Abstract
Data on the prevalence of psychiatric disorders in late life are lacking. The present study addresses this gap in the literature by examining the prevalence of the broadest range of psychiatric disorders in late life to date; comparing prevalences across older adult age groups using the largest sample of adults aged 85+; and exploring gender differences in the prevalence of psychiatric disorders in late life. Using data from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions, we examined the prevalence of past-year mood, anxiety, and substance use disorders, and lifetime personality disorders in a nationally representative sample of 12,312 U.S. older adults. We stratified our analyses by gender and by older age groups: young-old (ages 55-64), middle-old (ages 65-74), old-old (ages 75-84), and oldest-old (ages 85+). The proportion of older adults who experienced any past-year anxiety disorder was 11.4%, while the prevalence of any past-year mood disorder was 6.8%. A total of 3.8% of older adults met criteria for any past-year substance use disorder, and 14.5% of older adults had one or more personality disorder. We observed a general pattern of decreasing rates of psychiatric disorders with increasing age. Women experienced higher rates of mood and anxiety disorders, while men had higher rates of substance use disorders and any personality disorder. Gender differences in rates of most psychiatric disorders decreased with increasing age. These data indicate that psychiatric disorders are prevalent among U.S. older adults, and support the importance of prevention, diagnosis, and treatment of psychiatric disorders in this population.
Keywords: Psychiatric disorders, anxiety disorders, mood disorders, substance use disorders, personality disorders, older adults, oldest-old
We are in the midst of a global demographic shift in population aging, a trend that is the first of its kind in the evolution of the human species (1). In the U.S., the proportion of adults aged 65 years and older is projected to increase from 13% of the population in 2010 to 16% by 2020. Furthermore, the gender gap in life expectancy, with women living longer than men, is narrowing over time (1).
There is current debate in the literature regarding whether prevalence rates of psychiatric disorders increase or decrease in later life. Extant epidemiologic research has primarily focused on trends of psychiatric disorders across the entire adult lifespan, and results have been mixed with respect to the effect of age on the prevalence of disorders.
Research studies using primarily smaller, community-based samples have found that rates of mood disorders increase across the adult lifespan (2–4), while other studies have observed a U-shaped relationship, with the highest prevalence of these disorders among younger and older adults, compared to middle-aged adults (5–7).
In contrast, other studies have shown a reversed U-shaped relationship between age and well-being across the adult lifespan, with increased well-being in young and older adults and decreased well-being in middle-aged adults (8,9). In line with this finding, the literature provides the strongest support for decreased prevalence of mood, anxiety, and substance use disorders in late life (10). This trend of decreased prevalence of psychiatric disorders is corroborated by data from the U.S. Epidemiologic Catchment Area Survey, which indicated a linear decrease in DSM-III psychiatric disorders (excluding dementia) across the adult lifespan (11). Further, data from the National Comorbidity Survey – Replication (NCS-R) revealed that the prevalence of past-year and lifetime DSM-IV mood, anxiety, and substance use disorders were lower for older adults (65+) compared to younger age groups (ages 18-64) (12).
Data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) demonstrated similar trends when comparing the prevalence of personality disorders among older and younger adults (13). Data from a Canadian population-based sample further supports a pattern of decreased rates of major depression, bipolar disorder, social phobia, agoraphobia, and panic disorder in late life (14).
Research focused on examining trends of psychiatric disorders among older age groups is limited. Specifically, there is a significant dearth of epidemiological research that examines demographic trends of psychiatric disorders across late-life age groups, as several extant data sets do not have adequate sample sizes, particularly of the oldest-old segment of the population (aged 85+).
In a recent study exploring the prevalence of a broad range of psychiatric disorders across older adult age groups, Byers et al (15) found a general decline in the prevalence of DSM-IV past-year mood and anxiety disorders among individuals aged 55+ who participated in the NCS-R. While informative in characterizing the prevalence of mood and anxiety disorders in older adults, the prevalence of past-year substance use disorders and lifetime personality disorders, and gender-stratified analyses were not reported in this study. Furthermore, the sample size of older adults in the oldest-old age group (85+) was small (N+122).
A small body of research has examined gender differences across late-life psychiatric disorders. Existing data is limited to depression, with the majority of studies indicating that gender differences in the prevalence of this disorder (i.e., higher rates in women) decrease with increasing age (16–20).
