a very useful tool for the evaluation of these patients. We evaluated the scans and records of 192 consecutive patients who underwent MRD at our center between January 2011 and January 2012. Abnormal descent, rectoceles, rectorectal intussusceptions, enteroceles, and spastic perineum were observed in a large number of these patients, usually in various combinations. We discuss the technique, its advantages and limitations, and the normal findings and various pathologies.
Keywords: Chronic constipation, magnetic resonance defecography, obstructed defecation syndrome, pelvic floor
Introduction
Constipation has a high prevalence in the general population and is a cause for significant morbidity. It has been estimated that approximately 10% of the Indian population suffers from constipation.[1] Chronic constipation leads to approximately 2.5 million visits to the physicians in the United States annually.[2] Various definitions have been used for chronic constipation. However, recently, the Rome II criteria were developed to promote consistency in the diagnosis.[3] Constipation may be primary or secondary. Primary constipation may be due to slow transit disorder or anorectal expulsion disorder (obstructive defecation) or a combination of these. According to the National Institute for health and Clinical Excellence (NICE) guidelines issued in 2010, obstructed defecation syndrome (ODS) is characterized by the urge to defecate but an impaired ability to expel the fecal bolus. Symptoms include unsuccessful fecal evacuation attempts, excessive straining, pain, bleeding after defecation, and a sense of incomplete fecal evacuation.[4] Patients may also resort to digital rectal evacuation. Evaluation and treatment of these patients has been difficult. Magnetic resonance defecography (MRD) has been shown to demonstrate the structural abnormalities associated with ODS, and patients with significant structural abnormalities may benefit from surgical interventions like stapled transanal resection of rectum (STARR). Patients who do not demonstrate significant structural abnormalities can be referred for biofeedback techniques. We present our experience in a large series of patients with suspected ODS who underwent MRD at our tertiary care center.
Imaging Technique
Patients with suspected ODS (based on NICE guidelines 2010) are referred to our department for MRD. All patients undergo colonoscopy prior to the MRD to exclude other colonic pathologies like colon neoplasms and polyps. The MRD is performed on a 1.5 T (Signa Excite; GE Medical Systems, Milwaukee, WI, USA) MRI system having a closed (tunnel) configuration using a standardized protocol. No prior colon preparation is necessary. Since patient cooperation is essential for good quality studies, he/she is first explained the procedure in detail; all queries are answered and a written consent is obtained. Three hundred milliliters of ultrasound jelly is instilled in the patient's rectum using rectal tube in left lateral decubitus position. The patient is then made to lie down in the supine position on the MR machine gantry and imaging is performed using an 8-channel pelvic phased array coil. Initially static imaging is performed using high-resolution T2W turbo spin-echo sequences [repetition time msec (TR)/echo time msec (TE): 4500/90; matrix: 288 × 224; field of view (FOV): 24 × 24; 5 mm slice thickness ; Number of Excitations (NEX): 2, bandwidth: 31.2 kHz] in the axial and coronal planes. Dynamic imaging is then performed using a T2-weighted multiphasic 2D fast imaging employing steady-state acquisition (FIESTA) sequence (TR/TE: 4.4/2.0; matrix: 288 × 192; FOV: 32 × 32; flip angle: 45°; 150 images at 1 image every second; 8 mm slice thickness; bandwidth: 83.3 kHz; NEX: 1.0) in the midsagittal plane through the anal canal. This sequence is run for almost 2 min, while the patient performs various maneuvers as follows. He/she is first asked to squeeze the anal sphincters inward, so as to elevate the pelvic floor. Then, he/she is asked to apply short transient downward straining effort and relax immediately. Finally, the patient is asked to apply sustained downward straining effort and pass the ultrasound jelly (defecate). The dynamic scan is repeated if necessary. A study is considered to be of non-diagnostic quality if the patient is unable to effectively strain in the supine position. These patients are then considered for erect conventional defecography.
The images are evaluated on a dedicated workstation (Advantage GE workstation version 4.5) and the dynamic sequence is viewed in the cine loop mode.
