Abstract
College students’ use of protective behavioral strategies (PBS; e.g., determining not to exceed a set number of drinks, avoiding drinking games) is related to lower levels of alcohol consumption and problems. The present study evaluated the efficacy of a novel brief, single-session group PBS skills training intervention aimed at increasing college students’ use of PBS and reducing risky drinking and consequences. Participants (N = 226) were heavy-drinking incoming first-year college women randomized to either a PBS skills training intervention or study skills control condition. Participants attended a 45-min group session and completed online surveys pre- and postintervention (1 month and 6 months). We conducted a series of 2 × 2 × 3 repeated-measures ANCOVAs with condition and baseline mental health (anxiety/depression) as the between-subjects factors and time as the within-subjects factor. Intervention participants, relative to controls, reported significantly greater increases in PBS use and reductions in both heavy episodic drinking and alcohol consequences. The intervention was particularly effective in increasing PBS use at 1 month among participants with high anxiety. Further, tests of moderated mediation showed a significant conditional indirect effect of condition on 1-month consequences through PBS use among participants with high levels of anxiety. Findings provide preliminary support for a brief PBS-specific group intervention to reduce alcohol risk among college women, particularly anxious women. Future research is needed to strengthen the long-term effectiveness of the present approach and further explore the moderating effects of mental health.
Keywords: protective behavioral strategies, intervention, alcohol, mental health, college students
Despite advances in young adult alcohol prevention and intervention programs over the past decade, the use and misuse of alcohol on U.S. college campuses remains a leading public health concern. Heavy alcohol consumption among college students is prevalent and has serious consequences for both the drinker and proximal others (e.g., academic neglect, psychological or interpersonal problems, unsafe driving, and risky sexual behavior/victimization; Hingson, Heeren, Winter, & Wechsler, 2005; Hingson, Zha, & Weitzman, 2009; Nelson, Xuan, Lee, Weitzman, & Wechsler, 2009). Considerable attention has been drawn to the potential for protective behavioral strategies (PBS; e.g., alternating alcohol and nonalcoholic drinks, determining not to exceed a set number of drinks, drinking only with close friends, or using a designated driver) to reduce alcohol risk in collegiate populations (Martens et al., 2005). The vast majority of this research supports that students who naturally utilize PBS drink less and experience fewer consequences than peers not employing or employing fewer PBS (Benton et al., 2004; Haines, Barker, & Rice, 2006; Martens et al., 2004; Park & Grant, 2005).
PBS Skills Training in College Alcohol Interventions
Skills training and personalized feedback on drinking behaviors are well-established treatment modalities in the substance misuse field (Baer, Kivlahan, & Donovan, 1999; Kivlahan, Marlatt, Fromme, Coppel, & Williams, 1990; Monti, Abrams, Kadden, & Cooney, 1989; Neighbors, Larimer, & Lewis, 2004; Ståhlbrandt, Johnsson, & Berglund, 2007). PBS skills training is often incorporated into multicomponent brief motivational interventions (BMIs; Larimer, Cronce, Lee, & Kilmer, 2004) that effectively reduce risky drinking among college students. In fact, postintervention PBS use mediated intervention efficacy in reducing drinking in both BMI (Barnett, Murphy, Colby, & Monti, 2007) and mailed feedback interventions (Larimer et al., 2007) and partially mediated the effectiveness of a BMI substance-free activity session in reducing alcohol problems (Murphy et al., 2012). Another study found that students who were given a list of drinking control strategies did increase their use of PBS, but did not drink less (Sugarman & Carey, 2009). Overall, however, reviews of individual-focused interventions for college drinkers support the effectiveness of brief skills-based programs using personalized feedback, such as those related to protective behaviors (Carey, Scott-Sheldon, Carey, & DeMartini, 2007; Cronce & Larimer, 2011; Larimer & Cronce, 2007).
Although providing students with training and personalized feedback on PBS may be a promising approach by which to reduce risky drinking among college students, it is not clear whether providing PBS training alone (i.e., not as part of a multicomponent intervention) is sufficient to reduce alcohol risk. Indeed, preliminary data from a recent standalone individual PBS intervention indicates that this approach may lead to substantial increases in PBS over time, but that these changes do not result in fewer consequences (LaBrie, Kenney, & Napper, 2013). However, this study targeted students accessing mental health services who may have lacked the resources to effectively utilize new PBS in complex social settings, especially after a single training session. Similarly, Martens and colleagues’ (Martens, Smith, & Murphy, 2013) 15-min single-session intervention that involved the delivery of personalized feedback regarding PBS use was not efficacious relative to a control condition at reducing alcohol use or related problems. This study, however, may have been too brief to impact behavioral change. More research is needed to determine which modes of delivery might enhance the effectiveness of standalone PBS interventions. For example, no intervention to date has evaluated the effects of a facilitator-led, group-based standalone PBS skills training intervention.
Incoming First-Year College Women and PBS
The National Institute on Alcohol Abuse and Alcoholism identified college transitions as “critical period(s)” for alcohol risk, often typified by excessive drinking, increased consequences, and the development of patterns of problematic use (National Institute on Alcohol Abuse and Alcoholism, 2002; Schulenberg et al., 2001). This period is especially risky for women who report the single largest lifetime increases in drinking from high school to college (Center on Addiction and Substance Abuse, 2003). Moreover, evidence suggests that women’s drinking rates are approaching those of their male peers (e.g., Grucza, Norberg, & Bierut, 2009; O’Malley & Johnston, 2002; Young, Morales, McCabe, Boyd, & Darcy, 2005); this despite physiological gender differences that accelerate intoxication and, consequently, increase risks for related harms in females.
College women with poor mental health are especially vulnerable to experiencing alcohol-related problems (e.g., academic difficulties, risky sexual behaviors, and alcohol dependence) than peers with stronger mental health, even at comparable levels of drinking (LaBrie, Kenney, & Lac, 2010; LaBrie, Kenney, Lac, Garcia, & Ferraiolo, 2009; Weitzman, 2004). Further, compared to males, college women are more likely to experience mental distress and co-occurring mental health and substance misuse (Fillmore et al., 1997; Pace & Trapp, 1995; Silverman, 2004; Walitzer & Sher, 1996; Weitzman, 2004). Not only are depressed mood and anxiety associated with increased salience of alcohol cues and decreased attention to alcohol-related risks (Feldstein Ewing, Filbey, Chandler, & Hutchison, 2010; Monti, Rohsenow, & Hutchison, 2000), but women are susceptible to consuming alcohol as a means to self-medicate in order to cope with distress or alleviate anxiety (Bischof, Rumpf, Meyer, Hapke, & John, 2005; Park & Grant, 2005). This type of incentivized drinking not only fails to effectively resolve problems, but is likely to lead to excessive consumption, related consequences, and maladaptive drinking patterns (Cooper, Agocha, & Sheldon, 2000; Karwacki & Bradley, 1996; Labouvie & Bates, 2002).
Targeted PBS Skills Training for Women
PBS are considered important harm-reduction tools for college women who are more likely to implement PBS than their males peers (Benton et al., 2004; Delva et al., 2004; Haines et al., 2006; Walters, Roudsari, Vader, & Harris, 2007). This may be due in part to PBS’ focus on self-protection, which may be a more salient concern among college women compared to college men. Further, studies demonstrate that PBS may be particularly effective in reducing drinking and related consequences among college women with poorer as compared to stronger mental health (LaBrie et al., 2010; LaBrie et al., 2009). Existing research examining PBS use among college women, however, is cross-sectional and focuses on women’s natural use of PBS. No study to date has assessed a PBS-specific skills training intervention targeting at-risk college women.