To address these gaps in the literature, we analyzed data from a large, nationally representative study of the U.S. adult population. Our aims were: a) to examine the prevalence of the broadest range of psychiatric disorders in the literature to date, including mood, anxiety, substance use, and personality disorders, as well as mental health-related quality of life among adults aged 55+; b) to compare the prevalence of psychiatric disorders across older adult age groups, including the largest extant sample of community-based older adults aged 85+; and c) to examine the relationship between gender and prevalence of late-life psychiatric disorders.
METHODS
Sample and procedure
We analyzed data from Wave 2 of the NESARC, conducted by the National Institute on Alcohol Abuse and Alcoholism between 2004 and 2005. Wave 2 was a follow-up survey to Wave 1, which was conducted between 2001 and 2002. We chose to analyze data from Wave 2 because the first wave did not assess post-traumatic stress disorder (PTSD) or borderline, schizotypal, and narcissistic personality disorders.
Wave 2 of the NESARC surveyed a nationally representative sample of community-dwelling American adults aged 20 years and older residing in the U.S., including the District of Columbia, Alaska, and Hawaii. The sample excluded adults who were deceased, deported, institutionalized, or on active military duty. The response rate was 86.7%, which was the proportion of Wave 1 participants who responded in Wave 2, resulting in a total sample size of 34,653. Consistent with prior geropsychiatry research (21–23), we restricted our analyses to older adults aged 55+, which resulted in a subsample of 12,312 respondents. We compared young-old (55-64; N+5,135), middle-old (65-74; N+3,634), old-old (75-84; N+2,673), and oldest-old (85+; N+870) age groups.
Trained lay interviewers from the U.S. Census Bureau with at least five years of experience conducted face-to-face lay interviews, and all participants provided written informed consent. The U.S. Census Bureau and the U.S. Office of Management and Budget reviewed the research protocol and provided full ethical approval. A more detailed description of methodology and sampling procedures of the NESARC can be found elsewhere (24–26).
Assessments
Psychiatric disorders
The NESARC used the Alcohol Use Disorders and Associated Disabilities Interview Schedule IV (AUDADIS-IV), a reliable and valid instrument designed for lay interviewers to assess DSM-IV psychiatric disorders. The reliability for the AUDADIS-IV ranges from good to excellent across all assessed psychiatric disorders, as detailed elsewhere (26,27).
We examined past-year diagnoses of mood (i.e., major depression, dysthymia, and mania or hypomania), anxiety (i.e., panic disorder with and without agoraphobia, social phobia, specific phobia, generalized anxiety disorder, and PTSD), and substance use (i.e., alcohol abuse and dependence, drug abuse and dependence, and nicotine dependence) disorders. In addition to examining these psychiatric disorders individually, we also generated any mood, anxiety, and substance use categories to assess the prevalence of being diagnosed with at least one psychiatric disorder within each category. We analyzed nicotine dependence individually and did not include it in the any substance use disorder category.
Wave 2 of the NESARC included all ten DSM-IV personality disorders: borderline, antisocial, avoidant, dependent, obsessive-compulsive, paranoid, schizoid, histrionic, schizotypal, and narcissistic. In light of empirical support for the classification of personality disorders into clusters A, B, and C using the AUDADIS-IV (28), we further categorized personality disorders into DSM-IV cluster A – odd or eccentric disorders (i.e., paranoid, schizoid, and schizotypal), cluster B – dramatic, emotional, or erratic disorders (i.e., antisocial, borderline, histrionic, and narcissistic), and cluster C – anxious or fearful disorders (i.e., avoidant, dependent, and obsessive-compulsive). We also included an any personality disorder category.
Finally, we created a continuous number of psychiatric disorders variable based on number of diagnosed mood, anxiety, substance use, and personality disorders.
Socio-demographic variables
We included the following socio-demographic variables: age, gender, ethnicity, education, household income, and marital status. We categorized age into four groups (young-old, middle-old, old-old, and oldest-old), as indicated above. We further categorized ethnicity (White, Black, American Indian/Alaska Native, Asian/Native Hawaiian/Other Pacific Islander, and Hispanic), education (less than high school, high school, some college or higher), household income ($0-$19,999, $20,000-$34,999, $35,000-$59,999, and $60,000+), and marital status (married or living with someone as if married, widowed/separated/divorced, never married).