Normal Defecogram
The pelvic floor is divided into three compartments: the anterior compartment (lower urinary tract), the middle compartment (vagina/uterus), and the posterior compartment (ano-rectum). The pubococcygeal line is drawn from the inferior border of the pubic symphysis to the last coccygeal articulation. The anorectal angle is formed between the posterior walls of the rectum and anal canal at the anorectal junction. At rest, the anorectal angle is acute due to the indentation of the puborectalis sling on the posterior rectal wall. During normal defecation, there is mild pelvic floor descent with relaxation of the puborectalis. Consequently, the anorectal angle becomes wider, so that the rectum and anal canal become aligned in almost a straight line followed by evacuation [Figure 1].
Figure 1(A-D).
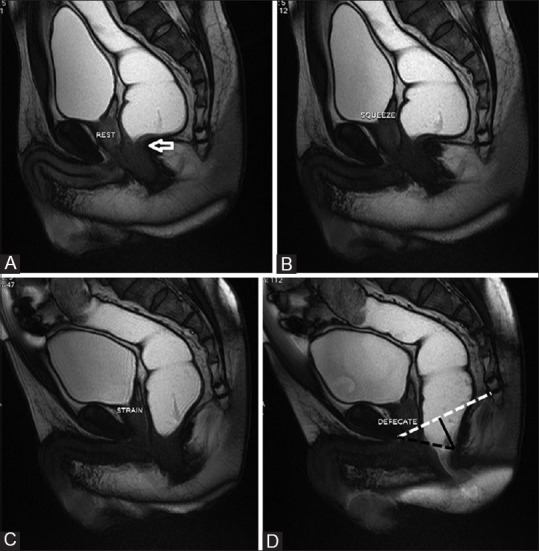
Normal MR defecogram. Normal position of the anorectal junction at rest (arrow in a) with mild pelvic floor lift on squeeze (B) On straining (C) and defecation (D) there is mild descent of the anorectal junction, with the rectum and anal canal aligned in almost a straight line. The broken white line in (D) is the pubococcygeal line. The broken black line is the “H line” corresponding to the anteroposterior dimension of the hiatus. The solid black line is the “M line” which is the perpendicular distance between the pubococcygeal line and the posterior anorectal junction
Pathologies
Various pathologies can be diagnosed and graded using established criteria [Table 1].[5] The descent of the anorectal junction, vaginal vault, bladder (cystocele), and small bowel (enterocele) can be measured as the perpendicular distance below the pubococcygeal line. Usually, multiple pathologies are found to co-exist and can sometimes create a confusing overall picture.
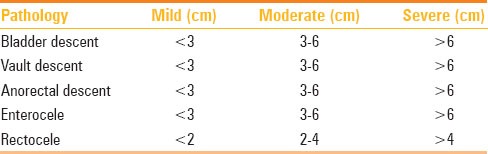
Table 1.
Grading of pathologies
Rectocele
Rectocele is defined as the protrusion of the rectal wall beyond the expected normal contour and is graded as small (<2 cm), moderate (2-4 cm), and large (>4 cm), depending on the depth of the protrusion [Figures 2 and 3]. The retention of the jelly within the rectocele at end defecation [Figure 4] is an important finding, since it is known to correlate with patient's symptoms. Rectoceles that exceed 2 cm, retain contrast media, and cause reproduction of patient's symptoms with need for evacuatory assistance (e.g. digital pressure) are considered clinically significant.[6]
Figure 2(A-D).
