Abstract
Purpose:
To quantitatively analyze central corneal thickness (CCT) in patients with primary angle closure glaucoma (PACG) and primary open-angle glaucoma (POAG), and to evaluate its correlation with severity of glaucoma.
Methods:
In this retrospective study, records of patients with previously diagnosed POAG or PACG at a tertiary glaucoma service were reviewed. CCT was measured by ultrasound pachymetry. Mean deviation (MD) on visual field (VF) testing was recorded for glaucoma severity determination. CCT and age- and sex-adjusted CCT were compared among the study groups using Student's t-test and analysis of covariance (ANCOVA), respectively. Univariate and multivariate regression models were used for correlation of age, MD and CCT.
Results:
A total of 115 patients with PACG, 215 with POAG, and 100 normal controls were included with mean age of 64.1 ± 10.4, 59.9 ± 10.5, and 62.04 ± 10.80 years, respectively. CCT was thicker in PACG eyes (545.5 ± 46.1 μm) as compared to POAG eyes (531.7 ± 37.3 μm) and controls (531.0 ± 38.3 μm) even after age and gender adjustment (ANCOVA, P = 0.05). CCT was found to decrease with increasing age only in the POAG group (β = -0.57, P = 0.01). Disease severity (MD of VF) was significantly and inversely correlated with CCT in both POAG and PACG eyes (β = 1.89, P = 0.02; and β = 1.38, P = 0.04, respectively) after age and sex correction.
Conclusion:
PACG eyes had thicker CCT as compared to POAG and normal healthy eyes in Iranian subjects. Severity of the disease was inversely correlated with CCT in eyes with both POAG and PACG.
Keywords: Central Corneal Thickness; Primary Angle Closure Glaucoma; Primary Open-angle Glaucoma, Intraocular Pressure
INTRODUCTION
The number of people with primary open angle glaucoma (POAG) is estimated to reach 58.6 million by 2020 worldwide, while primary angle closure glaucoma (PACG) will affect another 21 million.[1] More than 5.9 million people will be bilaterally blind from POAG in 2020.[1] However, half of all glaucoma induced blindness will be due to PACG. Asian populations represent 87% of all PACG cases.[1]
Intraocular pressure (IOP) is the key risk factor for glaucoma and any variable resulting in overestimation or underestimation of IOP in patients with glaucoma may significantly impact its treatment and prognosis. Goldmann applanation tonometry (GAT) has been the gold standard for IOP measurement since its introduction in 1956.[2]
The effect of central corneal thickness (CCT) on IOP measurements using GAT has been studied extensively in patients with POAG,[3] ocular hypertension, normotensive glaucoma,[4,5] and congenital glaucoma.[6] CCT has also been identified as a substantial glaucoma risk factor for progression of disease in open angle glaucoma[7] and normal tension glaucoma.[8,9,10]
There are few studies which compare CCT in patients with PACG and POAG. Moreover, correlation between CCT and severity of glaucoma in PACG patients has not been investigated well. The aim of the current study was to evaluate CCT in eyes with PACG and POAG and to determine the correlation between CCT and the severity of glaucoma in each subgroup.
METHODS
We reviewed the records of patients with POAG or PACG who were referred to the glaucoma service at Farabi Eye Hospital, Tehran, Iran since March 2005 to May 2008. A group of non-glaucomatous subjects were selected from the general eye clinic as controls.
Exclusion criteria included previous history of ocular trauma, intraocular laser or surgery, any systemic disease which may influence CCT, moderate to severe cataract, IOP more than 25 mmHg on the day of CCT measurement, chronic uveitis, central corneal opacity or scarring, corneal edema, and history of refractive surgery or penetrating keratoplasty. In healthy controls, exclusion criteria were IOP > 22 mmHg, typical glaucomatous disc appearance, visual field changes, and other conditions already mentioned above for glaucoma cases. If both eyes were eligible for the study, the study eye was selected randomly.