Teaching incoming college women, particularly heavy drinkers with poorer mental health, a variety of PBS may be a valuable strategy for reducing alcohol risk and promoting a more successful transition into college contexts. Past research indicates a number of approaches that may be useful for teaching PBS, including cognitive–behavioral therapy (CBT). CBT addresses maladaptive risk behaviors through improved cognitive awareness, skills acquisition and application, and goal setting, all of which may be well-suited to PBS skills training. Moreover, a facilitator-led CBT-based brief group intervention may be a particularly favorable approach for use with college women. In this subgroup, for example, brief in-person-delivered alcohol interventions are shown to promote substantially greater and longer-term alcohol-related risk reduction compared to computer-delivered interventions (Carey, Carey, Henson, Maisto, & DeMartini, 2011). Moreover, small group-based interventions are consistent with women’s preference for intimate, discussion-oriented settings that allow for peer collaboration and support (Gleason, 1994). Therefore, providing CBT-based PBS training within a small group setting may be a particularly effective approach for teaching and motivating PBS use among college women.
Project Aims and Objectives
The present study implemented a brief single-session group cognitive–behavioral skills training intervention aimed at increasing PBS use and decreasing risky drinking and related consequences among heavy-drinking women during their transition to college. We hypothesized that participants receiving the PBS intervention would report significantly greater use of PBS and lower levels of risky drinking and negative consequences relative to participants in the control condition at 1- and 6-months postintervention. Further, we expected severity of mental distress to moderate intervention effectiveness, such that participants with high (compared to low) levels of depression or anxiety would report greater increases in the use of PBS and, in turn, decreases in alcohol consumption and consequences. Although depression and anxiety both involve general affective distress, depression (low positive affect) and anxiety (hyperarousal) are pathologically distinct and thus may result in different pathways to risk (Brown, Chorpita, & Barlow, 1998). Therefore, we will examine whether depression and anxiety have different moderating effects on the relationship between PBS use and alcohol risk. Finally, we hypothesized that postintervention PBS use would mediate the relationship between condition and prospective alcohol outcomes, and that the indirect effect of condition on alcohol outcomes would be greatest among those with higher mental distress.
Method
Participants
Participants were incoming first-year female students from a private midsize university of approximately 5,700 full-time undergraduates (58% female). The final sample is comprised of 226 participants reporting past-month heavy episodic drinking (HED; consuming four or more drinks on a drinking occasion) who attended a brief group session and completed all study surveys both pre- and postintervention. Participants had a mean age of 18.07 years (SD = 0.54) and racial composition was as follows: 62.4% White, 14.2% multiracial, 8.4% Asian, 7.1% “other,” 3.5% African American, 1.8% Hawaiian/Pacific Islander, and 0.9% American Indian/Alaskan Native. Additionally, 16.4% reported Hispanic ethnicity.
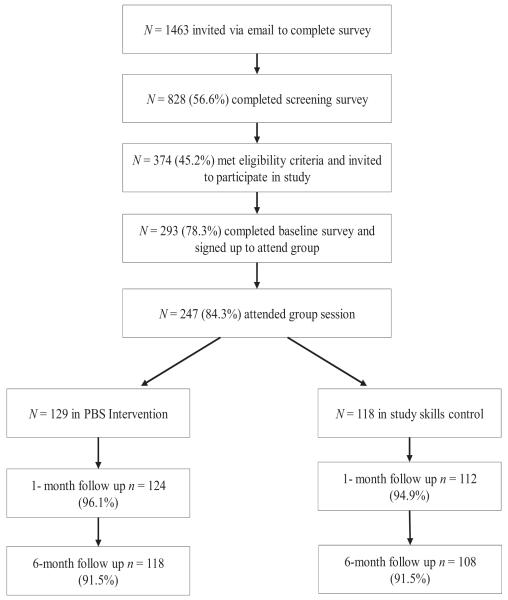
Design and Procedure
Three weeks into their first semester on campus, all first-year women (N = 1,463) were invited via e-mail to participate in a study “regarding health and wellness issues among first-year college women.” Figure 1 illustrates the flow of participants into the study. Students opting to participate clicked on a link directing them to the initial 10-min online screening survey. Before entering the survey, participants electronically signed an Institutional Review Board-approved informed consent form. Over 2 years, a total of 828 participants (56.6% of invited sample) completed the initial online screening survey that assessed demographics, drinking-related behaviors, and mental health. Of these, 374 (45.2%) met the inclusion criteria for past-month HED and were invited to participate in the study by completing an additional 10–15-min baseline survey, attending one 45-min group session with approximately 10 other first-year women and completing two brief online follow-up surveys. At the end of the baseline survey, participants were prompted to select a group meeting to attend over the next 3 weeks. Participants were blind to condition, and attendee names were not released. Over 2 years, 293 students completed the baseline survey and signed up to attend a group session, and 247 participants attended a group session (129 intervention, 118 control). The final sample was comprised of 226 participants (118 intervention, 108 control) who attended a session and completed 1- and 6-month postintervention online surveys (refer to Figure 1 for follow-up rates). The final sample did not differ significantly from those who attended a group session but did not complete the follow-up surveys in preintervention alcohol or mental health variables. Incentives included a raffle for $100 gift cards (screening survey), a $30 voucher (baseline survey and group session), a $10 check (1- and 6-month follow-up surveys), and a $10 bonus check for completing both follow-up surveys.
Figure 1.
Participant flow diagram. PBS = protective behavioral strategies.
Measures
In addition to demographics, online surveys assessed health behaviors and beliefs related alcohol and mental health. Visual images displayed examples of standard drinks (e.g., 12 oz. beer, 10 oz. wine cooler, 1 oz. 100-proof [1.25 oz. 80-proof] liquor).
PBS
Participants reported on their PBS use before or while drinking using the 15-item Protective Behavioral Strategy Surveys (PBSS; Martens et al., 2005) and seven items from the 21-item Strategy Questionnaire (Sugarman & Carey, 2007). The PBSS is the most rigorously tested and psychometrically validated measure of protective behaviors (Martens, Ferrier, & Cimini, 2007; Martens, Pederson, Labrie, Ferrier, & Cimini, 2007; Walters et al., 2007). Further, seven items from the Strategy Questionnaire were determined to be relevant to college women, and thus were included in the study, while items conceptually similar to PBSS items were excluded. Using a 6-point scale ranging from never to always, participants were instructed to indicate the degree to which they had engaged in protective behaviors while consuming alcohol or “partying” in the past month. Assessed PBS included “leave the bar/party at a predetermined time,” “make sure you go home with a friend,” “drink slowly rather than gulp/chug,” “use a designated driver,” and “eat before or while drinking.” The 22 items were summed to form a composite score for each assessment time point: baseline (α= .89), 1 month (α= .91), and 6 months (α= .93).
Alcohol use
Weekly drinks assessed the total number of drinks consumed in a typical week using the Daily Drinking Questionnaire (Collins, Parks, & Marlatt, 1985; Dimeff, Baer, Kivlahan, & Marlatt, 1999). Participants were asked, “Consider a typical week in the last month. How much alcohol, on average (measured in number of drinks), did you drink on each day of a typical week?” Participants responded by reporting the typical number of drinks consumed on each day of the week. Weekly drinking was calculated by summing participant’s responses for each day. The Daily Drinking Questionnaire has been used in previous studies of college student drinking and has demonstrated good validity (Larimer et al., 2001; Marlatt et al., 1998). HED occasions in the past month were assessed using participants’ open-ended responses to the question, “On how many occasions did you consume four or more drinks in a 2-hr period?”
Alcohol-related negative consequences
The 23-item Rutgers Alcohol Problem Index (White & Labouvie, 1989) was used to assess the frequency of alcohol-related negative consequences experienced (e.g., “Suddenly found yourself in a place you could not remember getting to,” “Felt physically or psychologically dependent on alcohol,” “Passed out or fainted suddenly,” “Had a fight, argument, or bad feelings with a friend/family member”) in the past month. Response options ranged from 0 (never) to 4 (10 or more times), and items were summed to form a composite score for each time point: baseline (α= .82), 1 month (α= .88), and 6 months (α= .84).