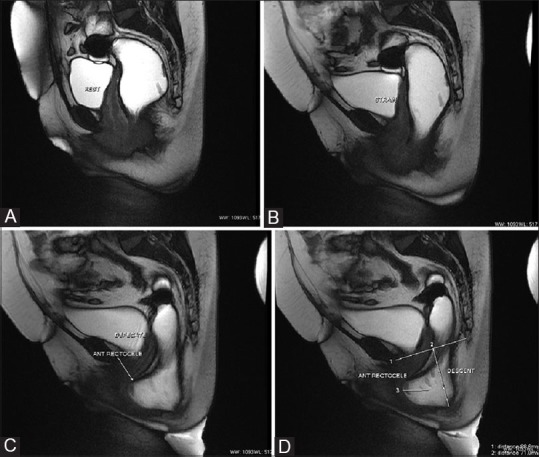
Severe descent of the anorectal junction with moderate anterior rectocele. Normal position of anorectal junction at rest (A) with normal alignment on straining (B). During defecation (C and D), there is severe descent of the anorectal junction which is located approximately 7 cm below the pubococcygeal line (line 1 in d). Also, note the moderate anterior rectocele measuring approximately 3 cm in length. The descent and the rectocele are measured as shown in (D)
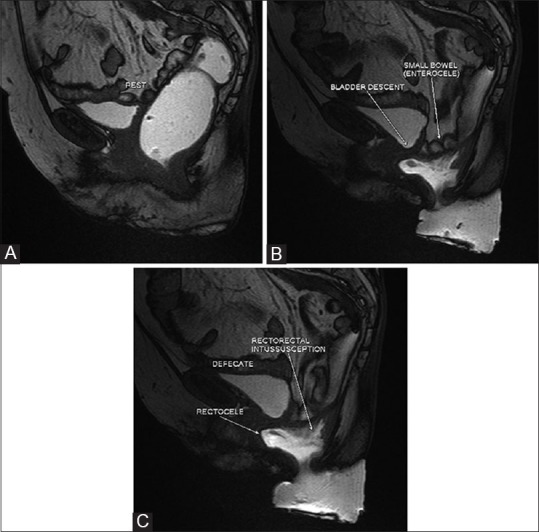
Figure 3(A-C).
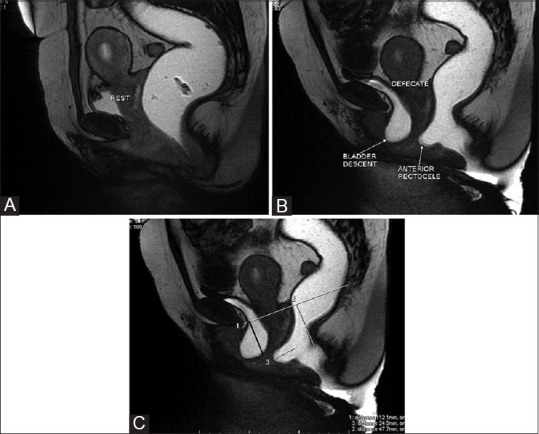
Moderate descent of anorectal junction and bladder with moderate anterior rectocele. Normal positions at rest (A) with moderate anorectal and bladder descent on defecation (B). Moderate anterior rectocele is also seen. The bladder and anorectal descents are measured as the respective perpendicular distance below the pubococcygeal line, while the rectocele is measured as the maximum depth of protrusion of the rectal wall beyond its expected normal contour as shown in (C)
Figure 4(A-D).
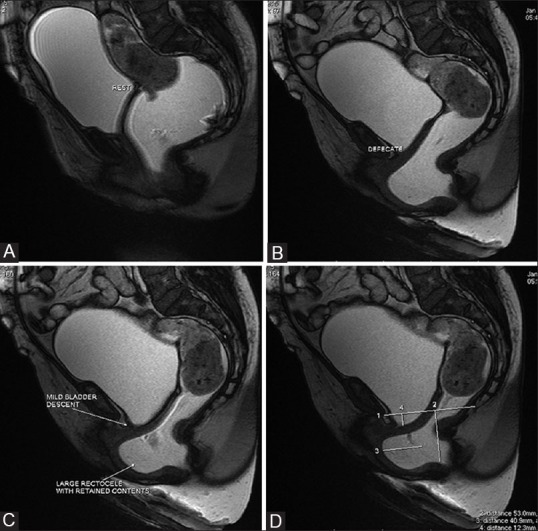
Retained contents in large anterior rectocele. Normal position at rest (A). On defecation (B-D), there is moderate anorectal descent (5.3 cm) and mild bladder descent (1.2 cm) with a large anterior rectocele (4.1 cm). The rectocele showed retained contents at the end of the defecating effort, (D) shows the measurements with line 1 representing the pubococcygeal line, lines 2 and 4 representing the anorectal and bladder descents, respectively, and line 3 representing the length of the rectocele
Rectal Intussusception and Rectal Prolapse
Invagination of a part (mucosa) or the entire thickness of the rectal wall into its lumen represents rectal intussusception [Figure 5]. It may involve the entire circumference of the rectum and may extend downward to various degrees (rectorectal/rectoanal intussusception). Extension beyond the anal verge represents rectal prolapse [Figure 6]. Intussusceptions are an important cause of outlet obstruction and incomplete defecation.
