Abstract
The authors examined the relationship between global sleep quality and alcohol risk, including the extent to which global sleep quality moderated the relationship between alcohol use and drinking-related consequences. Global sleep quality was measured using the Pittsburgh Sleep Quality Index (PSQI) and alcohol-related consequences were assessed using the Rutgers Alcohol Problem Index (RAPI). The sample consisted of 261 college students (61.3% female, 58.2% Caucasian) who completed online surveys. Using a four-step hierarchical multiple regression model, global sleep quality was found to predict alcohol consequences, over and above assessed covariates (demographics and weekly drinking). Further, global sleep quality emerged as a strong moderator in the drinking-consequences relationship such that among heavier drinkers, those with poorer global sleep quality experienced significantly greater alcohol-related harm. Campus health education and alcohol interventions may be adapted to address the importance of maintaining a healthy lifestyle, both in terms of healthful sleeping and drinking behaviors, which appear to play a strong synergistic role in alcohol-related risk.
Keywords: Alcohol, Sleep, College students, Health education
1. Introduction
Heavy drinking among college students persists as a serious social, academic, and health concern, with students experiencing a variety of alcohol-related academic, legal, physical, sexual, and social consequences (Dowdall, 2009; Hingson, Heeren, Winter, & Wechsler, 2005; Hingson, Zha, &Weitzman, 2009; Perkins, 2002). Despite growing public awareness and the initiation of significant prevention and intervention efforts aimed at reducing problematic drinking, prevalence rates of high-risk drinking and related consequences have remained relatively stable since 1993 (Hingson et al., 2009; Johnston, O'Malley, Bachman, & Schulenberg, 2007; Nelson, Xuan, Lee, Weitzman, &Wechsler, 2009). Understandably then, researchers continually seek to identify and understand correlates and predictors of risky alcohol use and associated negative consequences. Further, over a decade ago, the National Institutes of Health recognized emerging adults (18–25 year olds) as a population increasingly susceptible to sleepiness and its associated consequences (National Institutes of Health, 1997). While some efforts have been made to understand the extent to which a relationship exists between these health-risk behaviors (alcohol use and sleep) in college populations, surprisingly few conclusions have been reached.
1.1. Sleep quality in college students
The lack of quality sleep among college students has been steadily increasing over time (Wolfson, 2010), with approximately half of college students reporting insufficient sleep, irregular sleep or other sleep difficulties (Buboltz et al., 2006; Tsai & Li, 2004) and 27% categorized as meeting the threshold for an undiagnosed sleep disorder (e.g., narcolepsy, insomnia, restless leg syndrome, sleep apnea; Gaultney, 2010). In fact, in a 2010 study of 1125 college students, over 60% were classified as poor-quality sleepers (Lund, Reider, Whiting, & Prichard, 2010). In addition, national surveys of undergraduates have shown a steady decline in median hours of sleep reported, from 7.75 in 1969 to 6.65 in 2001, with first- and second-year students reporting less time in bed because of earlier wake times and more erratic sleep-wake schedules (Hicks, Fernandez, & Pellegrini, 2001; Singleton & Wolfson, 2009; Tsai & Li, 2004). Indeed, sleep habits are one of the first daily habits to change for first-year college students (Pilcher, Ginter, & Sadowsky, 1997). The first two years of college represent an important developmental transition accompanied by a host of challenges (e.g., greater autonomy and control over free time, residence hall living, emotional and academic stress), which may contribute to irregular sleep schedules, sleep disruption, and sleep deprivation. Sleep deprivation, in turn, is associated with driving accidents (Marcus & Loughlin, 1996), major mood problems such as depression (Brooks, Girgenti, & Mills, 2009), and poor academic performance (Gaultney, 2010; Pilcher &Walters, 1997).
1.2. Sleep quality, alcohol use, and risk-taking behaviors
Heightening the concern over high prevalence rates of sleep problems and alcohol use on college campuses is the likely risk associated with co-morbid sleep–alcohol problems. For example, the use of alcohol reduces sleep latency (i.e., the amount of time it takes to fall asleep), which encourages those with insomnia, including adolescents, to use alcohol as a sedative (Johnson & Breslau, 2001; Roane & Taylor, 2008; Roehrs & Roth, 2001). In fact, in a recent study of 1039 undergraduates, 11.36% of non-abstainers reported using alcohol as a sleep aid in the past week (Taylor & Bramoweth, 2010). Risks associated with alcohol-induced sleep include the need for higher doses of alcohol as individuals build up tolerance; deficient fragmented sleep, resulting in less sleep (Galambos, Dalton, & Maggs, 2009); and poor quality sleep as defined by irregularities in REM (Rapid Eye Movement; Roehrs & Roth, 2001). Given the consistent link between alcohol use and sleep problems, high rates of alcohol misuse and poor sleep quality in college populations, and negative consequences associated with each independently, research is needed to explore their possible additive influence on behavioral health outcomes among college students.
