Abstract
Purpose:
To evaluate long term intraocular pressure (IOP) control after repeat selective laser trabeculoplasty (SLT).
Methods:
This single center study retrospectively reviews the electronic medical records of patients with open angle glaucoma undergoing repeat SLT. Eyes with prior argon laser trabeculoplasty, or incisional surgery before or during the study period were excluded. Demographics, laser parameters, number of glaucoma medications and IOP at baseline and after 1, 4, 8, 12, 18 and 24 months were collected. The percentage of subjects with IOP reduction >20% and ≥15% from baseline was determined.
Results:
A total of 45 eyes of 25 subjects with mean age of 73 ± 9 years undergoing repeat SLT were included. Repeat SLT was performed at a mean interval of 28.3 ± 12.7 months after initial treatment. Mean IOP reductions were statistically significant with repeat SLT as compared to baseline at 1, 4, 8, 12, 18 and 24 months’ follow-up. Change in IOP after first and repeat SLT were comparable at most time points except at 4, 8 and 12 months when initial treatment had yielded significantly greater reductions. At 24 months, 29% and 39% of eyes achieved IOP reduction >20% and ≥15% respectively after repeat SLT as compared to 36% and 54% of eyes following initial treatment (P > 0.05).
Conclusion:
Repeat SLT is effective in lowering IOP up to 24 months. Long term IOP control was achieved in 29–39% of eyes following repeat treatment in this cohort of patients.
Keywords: Glaucoma Treatment, Intraocular Pressure, Repeat Selective Laser Trabeculoplasty
INTRODUCTION
Selective laser trabeculoplasty (SLT) is an effective intraocular pressure (IOP) lowering treatment for patients with open angle glaucoma or ocular hypertension.[1,2,3,4,5] It is believed to work by selective targeting of pigmented trabecular meshwork cells with minimal structural damage to the trabecular meshwork.[6,7] This is in contrast to argon laser trabeculoplasty (ALT) that is associated with significant tissue disruption and coagulative damage.[8,9] The efficacy of SLT and its minimal disruption of trabecular meshwork tissue as compared to other modalities of laser treatment make it a potentially repeatable treatment.
Repeating SLT treatment has become common practice and a popular alternative in patients requiring additional IOP reductions. However, evidence in the literature remains limited on the efficacy of repeat SLT treatment.[10,11] Another pressing question is whether repeating SLT after an initially successful treatment yields sustained long term IOP reductions. In this study we report the long term results from a retrospective analysis on the efficacy of repeat SLT in patients with open angle glaucoma.
METHODS
A review of efficacy of repeat SLT was conducted within a single comprehensive ophthalmology practice. The study was approved by the Institutional Review Board of the University of Medicine and Dentistry of New Jersey. Inclusion criteria were open angle glaucoma patients more than 18 years of age, including primary open angle glaucoma, pseudoexfoliation glaucoma, and pigmentary glaucoma who required additional IOP reduction while on medical treatment.
All subjects undergoing initial and repeat 360° SLT between May 2003 and May 2010 were included. Repeat SLT treatment was performed when further IOP reduction was necessary to meet target IOP as set by the treating physician. Exclusion criteria were patients below 18 years of age (including cases of juvenile glaucoma) and history of ALT or any incisional surgery (including cataract and glaucoma surgery) before or during the study period. In order to account for the incremental efficacy of SLT, subjects undergoing treatment less than 360° were also excluded.
Both initial and repeat SLT procedures were performed by treating all 4 quadrants using a Latina SLT gonioscopy laser lens (Ocular Instruments Inc., WA, USA) under topical anesthesia. Energy levels were titrated by the clinician just at the level required to observe “champagne bubble” formation. None of the patients were treated with topical steroids or nonsteroidal anti-inflammatory drugs after SLT. Data on anterior chamber cell and flare, and conjunctival hyperemia were not consistently recorded and thus not collected for analysis.
Data was extracted from an electronic medical record system. Patient demographics (age, sex, type of glaucoma), and SLT parameters including number of shots, mean energy and total energy (number of shots multiplied by mean energy used in mJ) were collected. Baseline Goldmann applanation IOP was calculated as the mean of the last two visits prior to SLT to reduce the effect of regression to the mean. IOP and number of glaucoma medications were collected at baseline and at 1, 4, 8, 12, 18, and 24 months. A window of ± 2 weeks was allowed for the 1st month time point; while ± 6 weeks was allowed for all other time points.