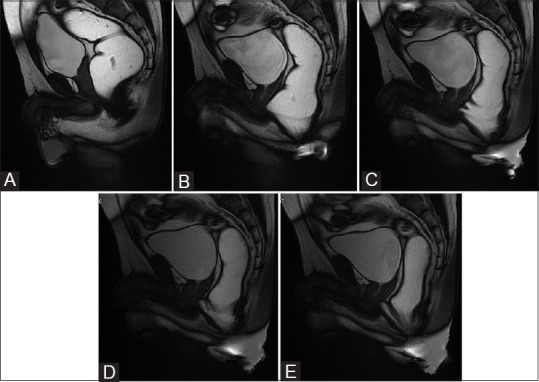
Figure 5(A-D).
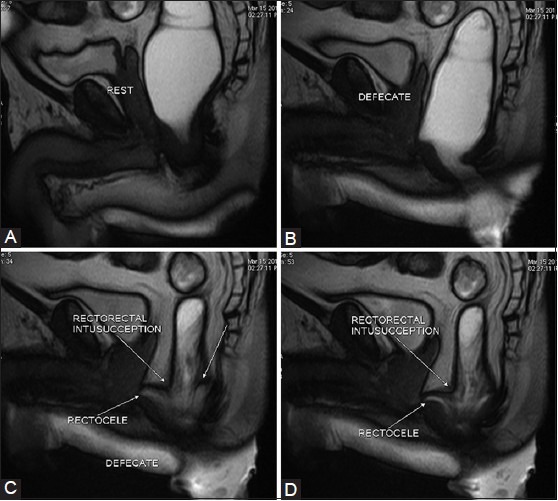
Rectorectal intussusception. Normal position at rest (A) with moderate anorectal descent on defecation (B). There is evidence of telescoping of the proximal rectum into the distal rectum representing rectorectal intussusception (C and D). Note the classical “arrowhead” configuration of the intussusception
Figure 6(A-E).
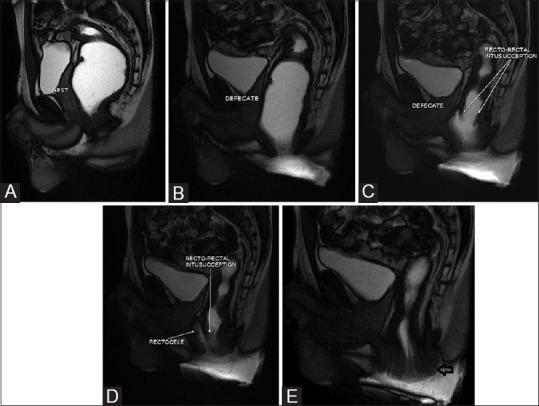
Rectal prolapse. Normal position at rest (A). During defecation (B-E), there is a rectorectal intussusception which progressively descends and eventually causes a rectal prolapse with mucosal outpouching through the anal verge (open arrow in E)
Spastic Perineum Syndrome
Normally, during defecation, the puborectalis muscle relaxes and the anorectal angle widens. Spastic perineum syndrome is diagnosed when there is persistent prominent indentation of the puborectalis sling on the posterior rectal wall with an acute anorectal angle during defecation [Figure 7]. The puborectalis frequently appears hypertrophied and these patients show elevated pressures on anorectal manometry.[7]
Figure 7(A-D).