In a large study of adolescents, individuals reporting higher levels of sleep problems also reported higher levels of risk-taking behaviors (O'Brien & Mindell, 2005; Taylor & Bramoweth, 2010). Moreover, rates of risk-taking behaviors and sleep problems increased incrementally from 9th to 12th grade. Because risky and excessive alcohol consumption (Grekin & Sher, 2006; Thompson, Leinfelt, & Smyth, 2006) and sleep problems (Tsai & Li, 2004) are common in college populations, college students may be especially susceptible to the negative consequences resulting from the interactive effects of poorer sleep and alcohol use. Although much attention has been drawn to negative alcohol-related consequences among college students and their impact on personal and communal health risk, less is known of the role sleep may play in exacerbating collegiate drinking and consequences.
1.3. Current study and hypotheses
The current study sought to explore the relationship between global sleep quality, alcohol use, and alcohol consequences among a sample of primarily first- and second-year college students. Global sleep quality assessed seven indicators of sleep (dys) function: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction using the Pittsburg Sleep Quality Index (PSQI; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989). Global sleep quality was expected to be associated with riskier drinking behaviors, such as heavy episodic drinking (i.e., 4/5+ drinks within two-hour period for women/men). Consistent with previous research, alcohol use was expected to predict negative alcohol-related consequences. Given the established link between sleep problems and risk-taking behaviors, poorer global sleep quality was predicted to be associated with alcohol consequences, even after controlling for the effects of alcohol use itself. Finally, the relationship between alcohol use and consequences was expected to be strongest among individuals who reported poorer global sleep quality.
2. Materials and methods
2.1. Participants and procedures
Across the Academic Year 2009–2010, 261 students from a private, mid-size university on the West Coast completed online surveys for class credit as part of the psychology subject pool. Participants had a mean age of 19.02 years (SD=1.53), and were primarily first-year (58.8%) and second-year (29.1%) students. In addition, 61.3% were female and 58.2% were Caucasian. Over one-third of participants were affiliated with Greek houses: 20.8% were current members of, and 16.9% intended to pledge, a fraternity or sorority. The majority of sample participants (82.4%) lived in on-campus residential housing, while the remaining participants lived off-campus: 6.1% with roommate(s), 8.4% with family, 2.7% alone, and .4% in a fraternity/sorority house.
Students in introductory psychology courses were presented with several studies in which to participate. Students choosing to participate in the current study were sent an email containing a study description as well as a link by which to access the 30-minute IRB-approved confidential online survey. Upon submitting their electronic consent on the opening screen, the students were taken to their online surveys. Before answering questions related to drinking behavior, a standard drink was defined as a drink containing one-half ounce of ethyl alcohol — one 12 oz. beer, one 4 oz. glass of wine, or one 1.25 oz. shot of 80 Proof liquor. Pictures of standard drinks accompanied these descriptions.
2.2. Measures
Measures appropriate to the current study included sex, age, race, Greek affiliation (i.e., intent to pledge or current membership in a fraternity or sorority), alcohol use, global sleep quality, and alcohol-related negative consequences.
2.2.1. Global sleep quality
Participants completed the 19-item Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989). The PSQI assesses past month sleep (dys) function using seven subcomponents: sleep duration (average number of hours of actual sleep per night), sleep latency (how long it usually takes to fall asleep per night), sleep disturbance (e.g., “Wake up in the middle of the night or early morning” and “had bad dreams”), use of sleeping medication (prescribed or “over the counter”), daytime dysfunction due to sleepiness (e.g., “During the past month, how much of a problem has it been for you to keep up enough enthusiasm to get things done?”), sleep efficiency (actual hours of sleep versus hours spent in bed), and overall sleep quality (perception of one's own sleep quality). The sum of the scores for these seven subcomponents yields one global score, ranging from 0 to 21, in which higher cumulative scores indicate poorer global sleep quality. This global measure was used in the current study. The PSQI has demonstrated good test–retest reliability (Backhaus, Junghanns, Broocks, Riemann, & Hohagen, 2002; Buysse et al., 1989) and criterion validity (Backhaus et al., 2002; Fictenberg, Putnam, Mann, Zafonte, & Millard, 2001; Grandner, Kripke, Yoon, & Youngstedt, 2006).
2.2.2. Alcohol-related consequences
The Rutgers Alcohol Problem Index (RAPI; White & Labouvie, 1989) assessed the occurrence of 23 negative consequences resulting from one's drinking in the past month (e.g., “Not able to do your homework or study for a test” and “caused shame or embarrassment to someone”). Each item is rated on a scale from 0 to 4 with 0 indicating “never” and 4 indicating “more than 10 times”. Inter-item reliability was very good for the RAPI (α=.91).
2.2.3. Weekly alcohol consumption
The Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985; Dimeff, Baer, Kivlahan, & Marlatt, 1999) assessed the total number of drinks consumed in a typical week. Participants were asked, “Consider a typical week in the last month. How much alcohol, on average (measured in number of drinks), did you drink on each day of a typical week?” Participants responded by reporting the typical number of drinks consumed on each day of the week. Weekly drinking was calculated by summing participant's responses for each day of the week. The DDQ has been used in previous studies of college student drinking and has demonstrated good validity (Larimer, Turner, Cronce, et al., 2001; Marlatt, Baer, Williams, et al., 1998).
