Abstract
Background:
Demand for ICU beds is exceeding its supply. Since the sources are limited in some centers, it is necessary to design a model to identify the patients who benefit more from ICU beds.
Objectives:
The present study aimed to develop a model to prioritize adult patients according to their clinical indications by a three rounded Delphi method study.
Patients and Methods:
In this study, 22 physicians who practiced in a source limited hospital in southern Iran were invited to participate in a three phase Delphi survey.
Results:
At first, the panelists recommended 30 indications. The indications in the first checklist plus those obtained by literature review formed the second checklist which contained 36 items. The items were scored from 0 to 10 by the panelists. According to the scores, the indications were categorized into three priority levels, which were confirmed by the panelists in the third round.
Conclusions:
This simple checklist contains the indications for ICU admission categorized into three priority levels. This checklist can be considered as a guide for physicians who practice in hospitals with limited number of ICU beds.
Keywords: Intensive Care Unit, Delphi, Prioritizing
1. Background
The number of the Intensive Care Unit (ICU) beds has been increasing all over the world, but it seems that demands for them exceed the supply (1-3). On the other hand, as the ICU technology becomes more advanced, its costs rise, as well (4-6). Since sources are limited, it is crucial to design a model for ICU admission. In spite of the importance of this issue, few studies have been focused on decision making for ICU admission. Generally, decision making for ICU admission is based on identifying the patients who benefit more from ICU and rejection of those who are too well or too bad to benefit from the unit (7, 8). Today, there are few guidelines which have identified all the indications for ICU admission of the patients (9, 10); however, they are not always useful in practice. In some hospitals, especially in developing countries where sources are limited, it is not possible to follow such guidelines (11, 12). Thus, decision making for ICU admission is performed according to the physicians' opinions rather than a standardized guideline (13). Therefore, it seems that designing a model which ranks the indications for ICU admission according to their importance could be useful in prioritizing the candidates for ICU admission. Delphi method is a forecasting method used to reach consensus by asking some experts to respond to questionnaires in several rounds (14).
2. Objectives
The present study aims to identify the indications in adult patients for decision making about ICU admission and rank them regarding their importance by using Delphi process for consensus building.
3. Patients and Methods
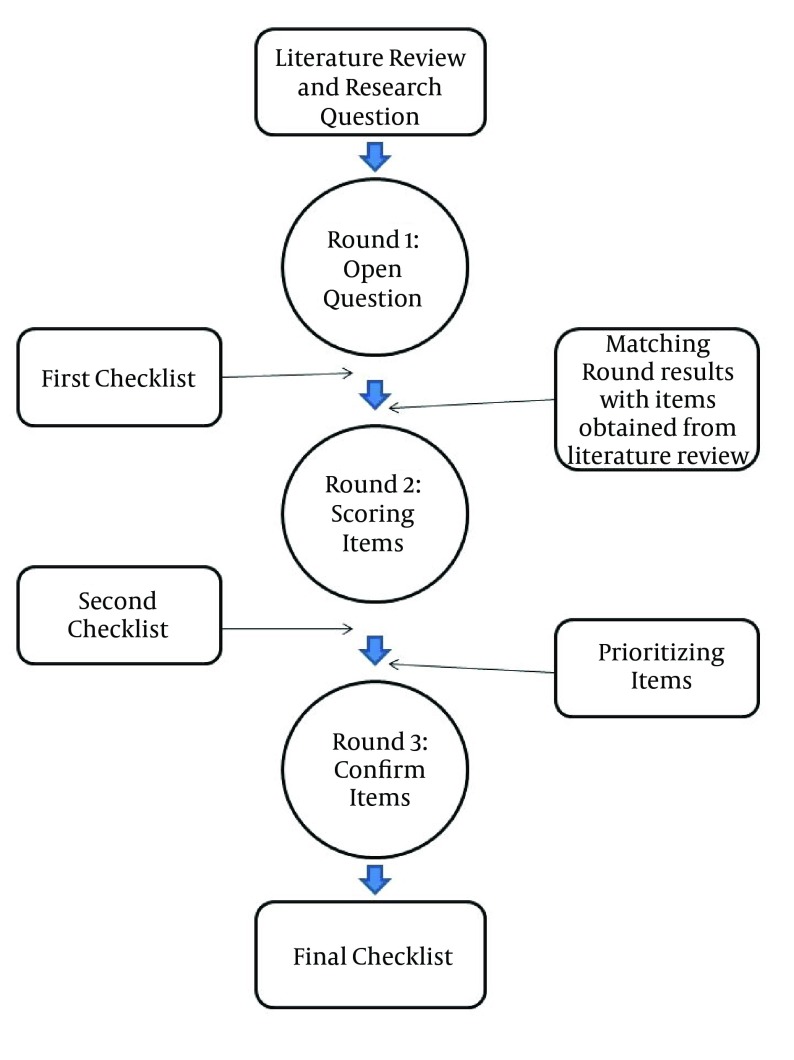
We performed a 3-phase Delphi process in the present study. The panelists' responses (in anonymous forms) regarding the scoring of different indications for decision making about ICU admission were collected at a specific time and then disseminated back to the panel. A summary of our Delphi steps is illustrated in Figure 1.