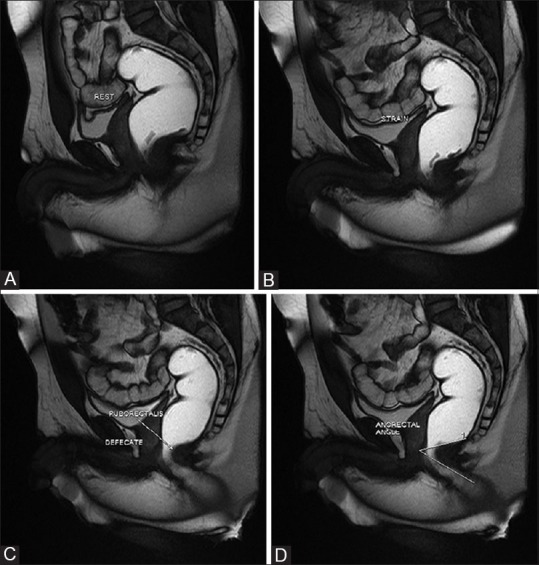
Spastic pelvic floor syndrome. Normal position at rest (A). During straining (B) and defecation (C), there is persistent prominent indentation of the puborectalis sling on the posterior rectal wall with an acute anorectal angle. (D) shows the acute anorectal angle of approximately 44° (measured between the posterior rectal and anal walls) during defecation. Compare with the normal defecogram in Figure 1
Enteroceles
Enterocele is the downward herniation of the peritoneal sac and small bowel loops into the pouch of Douglas along the anterior rectal wall [Figure 8]. MRI can demonstrate the small bowel loops without the need for oral contrast. It is important to detect enterocele because many authors consider it to be a contraindication for STARR surgery as there is a risk of injury to the low-placed small bowel by the stapler as it draws in the rectal wall.[8]
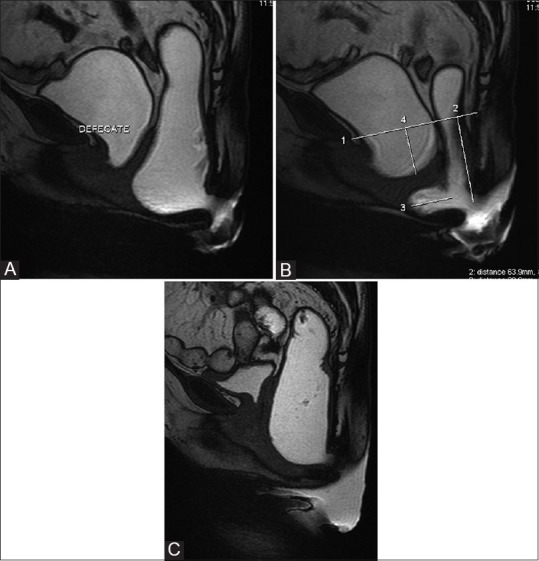
Figure 8(A-C).
Enterocele. Normal position at rest (A). During defecation (B and C), there is descent of the peritoneal sac with small bowel loops along the anterior rectal wall representing an enterocele. Also note the bladder and anorectal descent, anterior rectocele, and rectorectal intussusception
Descending Perineum
As the name suggests, it represents abnormal descent of one or all the three compartments of the pelvic floor due to poor muscle tone. Additional opacification of the vaginal vault by ultrasound jelly may be performed to obtain a tricompartmental MRD (urine in bladder is a natural contrast) which may better delineate the degree of descent [Figure 9].
Figure 9(A-D).