Comparison of means with student t-test, and one way ANOVA followed by Tukey's test were used for analysis. P < 0.05 were considered to be statistically significant. Means and standard deviation of IOP and number of glaucoma medications were calculated at baseline and at all time points. The percentage of subjects with IOP reduction >20% and >15% from baseline were determined. Box and Whisker, and Kaplan–Meier survival plots were used for analysis.
RESULTS
Forty-five eyes of 25 subjects including 15 female and 10 male patients with mean age of 73 ± 9 years that had undergone repeat SLT were included in the study. All SLT treatments were delivered to 360° of the angle. Repeat SLT treatment was performed at a mean interval of 27 ± 12 months after initial therapy. Initial and repeat SLT had mean energy levels of 0.94 ± 0.05 and 1.08 ± 0.23 mJ, and a mean total number of 111 ± 8 and 104 ± 7 spots respectively (P < 0.05). However mean total laser energy (calculated by multiplying mean energy [mJ] levels by the number of treatment spots) was not statistically different between initial (104 ± 8 mJ) and repeat SLT (112 ± 24 mJ) sessions (P > 0.05).
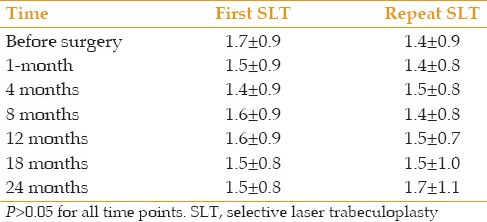
The mean number of glaucoma medications at baseline in patients undergoing repeat SLT was slightly lower than that before initial SLT (1.4 ± 0.8 vs. 1.7 ± 0.9); however this difference was not statistically significant. The mean number of glaucoma medications at 1, 4, 8, 12, 18 and 24 months were not significantly different from baseline or between initial and repeat SLT treatments at any time point [Table 1]. Medication use was stable for fellow eyes.
Table 1.
Number of glaucoma medications
Mean IOP and change in IOP after SLT are detailed in Tables 2 and 3. Baseline mean IOP before initial and second SLT were comparable at 19.7 and 19.1 mm Hg, respectively. Mean IOP at 1, 4, 8, 12, 18 and 24 months after initial and second SLT were significantly lower than baseline IOP (P < 0.05) [Figure 1]. A Box and Whisker plot and a Kaplan–Meier survival plot for first and repeat SLT show IOP reduction and survival over time [Figures 2 and 3].
Table 2.
Mean IOP
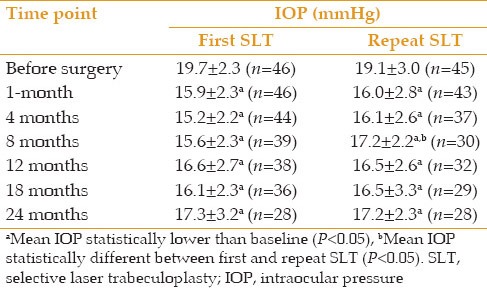
Table 3.
Reduction in IOP from baseline
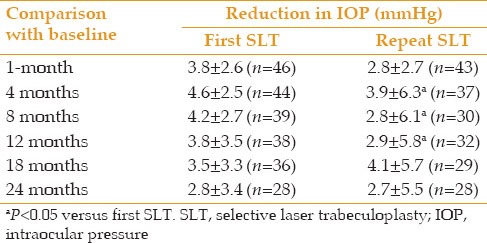
Figure 1.
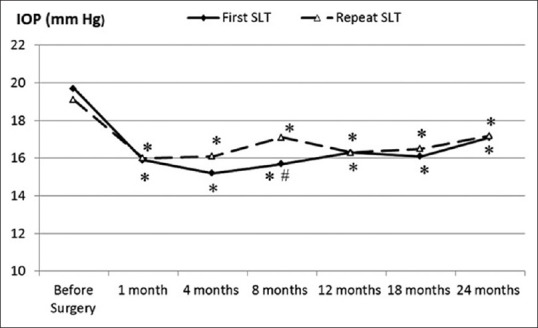
Mean intraocular pressure (IOP) at all time points following first and repeat SLT. *Mean IOP was statistically lower than baseline (P< 0.05), #mean IOP statistically different between first and repeat SLT.