Figure 1. Schematic of the Steps of the Present 3-Rounded Delphi Study.
In this study, four intensivists served as the steering committee. The role of the steering committee was reviewing the literature, identifying the study methodology, designing the initial questions, disseminating them to the panel, reviewing the feedbacks, and performing further steps of the Delphi process. Nonetheless, they did not take part in answering the questions in the panel.
The present study aimed to design a model to recommend a checklist to help the physicians in decision making for referring the patients to ICU in case the number of the ICU beds is limited and also to prioritize the patients who benefit more from the intensive care services. The study protocol was approved by Ethics Committee of Shiraz University of Medical Sciences with Code of Ethics of "5349".
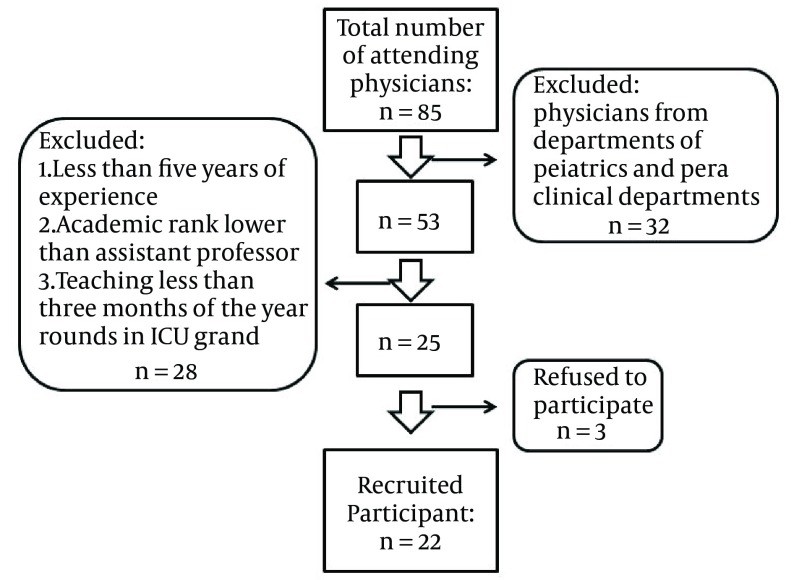
Moreover, 22 specialists served as the Delphi panelists. The flowchart of recruiting participants is illustrated in Figure 2. The physicians from departments of pediatrics and para clinical departments such as pathologists, radiologists, and physical therapy and rehabilitation physicians were excluded. Physicians with following criteria were invited for participation:
Figure 2. Expert Recruitment Flowchart.
Have over five years of experience as attending physician
Attending physicians with at an Academic rank of assistant professor or more
Teaching at least three months of the year in ICU grand rounds
Twenty five physicians were invited to participate, and 22 joined this study. However three physicians rejected to participate in the study because they were too busy. The panel of experts was formed by inviting the physicians with different specialties, including 5 intensivists, 5 cardiologists, 4 neurologists, 4 pulmonologists, and 4 surgeons.
These experts were selected from the physicians who were responsible for referring the patients to ICUs in the hospitals affiliated to Shiraz University of Medical Sciences. These hospitals were in fact selected due to their high workload. Thus, the panelists were experienced in managing ICU admission while the ICU beds are not sufficient.
Literature review was performed by the steering committee members and all the clinical signs mentioned as the indications for ICU admission in the literature were gathered.
