Abstract
Purpose:
To report a keratoconic eye that developed severe sterile keratitis and corneal scar after collagen crosslinking necessitating corneal transplantation.
Case Report:
A 26-year-old man with progressive keratoconus underwent collagen crosslinking and presented with severe keratitis 72 hours after the procedure. The initial impression was infectious corneal ulcer and a fortified antibiotic regimen was administered. However, the clinical course and confocal microscopy results prompted a diagnosis of sterile keratitis. The eye developed severe corneal scars leading to reduced visual acuity and necessitating corneal transplantation.
Conclusion:
Sterile keratitis may develop after collagen crosslinking resulting in profound visual loss leading to corneal transplantation.
Keywords: Collagen Crosslinking, Keratoconus, Sterile Keratitis
INTRODUCTION
Corneal collagen crosslinking (CXL) with riboflavin is a new treatment modality applied to strengthen the cornea in eyes with progressive keratoconus in which corneal thickness is more than 400 μm.[1] The photoactivated riboflavin enhances corneal strength and integrity by increasing collagen crosslinking and can halt the progression of keratoconus. Moreover, crosslinking has been advocated as a means to treat corneal melt and ulceration.[2]
Although corneal collagen crosslinking represents the first approach to reduce or even stop the progression of keratoconus, several complications including haze,[3] infectious and sterile keratitis,[3,4,5,6] corneal melting,[7] and diffuse lamellar keratitis[8] have been reported.
Herein, we report a patient who developed sterile keratitis and corneal scarring after uneventful collagen crosslinking for keratoconus, necessitating corneal transplantation.
CASE REPORT
A 26-year-old man presented with progressive keratoconus. The patient had no history of contact lens use, allergy, herpetic keratitis, dry eye, or autoimmune disease. Uncorrected visual acuity (UCVA) was 20/60 in his right eye and 20/30 in the left eye. Preoperatively, best spectacle-corrected visual acuity (BSCVA) was 20/20 in the left eye with no improvement in the right eye. Minimum thickness of the cornea was 434 μm in the left eye.
Under strict sterile conditions using topical anesthesia, and following central 9-mm mechanical epithelial debridement, CXL was performed according to the standard method. At the conclusion of the procedure, topical chloramphenicol eye drops were instilled and a bandage soft contact lens was fitted. Postoperatively, chloramphenicol and betamethasone 0.1% eye drops were prescribed every 6 hours.
On postoperative day-1, there was a central area of epithelial defect measuring about 5.0 mm × 5.0 mm and the stroma was clear. The bandage contact lens was in place. Three days after the procedure, the patient came back complaining of redness and low visual acuity. Slit lamp examination revealed diffuse conjunctival injection, a small epithelial defect measuring 3.0 mm × 1.5 mm, and multiple superficial stromal infiltrates in the central cornea. There were no keratic precipitates or anterior chamber reaction [Figure 1]. With a presumptive diagnosis of bacterial ulcer, the contact lens was removed and frequent fortified topical antibiotics consisting of cephalexin (50 mg/ml) and gentamicin (14 mg/ml) were initiated. One day later, when the epithelial defect completely improved, the frequency of topical antibiotics was reduced to every 4 hours and betamethasone 0.1% eye drops were resumed every 12 hours.
Figure 1.
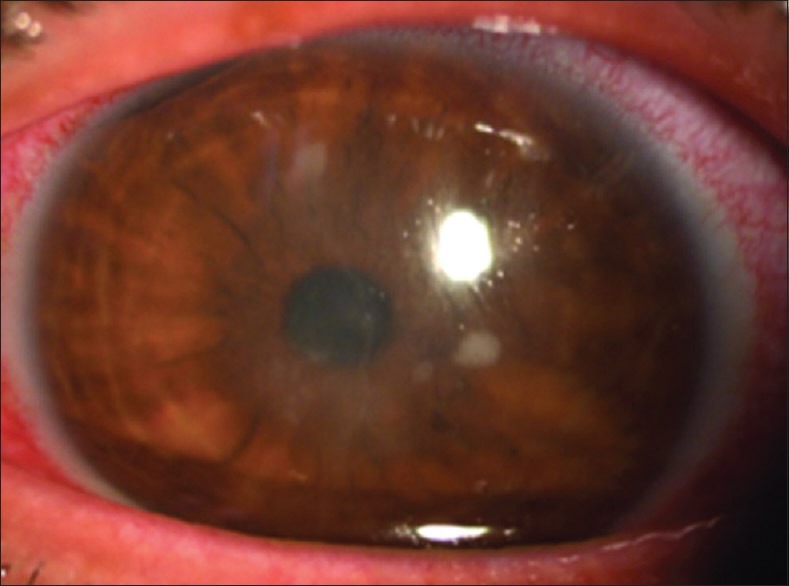
Multiple superficial stromal infiltrates in the central cornea.