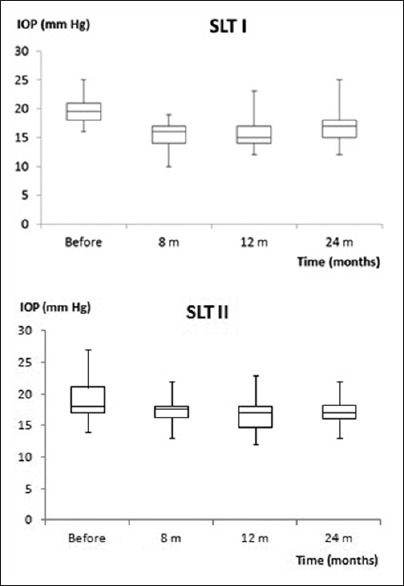
Figure 2.
Box and Whisker plot denoting intraocular pressure median, upper and lower quartiles, and range at different time points.
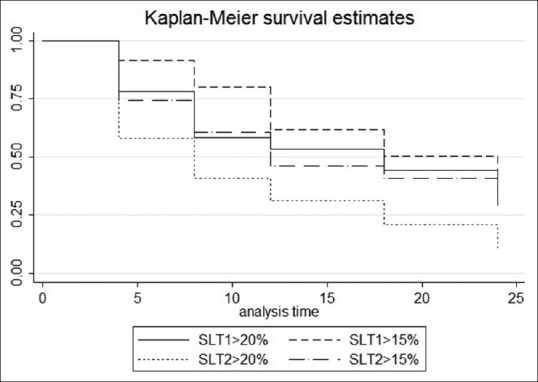
Figure 3.
Kaplan–Meier survival showing 20% and 15% plots for first and repeat SLT over 24 months.
When comparing initial and repeat SLT; mean IOP was not significantly different at any time point except at 8 months when IOP was significantly lower after initial SLT (15.6 vs. 17.2 mm Hg, P < 0.05). Change in IOP after first and repeat SLT were comparable except at 4, 8 and 12 months when initial SLT yielded significantly greater reductions. However, SLT efficacy was lowest at 24 months when mean change in IOP from baseline for initial and repeat SLT was 2.8 and 2.7 mm Hg respectively. This trend was also noted on the Box and Whisker and Kaplan–Meier survival plots [Figures 2 and 3].
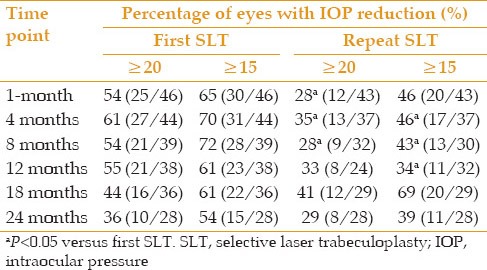
We also compared the percentage of eyes achieving IOP reductions >20% and >15% from baseline after initial and repeat SLT [Table 4]. Less eyes achieved IOP reductions >20% or >15% after repeat SLT as compared to initial treatment at all time points (except at 18 and 24 months).
Table 4.
Percentage of eyes with IOP reduction more than 20% and 15% from baseline
In order to evaluate IOP spikes after SLT, we examined data for IOP 26 mm Hg at the 1-month (±2 weeks) time point. For initial and repeat SLT, data was available for 46 of 46 and 43 of 45 eyes, respectively. No eye had IOP >26 mm Hg. The highest recorded IOP after first and repeat SLT was 20 and 22 mm Hg respectively.
DISCUSSION
Selective laser trabeculoplasty employs a 532-nm Q-switched frequency doubled Nd: YAG laser system that emits a single ultra-short duration low fluency (energy/area) pulse that selectively targets pigmented trabecular meshwork cells. At these values, thermal diffusion from targeted cells is minimized and adjacent trabecular meshwork cells are spared from thermal damage.[7,8] Although evidence suggests some ultrastructural changes to trabecular beams after SLT, those are more subtle than tissue changes observed after argon laser trabeculoplasty.[12] Selective tissue targeting and minimal trabecular meshwork structural changes after SLT support the repeatability of SLT treatment.
At present, repeat SLT is commonly performed by clinicians, although there is a paucity of literature on the efficacy of repeat SLT treatment. It is especially challenging to accurately compare studies where SLT is performed on eyes with or without prior trabeculoplasty or when 180 or 360° SLT is performed. Few groups have reported their experience with repeat SLT (Lai et al IOVS 2005;46: ARVO E-Abstract 119, Mequio et al IOVS 2007;48: ARVO E-Abstract 3972, Franco et al IOVS 2011 ARVO E-Abstract 2621). Although repeat SLT was effective, the results were variable and generally short term.