One of the steering committee members explained the goal of the study to all 22 participants, individually, by face-to-face visit. In each step, participants asked to complete a questionnaire in one week. The questionnaires in each step contained both an explanation about the study and a question to answer. In the first round of our Delphi study, the panelists were asked to write the indications they used for making decision about referring the patients to ICU. After collecting the panelists' responses, a checklist of clinical signs was designed from all the indications for ICU admission of the patients and was disseminated back to the panel. The second checklist was obtained from the panelists' responses in the first round in addition to the items obtained through literature review by the steering committee. In the second round, the panel was requested to assign a score of 0-10 to each item according to its importance in decision making for ICU referring and prioritization. After the responses from the second round were collected, the indications for ICU admission were prioritized according to their mean scores. Finally, the third checklist was designed by categorizing the indications into three groups based on their mean scores and importance.
4. Results
All the participants completed the first round of the study. According to the panelists' responses, 31 items were identified. The identified items were gathered as an initial checklist of the indications for referring the adult patients to ICU. Then, according to the results of the literature review, 5 extra indications for ICU admission which were not included in the initial checklist were added to form the second checklist. These indications were urine output monitoring, blood sugar > 250 or < 70, BUN > 60, Na > 150 or < 130, and K > 6 or < 3. The second checklist contained 36 items (Table 1). In the second round, the panelists assigned a score of 0-10 to each of the 36 items. The mean scores of the panelists' responses are shown in Table 1. Then, according to the mean scores of the responses and opinions of the two intensivists (steering committee members), the indications were categorized into three groups. In the third round, all the panelists confirmed the ranking and categorization of the indications. The critical indications included ventilatory support, irregular or gasping breathing patterns, Cardiopulmonary resuscitation, Intracranial pressure monitoring, systolic pressure > 170 or < 90, diastolic pressure > 110 or < 50, requiring ICU-level nursing care, asymmetric pupils, intra-aortic balloon pump, and continuous seizures. The following 10 indications were also categorized as important indications: pH > 7.7 or < 7.1, endotracheal intubation, inotropic infusion therapy, defibrillation, K > 6 or < 3, Glasgow coma scale < 13, lateralizing signs, SaO2 < 90, respiratory rate > 35, and heart rate > 120. The remaining indications of ICU admission were categorized as other indications.
Table 1. The Final Checklist Items, the Mean Score of Each Indication, and Categorization of Indications.
| Variables | Values |
|---|---|
| Critical indications | |
| Ventilatory support | 8.72 |
| Irregular or gasping breathing patterns | 8.63 |
| Cardiopulmonary resuscitation | 8.36 |
| Intracranial pressure monitoring | 8.31 |
| Sys pressure > 170 or < 90 | 8.31 |
| Dia pressure > 110 or < 50 | 8.31 |
| requiring ICU-level nursing care | 8 |
| Asymmetric pupils | 7.90 |
| Intra-aortic Balloon pump | 7.81 |
| Continuous seizures | 7.77 |
| Important indications | |
| pH > 7.7 or < 7.1 | 7.68 |
| Endotracheal intubation | 7.54 |
| Inotropic infusion therapy | 7.22 |
| Defibrillation | 6.13 |
| K > 6 or < 3 | 5.77 |
| Glasgow coma scale < 13 | 5.72 |
| Lateralizing signs | 5.68 |
| Sa O2 < 90 | 5.63 |
| Respiratory Rate > 35 | 5.50 |
| Heart Rate > 120 | 5.50 |
| Other indications | |
| Na > 150 or < 130 | 5.45 |
| Blood Transfusion > 4 PRBCs /day a | 5.13 |
| Serum Creatinine Level > 3 | 4.90 |
| Pa O2 < 50 with FiO2 > 60% | 4.68 |
| Fluid therapy > 5 L/d | 4.18 |
| ECG monitoring | 4.13 |
| Pace Maker | 3.86 |
| Dialysis | 3.77 |
| Fever with positive blood culture test | 3.40 |
| BUN > 60 | 3.27 |
| Ca > 10 or < 6.5 | 3.18 |
| Emergency Angiography | 3.04 |
| Blood sugar > 250 or < 70 | 2.72 |
| Central line | 2.63 |
| P CO2 > 60 | 2.63 |
| Urine Output Monitoring | 02 |
a Is Blood transfusion of > 4 units of packed red blood cells.
5. Discussion
Although there are some guidelines for identifying the indications for ICU admission, none of them is suitable for the centers with a limited number of ICU beds (15). Moreover, the present study checklist is the first one which is able to prioritize the candidates for ICU admission. This study used Delphi method as a structured method of consensus building to develop a checklist for identification and prioritization of the candidates for ICU admission. The present checklist contains 36 indications for referring the patients to ICU. This means that the patients with any of these indications should be referred to ICU.