Data collected from all subjects included age, gender, type of glaucoma, cup/disc ratio, IOP at initial visit, and medical therapy. Carbonic anhydrase inhibitors (CAI) use was defined as having used systemic or topical CAIs for at least 1 month before pachymetry. Best corrected visual acuity (BCVA), slit lamp biomicroscopy, GAT, and dilated pupil ophthalmoscopy were performed for all subjects. Visual field (VF) was evaluated with the Humphrey VF analyzer (central 24-2 SITA standard program; Carl Zeiss Meditec Inc., Dublin, CA, USA). VF reliability criteria included fixation losses and false-positive and false-negative rates of less than 25%. Severity of glaucoma was categorized based on perimetry according to the Hodapp-Parrish-Anderson classification.[11]
Corneal thickness was measured during the day (between 9 a.m. and 12 a.m.) by a masked examiner. After corneal anesthesia using topical tetracaine, the probe of the ultrasound pachymeter was perpendicularly touched to the center of the cornea and five measurements were recorded. The same pachymeter (Sonomed 200P + Micropach, Sonomed Inc., NY, USA) was used for all measurements. Care was taken to be as perpendicular to the central cornea as possible.
Statistical analyses were performed by SPSS software (version 13.0; SPSS, Chicago, IL, USA) using independent-samples t-test to evaluate normally distributed continuous variables. Pearson correlations and linear regression were used to examine the association between CCT and continuous variables in each group. CCT in POAG and PACG were adjusted for sex, age and disease severity and compared using analysis of covariance (ANCOVA) test. P <0.05 were considered as statistically significant.
RESULTS
We evaluated a total of 215 eyes of 215 subjects with POAG (117 male and 98 female subjects), 115 eyes of 115 subjects with PACG (33 male and 82 female subjects), and 100 normal controls (33 male and 67 female subjects) in the study. Mean age of the study subgroups was 64.1 ± 10.4, 59.9 ± 10.5, and 62.0 ± 10.8 years, respectively. Patient demographics and clinical features have been summarized in Table 1.
Table 1.
Patient characteristics and CCT in eyes with POAG, PACG, and control subjects
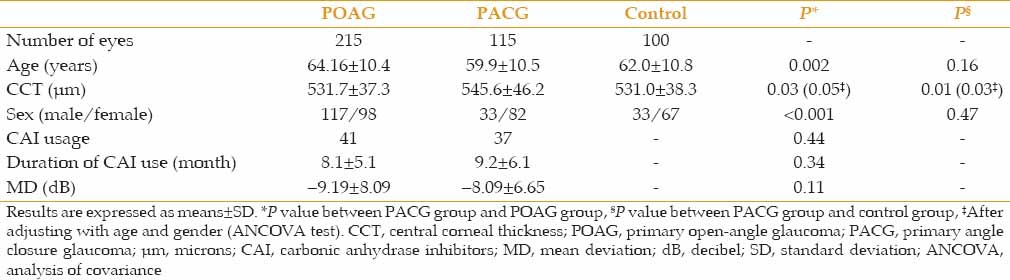
There were significantly more female subjects (P < 0.001) and mean age was significantly younger (59.97 ± 10.5 years vs. 64.16 ± 10.4 years, P = 0.002) in the PACG group as compared to POAG patients. There were no differences between the two glaucoma groups in MD on VF testing. The PACG and control groups were comparable in terms of sex and age [Table 1].
Mean CCT values were 531.7 ± 37.3, 545.5 ± 46.1, and 531.0 ± 38.3 microns (µ) in eyes with POAG, PACG and controls, respectively. CCT was significantly thicker in the PACG group (P = 0.03) even after adjusting for age and gender [ANCOVA, P = 0.0, Table 1]. CCT was found to decrease with increasing age in the POAG group (β = -0.57, P = 0.01), however no relationship was found between age and CCT in the PACG group (β = -0.19, P = 0.65) [Figure 1]. We observed a non-significant difference in CCT between male and female subjects in both POAG (535.1 ± 39.2 μm in female vs 528.8 ± 35.5 μm in male subjects) and PACG groups (550.4 ± 45.6 μm in female vs. 533.3 ± 45.9 μm in male subjects). CCT in female participants was non-significantly thicker than male patients in both glaucoma groups even after adjusting for age (ANCOVA, P = 0.30 and P = 0.09 for the POAG and PACG groups, respectively).