To date we are aware of only a few published reports on the efficacy of repeat 360° SLT in eyes previously treated with 360° SLT.[10,11] In one report, the short term response of first SLT (4 weeks) and repeat SLT (mean 4 months) was measured.[10] No significant difference between initial and repeat treatments was found in terms of mean IOP reduction or success rate in achieving >20% reduction. In another more elaborate report, Hong et al[11] reported on the efficacy of repeat SLT in 44 eyes with open angle glaucoma. At 5–8 months, IOP reduction from first and repeat SLT were 4.0 and 2.9 mm Hg respectively (P = 0.16). The percentage of eyes achieving >20% IOP reduction at 5–8 months was 50% and 43% for first and repeat SLT eyes respectively. They concluded that repeat SLT was as effective as the first SLT at about 6 months’ follow-up. In our cohort of patients, IOP reductions at 8 months were comparable to Hong et al (initial and repeat SLT, 4.2 and 2.8 mm Hg respectively), however this difference in our series was significant in favor of initial SLT. However, follow-up was much longer in our cohort and we found IOP reductions with repeat SLT to be sustained up to 24 months. We chose to be consistent with previous studies in calculating the percentage of eyes achieving >20% IOP reduction.[10,11,12,13] However in order to better stratify the response, we also calculated eyes achieving >15% IOP reduction. The number of eyes achieving >20% IOP reduction at 8 months was similar after initial SLT (54% in our series vs. 50% in Hong’s), but not with repeat SLT (28% in our series vs. 43% in Hong’s). This trend was similarly noted with eyes achieving >15% reduction (repeat SLT efficacy was lower than initial SLT at all time points (except at 18 months). Upon longer follow-up in our series, we found that a similar percentage of eyes undergoing first and repeat SLT achieved >20% and >15% IOP reduction at the 24 months time point (>20% IOP reduction: 36% and 29%; >15% IOP reduction 54% and 39%, respectively).
Changes in IOP after initial and repeat SLT were comparable, except at 4, 8 and 12 months when the first SLT yielded reductions that were significantly higher. The change in IOP with first SLT ranged between 4.6 and 2.8 mm Hg, and efficacy seemed to gradually diminish up to the 24 months time point. The time to repeat SLT treatment in our series was 26.6 ± 12.2 months which suggests that efficacy mostly waned by 24 months, necessitating repeat treatment. With repeat SLT, IOP reductions ranged between 2.7 and 4.1 mm Hg and were generally lower than the first SLT except at 18 months. Similar to initial SLT, the change in IOP was lowest at the 24 months time point [Table 3]. Thus, although repeat SLT reduced IOP, the reductions were generally lower than first SLT. At 24 months, both first and repeat SLT effects were degraded. This may suggest a similar loss of efficacy, but longer follow-up is needed to determine whether IOP reductions are sustained beyond 24 months.
The current study is limited by its retrospective nature and data was not available for all subjects at all time points. The decision and timing of repeat SLT, and changes in medications were made by treating physicians based on individual patient needs necessary to achieve IOP control. However, there were no significant differences in baseline IOP between first and repeat SLT, or in the number of glaucoma medications throughout the study. This allowed for meaningful comparisons to be made between first and repeat SLT without inherent bias. Our study also did not have a control group that could have been useful to provide further insight into the relationship between repeat SLT and adjunct medical therapy alone. Further studies are required to evaluate this issue.
To date, there are no peer reviewed publications on the long term efficacy of repeat SLT. Follow-up to 24 months allowed us to examine the long term IOP reduction effect of repeat SLT. Of note, slightly higher energy levels were used with repeat SLT (1.08 mJ vs. 0.94 mJ with initial SLT, P < 0.05), although total energy was comparable with repeat and initial SLT (112 vs. 104 mJ respectively, not significant). It is unclear whether higher energy levels were needed to observe champagne bubbles in repeat SLT. Laser energy settings have been found to influence SLT outcomes with higher energy levels associated with higher success in 90° SLT.[14] In comparison, our subjects underwent 360° SLT and received a higher total energy dose than the aforementioned study. The effects of higher energy on the efficacy of repeat SLT are unclear.