2.2.4. Heavy episodic drinking
Heavy episodic or “binge” drinking (O'Malley & Johnston, 2002; Wechsler & Nelson, 2008) was assessed by asking participants how many times they consumed 4 (if female) or 5 (if male) drinks within a two-hour period in the last two weeks.
3. Results
Consistent with recent college-based studies (e.g., Lund et al., 2010), participants reported considerable sleep problems: 64.4% of females and 39.6% of males reported global sleep quality scores indicative of poor-quality sleepers, according to the PSQI diagnostic criteria.1 Further, 50.0% of females and 53.5% of males in this sample reported engaging in heavy episodic drinking in the two weeks prior to the survey. Table 1 presents comparison of means as a function of gender, including means, standard deviations, and ranges for global sleep quality and subcomponents, as well as drinking and alcohol consequences variables. Overall, females reported significantly poorer global sleep quality (p<.001), including components of subjective sleep quality (p=.050), sleep duration (p<.001), sleep disturbances (p=.003), and daytime dysfunction (p=.012), as well as fewer typical drinks per week (p=.002) compared to male peers.
Table 1.
Mean differences in main variables compared by gender.
| Measures | Males (n = 101) |
Females (n = 160) |
Range | t value |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Global Sleep Quality | 5.47 (2.56) | 6.90 (2.97) | 1–16 | 4.00*** |
| Subjective Sleep Quality | 0.99 (0.64) | 1.15 (0.64) | 0–3 | 1.97* |
| Sleep Latency | 0.95 (0.80) | 1.14 (0.97) | 0–3 | 1.68 |
| Sleep Duration | 0.92 (0.85) | 1.26 (0.82) | 0–3 | 3.23*** |
| Habitual Sleep Efficiency | 0.42 (0.77) | 0.51 (0.81) | 0–3 | 0.92 |
| Sleep Disturbances | 0.95 (0.50) | 1.16 (0.56) | 0–3 | 3.03** |
| Use of Sleeping Medication | 0.16 (0.49) | 0.31 (0.70) | 0–3 | 1.85 |
| Daytime Dysfunction | 1.10 (0.90) | 1.38 (0.84) | 0–3 | 2.52* |
| Alcohol Consumption | ||||
| Drinks per Week | 9.77 (10.69) | 6.40 (6.38) | 0–48 | −3.19** |
| HED Events | 1.58 (2.02) | 1.18 (1.66) | 0–8 | −1.71 |
| Consequences | ||||
| RAPI | 2.92 (4.88) | 3.32 (4.99) | 0–29 | 0.63 |
Note. Ranges displayed are sample ranges.
p<.05.
p<.01.
p<.001.
Bivariate correlational analyses (Table 2) show that poorer global sleep quality was positively correlated with heavy episodic drinking (p=.024) and alcohol-related consequences (p<.001), but not weekly alcohol consumption. Subcomponents of the Global Sleep Quality measure showed significant intercorrelation overall, and each positively correlated with global sleep quality (all ps<.001). Moreover, habitual sleep quality positively correlated with drinking outcomes: weekly drinking (p=.008), heavy episodic drinking (p<.001), and alcohol consequences (p<.001). Sleeping disturbances (p=.013) and daytime dysfunction (p=.003) were both positively associated with consequences, and use of sleeping medication positively correlated with weekly drinking (p=.005), heavy episodic drinking (p=.004), and consequences (p=.016). Global sleep quality (p<.001), subjective sleep quality (p=.05), sleep duration (p<.001), sleep disturbances (p=.003), and daytime dysfunction (p=.012) correlated with gender, such that females reported poorer sleep function than their male peers. Those reporting Greek affiliation were more likely than non-Greeks to use sleeping medication (p=.049), engage in heavy episodic drinking (p=.046), and experience greater alcohol consequences (p<.001). Finally, as expected, weekly alcohol consumption and heavy episodic drinking were positively correlated with the experience of alcohol consequences (ps<.001).
Table 2.
Correlation matrix of variables.