On confocal scan, performed on postoperative days 3, multifocal hyperreflective areas with irregular borders and scattered inflammatory cells were observed in the corneal stroma. A couple of high contrast elongated structures measuring about 3 μm in diameter were noted adjacent to the hyperreflective areas, raising a suspicion of fungal keratitis [Figure 2]. However, the clinical course was not compatible with this diagnosis as the stromal infiltration remained stable with no anterior chamber reaction. Therefore, the medications were changed to chloramphenicol eye drops every 6 hours and fluorometholone eye drops every 8 hours, at 7 days after surgery. Thereafter, the infiltrations were gradually replaced with scars leading to an increase in the frequency of the topical steroid and discontinuation of chloramphenicol. Three months later, visual acuity was 20/400 in the left eye and slit lamp examination demonstrated a dense stromal scar overlying the pupil entrance [Figure 3]. At this time point, the patient underwent deep anterior lamellar keratoplasty (DALK) using Anwar's big-bubble technique which yielded a bared Descemet's membrane. Histopathologic examination of the harvested cornea revealed subepithelial bulla and non-specific fibro-inflammatory changes in the anterior stroma where scattered myofibroblast-like cells with plump nuclei, immune reactive for α-SMA (alpha smooth muscle actin) and a few macrophages, immune reactive for CD68 were present. The post-keratoplasty course was uneventful and BSCVA was 20/30 with + 3.50 − 3.50 × 50, 15 months after corneal transplantation.
Figure 2.
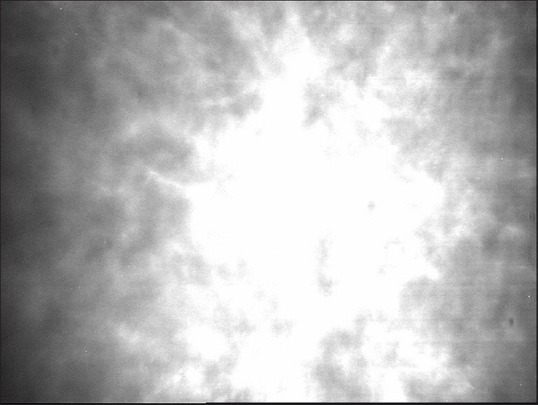
Multifocal hyperreflective areas with irregular borders and scattered inflammatory cells. A couple of high contrast elongated structures measuring about 3 μm in diameter are noted adjacent to the hyperreflective areas.
Figure 3.
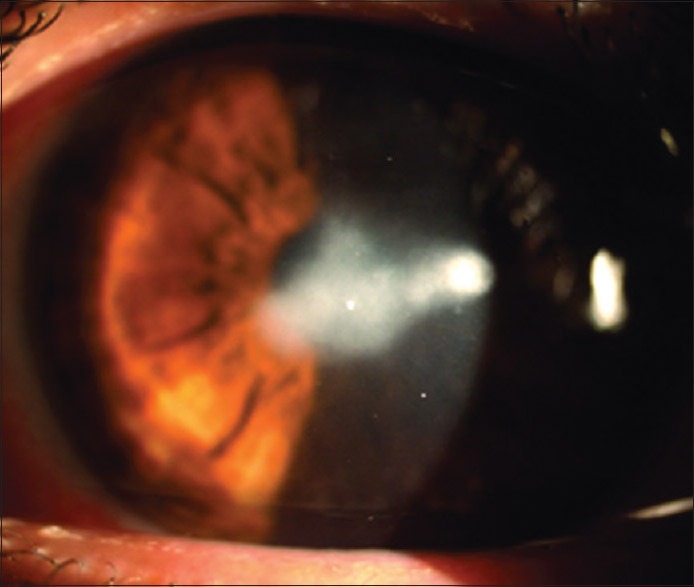
A dense stromal scar obliterating the pupil entrance 3 months after operation.
DISCUSSION
Corneal crosslinking is a safe and effective method for halting keratoconus progression which can avoid or at least delay corneal transplantation.[1,9] However, more experience and longer follow-up are required to ensure its safety. Several case reports and original studies have reported complications ranging from insignificant stromal haze to sight-threatening infectious keratitis and non-infectious corneal melting. Microbial keratitis after CXL occurs rarely. Keratitis following CXL has been reported due to herpes simplex,[10] Acanthamoeba,[11] and a number of bacteria such as Escherichia coli, and staphylococcus and streptococcus species.[5,6,12] Kymionis et al[10] report a case of herpes keratitis with iritis and suggest that UVA light could be a potent stimulus to trigger/induce reactivation of latent herpes simplex infection. Infection due to Acanthamoeba had a fulminating course and a full-thickness keratoplasty was needed to control the infection as well as for visual rehabilitation.[11]
Sharma et al[13] reported a case of Pseudomonas aeruginosa keratitis that developed 3 days following CXL and considered the presence of an epithelial defect, use of a soft bandage contact lens, and topical corticosteroids in the immediate postoperative period as risk factors.