Mental health-related quality of life
We derived a mental health component score (MCS-12) from the Short-Form Health Survey (SF-12, 29) as a measure of mental health-related quality of life, with higher scores indicating better mental health-related quality of life. Prior research indicates that the MCS-12 has good reliability and validity. Specifically, scores on the MCS-12 correlate strongly with scores on the MCS-36 and have high test-retest reliability (r+0.76) (29).
Statistical analysis
We conducted cross-tabulations to compare the weighted prevalence of socio-demographic variables across the any disorder categories (i.e., any mood, anxiety, substance use, and personality disorders). We then conducted chi-square analyses to evaluate whether socio-demographic characteristics differed among disorder categories. We also conducted cross-tabulations and chi-square analyses to establish the prevalence of all psychiatric disorders across the older adult age groups (i.e., young-old, middle-old, old-old, and oldest-old), and the presence of significant differences among these groups. We further stratified these prevalence estimates by gender.
We conducted bivariate and multivariate logistic regressions to examine the relationship between each older adult age group and the any psychiatric disorder categories, with older adults aged 85+ serving as the reference group. We report unadjusted logistic regression models, as well as models adjusted for socio-demographics.
We analyzed data using SUDAAN 10.0.1 (30), which employs the Taylor Series Linearization method (31) for variance estimation to account for the complex sampling design of the NESARC. We applied appropriate weighting and stratification variables to these data to ensure generalizability to the U.S. adult population. The statistical weights adjusted the data for socio-demographic variables, response/non-response, and oversampling of Blacks and Hispanics based on the 2000 Census.
RESULTS
Table1 presents cross-tabulations and results of chi-square analyses of socio-demographic characteristics and weighted DSM-IV prevalence of any past-year mood, anxiety, and substance use disorder, and any lifetime personality disorder. The prevalence of disorders differed significantly by gender, ethnicity, education, household income, and marital status. Specifically, women had significantly higher rates of any past-year mood and anxiety disorder, whereas men had significantly higher rates of any past-year substance use disorder and any lifetime personality disorder.
Table 1.
Socio-demographic variables in 12,312 adults aged 55 years and older by DSM-IV psychiatric disorders
| N (weighted %) | Any past-year mood disorder N (weighted %) | Any past-year anxiety disorder N (weighted %) | Any past-year substance use disorder N (weighted %) | Any lifetime personality disorder N (weighted %) | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 4938 (45.01) | 248 (4.49) | 417 (7.90) | 345 (6.62) | 868 (16.79) |
| Female | 7374 (54.99) | 666 (8.64) | 1092 (14.24) | 105 (1.40) | 1045 (12.68) |
| χ2 (df) | 58.59 (1)*** | 64.49 (1)*** | 92.43 (1)*** | 29.23 (1)*** | |
| Ethnicity | |||||
| White (non-Hispanic) | 8117 (79.25) | 567 (6.53) | 950 (11.10) | 321 (3.91) | 1154 (13.67) |