| Variable | 1 | 1a | 1b | 1c | 1d | 1e | 1f | 1g | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Global Sleep Quality | – | ||||||||||||||
| Global Sleep Quality Components: | |||||||||||||||
| 1a. Subjective Sleep Quality | .64*** | – | |||||||||||||
| 1b. Sleep Latency | .58*** | .28*** | – | ||||||||||||
| 1c. Sleep Duration | .55*** | .33*** | −.02 | – | |||||||||||
| 1d. Habitual Sleep Efficiency | .60*** | .26*** | .21*** | .38*** | – | ||||||||||
| 1e. Sleep Disturbances | .55*** | .26*** | .40*** | .12 | .18* | – | |||||||||
| 1f. Use of Sleeping Medication | .38*** | .16** | .25*** | −.04 | .10 | .12* | – | ||||||||
| 1g. Daytime Dysfunction | .55*** | .30*** | .07 | .23*** | .12* | .24*** | .03 | – | |||||||
| 2. Weekly Alcohol Consumption | .05 | −.01 | .05 | −.10 | .17** | .03 | .17** | −.08 | – | ||||||
| 3. Heavy Episodic Drinking | .14* | .06 | .05 | −.02 | .21*** | .06 | .18** | .02 | .70*** | – | |||||
| 4. Alcohol-Related Consequences | .23*** | .04 | .06 | .02 | .27*** | .15* | .15* | .18** | .48*** | .48*** | – | ||||
| 5. Gender (Female)a | −.24*** | −.12* | −.10 | −.20*** | −.06 | −.19** | −.12 | −.16* | −.19** | −.11 | −.04 | – | |||
| 6. Age | −.11 | −.12 | .04 | −.11 | −.01 | .02 | −.11 | −.11 | −.05 | −.07 | −.08 | .06 | – | ||
| 7. Race (Caucasian)b | .05 | .06 | .12 | −.12 | −.03 | .08 | .06 | .04 | .10 | .08 | .12 | −.05 | .09 | – | |
| 8. Greek Affiliationc | .02 | .08 | −.03 | −.02 | −.08 | .04 | .12* | .03 | .08 | .12* | .24*** | −.28*** | −.10 | .08 | – |
Note. In Global Sleep Quality and subcomponent measures, higher scores indicate poorer sleep-related function.
p<.05.
p<.01.
p<.001.
For Gender, reference level is male.
For Race, reference level is non-Caucasian.
For Greek Affiliation, reference level is non-Greek.
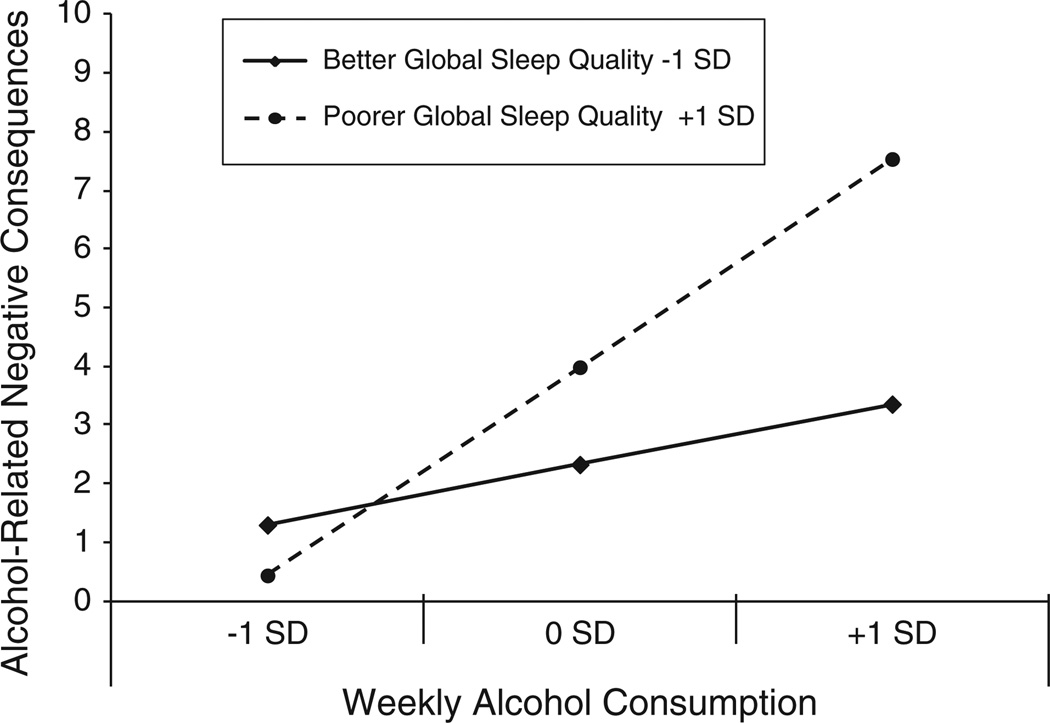
In Table 3, a four-step hierarchical multiple regression model predicting alcohol-related negative consequences is presented [F(7, 253)=18.85, p<.001]. All variables were standardized prior to computing the interaction term, and all results were assessed at the final step of the model. Each of the following steps added significant and unique variance over previous steps: sex, age, race, and Greek affiliation were included as covariates in Step 1 (ΔR2=.07, p=.001); drinks consumed per week served as a covariate in Step 2 (ΔR2=.18, p<.001); level of global sleep quality was entered in Step 3 (ΔR2=.03, p=.001); and the interaction term Weekly Drinks × Global Sleep Quality was entered in Step 4 (ΔR2=.06, p<.001). The final model accounted for a total of 34.3% of the variance in the experience of negative alcohol-related consequences. Greek affiliation (β=.17, p=.002), weekly alcohol consumption (β=.42, p<.001), global sleep quality (β=.16, p=.003), and the Weekly Alcohol Consumption × Global Sleep Quality (β=.25, p<.001) emerged as significant predictors of negative consequences, over and above assessed covariates. As illustrated in Fig. 1, the significant interaction was graphed according to established procedures (Aiken & West, 1991): interaction terms were graphed at one standard deviation below (lower levels of alcohol consumption, better global sleep quality) and above the mean (greater levels of alcohol consumption, poorer global sleep quality). Results revealed that among heavy drinking participants, those with poorer global sleep quality experienced significantly more alcohol-related harm than those with better global sleep quality.