In the case reported herein, the initial impression was bacterial keratitis and a fortified antibacterial regimen was started. One limitation in this report is that smear and culture were not taken, so the possibility of infectious kertitis cannot be excluded with certainty. However, the clinical course including the absence of pain, keratic precipitates and anterior chamber reaction, and also rapid improvement of the epithelial defect convinced us that an immune response should be considered.
Several mechanisms have been proposed for keratitis after collagen crosslinking. One mechanism is infectious etiologies such as herpes simplex virus,[10] Escherichia coli, Staphylococcus epidermidis, and Staphylococcus salivarius.[5,6,12] One proposed mechanism is an immunologic reaction which can cause sterile corneal infiltrates.[3,8,14,15] Reporting a large series of keratoconic patients undergoing collagen crosslinking, Koller et al[3] noted sterile infiltrates in 7.6% of eyes which resolved over 4 weeks with no significant reduction in corrected visual acuity.
Koppen et al[15] reported four cases of stromal scarring following keratitis in a series comprising of 117 patients. This complication led to a decrease the final visual acuity. The UVA/riboflavin complex can evoke an exaggerated immunologic response to stromal antigens or other substances such as bandage contact lenses. The immunologic reaction after collagen crosslinking was observed by Kymionis et al[8] who reported a case of diffuse lamellar keratitis after collagen crosslinking in a patient with postoperative LASIK ectasia. Supporting this speculation, inflammatory cells were observed on histopathologic sections of the corneal button harvested from our case as well as from another patient undergoing penetrating keratoplasty due to acute corneal melt with perforation after CXL.[7]
Confocal scan has been found to be a sensitive and specific tool for the diagnosis of microbial keratitis.[16] However, the results of the current report indicate that findings by confocal scan might be inaccurate to differentiate filamentous fungi from apoptotic keratocytes and newly synthesized collagen.[17] Difficulty in distinguishing altered host cells and extracellular matrix from pathogenic organisms limits the value of confocal microscopy as a stand-alone tool in diagnosing microbial keratitis after collagen crosslinking.
Whatever the underlying cause of sterile keratitis following CXL is, it seems that the healing response is more exaggerated after collagen crosslinking as the cornea in our patient developed dense central stromal scarring. Such scars after CXL-induced keratitis have also been reported by other authors.[14,15] Immediately after collagen crosslinking, the anterior stroma is depleted from keratocytes. This stage is followed by gradual repopulation by keratocytes which synthesize new collagen fibers, resulting in an increase in the density of the extracellular matrix. These activated keratocytes can produce large amounts of extracellular matrix and transform to myofibroblast in response to keratitis which explain why dense scars developed in this case.
Since our patient was dissatisfied with the results of the intervention, we decided to proceed to corneal transplantation after 3 months. Structural changes after CXL are confined to the anterior and middle stroma, leaving posterior stroma and endothelium intact. Therefore, deep anterior lamellar keratoplasty using Anwar's big-bubble technique can be performed with ease after CXL which was the case in our patient who achieved BSCVA of 20/25 after keratoplasty.