Mental health
Anxiety was assessed using the 21-item Beck Anxiety Inventory (BAI; Beck & Steer, 1993; α= .90). Participants reported on their past-month symptoms of anxiety, including “numbness or tingling” and “fear of losing control,” on a scale ranging from 0 (not at all) to 3 (severely). The BAI was designed to minimize overlap with depressive symptoms (McDowell, 2006) and is found to have acceptable reliability and validity (Beck, Epstein, Brown, & Steer, 1988; Fydrich, Dowdall, & Chambless, 1992). Summed BAI scores less than eight indicate minimal anxiety and eight or greater indicate mild to high levels of anxiety. Based on these guidelines, the BAI responses were dichotomized for analysis (0 = minimal anxiety, 1 = mild-to-high anxiety).
The 20-item Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1991; α= .90) measured participant’s depressive symptomatology in the past week (e.g., “I had crying spells” and “I felt that everything I did was an effort”) using a 4-point scale ranging from 0 (rarely or none of the time [less than 1 day]) to 3 (most or all of the time [5–7 days]). The CES-D is demonstrated to be valid and reliable (Cuijpers, Boluijt, & van Straten, 2008; Santor, Zuroff, Ramsay, Cervantes, & Palacios, 1995). Based on standard cutoffs, the CES-D was dichotomized such that summed scores greater or equal to 16 indicated clinically significant depressive symptomatology (1) and scores less than 16 indicated no clinically significant depression (0).
Intervention and control sessions
Each session was attended by 8–12 incoming first-year college female participants, was approximately 45 min in length, and was led by two trained facilitators. Facilitators included five members of the university alcohol research lab, including the principal investigator (PI) and project coordinator, who are trained in group motivational enhancement and CBT techniques, and are experienced in leading group interventions. During the summer preceding each cohort, the research team received training on PBS intervention delivery and intervention protocol. Trainings included role-playing scenarios likely to be encountered during the proposed intervention. Issues of adherence to protocol were discussed and each facilitator delivered three pilot interventions. With participants’ consent, sessions were audio recorded and randomly selected for review by the PI. The PI provided weekly group supervision to all facilitators that addressed and resolved any difficulties encountered.
PBS intervention condition
The Group PBS session followed a cognitive–behavioral skills training model and focused on PBS and participants’ use of them. The goals of the intervention included raising participants’ awareness and developing skills for using PBS to reduce risky drinking and consequences. At the beginning of the session, participants were reminded of the information in the informed consent form and the confidentiality of their responses to both the surveys and what they shared in the group. Norms for group participation modeled nonjudgmental acceptance of others, willingness to self-disclose, and respecting confidentiality (Velasquez, Maurer, Crouch, & DiClemente, 2001). With this orientation in mind, facilitators began by encouraging participants to talk about the college drinking culture and engaged participants in a conversation about both the positive and negative aspects of alcohol use in their own lives and lives of other students. As negative consequences emerged, the facilitator asked the group to generate behavioral strategies for avoiding the kind of drinking that leads to the consequences. Participants discussed the practicality of using each strategy and were encouraged to describe specific drinking situations that may facilitate or impede its usage.
With the use of visual aids, the facilitators then introduced PBS before briefly explaining how they can be used to drink more safely, enhance the positive aspects of drinking, and reduce risks prevalent in college women. Facilitators distributed personalized PBS feedback sheets that included each participant’s prior survey responses and summarized the PBS she reported using in the month prior to completing the survey. For each of 22 unique PBS, personalized feedback sheets reflected if the participants reported using it never, rarely, occasionally/sometimes, or usually/always. Participants reflected on the PBS they used most and shared how and in what drinking contexts they were able to implement it effectively. This dialogue was important in promoting awareness of PBS, identifying high-risk drinking situations, and sharing the skills (i.e., PBS) found to be effective. Participants then discussed the PBS they did not use as often and anticipated barriers to their use. Throughout the intervention, the facilitators reinforced statements of efficacy and encouraged participants to continue using PBS and adopt PBS not currently employed.
Each participant was asked to choose three PBS that she would like to begin using or using more frequently. After discussing any anticipated challenges associated with implementing their chosen PBS, participants wrote specific behavioral goals (i.e., how PBS will be implemented) for each chosen strategy on behavioral goal sheets.
Study skills control condition
The format of the control condition was similar to the intervention group. After reminding participants of their informed consent and confidentiality, facilitators discussed the importance of good study skills for academic success. Next, students reflected on the benefits and challenges of note taking. Students were provided with a list of 16 note-taking skills and were asked to indicate how frequently they used each strategy. Participants reflected on the note-taking skills they used most often and shared how they applied them effectively. Participants then identified note-taking skills they were interested in using more often and barriers to implementation. Using visual aids, facilitators contributed additional information about effective strategies for promoting note-taking skills (e.g., reading class handouts before class, identifying keywords, reviewing notes after lectures).
Data analyses
Prior to analyses, we explored the distributional properties of all variables. Positively skewed variables included baseline anxiety, alcohol-related negative consequences, weekly drinks, and HED at all three time points. Each respective composite was square-root transformed for analyses (Cohen, Cohen, West, & Aiken, 2003). Following transformations, none of the skewness or kurtosis levels exceeded an absolute value of 0.8. For ease of interpretation, nontransformed values are reported in texts, tables, and figures. Next, means-based testing was used to compare baseline differences by condition. To evaluate the efficacy of the intervention, we implemented analysis of covariance (ANCOVA) with condition (PBS intervention, study skills control), baseline depression (low/high depression), and baseline anxiety (low/high anxiety) as the between-subjects factors and time (baseline, 1 month, and 6 months) as the within-subjects factor. Serving as the dependent measures in analyses were past month PBS use, weekly drinking, HED, and alcohol-related negative consequences. Following a significant omnibus test, contrasts were used to examine pairwise differences by time or condition. All analyses assessing PBS and consequences controlled for baseline alcohol use in order to statistically rule out any initial differences.
To test the hypothesis of mediation, we examined intervention effects on prospective alcohol consequences (1 month and 6 months) as mediated by PBS use at 1 month. More specifically, PROCESS macro via IBM SPSS (Hayes, 2013) was employed to examine moderated mediation. That is, whether the indirect effect of condition on alcohol consequences is conditional on mental health status. Conditional indirect effects were examined and 95% bias-corrected confidence intervals were computed using 1,000 bootstrap samples.
Results
Randomization Check
At baseline, no significant differences emerged between conditions on either drinking-related (PBS, weekly drinking, HED, alcohol-related negative consequences) or mental health (depression or anxiety) measures. Preintervention, this sample of first-year college women drinkers reported high levels of mental distress: 31.9% met CES-D criteria for clinically significant depressive symptoms (total: M = 13.00, SD = 9.71; intervention: M = 12.48, SD = 9.22; control: M = 13.57, SD = 10.24) and 38.9% met BAI criteria for mild to high levels of anxiety (total: M = 7.79, SD = 7.88; intervention: M = 7.91, SD = 7.58; control: M = 7.65, SD = 8.25). Overall, alcohol risk was also high: in the past month, the majority of participants (56.2%) reported engaging in HED on typical drinking occasions and experiencing alcohol-related negative consequences (80.5% reported one and 66.3% reported two or more consequences).