| Black (non-Hispanic) | 2268 (8.90) | 158 (6.56) | 295 (12.59) | 70 (3.59) | 441 (19.36) |
| American Indian/Alaska Native (non-Hispanic) | 207 (2.26) | 24 (9.75) | 36 (15.86) | 8 (2.95) | 54 (23.99) |
| Asian/Native Hawaiian/Other Pacific Islander (non-Hispanic) | 232 (3.24) | 16 (5.83) | 17 (7.74) | 3 (1.74) | 23 (9.45) |
| Hispanic | 1488 (6.34) | 149 (9.48) | 211 (13.59) | 48 (3.25) | 241 (17.67) |
| χ2 (df) | 2.47 (4) | 3.37 (4)* | 0.87 (4) | 5.89 (4)*** | |
| Education | |||||
| Less than high school | 2867 (19.69) | 261 (7.97) | 370 (12.79) | 82 (2.91) | 431 (14.75) |
| High school | 3780 (31.83) | 256 (6.35) | 475 (11.45) | 117 (3.07) | 524 (13.12) |
| Some college or more | 5665 (48.48) | 397 (6.56) | 664 (10.78) | 251 (4.53) | 958 (15.37) |
| χ2 (df) | 2.67 (2) | 2.38 (2) | 8.83 (2)*** | 3.49 (2)* | |
| Household income | |||||
| $0-$19,999 | 4197 (26.36) | 407 (9.63) | 585 (13.51) | 99 (2.36) | 705 (16.61) |
| $20,000-$34,999 | 2786 (22.48) | 194 (6.61) | 335 (11.51) | 71 (2.35) | 411 (13.34) |
| $35,000-$59,999 | 2642 (24.09) | 180 (6.49) | 301 (10.87) | 133 (5.00) | 405 (14.52) |
| $60,000+ | 2687 (27.06) | 133 (4.38) | 288 (9.69) | 147 (5.15) | 392 (13.50) |
| χ2 (df) | 11.16 (3)*** | 4.33 (3)** | 11.72 (3)*** | 3.81 (3)* | |
| Marital status | |||||
| Married/cohabiting | 6180 (64.22) | 358 (5.39) | 611 (10.09) | 233 (3.90) | 886 (13.66) |
| Widowed/separated/divorced | 5347 (31.44) | 489 (9.46) | 763 (14.15) | 183 (3.23) | 886 (15.93) |
| Never married | 785 (4.35) | 67 (7.76) | 85 (10.57) | 34 (5.19) | 141 (17.22) |
| χ2 (df) | 20.19 (2)*** | 14.09 (2)*** | 2.14 (2) | 4.62 (2)* |
p<0.05
p<0.01
p<0.001
Table2 shows weighted prevalences of DSM-IV psychiatric disorders among subgroups of older adults aged 55+. The prevalence of any past-year mood disorder was 6.8%, the most prevalent of which was major depression (5.6%). A higher proportion of older adults reported any past-year anxiety disorder (11.4%), the most prevalent of which was specific phobia (5.8%). The prevalence of any past-year substance use disorder among older adults was 3.8%. A total of 14.5% of older adults met criteria for at least one personality disorder, the most prevalent of which was obsessive-compulsive personality disorder (6.5%).
Table 2.
Prevalence of DSM-IV psychiatric disorders and mental health-related quality of life among adults aged 55 years and older
| Total N (weighted %) | Age 55–64 N (weighted %) | Age 65–74 N (weighted %) | Age 75–84 N (weighted %) | Age 85+ N (weighted %) | χ2 (df) | |
|---|---|---|---|---|---|---|
| Mood disorders | ||||||
| Major depression | 751 (5.63) | 420 (7.41) | 184 (4.58) | 107 (3.87) | 40 (4.23) | 13.06 (3)*** |
| Dysthymia | 138 (0.94) | 87 (1.34) | 27 (0.67) | 17 (0.54) | 7 (0.77) | 4.80 (3)** |
| Mania or hypomania | 207 (1.49) | 131 (2.27) | 49 (1.26) | 23 (0.53) | 4 (0.50) | 10.24 (3)*** |
| Any mood disorder | 914 (6.77) | 518 (9.02) | 228 (5.68) | 128 (4.48) | 40 (4.23) | 17.28 (3)*** |
| Anxiety disorders | ||||||
| Panic disorder | 185 (1.35) | 120 (2.02) | 34 (0.91) | 23 (0.77) | 8 (0.74) | 6.10 (3)** |
| Social phobia | 205 (1.45) | 129 (2.14) | 42 (1.08) | 28 (0.83) | 6 (0.49) | 11.14 (3)*** |
| Specific phobia | 766 (5.79) | 432 (7.74) | 200 (4.91) | 106 (3.84) | 28 (3.12) | 12.84 (3)*** |