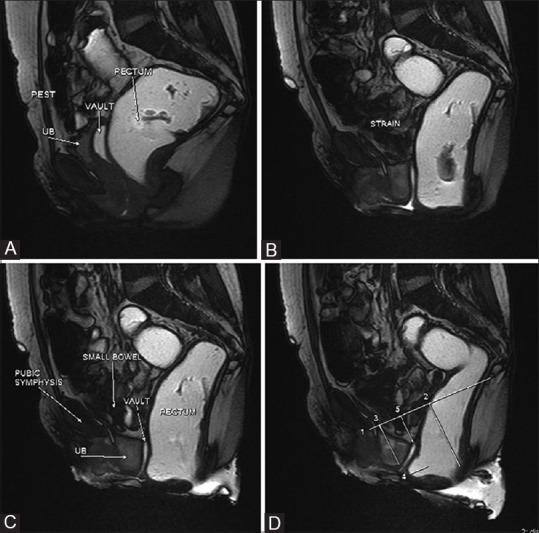
Descending perineum on tricompartmental defecogram. Normal position at rest (A). Note the opacification of the vaginal vault by T2-hyperintense jelly improving its visualization. During straining (B) and defecation (C), there is significant descent of all the three compartments (i.e. urinary bladder, vaginal vault, and anorectal junction). The descents are measured below the pubococcygeal line as shown in (D). A small anterior rectocele is also seen
Our Experience and the Role of MRD in ODS
Various modalities have been used for the evaluation of defecation dynamics. These include fluoroscopic defecography and MRD. MRI has the advantages of much better delineation of all the pelvic soft tissue structures and absence of ionizing radiation. MRD can be performed in open magnets in a sitting position or in closed tunnel magnets in a supine position. Open magnets with sitting configuration are not easily available. Supine position during defecography is considered non-physiological and some patients may find it difficult to strain effectively in this position. However, supine MRD compares well with erect MRD for the depiction of clinically relevant pathologies.[9] The reason postulated for this is that the straining forces during defecation are far greater than gravity, and hence, these would be enough to elicit the pathologies.[10]
We found that sometimes abnormalities, especially rectal intussusceptions, developed in the later stages of defecation on prolonged straining. Hence, it is important to run the dynamic sequence long enough so as not to miss these delayed findings [Figure 10].
Figure 10(A-E).
Delayed rectorectal intussusception. Normal position at rest (A). During early defecation (B), no obvious abnormality was detected. However, during later stages of defecation, undulations appeared in the anterior rectal wall (C) with progressive development of rectorectal intussusception (D and E). This emphasises the need to run the dynamic sequence long enough to detect these delayed abnormalities which manifest on prolonged straining effort
Paste of mashed potatoes can be used instead of ultrasound jelly. A T1W multiphasic dynamic sequence can also be used for the defecography. We used a combination of ultrasound jelly and T2W defecography because the jelly provides good natural T2 contrast. Also, the T2W defecography provides better depiction of the other pelvic structures like the bladder, uterus, and vagina. Moreover, ultrasound jelly is readily available in radiology departments.
Various treatment options are available for patients with ODS and imaging plays a very important role in deciding the optimal treatment strategy for a particular patient. If imaging does not reveal significant structural abnormalities, then the patient is offered conservative treatment like diet and lifestyle modifications and biofeedback therapy.[4]
On the other hand, patients with significant structural abnormalities on imaging studies are more likely to benefit from surgical approaches that attempt to correct those structural abnormalities.[11] Various surgical techniques have been described for treatment of ODS, including transvaginal, transperineal, transanal, transabdominal, and combined approaches. STARR, described by Longo in 2004, is a relatively new and less invasive addition to the surgical armamentarium for treating patients with ODS.[11] As a result, there is now an increasing emphasis on imaging tests like MRD to identify this subset of patients who would benefit by STARR. Moreover, MRD allows a multi-compartmental evaluation and, thus, further aids surgical planning. So, patients with significant co-existing bladder and/or vaginal descent may need additional pelvic floor strengthening procedures along with STARR.[12] MRD can be used to assess the success of the operative repair [Figure 11]. MRD also helps to identify patients with spastic perineum syndrome who may respond well to botulinum toxin type A injection into the hyperactive puborectalis muscle.[13]
Figure 11(A-C).
Pre- and post-operative MRD. Pre-operative MRD images (A and B) show significant bladder, vault, and anorectal descent with moderate anterior rectocele. The patient underwent anterior and posterior colporrhaphy and sacrospinous ligament fixation with trans-obturator band. Defecation phase of postoperative MRD (C) shows complete resolution of the bladder and vault descent and the anterior rectocele. The patient also showed symptomatic improvement
Our observations and experience show that supine MRD demonstrates the structural abnormalities associated with ODS in a high percentage of patients. It was also able to grade the pathologies and provide holistic information regarding the pelvic floor, which is essential for optimal treatment planning. To our knowledge, this is the largest series of MRD in ODS in the Indian population.