Evaluating the Efficacy of the Intervention
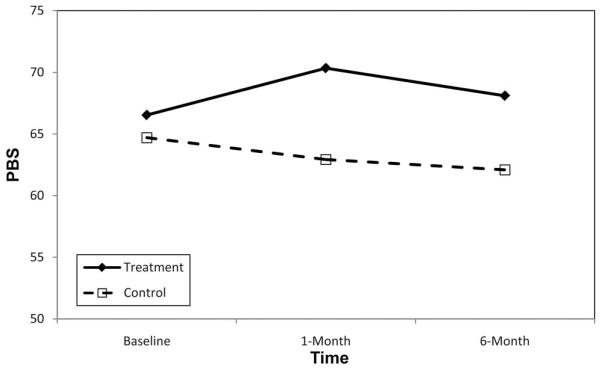
PBS
The 2 × 2 × 3 repeated-measures ANCOVA on PBS use revealed no main effect for time, but a significant main effect for condition, F(1, 219) = 4.89, p = .028 and Time × Condition effect, F(2, 438) = 3.14, p = .044 (see Table 1 and Figure 2). Further, the Time × Condition × Anxiety interaction was significant, F(2, 438) = 3.18, p = .043. Post hoc contrasts showed no differences in PBS use between the intervention group and the control group at baseline; however, intervention participants reported significantly greater PBS use, relative to control group participants, at both 1- and 6-month follow-ups (ps < .01). Within the intervention condition, participants reported increases in PBS use from baseline to 1-month follow-up (p < .05), although neither baseline nor 1-month PBS use differed significantly from 6-month PBS use. Further, although there were no significant baseline differences in PBS use by condition as a function of anxiety (low [minimal anxiety] or high [mild to high anxiety]), postintervention differences emerged. Among high-anxiety participants, intervention participants reported significantly higher levels of PBS use than high-anxiety control participants at 1-month follow-up (p < .05). Among low-anxiety participants, intervention participants reported significantly higher levels of PBS use than low-anxiety control participants at 6-month follow-up (p < .05). All interactions involving depression were nonsignificant.
Table 1. Repeated-Measures ANCOVAs Examining Past-Month Alcohol Consumption and Consequences by Condition at Baseline, 1-Month, and 6-Month Follow-ups.
| Intervention |
Control |
Time × Condition |
Time × Condition × Depression |
Time × Condition × Anxiety |
|||
|---|---|---|---|---|---|---|---|
| (N = 118) |
(N = 108) |
Time |
Condition |
||||
| Measure | M (SD) | M (SD) | F | F | F | F | F |
| PBS | |||||||
| Baseline | 66.54(15.83) | 64.70 (19.24) | |||||
| 1 month | 70.34(15.99) | 62.93 (21.70) | |||||
| 6 months | 68.10(18.72) | 62.09 (23.74) | 2.08 | 4.89* | 3.14* | .32 | 3.18* |
| Weekly drinking | |||||||
| Baseline | 7.85 (5.41) | 8.43 (7.53) | |||||
| 1 month | 6.72 (4.52) | 8.35 (8.15) | |||||
| 6 months | 7.21 (5.74) | 7.96 (8.20) | 2.24 | .05 | .18 | .21 | 1.27 |
| HED occasions | |||||||
| Baseline | 3.69(1.37) | 3.63 (1.73) | |||||
| 1 month | 3.61 (1.43) | 3.91 (1.75) | |||||
| 6 months | 3.49(1.71) | 4.00(1.99) | .43 | .08 | 4.29* | .02 | .42 |
| Alcohol consequences | |||||||
| Baseline | 5.14(5.42) | 4.07 (4.55) | |||||
| 1 month | 4.58 (4.40) | 4.95 (5.31) | |||||
| 6 months | 4.42 (4.50) | 4.60 (5.91) | .71 | .43 | 4.51** | .65 | .13 |
Note. PBS = protective behavioral strategies; HED = heavy episodic drinking. All analyses controlled for anxiety and depression; analysis examining PBS and alcohol-related consequences also controlled for baseline drinking.
p < .05.
p < .01.
p < .001.
Figure 2.
Protective behavioral strategies (PBS) use over time (baseline through 6-month follow-up) by condition.
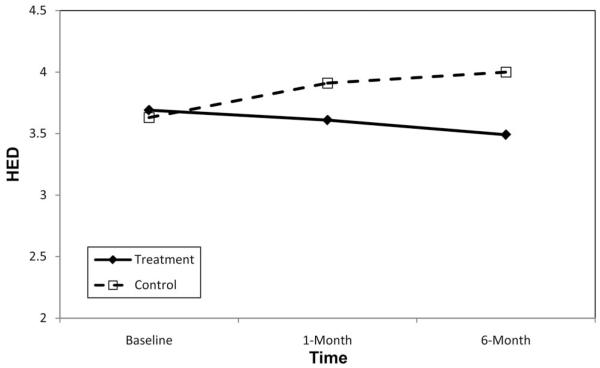
Alcohol consumption
A series of 2 × 2 × 3 repeated-measures ANOVAs was used to assess changes in both typical weekly drinking and HED (see Table 1). The overall main effects of both time and condition were nonsignificant. With respect to HED, a significant Time × Condition effect was found, F(2, 440) = 4.29, p = .014 (see Figure 3). Post hoc contrasts revealed a significant decrease in HED occasions within the intervention condition only, such that baseline HED was significantly lower at 1-month (but not 6-month) follow-up (p < .05).
Figure 3.
Heavy episodic drinking (HED) over time (baseline through 6-month follow-up) by condition.
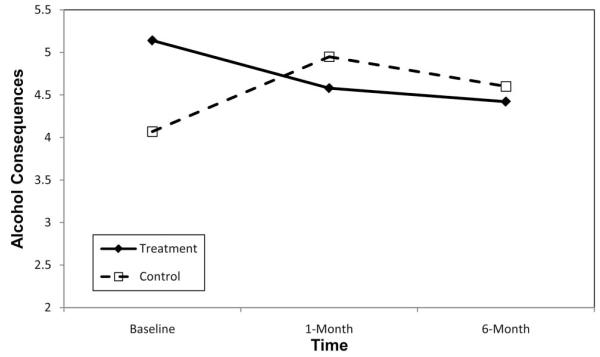
Alcohol-related negative consequences
The main effects of time and condition were nonsignificant; however, a significant Time × Condition effect was found, F(2, 438) = 4.51, p = .011 (see Figure 4). Post hoc analyses showed that, within the control condition, mean consequences at baseline were not significantly different from either follow-up time point. In the intervention condition, however, reported consequences following the intervention were significantly lower than baseline consequences at both 1-month (p < .05) and 6-month (p < .01) postintervention.
Figure 4.
Alcohol-related negative consequences over time (baseline through 6-month follow-up) by condition.
Tests of Moderated Mediation
Moderated mediation analyses examined whether PBS use at 1 month mediated the relationship between condition and alcohol-related consequences at 1-month and 6-months postintervention, conditional on anxiety level. Given that the ANCOVA results indicated that participants’ level of anxiety moderated the influence of condition on PBS use, we examined whether the indirect effect of condition on consequences through PBS use was moderated by participants’ level of anxiety. We hypothesized that the indirect effect of condition on consequences would be greater for those with higher levels of anxiety. Baseline alcohol use and depression were included as control variables. A significant conditional indirect effect was decomposed at values of anxiety that corresponded to the 10th, 25th, 50th, 75th, and 90th percentiles of the distribution (Hayes, 2013).
Analyses examining alcohol consequences at 6 months indicated that PBS use at 1 month did not mediate the relationship between condition and consequences (bootstrap indirect effect =−.02, 95% confidence interval [CI] = [−.10, .03]), nor did anxiety moderate the indirect effect (see Table 2). In contrast, the model predicting alcohol consequences at 1 month did provide evidence of moderated mediation (see Table 2). At high levels of anxiety (75th and 90th percentiles), the indirect effect of condition through PBS use was negative and significantly different from zero (bootstrap conditional indirect effects =−.09, 95% CI = [−.24, −.01], and .16, 95% CI = [−.43, −.01], respectively). These findings indicate that among those high in anxiety, the intervention was associated with greater PBS use, which in turn reduced alcohol consequences at 1-month postintervention. Interestingly, anxiety did not moderate the relationship between condition and PBS use (b = 1.48, p = .39); however, anxiety did moderate the relationship between PBS use and consequences (b =−.01, p = .046). The Johnson-Neyman technique was used to probe this interaction. PBS use was associated with fewer alcohol-related consequences for those who reported higher levels of anxiety (0.4 standard deviations above the mean or greater). At low and mean levels of anxiety, PBS use was not associated with alcohol consequences.