In the present study, the indications were scored, ranked, and prioritized. Then, they were categorized into three groups of critical indications, important indications, and other indications for ICU admission. These indications were obtained from literature review and were confirmed by the physicians with different specialties. We collected the indications from both panelists' opinions and literature review in order to increase the sensitivity of the items selection and avoid missing any probable indication. The current criteria for ICU admission are based on identifying the patients who benefit more from ICU beds which is performed by rejecting those who are too well or too sick to benefit from intensive cares. Up to now, some models have been developed as assessment instruments for evaluating the patients' conditions and their prognosis (16-18). However, these predictive tools are mostly applied to the patients who have been admitted to ICU and have not been tested as preadmission screening instruments. Moreover, few studies have been conducted on designing a model for ICU admission. In a review of guidelines for ICU admission, discharge, and triage, all the indications for ICU admission were collected and identified thoroughly (9). That study included a diagnosis model (uses specific conditions or diseases) and an objective parameter model (uses various clinical and laboratorial signs) to determine the appropriateness of ICU admission. Also, it defined 4 levels of priority for the candidates of ICU admission from the patients who would benefit most (priority 1) to those who would not benefit at all (Priority 4) from ICU. However, that model was not designed as a checklist and it was a little complicated to be used as a guideline in practice. Furthermore, although that study defined 4 levels of priority for the patients to be admitted to ICU, it did not prioritize the indications. In other words, according to this system, all the indications were considered to have similar values in identifying the candidates of ICU admission. In another study, a model was designed to identify the patients who might not need ICU admission (19). Unlike ours, that study was conducted in a setting where the admission rate was higher than the demand. Hence, these studies and guidelines may be useful in the hospitals where the demands for ICU beds do not exceed the supply. In the centers with a limited number of ICU beds, however, prioritization of the candidates for ICU admission is necessary (12).
In this study, we invited the physicians from different specialties. Also, we chose the physicians who were experienced in managing limited facilities from the hospitals with high workloads and a limited number of ICU beds (20, 21). Yet, the main limitation of our study was the selection of the panel participants which was not properly geographically distributed and was limited to the physicians of the hospitals located in south west of Iran (22). And we may not be able to generalize it to all other similar settings. Furthermore, present model is only suggested for adult patients and not applicable for children patients. Also, similar to other qualitative studies, the present study has its own limitations and quantitative studies are required to be conducted on the issue. To the best of our knowledge, this is the first study which has prioritized the indications for ICU admission.
Present model for ICU admission is obtained by consensus among the experts who are experienced in managing patients in hospitals with limited number of ICU beds. This model can be useful for conducting further studies and designing guidelines.
Acknowledgments
The authors would like to thank Mrs. Sareh Roosta at the Center for Development of Clinical Research of Nemazee Hospital for her assistance in statistical analysis of the data. They are also grateful for Ms. A. Keivanshekouh at the Research Improvement Center of Shiraz University of Medical Sciences for improving the use of English in the manuscript.
Footnotes
Authors’ Contributions:Study concept and design: Behzad Maghsoudi and Seyed Hesamodin Tabei. Analysis and interpretation of data: Behzad Maghsoudi, Seyed Hesamodin Tabei, and Hamidreza Tabatabaee, Farid Zand. Drafting of the manuscript: Seyed Hesamodin Tabei, Armin Akbarzadeh, and Farid Zand, Critical revision of the manuscript for important intellectual content: Behzad Maghsoudi, Seyed Hesamodin Tabei, Farid Zand, Hamidreza Tabatabaee, and Armin Akbarzadeh. Statistical analysis: Hamidreza Tabatabaee and Armin Akbarzadeh.