Figure 1.
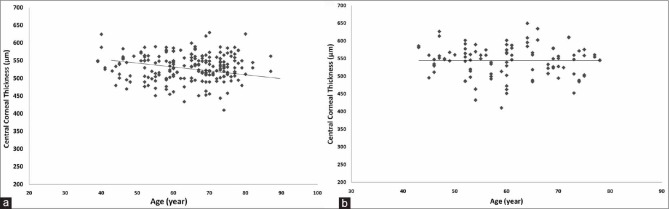
Relationship between age and central corneal thickness (CCT) in the two study groups: CCT was found to decrease with increasing age in the primary open angle glaucoma group (β = -0.57, P=0.01) (a) but no relationship was found between age and CCT in the primary angle closure group (β = -0.19, P=0.65) (b).
Univariate analysis demonstrated that disease severity (MD) was significantly and inversely correlated with CCT in both POAG and PACG groups [r = 0.26, P = 0.001 and r = 0.24, P = 0.02, respectively, Figure 2]. The same results were obtained after multivariate analysis, in which MD was significantly associated with CCT in both POAG (β = 1.89, P = 0.02) and PACG (β = 1.38, P = 0.04) groups after age and sex adjustment.
Figure 2.
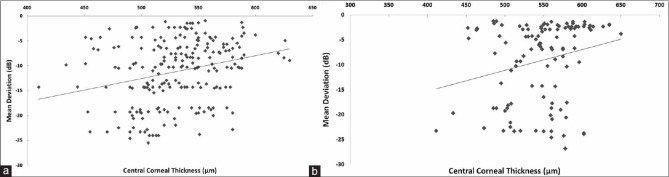
Univariate analysis demonstrated that disease severity (mean deviation) was significantly correlated with central corneal thickness in both primary open angle glaucoma (a) and primary angle closure glaucoma (b) (r=0.26, P=0.001 and r=0.24, P=0.02, respectively).
DISCUSSION
In this clinic-based study, we found that CCT in PACG was significantly thicker than POAG or normal controls. There are some studies on CCT in PACG reporting no difference in CCT between PACG and controls.[12,13] However, these studies suffer from small sample size. Two studies investigated CCT in Asian populations and reported no difference in CCT between various glaucoma subtypes.[14,15] On the other hand, Shah et al reported significantly higher CCT in PACG eyes as compared to POAG and normal eyes.[16] Another recent report in an Asian population reported that CCT is significantly higher in both PACG and POAG as compared to the normal population.[17] The current study revealed that CCT in PACG eyes was significantly thicker than POAG cases. After adjustment for age and sex, CCT was still significantly higher in the PACG group. Considering these findings, it can be hypothesized that a thicker cornea may have a contributory effect on angle occludability, that is, a thicker CCT may be associated with a thick peripheral cornea and thus a more crowded angle.
To our knowledge, this is the first report on CCT in patients with PACG in an Iranian population. There are a few studies measuring CCT in normal populations in different areas of Iran including a population-based study in Tehran, Iran through which CCT was reported to be 528 μm.[18] Similar to many other reports in other communities,[19,20,21,22] CCT in POAG eyes in our study was comparable to CCT in normal controls. Our data revealed a statistically significant higher CCT in eyes with PACG in comparison to the POAG group or normal controls.
There is no consensus on the effect of gender on CCT. Some reports have indicated that female gender is associated with a thicker cornea, although others have reported slightly thicker CCT in male subjects.[15,23,24,25,26] The Beijing Eye Study reported higher CCT in male subjects in both the glaucomatous and normal populations.[15] Another study reported a similar association for subjects with normal tension glaucoma (NTG).[27] In the present study, there was no significant difference in CCT between male and female subjects in both glaucoma groups, although there was a trend toward thicker CCT in females with PACG (P = 0.09 after adjustment for age) which may explain the higher risk of PACG among women.