Table 2. Moderated Mediation Analysis of the Relationship Between Condition and Alcohol-Related Negative Consequences Through PBS Use With Anxiety as a Moderator.
| Predictor | Estimate | SE | T | p |
|---|---|---|---|---|
| PBS use | ||||
| Constant | 78.93 | 4.15 | 19.03 | .00 |
| Condition | 3.89 | 4.80 | .81 | .42 |
| Anxiety | −2.46 | 1.29 | −1.90 | .06 |
| Condition × Anxiety | 1.48 | 1.73 | .85 | .39 |
| Alcohol consequences (1 month) | ||||
| Constant | .12 | .59 | .21 | .83 |
| Condition | .01 | .15 | .04 | .97 |
| PBS use | .01 | .01 | .78 | .44 |
| Anxiety | .54 | .19 | 2.82 | .01 |
| PBS Use × Anxiety | − .01 | .00 | −2.01 | .05 |
| Alcohol consequences (6 months) | ||||
| Constant | −.33 | .65 | −.51 | .61 |
| Condition | .01 | .16 | .07 | .94 |
| PBS use | .01 | .01 | 1.16 | .25 |
| Anxiety | .61 | .21 | 2.91 | .00 |
| PBS Use × Anxiety | −.00 | .00 | −1.72 | .09 |
| Conditional effects | |||
|---|---|---|---|
| Anxiety quintiles | Bootstrap indirect effect | Bootstrap SE | 95% CI bias corrected |
| Alcohol consequences (1 month) | |||
| 10th | .02 | .05 | [−.04, .20] |
| 25th | −.01 | .04 | [−.11, .05] |
| 50th | −.05 | .04 | [−.16, .01] |
| 75th | −.09 | .06 | [−.24, −.01] |
| 90th | −.16 | .10 | [−.43, −.01] |
| Alcohol consequences (6 months) | |||
| 10th | .04 | .06 | [−.04, .24] |
| 25th | .02 | .03 | [−.03, .09] |
| 50th | −.02 | .03 | [−.09, .04] |
| 75th | −.05 | .05 | [−.16, .02] |
| 90th | −.11 | .09 | [−.34, .00] |
Note. PBS = protective behavioral strategies. All analyses controlled for baseline alcohol use and depression. Unstandardized regression coefficients are reported. Condition (0 = study skills control, 1 = PBS intervention).
Discussion
This study was the first to examine the efficacy of a brief, single-session PBS-specific group intervention. As expected, relative to control participants, intervention participants reported greater use of PBS, lower levels of risky drinking (i.e., HED), and fewer negative consequences postintervention. Even after controlling for baseline drinking, the intervention was related to greater PBS use than the control condition up to 6 months following the intervention. Within the intervention condition, the risk-reducing changes (increased PBS use and lower levels of HED and alcohol-related consequences) were evident at 1 month following the intervention. However, only reductions in consequences remained significant at 6-months postintervention. In addition, the intervention was most effective at reducing high-risk drinking behaviors (e.g., HED), rather than overall drinking levels. This disparity suggests that although intervention participants may have been motivated to decrease excessive drinking in order to drink more safely, they tended to maintain overall consumption. These results are promising given the cost-effective and easily transportable intervention design. After just one 45-min session targeting heavy drinking among incoming first-year college women, those receiving PBS skills training exhibited safer drinking behaviors postintervention than those randomized to the control condition.
Many women transitioning to college for the first time may not be adequately equipped to safely navigate alcohol pervasive social contexts. This study supports the notion that incoming college women may be particularly receptive to group-based PBS skills training. PBS are practical and easily implementable, which encourages their use. Further, given the array of PBS available, personalized PBS feedback enables each participant to self-select the use of those strategies that may best resonate with her. Future applications of this intervention should examine its efficacy among other high-risk groups of women, including female athletic teams and sorority houses. Although men utilize less PBS than women in general (Benton et al., 2004; Delva et al., 2004; Haines et al., 2006;Walters et al., 2007), the present intervention approach (group, standalone PBS intervention) has not been tested on men. It is possible that a group discussion with same-sex peers and receipt of personalized PBS feedback may enable men to better understand how certain strategies may benefit them. Further, given their lower likelihood to use PBS inherently, PBS skills training may present men with considerable opportunities to learn and implement new PBS.
Although this single session intervention offers much potential, its effects appear to be most pronounced at 1-month postintervention. By 6-month follow-up intervention, participants’ reports of PBS use were not significantly different from baseline. Furthermore, PBS use at 1-month follow-up did not mediate the relationship between condition and 6-month consequences. Although the intervention appears to mitigate the natural decrease in PBS use seen in the control condition, it is not clear how effective the intervention was in promoting longer-term behavior change. It is our hope that once participants implement PBS and recognize that these easy to use strategies can enhance their safety as well as enjoyment in drinking contexts, they will continue to use PBS. Incorporating additional booster sessions or email and text message reminders of PBS goals might help increase intervention efficacy over time. Regardless, more research is needed to assess the long-term efficacy of this PBS-specific intervention.
The current study provides important insights into how mental health may moderate the effect of the intervention. Based on past cross-sectional research (Kenney & LaBrie, 2013; LaBrie et al., 2010; LaBrie et al., 2009; Weitzman, 2004), we hypothesized that severity of mental distress (depression and anxiety) would moderate intervention effectiveness, such that participants with high (compared to low) levels of depression or anxiety would benefit most from the intervention. Our findings, however, were mixed. In the ANCOVA analyses, only anxiety moderated the effect of the intervention on PBS use. The intervention was effective in increasing PBS use at 1-month postintervention among participants with high anxiety, indicating that participants with high anxiety at the time of the intervention were particularly amenable to learning and implementing PBS.
The results of the moderated mediation analysis shed further light on the relationship between anxiety and PBS use. Only among those with higher levels of anxiety did PBS use mediate the relationship between condition and alcohol consequences at 1-month postintervention. Among those with higher levels of anxiety, the intervention led to greater PBS use, which in turn was associated with fewer alcohol-related consequences. In contrast to the ANCOVA results, anxiety did not moderate the relationship between condition and PBS use at 1 month; however, anxiety did moderate the relationship between PBS use and alcohol consequences. Consistent with previous research demonstrating that PBS may be particularly beneficial for those with poor mental health (LaBrie et al., 2010; LaBrie et al., 2009; Napper, Hummer, & LaBrie, in press), PBS use was associated with fewer alcohol consequences for those who reported higher levels of anxiety. These findings are enlightening given that students with high anxiety, compared to low anxiety, naturally use less PBS (LaBrie et al., 2010; LaBrie et al., 2009; Napper et al., in press) and may lack the emotional regulation, volitional control, and social resources that offer protection in risky drinking contexts. In the context of the current intervention, students with higher anxiety, compared to those with higher levels of depression, appeared to be particularly amenable to implementing self-protective behaviors. These findings may reflect highly anxious students’ hyperarousal and feelings of distress about negative past events or future uncertainties; this anticipation and aversion to potential harm may motivate attempts to minimize risks for drinking-related negative outcomes. PBS skills training appears to be a promising avenue to encourage anxious women to incorporate learned strategies and avoid potential harm. However, more intense integrated interventions that address underlying affective issues may be needed for long-term efficacy.
Given the high prevalence rates of co-occurring anxiety and alcohol problems on college campuses (Cranford, Eisenberg, & Serras, 2009; Kushner & Sher, 1993), this intervention approach may be useful during periods of heightened stress (e.g., precollege orientations, final exam periods). Further, PBS skills training may be effectively incorporated into prevention protocols targeting students presenting at campus health or psychological centers— these students are at increased risk for not only anxiety, but heavy alcohol misuse (Center for the Study of Collegiate Mental Health, 2009; Napper et al., in press). Training counselors and affiliated personnel to discuss PBS and how best to implement them with those students screening positive for anxiety and alcohol problems may enable high-risk students to receive the treatment they need.