Table 3.
Hierarchical multiple regression model predicting alcohol-related negative consequences by global sleep quality.
| Predictor | Negative consequences | ||||
|---|---|---|---|---|---|
| ΔR2 | B | SE | β | 95% CI | |
| Step 1: | .07*** | ||||
| Sex (male = 0, female= 1) | −0.27 | .29 | .05 | [−0.84, 0.30] | |
| Age | −0.13 | .26 | −.03 | [−0.64, 0.39] | |
| Race | 0.32 | .26 | .06 | [−0.19, 0.84] | |
| Greek Affiliation | 0.87 | .27 | .17** | [0.33, 1.41] | |
| Step 2: | .18*** | ||||
| Weekly Alcohol Consumption | 2.29 | .29 | .42*** | [1.72, 2.85] | |
| Step 3: | .03*** | ||||
| Global Sleep Qualitya | 0.83 | .27 | .16** | [0.29, 1.37] | |
| Step 4: | .06*** | ||||
| Consumption × Sleep Quality | 1.26 | .26 | .25*** | [0.74, 1.78] | |
| Total R2 | .34 | ||||
Note. ΔR2 significance levels represent unique variance explained over and above prior steps; B, SE, β and CI form the final step with all predictors entered;
CI=confidence interval.
p<.01.
p<.001.
A higher score indicates poorer global sleep quality.
Fig. 1.
Total Weekly Alcohol Consumption × Global Sleep Quality on experience of alcohol-related negative consequences.
4. Discussion
It is well established that college students drink frequently and often excessively, and, more recently, evidence has revealed widespread sleep deficiencies and erratic sleep-wake cycles in this population. The current study was the first to examine how these known risk factors may interact to heighten negative alcohol-related outcomes. Although there was no bivariate relationship between global sleep quality and weekly drinking, poorer global sleep quality was correlated with the riskiest form of drinking, heavy episodic drinking, as well as alcohol-related consequences. Further, global sleep quality appears to play an important role in the relationship between alcohol consumption and alcohol consequences such that among heavier drinking students, those with poorer sleep quality experienced significantly greater levels of alcohol consequences than students with better sleep quality. These findings are both disconcerting and informative given that heavier drinkers experienced significantly greater consequences than lighter drinking peers, and sleeping problems may exacerbate this already heightened risk.
The observed bivariate association between heavy episodic drinking and poorer global sleep quality, along with the absence of a direct relationship with typical weekly drinking, may reflect important subtleties regarding the mutual influence of these health-risk behaviors. That heavy episodic drinking episodes were significantly related to poorer global sleep quality may reveal a more direct and acute relationship in which heavier drinking during a night directly accounts for sleep irregularities on the same night (Roehrs & Roth, 2001; Schoenborn & Adams, 2008). On the other hand, it is possible that those suffering sleep difficulties may lack the volitional control and cognitive judgment needed to avoid excessive consumption. Findings assessing the associations between subcomponents of the overall global sleep measure and drinking outcomes also shed light on uniquely important relationships. For example, both habitual sleep efficiency and use of sleeping medication significantly correlated with alcohol use (weekly drinking and heavy episodic drinking) and alcohol consequences. These findings point to the need for a refined research focus that examines the extent to which specific areas of sleep may influence alcohol behaviors and risk. In particular, the relationship between use of sleeping medication and drinking behaviors may be indicative of co-morbid alcohol and prescription drug abuse, and warrants additional research.