The correlation between CCT and age in normal population has been studied well before. Most of these studies have revealed an inverse correlation between CCT and age (a decrease of 3–7 μm in CCT per decade of older age).[22,24,25,28,29] A meta-analysis by Doughty et al[3] reported a reverse relationship between age and corneal thickness only in non-white populations. The inverse correlation between CCT and age in our Middle Eastern subjects is consistent with previous literature. Although we found a significant decrease in CCT with increase in age in our POAG cases, the relationship was not significant in PACG eyes.
Several investigators reported a reverse correlation between CCT and visual field defects in POAG;[30,31] however, there are few studies demonstrating this correlation in PACG. In the present study, we found a correlation between CCT and MD in both PACG and POAG. Similar to our study, Hong et al showed that PACG patients with a cornea thinner than 540 μm are at greater risk for visual field progression even if they maintain low IOP after treatment.[32]
Few studies have evaluated the role of anterior chamber depth and lens parameters in Iranian populations;[33,34] but to our knowledge, this is the first report on CCT measurement in PACG in an Iranian population. Our results showed that in PACG eyes, similar to POAG cases, thinner cornea is a risk factor for advanced disease, therefore PACG cases with thinner cornea should be followed more carefully. Thinner lamina cribrosa in eyes with thinner CCT might be a reason for this finding; thus, evaluating the lamina cribrosa in these cases could be useful to address this hypothesis in PACG eyes.
The findings of our study should be interpreted in view of its limitations. As the patients were of Iranian descent, the results may not be applicable to other racial groups. Our patients were recruited from the glaucoma and general clinic at Farabi Eye Hospital, which is a tertiary care center and may not be generalizable to all races in Iran. Although the average difference of 14 μm in CCT in PACG eyes compared to normal controls may not be clinically significant or affect IOP measurements, it might predispose to a narrower drainage angle.
In summary, the current study revealed that CCT in PACG is significantly thicker than POAG and normal controls in a convenience sample from our hospital. We also found an inverse correlation between CCT and severity of glaucoma in patients with PACG and POAG. Population based studies may be required to generalize the results of this study to Iranian population.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldmann H, Schmidt T. Applanation tonometry. Ophthalmologica. 1957;134:221–242. doi: 10.1159/000303213. [DOI] [PubMed] [Google Scholar]
- 3.Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: A review and meta-analysis approach. Surv Ophthalmol. 2000;44:367–408. doi: 10.1016/s0039-6257(00)00110-7. [DOI] [PubMed] [Google Scholar]
- 4.Ehlers N, Hansen FK. Central corneal thickness in low-tension glaucoma. Acta Ophthalmol (Copenh) 1974;52:740–746. doi: 10.1111/j.1755-3768.1974.tb01109.x. [DOI] [PubMed] [Google Scholar]
- 5.Morad Y, Sharon E, Hefetz L, Nemet P. Corneal thickness and curvature in normal-tension glaucoma. Am J Ophthalmol. 1998;125:164–168. doi: 10.1016/s0002-9394(99)80086-5. [DOI] [PubMed] [Google Scholar]