Although participants with low anxiety in the intervention (compared to low-anxiety control participants) reported greater PBS use at 6-months postintervention, this finding is best explained by control participants’ significant decreases in PBS use from baseline to 6-month follow-up. Perhaps this finding exposes a natural trajectory of decreased PBS use over the course of the first year of college in which women without anxiety may feel that they can manage their drinking without specific strategies. Yet, exposure to PBS skills training appears beneficial in counteracting trajectories of decreased PBS use over time in this subgroup. Women who are not under stress may have the resources and ability to effectively utilize and maintain a repertoire of learned PBS. In contrast, anxious women may lack the ability to sustain their use of newly learned skills, and thus may require enhanced intervention approaches, including in person or online booster sessions, or integrated interventions that address putative correlates of anxiety (for review, see Baker, Thornton, Hiles, Hides, & Lubman, 2012).
Effective approaches may necessitate that participants scrutinize their motives for drinking that interfere with PBS use and learn skills that can help them avoid risky drinking. For instance, discussing healthy coping behaviors (e.g., developing social support networks, conversational skills, or positive reframing; Dolan, Rohsenow, Martin, & Monti, 2013; Monti et al., 1989; Monti, Kadden, Rohsenow, Cooney, & Abrams 2002), highlighting substance-free alternative social activities (e.g., campus events that do not involve drinking; Murphy et al., 2012), and facilitating nonconformity (e.g., building drinking refusal self-efficacy; Goldsmith, Thompson, Black, Tran, & Smith, 2012) may help at-risk students develop skill sets to best implement PBS and avoid risky drinking. Among hazardous drinkers, those with high social anxiety report greater interest in attending a social anxiety workshop and trend toward greater interest in attending an alcohol workshop compared to peers with low social anxiety (Tran, Anthenelli, Smith, Corcoran, & Rofey, 2004). These findings highlight the potential for integrated interventions targeting this high-risk sub-group. Still, more research is needed to identify the role of mental health as it relates to PBS utilization and skills training interventions.
The current project is limited in a number of ways. Data relied on self-report measures, which may carry response bias, especially given their personal nature. However, we made all necessary efforts to ensure respondents that surveys were confidential, conforming to methods deemed valid and reliable in evaluating alcohol use (Maisto, Connors, & Allen, 1995). In addition, the fairly small, single-sex and single-site sample limits the generalizability of the findings. Nonetheless, these findings offer strong preliminary support for a novel intervention that is both low-cost and can be easily implemented in other settings. Future research is needed to replicate this study design with different subgroups of students (e.g., college males, athletic teams, Greeks houses). The prospective design was used to examine overall past month PBS use, alcohol use, and related consequences. Future studies utilizing event-level designs are needed to explicate the causal relationships among these variables. These studies would also clarify the effectiveness of specific types of PBS on drinking and consequences.
In sum, this study provides valuable data on the efficacy of a group cognitive–behavioral skills training intervention focused on PBS use and offers important insights into the role of mental health status in the adoption and use of PBS. Given recent data showing that individual PBS skills training may have limited effects on drinking outcomes (LaBrie et al., 2013; Martens et al., 2013), it is important to determine optimal modes of delivery for standalone PBS interventions, as well as student subgroups that will benefit most from this design. The current study demonstrates the efficacy of a group-based approach targeting first-year college women. The brief intervention delivered in person, and incorporating discussion and collaboration with same-sex peers may appeal to women. Further, group approaches have the added advantage of being less labor-intensive and more cost-effective than individual approaches, allowing more students to receive these preventive interventions. However, more research is needed to examine whether additional intervention components, such PBS boosters or other components taken from multicomponent interventions (e.g., motivational enhancement techniques, normative feedback, expectancy challenge, blood alcohol content information), would help increase intervention efficacy over the longer term. Nonetheless, these preliminary findings indicate that a PBS-specific brief group intervention design offers much potential to effectively reduce alcohol-related risk in college populations.
Acknowledgments
This research was supported by a grant from ABMRF/The Foundation for Alcohol Research and Grants R21AA020104-02 and T32AA007459 from the National Institute on Alcohol Abuse and Alcoholism.
Contributor Information
Shannon R. Kenney, Center for Alcohol and Addiction Studies, Brown University
Lucy E. Napper, Department of Psychology, Loyola Marymount University; Department of Psychology, Lehigh University
Joseph W. LaBrie, Department of Psychology, Loyola Marymount University
Matthew P. Martens, Department of Educational, School, and Counseling Psychology, University of Missouri
References
- Baer JS, Kivlahan DR, Donovan DM. Integrating skills training and motivational therapies. Implications for the treatment of substance dependence. Journal of Substance Abuse Treatment. 1999;17:15–23. doi: 10.1016/s0740-5472(98)00072-5. http://dx.doi.org/10.1016/S0740-5472(98)00072-5. [DOI] [PubMed] [Google Scholar]
- Baker AL, Thornton LK, Hiles S, Hides L, Lubman DI. Psychological interventions for alcohol misuse among people with co-occurring depression or anxiety disorders: A systematic review. Journal of Affective Disorders. 2012;139:217–229. doi: 10.1016/j.jad.2011.08.004. http://dx.doi.org/10.1016/j.jad.2011.08.004. [DOI] [PubMed] [Google Scholar]
- Barnett NP, Murphy JG, Colby SM, Monti PM. Efficacy of counselor vs. computer-delivered intervention with mandated college students. Addictive Behaviors. 2007;32:2529–2548. doi: 10.1016/j.addbeh.2007.06.017. http://dx.doi.org/10.1016/j.addbeh.2007.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. http://dx.doi.org/10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory Manual. The Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- Benton SL, Schmidt JL, Newton FB, Shin K, Benton SA, Newton DW. College student protective strategies and drinking consequences. Journal of Studies on Alcohol. 2004;65:115–121. doi: 10.15288/jsa.2004.65.115. [DOI] [PubMed] [Google Scholar]
- Bischof G, Rumpf HJ, Meyer C, Hapke U, John U. Gender differences in temptation to drink, self-efficacy to abstain and coping behavior in treated alcohol-dependent individuals: Controlling for severity of dependence. Addiction Research & Theory. 2005;13:129–136. http://dx.doi.org/10.1080/16066350412331335305. [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. http://dx.doi.org/10.1037/0021-843X.107.2.179. [DOI] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Henson JM, Maisto SA, DeMartini KS. Brief alcohol interventions for mandated college students: Comparison of face-to-face counseling and computer-delivered interventions. Addiction. 2011;106:528–537. doi: 10.1111/j.1360-0443.2010.03193.x. http://dx.doi.org/10.1111/j.1360-0443.2010.03193.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32:2469–2494. doi: 10.1016/j.addbeh.2007.05.004. http://dx.doi.org/10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for the Study of Collegiate Mental Health 2009 pilot study: Executive summary: Pennsylvania State University. 2009 Retrieved from http://ccmh.squarespace.com/publications/