Data on overall behavioral patterns (i.e., sleep patterns, alcohol use behaviors, consequences), however, provided considerably greater insight into the complex relationship between the constructs. Bivariately, typical weekly drinking and global sleep quality demonstrated a weak, non-significant relationship. Yet multivariately, the current findings strongly support and extend previous research of adolescents and young adults that has linked sleep problems with a range of negative outcomes, including risk-taking behaviors (e.g., drowsy driving, violence, unsafe sex, substance use; O'Brien & Mindell, 2005; Taylor & Bramoweth, 2010; Wolfson & Carskadon, 1998) and poor academic performance (Buboltz et al., 2006; O'Brien & Mindell, 2005). In the current sample of college students, poorer global sleep quality was found to substantially exacerbate the effect of heavier alcohol use on the experience of alcohol-related harm. Insufficient sleep may increase alcohol risk among at-risk drinkers through its depletion of cognitive functioning (O'Brien & Mindell, 2005; Pilcher & Otto, 1998; Taylor & Bramoweth, 2010; Wolfson & Carskadon, 1998). While heavier drinkers already face cognitive impairment and heightened risk, being deprived of quality sleep and healthy sleep function may make arriving at safe decisions and warding off negative consequences all the more difficult. In contrast, lighter drinkers, even if deprived of quality sleep, may have less compromised cognitive functioning when drinking. Further, heavier drinkers may drink late into the night when risks escalate and may suffer consequences the following day due to poorer global sleep quality and/or early rise obligations [e.g., going to “work or school high or drunk” or “missing a day (or part of a day) of school or work”]. Additional research is needed to assess psychosocial factors that may moderate or mediate the relationship between global sleep quality and alcohol consequences. Sleepiness, for instance, may reduce one's capacity to fend off peer pressure or avoid impulsive behaviors that heighten alcohol risk.
4.1. Implications
By demonstrating global sleep quality to be an important moderator in heavier drinking college students' experience of alcohol consequences, results support the need to promote healthy sleeping behaviors in this age group, particularly among non-abstaining first-and second-year students. First- and second-year students are at higher risk for low quality sleep since they tend to exhibit heightened levels of stress known to disrupt sleep (e.g., Lund et al., 2010) as well as experience more erratic sleep schedules due to early wake-up times (Singleton &Wolfson, 2009; Tsai & Li, 2004). Interventions targeting high-risk groups, such as incoming first-year students and students judicially sanctioned for violating campus alcohol policy, could be adapted to address the importance of maintaining a healthy lifestyle, both in terms of getting enough sleep and safe alcohol use. Interventions could educate students about the risks associated with insufficient sleep and teach students how to improve sleep patterns (e.g., regulating bed/rise sleep cycles; developing sleep rituals; exercising regularly; and avoiding caffeine, tobacco or even alcohol prior to bedtime). Further, interventions that provide students with tools for efficient studying, coping with multiple social and academic demands, and easing anxiety may help students to better manage stressors associated with college life shown to disrupt sleep.
4.2. Limitations
Several limitations of this study should be noted. First, although the present findings indicate that sleep is an important moderator in the drinking-consequences relationship, its cross-sectional design does not allow us to ascertain causality. Although prior studies have supported that heavier drinking leads to sleep problems (e.g., Roehrs & Roth, 2001; Singleton & Wolfson, 2009), it is feasible that poorer quality sleep precedes excessive drinking or that experiencing alcohol-related negative consequences has adverse effects on sleeping patterns. While the current study illustrates the heightened risk associated with poorer global sleep quality among heavier (as opposed to lighter) drinkers, longitudinal or event-level studies are needed to establish causality. Second, the current analyses did not control for potential confounds, such as risk-taking or impulsive personalities or depression that may predispose students to unsafe drinking and unhealthful sleeping routines. Studies that control for such personality dispositions are warranted. Next, as with any self-report data, some of the current responses may have suffered participant response bias or inaccurate recollection. Previous studies reviewing self-report data specific to sleep quality and alcohol consequences, however, have indicated good validity and reliability (Babor, Steinberg, Del Boca, & Anton, 2000; Fictenberg et al., 2001). Finally, participants were recruited from psychology courses at one private mid-size university on the West Coast. Samples of students with greater academic, cultural, and socioeconomic heterogeneity may present different drinking and sleeping patterns.
4.3. Conclusions
The current study provides strong support for the relationship between risky alcohol consumption and global sleep quality, as well as global sleep quality as an important moderator in the drinking-consequences relationship. Although global sleep quality is not related to weekly drinking, it does appear to exacerbate the risk of alcohol-related negative consequences in heavier drinkers — consequences that have proven to be widely detrimental to both personal and campus life. In recent years, college students have demonstrated heightened levels of overall sleep dysfunction and disorders (e.g., Gaultney, 2010; Lund et al., 2010), and lower sleep satisfaction than in the past (Hicks et al., 2001). Contributing to the prevalence of sleep-related dysfunction may be rapidly changing demands of college life (Kadison & DiGeronimo, 2004; Kneser, 2004) and increased levels of stress (American College Health Association, 2003, 2009; American College Health Association National College Health Assessment (ACHANCHA), 2003; CSCMH, 2009; Gallagher, 2006; MtvU and the Associated Press, 2008). Clearly, the relationships between sleep, drinking, and alcohol consequences among college students are multifaceted and require further exploration. The current study begins to explore these complex relationships by highlighting the importance of sleep as a target for interventions aimed at reducing the negative impact of drinking on college campuses.
Acknowledgments
Role of funding sources
This research was supported by a grant from the Alcoholic Beverage Medical Research Foundation (ABMRF) awarded to Shannon Kenney. ABMRF did not play a role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
According to PSQI criteria, a global score of “5” or greater indicates a “poor” sleeper.