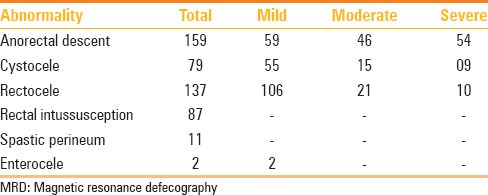
Out of the 192 patients that we have studied, 28 studies were normal or showed only mild descent of the anorectal junction. The remaining studies showed one or more abnormalities [Table 2].
Table 2.
Abnormalities and their grades detected in our series of MRD
Conclusion
MRD is a useful tool for the evaluation of patients with ODS and can demonstrate structural abnormalities which can guide treatment planning.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–91. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 2.Sonnenberg A, Koch TR. Physician visits in the United States for constipation: 1958 to 1986. Dig Dis Sci. 1989;34:606–11. doi: 10.1007/BF01536339. [DOI] [PubMed] [Google Scholar]
- 3.Lembo A, Camilleri M. Chronic constipation. N Engl J Med. 2003;349:1360–8. doi: 10.1056/NEJMra020995. [DOI] [PubMed] [Google Scholar]
- 4.National Institute for Health and Clinical Excellence. Stapled Transanal Rectal Resection for Obstructed Defecation Syndrome. NICE Interventional Procedure Guidance (IPG 351) Issued June 2010. [Last accessed on 2014 Jun 20]. Available from: http://www.nice.org.uk .
- 5.Kelvin FM, Maglinte DD, Hale DS, Benson JT. Female pelvic organ prolapse: A comparison of triphasic dynamic MR imaging and triphasic fluoroscopic cystocolpoproctography. AJR Am J Roentgenol. 2000;174:81–8. doi: 10.2214/ajr.174.1.1740081. [DOI] [PubMed] [Google Scholar]
- 6.Pfeifer J, Oliveira L, Park UC, Gonzalez A, Agachan F, Wexner SD. Are interpretations of video defecographies reliable and reproducible? Int J Colorectal Dis. 1997;12:67–72. doi: 10.1007/s003840050083. [DOI] [PubMed] [Google Scholar]
- 7.Roos JE, Weishaupt D, Wildermuth S, Willmann JK, Marincek B, Hilfiker PR. Experience of 4 years with open MR defecography: Pictorial review of anorectal anatomy and disease. Radiographics. 2002;22:817–32. doi: 10.1148/radiographics.22.4.g02jl02817. [DOI] [PubMed] [Google Scholar]
- 8.Schwandner O, Scherer R. Patient selection for stapled hemorrhoidopexy and STARR. In: Jayne D, Stuto A, editors. Transanal Stapling Techniques for Anorectal Prolapse. London: Springer; 2009. pp. 59–71. [Google Scholar]
- 9.Bertschinger KM, Hetzer FH, Roos JE, Treiber K, Marincek B, Hilfiker PR. Dynamic MR imaging of the pelvic floor performed with patient sitting in an open-magnet unit versus with patient supine in a closed-magnet unit. Radiology. 2002;223:501–8. doi: 10.1148/radiol.2232010665. [DOI] [PubMed] [Google Scholar]
- 10.Seynaeve R, Billiet I, Vossaert P, Verleyen P, Steegmans A. MR imaging of the pelvic floor. JBR-BTR. 2006;89:182–9. [PubMed] [Google Scholar]
- 11.Zhang B, Ding JH, Yin SH, Zhang M, Zhao K. Stapled transanal rectal resection for obstructed11.defecation syndrome associated with rectocele and rectal intussusception. World J Gastroenterol. 2010;16:2542–8. doi: 10.3748/wjg.v16.i20.2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosen A. Obstructed defecation syndrome: Diagnosis and therapeutic options, with special focus on the STARR procedure. Isr Med Assoc J. 2010;12:104–6. [PubMed] [Google Scholar]
- 13.Khaikin M, Wexner SD. Treatment strategies in obstructed defecation and fecal incontinence. World J Gastroenterol. 2006;12:3168–73. doi: 10.3748/wjg.v12.i20.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]