- Center on Addiction and Substance Abuse . The formative years: Pathways to substance abuse among girls and young women ages 8-22. National Center on Addiction and Substance Abuse, Columbia University; New York, NY: 2003. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Erlbaum Publishers; Mahwah, NJ: 2003. [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. http://dx.doi.org/10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Agocha VB, Sheldon MS. A motivational perspective on risky behaviors: The role of personality and affect regulatory processes. Journal of Personality. 2000;68:1059–1088. doi: 10.1111/1467-6494.00126. http://dx.doi.org/10.1111/1467-6494.00126. [DOI] [PubMed] [Google Scholar]
- Cranford JA, Eisenberg D, Serras AM. Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addictive Behaviors. 2009;34:134–145. doi: 10.1016/j.addbeh.2008.09.004. http://dx.doi.org/10.1016/j.addbeh.2008.09.004. [DOI] [PubMed] [Google Scholar]
- Cronce JM, Larimer ME. Individual-focused approaches to the prevention of college student drinking. Alcohol Research & Health. 2011;34:210–221. [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Boluijt P, van Straten A. Screening of depression in adolescents through the Internet. European Child & Adolescent Psychiatry. 2008;17:32–38. doi: 10.1007/s00787-007-0631-2. http://dx.doi.org/10.1007/s00787-007-0631-2. [DOI] [PubMed] [Google Scholar]
- Delva J, Smith MP, Howell RL, Harrison DF, Wilke D, Jackson DL. A study of the relationship between protective behaviors and drinking consequences among undergraduate college students. Journal of American College Health. 2004;53:19–27. doi: 10.3200/JACH.53.1.19-27. http://dx.doi.org/10.3200/JACH.53.1.19-27. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach. Guilford Press; New York, NY, US: New York: 1999. [Google Scholar]
- Dolan SL, Rohsenow DJ, Martin RA, Monti PM. Urge-specific and lifestyle coping strategies of alcoholics: Relationships of specific strategies to treatment outcome. Drug and Alcohol Dependence. 2013;128:8–14. doi: 10.1016/j.drugalcdep.2012.07.010. http://dx.doi.org/10.1016/j.drugalcdep.2012.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldstein Ewing SW, Filbey FM, Chandler LD, Hutchison KE. Exploring the relationship between depressive and anxiety symptoms and neuronal response to alcohol cues. Alcoholism: Clinical and Experimental Research. 2010;34:396–403. doi: 10.1111/j.1530-0277.2009.01104.x. http://dx.doi.org/10.1111/j.1530-0277.2009.01104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillmore KM, Golding JM, Leino EV, Motoyoshi M, Shoemaker C, Terry H, Ferrer HP. Patterns and trends in women’s and men’s drinking. In: Wilsnack RW, Wilsnack SC, editors. Gender and alcohol: Individual and social perspectives. Rutgers Center of Alcohol Studies; Piscataway, NJ: 1997. pp. 21–48. [Google Scholar]
- Fydrich T, Dowdall D, Chambless DL. Reliability and validity of the Beck Anxiety Inventory. Journal of Anxiety Disorders. 1992;6:55–61. http://dx.doi.org/10.1016/0887-6185(92)90026-4. [Google Scholar]
- Gleason NA. Preventing alcohol abuse by college women: A relational perspective 2. Journal of American College Health. 1994;43:15–24. doi: 10.1080/07448481.1994.9939079. http://dx.doi.org/10.1080/07448481.1994.9939079. [DOI] [PubMed] [Google Scholar]
- Goldsmith AA, Thompson RD, Black JJ, Tran GQ, Smith JP. Drinking refusal self-efficacy and tension-reduction alcohol expectancies moderating the relationship between generalized anxiety and drinking behaviors in young adult drinkers. Psychology of Addictive Behaviors. 2012;26:59–67. doi: 10.1037/a0024766. http://dx.doi.org/10.1037/a0024766. [DOI] [PubMed] [Google Scholar]
- Grucza RA, Norberg KE, Bierut LJ. Binge drinking among youths and young adults in the United States: 1979-2006. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48:692–702. doi: 10.1097/CHI.0b013e3181a2b32f. http://dx.doi.org/10.1097/CHI.0b013e3181a2b32f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines MP, Barker G, Rice RM. The personal protective behaviors of college student drinkers: Evidence of indigenous protective norms. Journal of American College Health. 2006;55:69–76. doi: 10.3200/JACH.55.2.69-76. http://dx.doi.org/10.3200/JACH.55.2.69-76. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; New York, NY: 2013. [Google Scholar]
- Hingson R, Heeren T, Winter M, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18-24: Changes from 1998 to 2001. Annual Review of Public Health. 2005;26:259–279. doi: 10.1146/annurev.publhealth.26.021304.144652. http://dx.doi.org/10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18-24, 1998-2005. Journal of Studies on Alcohol and Drugs. 2009;70:12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karwacki SB, Bradley JR. Coping, drinking motives, goal attainment expectancies and family models in relation to alcohol use among college students. Journal of Drug Education. 1996;26:243–255. doi: 10.2190/A1P0-J36H-TLMJ-0L32. http://dx.doi.org/10.2190/A1P0-J36H-TLMJ-0L32. [DOI] [PubMed] [Google Scholar]
- Kenney SR, LaBrie JW. Use of protective behavioral strategies and reduced alcohol risk: Examining the moderating effects of mental health, gender, and race. Psychology of Addictive Behaviors. 2013;27:997–1009. doi: 10.1037/a0033262. http://dx.doi.org/10.1037/a0033262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivlahan DR, Marlatt GA, Fromme K, Coppel DB, Williams E. Secondary prevention with college drinkers: Evaluation of an alcohol skills training program. Journal of Consulting and Clinical Psychology. 1990;58:805–810. doi: 10.1037//0022-006x.58.6.805. http://dx.doi.org/10.1037/0022-006X.58.6.805. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ. Comorbidity of alcohol and anxiety disorders among college students: Effects of gender and family history of alcoholism. Addictive Behaviors. 1993;18:543–552. doi: 10.1016/0306-4603(93)90070-p. http://dx.doi.org/10.1016/0306-4603(93)90070-P. [DOI] [PubMed] [Google Scholar]
- Labouvie E, Bates ME. Reasons for alcohol use in young adulthood: Validation of a three-dimensional measure. Journal of Studies on Alcohol. 2002;63:145–155. doi: 10.15288/jsa.2002.63.145. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Lac A. The use of protective behavioral strategies is related to reduced risk in heavy drinking college students with poorer mental and physical health. Journal of Drug Education. 2010;40:361–378. doi: 10.2190/DE.40.4.c. http://dx.doi.org/10.2190/DE.40.4.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Lac A, Garcia JA, Ferraiolo P. Mental and social health impacts the use of protective behavioral strategies in reducing risky drinking and alcohol consequences. Journal of College Student Development. 2009;50:35–49. doi: 10.1353/csd.0.0050. http://dx.doi.org/10.1353/csd.0.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Napper LE. The efficacy of a standalone protective behavioral strategies alcohol intervention among students with poorer mental health; Paper presented at the Research Society on Alcoholism; Orlando, FL. 2013; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999-2006. Addictive Behaviors. 2007;32:2439–2468. doi: 10.1016/j.addbeh.2007.05.006. http://dx.doi.org/10.1016/j.addbeh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM, Lee CM, Kilmer JR. Brief intervention in college settings. Alcohol Research & Health. 2004;28:94–104. [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Lee CM, Kilmer JR, Fabiano PM, Stark CB, Geisner IM, Neighbors C. Personalized mailed feedback for college drinking prevention: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2007;75:285–293. doi: 10.1037/0022-006X.75.2.285. http://dx.doi.org/10.1037/0022-006X.75.2.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Turner AP, Anderson BK, Fader JS, Kilmer JR, Palmer RS, Cronce JM. Evaluating a brief alcohol intervention with fraternities. Journal of Studies on Alcohol. 2001;62:370–380. doi: 10.15288/jsa.2001.62.370. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Connors GJ, Allen JP. Contrasting self-report screens for alcohol problems: A review. Alcoholism: Clinical and Experimental Research. 1995;19:1510–1516. doi: 10.1111/j.1530-0277.1995.tb01015.x. http://dx.doi.org/10.1111/j.1530-0277.1995.tb01015.x. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, Williams E. Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment. Journal of Consulting and Clinical Psychology. 1998;66:604–615. doi: 10.1037//0022-006x.66.4.604. http://dx.doi.org/10.1037/0022-006X.66.4.604. [DOI] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Cimini MD. Do protective behavioral strategies mediate the relationship between drinking motives and alcohol use in college students? Journal of Studies on Alcohol and Drugs. 2007;68:106–114. doi: 10.15288/jsad.2007.68.106. [DOI] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Sheehy MJ, Corbett K, Anderson DA, Simmons A. Development of the Protective Behavioral Strategies Survey. Journal of Studies on Alcohol. 2005;66:698–705. doi: 10.15288/jsa.2005.66.698. [DOI] [PubMed] [Google Scholar]