References
- 1.Garrouste-Orgeas M, Montuclard L, Timsit JF, Reignier J, Desmettre T, Karoubi P, et al. Predictors of intensive care unit refusal in French intensive care units: a multiple-center study. Crit Care Med. 2005;33(4):750–5. doi: 10.1097/01.ccm.0000157752.26180.f1. [DOI] [PubMed] [Google Scholar]
- 2.Adhikari NK, Rubenfeld GD. Worldwide demand for critical care. Curr Opin Crit Care. 2011;17(6):620–5. doi: 10.1097/MCC.0b013e32834cd39c. [DOI] [PubMed] [Google Scholar]
- 3.Mullins PM, Goyal M, Pines JM. National growth in intensive care unit admissions from emergency departments in the United States from 2002 to 2009. Acad Emerg Med. 2013;20(5):479–86. doi: 10.1111/acem.12134. [DOI] [PubMed] [Google Scholar]
- 4.Halpern NA, Pastores SM. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38(1):65–71. doi: 10.1097/CCM.0b013e3181b090d0. [DOI] [PubMed] [Google Scholar]
- 5.Iapichino G, Corbella D, Minelli C, Mills GH, Artigas A, Edbooke DL, et al. Reasons for refusal of admission to intensive care and impact on mortality. Intensive Care Med. 2010;36(10):1772–9. doi: 10.1007/s00134-010-1933-2. [DOI] [PubMed] [Google Scholar]
- 6.Vanhecke TE, Gandhi M, McCullough PA, Lazar MH, Ravikrishnan KP, Kadaj P, et al. Outcomes of patients considered for, but not admitted to, the intensive care unit. Crit Care Med. 2008;36(3):812–7. doi: 10.1097/CCM.0B013E318165FAC7. [DOI] [PubMed] [Google Scholar]
- 7.Louriz M, Abidi K, Akkaoui M, Madani N, Chater K, Belayachi J, et al. Determinants and outcomes associated with decisions to deny or to delay intensive care unit admission in Morocco. Intensive Care Med. 2012;38(5):830–7. doi: 10.1007/s00134-012-2517-0. [DOI] [PubMed] [Google Scholar]
- 8.Joynt GM, Gomersall CD, Tan P, Lee A, Cheng CA, Wong EL. Prospective evaluation of patients refused admission to an intensive care unit: triage, futility and outcome. Intensive Care Med. 2001;27(9):1459–65. doi: 10.1007/s001340101041. [DOI] [PubMed] [Google Scholar]
- 9.Egol A, Fromm R, Guntupalli KK, Fitzpatrick M, Kaufman D, Nasraway S. Guidelines for intensive care unit admission, discharge, and triage. Critic Medic J. 1999;27(3):633–8. doi: 10.1097/00003246-199903000-00048. [DOI] [PubMed] [Google Scholar]
- 10.Sprung CL, Danis M, Iapichino G, Artigas A, Kesecioglu J, Moreno R, et al. Triage of intensive care patients: identifying agreement and controversy. Intensive Care Med. 2013;39(11):1916–24. doi: 10.1007/s00134-013-3033-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chalya PL, Gilyoma JM, Dass RM, McHembe MD, Matasha M, Mabula JB, et al. Trauma admissions to the intensive care unit at a reference hospital in Northwestern Tanzania. Scand J Trauma Resusc Emerg Med. 2011;19:61. doi: 10.1186/1757-7241-19-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mery E, Kahn JM. Does space make waste? The influence of ICU bed capacity on admission decisions. Crit Care. 2013;17(3):315. doi: 10.1186/cc12688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet. 2010;376(9749):1339–46. doi: 10.1016/S0140-6736(10)60446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang X, Gao Z, Guo H. Delphi method for estimating uncertainty distributions. Inter Interdiscipl J. 2012;15(2):449–60. [Google Scholar]
- 15.Segura V, Reyes N, Tejada M, Zolano E. Mortality and priority level for ICU admission in the setting of limited critical care beds in El Salvador. Critical Care J. 2012;16(1):P384. [Google Scholar]
- 16.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29. [PubMed] [Google Scholar]
- 17.Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–36. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 18.Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today's critically ill patients. Crit Care Med. 2006;34(5):1297–310. doi: 10.1097/01.CCM.0000215112.84523.F0. [DOI] [PubMed] [Google Scholar]
- 19.Zimmerman JE, Kramer AA. A model for identifying patients who may not need intensive care unit admission. J Crit Care. 2010;25(2):205–13. doi: 10.1016/j.jcrc.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 20.Paydar S, Shokrollahi S, Jahanabadi S, Ghaffarpasand F, Malekmohammadi Z, Akbarzadeh A. Emergency Operating Room Workload Pattern: A Single Center Experience from Southern Iran. Emer Trauma. 2013;1(1):38–42. [PMC free article] [PubMed] [Google Scholar]
- 21.Paydar S, Parsijani PJ, Akbarzadeh A, Manafi A, Ghaffarpasand F, Abbasi HR. Short-term Outcome of Open Appendectomy in Southern Iran: A Single Center Experience. Emer Trauma. 2013;1(3):123–6. [PMC free article] [PubMed] [Google Scholar]
- 22.Welty G. Communications. PROBLEMS OF SELECTING EXPERTS FOR DELPHI EXERCISES. Academic Manag J. 1972;15(1):121–4. doi: 10.2307/254805. [DOI] [Google Scholar]