- 6.Simsek T, Mutluay AH, Elgin U, Gursel R, Batman A. Glaucoma and increased central corneal thickness in aphakic and pseudophakic patients after congenital cataract surgery. Br J Ophthalmol. 2006;90:1103–1106. doi: 10.1136/bjo.2006.096370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herndon LW, Weizer JS, Stinnett SS. Central corneal thickness as a risk factor for advanced glaucoma damage. Arch Ophthalmol. 2004;122:17–21. doi: 10.1001/archopht.122.1.17. [DOI] [PubMed] [Google Scholar]
- 8.Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, et al. The Ocular Hypertension Treatment Study: Baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:714–720. doi: 10.1001/archopht.120.6.714. [DOI] [PubMed] [Google Scholar]
- 9.Whitacre MM, Stein R. Sources of error with use of Goldmann-type tonometers. Surv Ophthalmol. 1993;38:1–30. doi: 10.1016/0039-6257(93)90053-a. [DOI] [PubMed] [Google Scholar]
- 10.Bron AM, Creuzot-Garcher C, Goudeau-Boutillon S, d’Athis P. Falsely elevated intraocular pressure due to increased central corneal thickness. Graefes Arch Clin Exp Ophthalmol. 1999;237:220–224. doi: 10.1007/s004170050222. [DOI] [PubMed] [Google Scholar]
- 11.Hodapp E, Parrish RI, Anderson D, editors. St. Louis: Mosby Co; 1993. Clinical Decisions in Glaucoma. [Google Scholar]
- 12.Lowe RF. Central corneal thickness. Ocular correlations in normal eyes and those with primary angle-closure glaucoma. Br J Ophthalmol. 1969;53:824–826. doi: 10.1136/bjo.53.12.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mello PR, Meirelles SH, Moraes HV., Júnior Correlation between central corneal thickness and axial length in patients with glaucoma and normal eyes. Arq Bras Oftalmol. 2009;72:497–502. doi: 10.1590/s0004-27492009000400012. [DOI] [PubMed] [Google Scholar]
- 14.Wu LL, Suzuki Y, Ideta R, Araie M. Central corneal thickness of normal tension glaucoma patients in Japan. Jpn J Ophthalmol. 2000;44:643–647. doi: 10.1016/s0021-5155(00)00275-6. [DOI] [PubMed] [Google Scholar]
- 15.Xu L, Zhang H, Wang YX, Jonas JB. Central corneal thickness and glaucoma in adult Chinese: The Beijing Eye Study. J Glaucoma. 2008;17:647–653. doi: 10.1097/IJG.0b013e3181666582. [DOI] [PubMed] [Google Scholar]
- 16.Shah S, Chatterjee A, Mathai M, Kelly SP, Kwartz J, Henson D, et al. Relationship between corneal thickness and measured intraocular pressure in a general ophthalmology clinic. Ophthalmology. 1999;106:2154–2160. doi: 10.1016/S0161-6420(99)90498-0. [DOI] [PubMed] [Google Scholar]
- 17.Day AC, Machin D, Aung T, Gazzard G, Husain R, Chew PT, et al. Central corneal thickness and glaucoma in East Asian people. Invest Ophthalmol Vis Sci. 2011;52:8407–8412. doi: 10.1167/iovs.11-7927. [DOI] [PubMed] [Google Scholar]
- 18.Hashemi H, Yazdani K, Mehravaran S, KhabazKhoob M, Mohammad K, Parsafar H, et al. Corneal thickness in a population-based, cross-sectional study: The Tehran Eye Study. Cornea. 2009;28:395–400. doi: 10.1097/ICO.0b013e31818c4d62. [DOI] [PubMed] [Google Scholar]
- 19.Wolfs RC, Klaver CC, Vingerling JR, Grobbee DE, Hofman A, de Jong PT. Distribution of central corneal thickness and its association with intraocular pressure: The Rotterdam Study. Am J Ophthalmol. 1997;123:767–772. doi: 10.1016/s0002-9394(14)71125-0. [DOI] [PubMed] [Google Scholar]
- 20.Ventura AC, Böhnke M, Mojon DS. Central corneal thickness measurements in patients with normal tension glaucoma, primary open angle glaucoma, pseudoexfoliation glaucoma, or ocular hypertension. Br J Ophthalmol. 2001;85:792–795. doi: 10.1136/bjo.85.7.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herman DC, Hodge DO, Bourne WM. Increased corneal thickness in patients with ocular hypertension. Arch Ophthalmol. 2001;119:334–336. doi: 10.1001/archopht.119.3.334. [DOI] [PubMed] [Google Scholar]