Contributors
Shannon Kenney, Joseph LaBrie, Justin Hummer, and Andy Pham have each contributed significantly to, and approve of this final manuscript. Specifically, Shannon Kenney generated the idea for the study, performed all analyses, created the tables and figure, and contributed to writing all sections of the manuscript. Dr. LaBrie oversaw its production and edited all sections. Justin Hummer oversaw data collection and contributed to the development and writing of all sections of the manuscript. Andy Pham performed the literature review, assisted with the development of initial outlines of the manuscript, and contributed to writing the Introduction.
Conflict of interest
All authors declare that they have no conflicts of interest.
Contributor Information
Shannon R. Kenney, Email: shannon.kenney@lmu.edu.
Joseph W. LaBrie, Email: jlabrie@lmu.edu.
Justin F. Hummer, Email: jhummer@lmu.edu.
Andy T. Pham, Email: apham9@lion.lmu.edu.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks: Sage; 1991. [Google Scholar]
- American College Health Association. National College Health Assessment Spring 2008 reference group data report (abridged) Journal of American College Health. 2009;57(5):477–488. doi: 10.3200/JACH.57.5.477-488. [DOI] [PubMed] [Google Scholar]
- American College Health Association National College Health Assessment (ACHA-NCHA) Spring 2003 reference group report. Journal of American College Health. 2003;53(5):199–210. [PubMed] [Google Scholar]
- Babor TF, Steinberg K, Del Boca F, Anton R. Talk is cheap: Measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of Psychosomatic Research. 2002;53(3):737–740. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- Brooks PR, Girgenti AA, Mills MJ. Sleep patterns and symptoms of depression in college students. College Student Journal. 2009;43:464–473. [Google Scholar]
- Buboltz WC, Loveland J, Jenkins SM, Brown F, Soper B, Hodges J. College student sleep: Relationship to health and academic performance. In: Landaw MV, editor. College students: Mental health and coping strategies. Hauppauge, N: Nova Science; 2006. pp. 1–39. [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Center for Study of Collegiate Mental Health (CSCMH) 2009 Pilot study: Executive summary. 2009 [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief Alcohol Screening and Intervention for College Students (BASICS): A harm reduction approach. New York: Guilford Press; 1999. [Google Scholar]
- Dowdall GW. College drinking: Reframing a social problem. Santa Barbara, CA: Praeger Publishers; 2009. [Google Scholar]
- Fictenberg NL, Putnam SH, Mann NR, Zafonte RD, Millard AE. Insomnia screening in postacute traumatic brain injury: Utility and validity of the Pittsburgh Sleep Quality Index. American Journal of Physical Medicine & Rehabilitation/Association of Academic Physiatrist. 2001;80:339–345. doi: 10.1097/00002060-200105000-00003. [DOI] [PubMed] [Google Scholar]
- Galambos NL, Dalton AL, Maggs JL. Losing sleep over it: Daily variation in sleep quantity and quality in Canadian students' first semester of university. Journal of Research on Adolescence. 2009;19(4):741–761. [Google Scholar]
- Gallagher R. National Survey of Counseling Center Directors. Washington D.C: International Association of Counseling Services; 2006. [Google Scholar]
- Gaultney JF. The prevalence of sleep disorders in college students: Impact on academic performance. Journal of American College Health. 2010;59:91–97. doi: 10.1080/07448481.2010.483708. [DOI] [PubMed] [Google Scholar]
- Grandner M, Kripke D, Yoon I, Youngstedt S. Criterion validity of the Pittsburgh Sleep Quality Index: Investigation in a non-clinical sample. Sleep and Biological Rhythms. 2006;4(2):129–136. doi: 10.1111/j.1479-8425.2006.00207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grekin ER, Sher KJ. Alcohol dependence symptoms among college freshmen: Prevalence, stability, and person–environment interactions. Experimental and Clinical Psychopharmacology. 2006;14(3):329–338. doi: 10.1037/1064-1297.14.3.329. [DOI] [PubMed] [Google Scholar]
- Hicks RA, Fernandez C, Pellegrini RJ. Striking changes in the sleep satisfaction of university students over the last two decades. Perceptual and Motor Skills. 2001;93(3) doi: 10.2466/pms.2001.93.3.660. [DOI] [PubMed] [Google Scholar]
- Hingson R, Heeren T, Winter M, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18–24: Changes from 1998 to 2001. Annual Review of Public Health. 2005;26:259–279. doi: 10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. Journal of Studies on Alcohol and Drugs. Supplement. 2009;16:12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Drug and Alcohol Dependence. 2001;64(1):1–7. doi: 10.1016/s0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national results on adolescent drug use: Overview of key findings, 2006. Bethesda, MD: National Institute on Drug Abuse; 2007. (NIH Publication No. 07–6202). [Google Scholar]
- Kadison R, DiGeronimo TF. College of the woverwhelmed: The campus metnal health crisis and what to do about it. San Francisco, CA US: Jossey-Bass; 2004. [Google Scholar]