| Generalized anxiety disorder | 353 (2.80) | 206 (3.73) | 84 (2.28) | 45 (1.78) | 18 (2.20) | 5.11 (3)** |
| Post-traumatic stress disorder | 484 (3.48) | 281 (4.67) | 109 (2.75) | 80 (2.59) | 14 (1.76) | 10.31 (3)*** |
| Any anxiety disorder | 1509 (11.39) | 831 (14.81) | 379 (9.45) | 239 (8.40) | 60 (7.15) | 18.76 (3)*** |
| Substance use disorders | ||||||
| Alcohol abuse/dependence | 418 (3.48) | 283 (5.58) | 93 (2.39) | 40 (1.73) | 2 (0.06) | 34.06 (3)*** |
| Any drug abuse/dependence | 50 (0.42) | 42 (0.84) | 7 (0.19) | 0 (0.00) | 1 (0.10) | 7.93 (3)*** |
| Any substance use disorder | 450 (3.75) | 308 (6.07) | 99 (2.57) | 40 (1.73) | 3 (0.15) | 39.24 (3)*** |
| Nicotine dependence | 1123 (9.29) | 710 (14.02) | 310 (8.49) | 90 (3.15) | 13 (1.36) | 43.47 (3)*** |
| Personality disorders | ||||||
| Borderline | 449 (3.16) | 278 (4.66) | 106 (2.54) | 53 (1.58) | 12 (1.19) | 13.82 (3)*** |
| Antisocial | 176 (1.64) | 119 (2.59) | 43 (1.34) | 12 (0.59) | 2 (0.13) | 19.96 (3)*** |
| Avoidant | 172 (1.30) | 111 (1.95) | 38 (0.94) | 15 (0.58) | 8 (0.87) | 6.67 (3)*** |
| Dependent | 37 (0.26) | 22 (0.36) | 8 (0.14) | 6 (0.24) | 1 (0.19) | 1.55 (3) |
| Obsessive-compulsive | 779 (6.53) | 401 (7.64) | 219 (6.33) | 118 (4.90) | 41 (5.39) | 5.53 (3)** |
| Paranoid | 339 (2.30) | 197 (3.17) | 90 (2.02) | 39 (1.24) | 13 (1.34) | 7.84 (3)*** |
| Schizoid | 286 (2.20) | 157 (2.83) | 73 (1.80) | 49 (1.77) | 7 (1.13) | 4.60 (3)** |
| Histrionic | 105 (0.70) | 59 (0.89) | 29 (0.67) | 11 (0.39) | 6 (0.58) | 3.13 (3)* |
| Schizotypal | 364 (2.40) | 222 (3.53) | 74 (1.53) | 53 (1.69) | 15 (1.05) | 11.97 (3)*** |
| Narcissistic | 566 (3.91) | 303 (4.90) | 148 (3.43) | 88 (2.95) | 27 (2.61) | 5.95 (3)** |
| Any cluster A | 809 (5.56) | 458 (7.52) | 200 (4.40) | 121 (4.03) | 30 (2.75) | 15.10 (3)*** |
| Any cluster B | 1013 (7.51) | 579 (10.17) | 265 (6.57) | 137 (4.75) | 39 (3.93) | 20.42 (3)*** |
| Any cluster C | 890 (7.36) | 471 (8.87) | 242 (6.89) | 131 (5.34) | 46 (5.97) | 7.97 (3)*** |
| Any personality disorder | 1913 (14.53) | 1018 (18.14) | 519 (13.24) | 294 (10.36) | 88 (10.67) | 20.49 (3)*** |
| Number of mental disorders (mean, SE) | 0.84 (0.02) | 0.50 (0.02) | 0.36 (0.02) | 0.30 (0.03) | Wald F+108.32*** | |
| Mental health-related quality of life (mean, SE) | 52.12 (0.18) | 52.99 (0.20) | 51.93 (0.24) | 50.89 (0.52) | Wald F+7.09*** |
p<0.05
p<0.01
p<0.001
Chi-square analyses indicated that, with the exception of dependent personality disorder, all past-year and lifetime psychiatric disorders differed significantly across late-life age groups. We observed an overall pattern of decreasing rates of mood, anxiety, substance use, and personality disorders with increasing age. We noted slight, non-significant upturns in prevalence rates of past-year major depression, dysthymia, generalized anxiety disorder, and any drug abuse/dependence as well as several lifetime personality disorders from ages 75-84 to ages 85+. The mean number of psychiatric disorders decreased significantly throughout the older adult lifespan, with adults aged 55-64 having the highest number of comorbid disorders. There was a significant difference in mental health-related quality of life across late-life age groups, with a pattern of higher quality of life among adults aged 55-74, and lower quality of life among adults aged 75-85+.