Repeat SLT was effective in lowering IOP in this cohort of patients already on medical treatment for glaucoma. IOP reductions were similar to initial SLT treatment and were observed up to 24 months. Although repeat SLT reduced IOP, the reductions were generally milder than initial SLT. At 24 months, the effects of both initial and repeat SLT waned off. Generally, only about one third of eyes achieved IOP reduction >20%. Repeat SLT seems to be a valuable adjunct in patients requiring further IOP reduction. Prospective randomized trials are needed to further characterize the long term efficacy and safety of repeat SLT treatment.
ACKNOWLEDGMENTS
This study was supported in part by Research to Prevent Blindness, New York, The Glaucoma Research and Education Foundation, Inc., New Jersey.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Latina MA, Tumbocon JA. Selective laser trabeculoplasty: A new treatment option for open angle glaucoma. Curr Opin Ophthalmol. 2002;13:94–96. doi: 10.1097/00055735-200204000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Latina MA, Sibayan SA, Shin DH, Noecker RJ, Marcellino G. Q-switched 532-nm Nd: YAG laser trabeculoplasty (selective laser trabeculoplasty): A multicenter, pilot, clinical study. Ophthalmology. 1998;105:2082–2088. doi: 10.1016/S0161-6420(98)91129-0. [DOI] [PubMed] [Google Scholar]
- 3.Katz LJ, Steinmann WC, Kabir A, Molineaux J, Wizov SS, Marcellino G, et al. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: A prospective, randomized trial. J Glaucoma. 2012;21:460–468. doi: 10.1097/IJG.0b013e318218287f. [DOI] [PubMed] [Google Scholar]
- 4.Johnson PB, Katz LJ, Rhee DJ. Selective laser trabeculoplasty: Predictive value of early intraocular pressure measurements for success at 3 months. Br J Ophthalmol. 2006;90:741–743. doi: 10.1136/bjo.2005.086363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lai JS, Chua JK, Tham CC, Lam DS. Five-year follow up of selective laser trabeculoplasty in Chinese eyes. Clin Experiment Ophthalmol. 2004;32:368–372. doi: 10.1111/j.1442-9071.2004.00839.x. [DOI] [PubMed] [Google Scholar]
- 6.Barkana Y, Belkin M. Selective laser trabeculoplasty. Surv Ophthalmol. 2007;52:634–654. doi: 10.1016/j.survophthal.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Latina MA, Park C. Selective targeting of trabecular meshwork cells: In vitro studies of pulsed and CW laser interactions. Exp Eye Res. 1995;60:359–371. doi: 10.1016/s0014-4835(05)80093-4. [DOI] [PubMed] [Google Scholar]
- 8.Kramer TR, Noecker RJ. Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology. 2001;108:773–779. doi: 10.1016/s0161-6420(00)00660-6. [DOI] [PubMed] [Google Scholar]
- 9.Rodrigues MM, Spaeth GL, Donohoo P. Electron microscopy of argon laser therapy in phakic open-angle glaucoma. Ophthalmology. 1982;89:198–210. doi: 10.1016/s0161-6420(82)34806-x. [DOI] [PubMed] [Google Scholar]
- 10.Avery N, Ang GS, Nicholas S, Wells A. Repeatability of primary selective laser trabeculoplasty in patients with primary open-angle glaucoma. Int Ophthalmol. 2013;33:501–506. doi: 10.1007/s10792-013-9729-3. [DOI] [PubMed] [Google Scholar]
- 11.Hong BK, Winer JC, Martone JF, Wand M, Altman B, Shields B. Repeat selective laser trabeculoplasty. J Glaucoma. 2009;18:180–183. doi: 10.1097/IJG.0b013e31817eee0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cvenkel B, Hvala A, Drnovsek-Olup B, Gale N. Acute ultrastructural changes of the trabecular meshwork after selective laser trabeculoplasty and low power argon laser trabeculoplasty. Lasers Surg Med. 2003;33:204–208. doi: 10.1002/lsm.10203. [DOI] [PubMed] [Google Scholar]
- 13.Damji KF, Shah KC, Rock WJ, Bains HS, Hodge WG. Selective laser trabeculoplasty v argon laser trabeculoplasty: A prospective randomised clinical trial. Br J Ophthalmol. 1999;83:718–722. doi: 10.1136/bjo.83.6.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayala M, Chen E. Predictive factors of success in selective laser trabeculoplasty (SLT) treatment. Clin Ophthalmol. 2011;5:573–576. doi: 10.2147/OPTH.S19873. [DOI] [PMC free article] [PubMed] [Google Scholar]