- Martens MP, Pederson ER, LaBrie JW, Ferrier AG, Cimini MD. Measuring alcohol-related protective behavioral strategies among college students: Further examination of the Protective Behavioral Strategies Scale. Psychology of Addictive Behaviors. 2007;21:307–315. doi: 10.1037/0893-164X.21.3.307. http://dx.doi.org/10.1037/0893-164X.21.3.307. [DOI] [PubMed] [Google Scholar]
- Martens MP, Smith AE, Murphy JG. The efficacy of single-component brief motivational interventions among at-risk college drinkers. Journal of Consulting and Clinical Psychology. 2013;81:691–701. doi: 10.1037/a0032235. http://dx.doi.org/10.1037/a0032235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Taylor KK, Damann KM, Page JC, Mowry ES, Cimini MD. Protective behavioral strategies when drinking alcohol and their relationship to negative alcohol-related consequences in college students. Psychology of Addictive Behaviors. 2004;18:390–393. doi: 10.1037/0893-164X.18.4.390. http://dx.doi.org/10.1037/0893-164X.18.4.390. [DOI] [PubMed] [Google Scholar]
- McDowell I. Measuring health: A guide to rating scales and questionnaires. Oxford University Press; New York, NY: 2006. http://dx.doi.org/10.1093/acprof:oso/9780195165678.001.0001. [Google Scholar]
- Monti PM, Abrams DB, Kadden RM, Cooney NL. Treating alcohol dependence: A coping skills training guide. Guilford Press; New York, NY: 1989. [Google Scholar]
- Monti PM, Kadden RM, Rohsenow DJ, Cooney NL, Abrams DB. Treating alcohol dependence: A coping skills training guide. 2nd ed. Guilford Press; New York, NY: 2002. [Google Scholar]
- Monti PM, Rohsenow DJ, Hutchison KE. Toward bridging the gap between biological, psychobiological and psychosocial models of alcohol craving. Addiction. 2000;95:S229–S236. doi: 10.1080/09652140050111799. http://dx.doi.org/10.1046/j.1360-0443.95.8s2.11.x. [DOI] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, Martens MP. A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology. 2012;80:876–886. doi: 10.1037/a0028763. http://dx.doi.org/10.1037/a0028763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napper LE, Hummer J, LaBrie JW. Anxiety and the use of alcohol related protective behavioral strategies. Journal of College Counseling. doi: 10.1002/j.2161-1882.2015.00066.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism . A call to action: Changing the culture of drinking at U.S. colleges. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 2002. NIH publication no. 02-5010. [Google Scholar]
- Neighbors C, Larimer ME, Lewis MA. Targeting misperceptions of descriptive drinking norms: Efficacy of a computer-delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology. 2004;72:434–447. doi: 10.1037/0022-006X.72.3.434. http://dx.doi.org/10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- Nelson TF, Xuan Z, Lee H, Weitzman ER, Wechsler H. Persistence of heavy drinking and ensuing consequences at heavy drinking colleges. Journal of Studies on Alcohol and Drugs. 2009;70:726–734. doi: 10.15288/jsad.2009.70.726. [DOI] [PubMed] [Google Scholar]
- O’Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. Journal of Studies on Alcohol. 2002;14:23–39. doi: 10.15288/jsas.2002.s14.23. [DOI] [PubMed] [Google Scholar]
- Pace TM, Trapp CM. A psychometric comparison of the Beck Depression Inventory and the Inventory for Diagnosing Depression in a college population. Assessment. 1995;2:167–172. [Google Scholar]
- Park CL, Grant C. Determinants of positive and negative consequences of alcohol consumption in college students: Alcohol use, gender, and psychological characteristics. Addictive Behaviors. 2005;30:755–765. doi: 10.1016/j.addbeh.2004.08.021. http://dx.doi.org/10.1016/j.addbeh.2004.08.021. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20:149–166. doi: 10.1007/BF01537606. http://dx.doi.org/10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Santor DA, Zuroff DC, Ramsay JO, Cervantes P, Palacios J. Examining scale discriminability in the BDI and CES-D as a function of depressive severity. Psychological Assessment. 1995;7:131–139. http://dx.doi.org/10.1037/1040-3590.7.2.131. [Google Scholar]
- Schulenberg J, Maggs JL, Long SW, Sher KJ, Gotham HJ, Baer JS, Zucker RA. The problem of college drinking: Insights from a developmental perspective. Alcoholism: Clinical and Experimental Research. 2001;25:473–477. http://dx.doi.org/10.1111/j.1530-0277.2001.tb02237.x. [PubMed] [Google Scholar]
- Silverman MM. College student suicide prevention: Background and blueprint for action. Student Health Spectrum. 2004:13–20. [Google Scholar]
- Ståhlbrandt H, Johnsson KO, Berglund M. Two-year outcome of alcohol interventions in Swedish university halls of residence: A cluster randomized trial of a brief skills training program, twelve-step-influenced intervention, and controls. Alcoholism: Clinical and Experimental Research. 2007;31:458–466. doi: 10.1111/j.1530-0277.2006.00327.x. http://dx.doi.org/10.1111/j.1530-0277.2006.00327.x. [DOI] [PubMed] [Google Scholar]
- Sugarman DE, Carey KB. The relationship between drinking control strategies and college student alcohol use. Psychology of Addictive Behaviors. 2007;21:338–345. doi: 10.1037/0893-164X.21.3.338. http://dx.doi.org/10.1037/0893-164X.21.3.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugarman DE, Carey KB. Drink less or drink slower: The effects of instruction on alcohol consumption and drinking control strategy use. Psychology of Addictive Behaviors. 2009;23:577–585. doi: 10.1037/a0016580. http://dx.doi.org/10.1037/a0016580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran GQ, Anthenelli RM, Smith JP, Corcoran KJ, Rofey DL. Alcohol use, cognitive correlates of drinking and change readiness in hazardous drinkers with high versus low social anxiety. Journal of Studies on Alcohol. 2004;65:715–724. doi: 10.15288/jsa.2004.65.715. [DOI] [PubMed] [Google Scholar]
- Velasquez MM, Maurer GG, Crouch C, DiClemente CC. Group treatment for substance abuse: A stages-of-change therapy manual. Guilford Press; New York, NY: 2001. [Google Scholar]
- Walitzer KS, Sher KJ. A prospective study of self-esteem and alcohol use disorders in early adulthood: Evidence for gender differences. Alcoholism: Clinical and Experimental Research. 1996;20:1118–1124. doi: 10.1111/j.1530-0277.1996.tb01956.x. http://dx.doi.org/10.1111/j.1530-0277.1996.tb01956.x. [DOI] [PubMed] [Google Scholar]
- Walters ST, Roudsari BS, Vader AM, Harris TR. Correlates of protective behavior utilization among heavy-drinking college students. Addictive Behaviors. 2007;32:2633–2644. doi: 10.1016/j.addbeh.2007.06.022. http://dx.doi.org/10.1016/j.addbeh.2007.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease. 2004;192:269–277. doi: 10.1097/01.nmd.0000120885.17362.94. http://dx.doi.org/10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Young AM, Morales M, McCabe SE, Boyd CJ, Darcy H. Drinking like a guy: Frequent binge drinking among undergraduate women. Substance Use & Misuse. 2005;40:241–267. doi: 10.1081/ja-200048464. http://dx.doi.org/10.1081/JA-200048464. [DOI] [PubMed] [Google Scholar]