In summary, sterile keratitis can develop after CXL leaving a hypertrophic scar and leading to profound visual loss necessitating corneal transplantation. This report also implies that confocal scan might not be a reliable tool to diagnose the etiology of keratitis after CXL. Our limited experience indicates DALK using Anwar's big-bubble technique can be performed with ease in such cases.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 2.Spoerl E, Wollensak G, Seiler T. Increased resistance of crosslinked cornea against enzymatic digestion. Curr Eye Res. 2004;29:35–40. doi: 10.1080/02713680490513182. [DOI] [PubMed] [Google Scholar]
- 3.Koller T, Mrochen M, Seiler T. Complication and failure rates after corneal crosslinking. J Cataract Refract Surg. 2009;35:1358–1362. doi: 10.1016/j.jcrs.2009.03.035. [DOI] [PubMed] [Google Scholar]
- 4.Angunawela RI, Arnalich-Montiel F, Allan BD. Peripheral sterile corneal infiltrates and melting after collagen crosslinking for keratoconus. J Cataract Refract Surg. 2009;35:606–607. doi: 10.1016/j.jcrs.2008.11.050. [DOI] [PubMed] [Google Scholar]
- 5.Pérez-Santonja JJ, Artola A, Javaloy J, Alió JL, Abad JL. Microbial keratitis after corneal collagen crosslinking. J Cataract Refract Surg. 2009;35:1138–1140. doi: 10.1016/j.jcrs.2009.01.036. [DOI] [PubMed] [Google Scholar]
- 6.Zamora KV, Males JJ. Polymicrobial keratitis after a collagen cross-linking procedure with postoperative use of a contact lens: A case report. Cornea. 2009;28:474–476. doi: 10.1097/ICO.0b013e31818d381a. [DOI] [PubMed] [Google Scholar]
- 7.Gokhale NS, Vemuganti GK. Diclofenac-induced acute corneal melt after collagen crosslinking for keratoconus. Cornea. 2010;29:117–119. doi: 10.1097/ICO.0b013e3181a06c31. [DOI] [PubMed] [Google Scholar]
- 8.Kymionis GD, Bouzoukis DI, Diakonis VF, Portaliou DM, Pallikaris AI, Yoo SH. Diffuse lamellar keratitis after corneal crosslinking in a patient with post-laser in situ keratomileusis corneal ectasia. J Cataract Refract Surg. 2007;33:2135–2137. doi: 10.1016/j.jcrs.2007.06.070. [DOI] [PubMed] [Google Scholar]
- 9.Caporossi A, Baiocchi S, Mazzotta C, Traversi C, Caporossi T. Parasurgical therapy for keratoconus by riboflavin-ultraviolet type A rays induced cross-linking of corneal collagen: Preliminary refractive results in an Italian study. J Cataract Refract Surg. 2006;32:837–845. doi: 10.1016/j.jcrs.2006.01.091. [DOI] [PubMed] [Google Scholar]
- 10.Kymionis GD, Portaliou DM, Bouzoukis DI, Suh LH, Pallikaris AI, Markomanolakis M, et al. Herpetic keratitis with iritis after corneal crosslinking with riboflavin and ultraviolet A for keratoconus. J Cataract Refract Surg. 2007;33:1982–1984. doi: 10.1016/j.jcrs.2007.06.036. [DOI] [PubMed] [Google Scholar]
- 11.Rama P, Di Matteo F, Matuska S, Paganoni G, Spinelli A. Acanthamoeba keratitis with perforation after corneal crosslinking and bandage contact lens use. J Cataract Refract Surg. 2009;35:788–791. doi: 10.1016/j.jcrs.2008.09.035. [DOI] [PubMed] [Google Scholar]
- 12.Pollhammer M, Cursiefen C. Bacterial keratitis early after corneal crosslinking with riboflavin and ultraviolet-A. J Cataract Refract Surg. 2009;35:588–589. doi: 10.1016/j.jcrs.2008.09.029. [DOI] [PubMed] [Google Scholar]
- 13.Sharma N, Maharana P, Singh G, Titiyal JS. Pseudomonas keratitis after collagen crosslinking for keratoconus: Case report and review of literature. J Cataract Refract Surg. 2010;36:517–520. doi: 10.1016/j.jcrs.2009.08.041. [DOI] [PubMed] [Google Scholar]
- 14.Rodríguez-Ausín P, Gutiérrez-Ortega R, Arance-Gil A, Romero-Jimenez M, Fuentes-Páez G. Keratopathy after cross-linking for keratoconus. Cornea. 2011;30:1051–1053. doi: 10.1097/ICO.0b013e3182096789. [DOI] [PubMed] [Google Scholar]
- 15.Koppen C, Vryghem JC, Gobin L, Tassignon MJ. Keratitis and corneal scarring after UVA/riboflavin cross-linking for keratoconus. J Refract Surg. 2009;25:S819–S823. doi: 10.3928/1081597X-20090813-11. [DOI] [PubMed] [Google Scholar]
- 16.Kanavi MR, Javadi M, Yazdani S, Mirdehghanm S. Sensitivity and specificity of confocal scan in the diagnosis of infectious keratitis. Cornea. 2007;26:782–786. doi: 10.1097/ICO.0b013e318064582d. [DOI] [PubMed] [Google Scholar]
- 17.Mazzotta C, Traversi C, Baiocchi S, Caporossi O, Bovone C, Sparano MC, et al. Corneal healing after riboflavin ultraviolet-A collagen cross-linking determined by confocal laser scanning microscopy in vivo: Early and late modifications. Am J Ophthalmol. 2008;146:527–533. doi: 10.1016/j.ajo.2008.05.042. [DOI] [PubMed] [Google Scholar]