- 22.Nemesure B, Wu SY, Hennis A, Leske MC Barbados Eye Study Group. Corneal thickness and intraocular pressure in the Barbados eye studies. Arch Ophthalmol. 2003;121:240–244. doi: 10.1001/archopht.121.2.240. [DOI] [PubMed] [Google Scholar]
- 23.Zhang H, Xu L, Chen C, Jonas JB. Central corneal thickness in adult Chinese. Association with ocular and general parameters. The Beijing Eye Study. Graefes Arch Clin Exp Ophthalmol. 2008;246:587–592. doi: 10.1007/s00417-007-0760-9. [DOI] [PubMed] [Google Scholar]
- 24.Alsbirk PH. Corneal thickness.I. Age variation, sex difference and oculometric correlations. Acta Ophthalmol (Copenh) 1978;56:95–104. doi: 10.1111/j.1755-3768.1978.tb00471.x. [DOI] [PubMed] [Google Scholar]
- 25.Hahn S, Azen S, Ying-Lai M, Varma R Los Angeles Latino Eye Study Group. Central corneal thickness in Latinos. Invest Ophthalmol Vis Sci. 2003;44:1508–1512. doi: 10.1167/iovs.02-0641. [DOI] [PubMed] [Google Scholar]
- 26.Shimmyo M, Ross AJ, Moy A, Mostafavi R. Intraocular pressure, Goldmann applanation tension, corneal thickness, and corneal curvature in Caucasians, Asians, Hispanics, and African Americans. Am J Ophthalmol. 2003;136:603–613. doi: 10.1016/s0002-9394(03)00424-0. [DOI] [PubMed] [Google Scholar]
- 27.Pang CE, Lee KY, Su DH, Htoon HM, Ng JY, Kumar RS, et al. Central corneal thickness in Chinese subjects with primary angle closure glaucoma. J Glaucoma. 2011;20:401–404. doi: 10.1097/IJG.0b013e3181f3e5d9. [DOI] [PubMed] [Google Scholar]
- 28.Foster PJ, Baasanhu J, Alsbirk PH, Munkhbayar D, Uranchimeg D, Johnson GJ. Glaucoma in Mongolia. A population-based survey in Hövsgöl province, northern Mongolia. Arch Ophthalmol. 1996;114:1235–1241. doi: 10.1001/archopht.1996.01100140435011. [DOI] [PubMed] [Google Scholar]
- 29.Aghaian E, Choe JE, Lin S, Stamper RL. Central corneal thickness of Caucasians, Chinese, Hispanics, Filipinos, African Americans, and Japanese in a glaucoma clinic. Ophthalmology. 2004;111:2211–2219. doi: 10.1016/j.ophtha.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 30.Sullivan-Mee M, Halverson KD, Saxon MC, Saxon GB, Qualls C. Central corneal thickness and normal tension glaucoma: A cross-sectional study. Optometry. 2006;77:134–140. doi: 10.1016/j.optm.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 31.Sullivan-Mee M, Halverson KD, Saxon GB, Saxon MC, Qualls C. Relationship between central corneal thickness and severity of glaucomatous visual field loss in a primary care population. Optometry. 2006;77:40–46. doi: 10.1016/j.optm.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 32.Hong S, Kim CY, Seong GJ, Hong YJ. Central corneal thickness and visual field progression in patients with chronic primary angle-closure glaucoma with low intraocular pressure. Am J Ophthalmol. 2007;143:362–363. doi: 10.1016/j.ajo.2006.09.038. [DOI] [PubMed] [Google Scholar]
- 33.Moghimi S, Vahedian Z, Fakhraie G, Ghaffari R, Eslami Y, Jabarvand M, et al. Ocular biometry in the subtypes of angle closure: An anterior segment optical coherence tomography study. Am J Ophthalmol. 2013;155:664–673. doi: 10.1016/j.ajo.2012.10.014. e1. [DOI] [PubMed] [Google Scholar]
- 34.Eslami Y, Latifi G, Moghimi S, Ghaffari R, Fakhraie G, Zarei R, et al. Effect of adjunctive viscogonioplasty on drainage angle status in cataract surgery: A randomized clinical trial. Clin Experiment Ophthalmol. 2013;41:368–378. doi: 10.1111/j.1442-9071.2012.02871.x. [DOI] [PubMed] [Google Scholar]