- Kneser G. College students leading hyper-enriched lives. St. Olaf E-newsletter; 2004. [Google Scholar]
- Larimer M, Turner A, Cronce J, et al. Evaluating a brief alcohol intervention with fraternities. Journal of Studies on Alcohol. 2001;62(3):370–380. doi: 10.15288/jsa.2001.62.370. [DOI] [PubMed] [Google Scholar]
- Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of Adolescent Health. 2010;46(2):124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Marcus CL, Loughlin GM. Effect of sleep deprivation on driving safety in housestaff. Sleep. 1996;19(10):763–766. doi: 10.1093/sleep/19.10.763. [DOI] [PubMed] [Google Scholar]
- Marlatt G, Baer J, Williams E, et al. Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment. Journal of Consulting and Clinical Psychology. 1998;66(4):604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- MtvU and the Associated Press. Center for the study of college student retention, college stress and mental health poll. 2008 Retrieved from: http://www.halfofus.com/_media/_pr/mtvU_AP_College_Stress_and_Mental_Health_Poll_Executive_Summary.pdf. [Google Scholar]
- National Institutes of Health. Working group report on problem sleepiness. Bethesda, MD: National Institutes of Health; 1997. National Center on Sleep Disorders Research and Office of Prevention, Education, and Control. [Google Scholar]
- Nelson TF, Xuan Z, Lee H, Weitzman ER, Wechsler H. Persistence of heavy drinking and ensuing consequences at heavy drinking colleges. Journal of Studies on Alcohol and Drugs. 2009;70(5):726–734. doi: 10.15288/jsad.2009.70.726. [DOI] [PubMed] [Google Scholar]
- O'Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behavioral Sleep Medicine. 2005;3(3):113–133. doi: 10.1207/s15402010bsm0303_1. [DOI] [PubMed] [Google Scholar]
- O'Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. Journal of Studies on Alcohol. 2002;(SUPPL 14):23–39. doi: 10.15288/jsas.2002.s14.23. [DOI] [PubMed] [Google Scholar]
- Perkins HW. Social norms and the prevention of alcohol misuse in collegiate contexts. Journal of Studies on Alcohol. 2002;(SUPPL 14):164–172. doi: 10.15288/jsas.2002.s14.164. [DOI] [PubMed] [Google Scholar]
- Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: Relationships between sleep and measures of health, well-being and sleepiness in college students. Journal of Psychosomatic Research. 1997;42(6):583–596. doi: 10.1016/s0022-3999(97)00004-4. [DOI] [PubMed] [Google Scholar]
- Pilcher JJ, Otto ES. The relationships between sleep and measures of health and well-being in college students: A repeated measures approach. Behavioral Medicine. 1998;23:170–177. doi: 10.1080/08964289809596373. [DOI] [PubMed] [Google Scholar]
- Pilcher JJ, Walters AS. How sleep deprivation affects psychological variables related to college students' cognitive performance. Journal of American College Health. 1997;46(3):121–126. doi: 10.1080/07448489709595597. [DOI] [PubMed] [Google Scholar]
- Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep: Journal of Sleep and Sleep Disorders Research. 2008;31(10):1351–1356. [PMC free article] [PubMed] [Google Scholar]
- Roehrs T, Roth T. Sleep, sleepiness, and alcohol use. Alcohol Research & Health. 2001;25(2):101–109. [PMC free article] [PubMed] [Google Scholar]
- Schoenborn CA, Adams PF. Sleep duration as a correlate of smoking, alcohol use, leisure-time physical inactivity, and obesity among adults. United States: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics 2004–2006; 2008. [Google Scholar]
- Singleton RA, Wolfson AR. Alcohol consumption, sleep, and academic performance among college students. Journal of Studies on Alcohol and Drugs. 2009;70(3):355–363. doi: 10.15288/jsad.2009.70.355. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Bramoweth AD. Patterns and consequences of inadequate sleep in college students: Substance use and motor vehicle accidents. Journal of Adolescent Health. 2010;46(6):610–612. doi: 10.1016/j.jadohealth.2009.12.010. [DOI] [PubMed] [Google Scholar]
- Thompson KM, Leinfelt FH, Smyth JM. Self-reported official trouble and official arrest: Validating a piece of the Core Alcohol and Drug Survey. Journal of Substance use. 2006;11(1):23–36. [Google Scholar]
- Tsai L-L, Li S-P. Sleep patterns in college students: Gender and grade differences. Journal of Psychosomatic Research. 2004;56(2):231–237. doi: 10.1016/S0022-3999(03)00507-5. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. What we have learned from the Harvard School of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. Journal of Studies on Alcohol and Drugs. 2008;69(4):481–490. doi: 10.15288/jsad.2008.69.481. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Wolfson AR. Adolescents and emerging adults' sleep patterns: New developments. Journal of Adolescent Health. 2010;46(2):97–99. doi: 10.1016/j.jadohealth.2009.11.210. [DOI] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Development. 1998;69:875–887. [PubMed] [Google Scholar]