Table3 presents unadjusted and adjusted logistic regression models examining odds ratios of any DSM-IV past-year mood, anxiety, and substance use disorder and any lifetime personality disorder. Results of these analyses revealed that, as age increased, the odds of mood, anxiety, substance use, and personality disorders decreased. This relationship was especially pronounced for young-old (55-64) and middle-old adults (65-74), who, in adjusted models, had significantly greater odds of having any past-year mood disorder, anxiety disorder, and substance use disorder, and any lifetime personality disorder compared to the oldest-old adult age group (85+).
Table 3.
Odds ratios of having a diagnosis of any DSM-IV past-year mood, anxiety, and substance use disorder and any lifetime personality disorder among young-old, middle-old, and old-old adults compared to the oldest-old (85+) reference group
| Unadjusted odds ratios (95% CI) | Adjusted odds ratios (95% CI) | |||||
|---|---|---|---|---|---|---|
| Young-old (55-64) adults | Middle-old (65-74) adults | Old-old (75-84) adults | Young-old (55-64) adults | Middle-old (65-74) adults | Old-old (75-84) adults | |
| Any mood disorder | 2.25 (1.54-3.28)*** | 1.36 (0.92-2.02) | 1.06 (0.68-1.67) | 4.11 (2.77-6.10)*** | 2.01 (1.35-2.99)*** | 1.30 (0.82-2.05) |
| Any anxiety disorder | 2.26 (1.65-3.09)*** | 1.36 (0.98-1.87) | 1.19 (0.84-1.68) | 3.38 (2.43-4.70)*** | 1.77 (1.26-2.47)** | 1.38 (0.97-1.97) |
| Any substance use disorder | 41.96 (10.42-168.96)*** | 17.14 (4.05-72.60)*** | 11.47 (2.73-48.15)** | 38.09 (9.62-150.85)*** | 16.49 (3.95-68.88)*** | 11.23 (2.71-46.62)** |
| Any personality disorder | 1.85 (1.36-2.52)*** | 1.27 (0.92-1.74) | 0.96 (0.69-1.36) | 2.25 (1.63-3.09)*** | 1.44 (1.04-1.99)* | 1.03 (0.73-1.45) |
p<0.05
p<0.01
p<0.001
Table4 displays weighted prevalence estimates of DSM-IV past-year psychiatric disorders by gender and late-life age group. Across the older adult lifespan, from the ages of 55 to 84, women had higher prevalence rates of past-year mood and anxiety disorders. Men had higher rates of all past-year substance use disorders across this age range in addition to any personality disorder. We observed an overall pattern of narrowing gender differences in the prevalence of psychiatric disorders with increasing age. Figure 1 illustrates this pattern for any past-year mood and anxiety disorders. When examining the oldest-old (85+) age group, the previously observed gender differences in prevalence estimates among adults ages 55-84 dissipated, and in some cases, reversed. Specifically, for adults 85 years and older, men had higher prevalence rates of all past-year mood disorders, as well as past-year PTSD and any anxiety disorder.
Table 4.
Prevalence of DSM-IV psychiatric disorders by gender among adults aged 55 years and older
| Total N (weighted %) | 55–64 N (weighted %) | 65–74 N (weighted %) | 75–84 N (weighted %) | 85+N (weighted %) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | |
| Mood disorders | ||||||||||
| Major depression | 197 (3.62) | 554 (7.27) | 110 (4.59) | 310 (10.05) | 44 (2.36) | 140 (6.38) | 31 (2.93) | 76 (4.55) | 12 (4.70) | 28 (3.98) |
| Dysthymia | 40 (0.61) | 98 (1.20) | 22 (0.82) | 65 (1.83) | 6 (0.31) | 21 (0.97) | 8 (0.41) | 9 (0.64) | 4 (1.37) | 3 (0.45) |
| Mania or hypomania | 69 (1.42) | 138 (1.56) | 45 (2.09) | 86 (2.44) | 15 (1.00) | 34 (1.47) | 7 (0.47) | 16 (0.57) | 2 (1.27) | 2 (0.09) |
| Any mood disorder | 248 (4.49) | 666 (8.64) | 142 (5.84) | 376 (12.00) | 58 (3.16) | 170 (7.72) | 36 (3.24) | 92 (5.37) | 12 (4.70) | 28 (3.98) |
| Anxiety disorders | ||||||||||
| Panic disorder | 47 (1.01) | 138 (1.62) | 33 (1.60) | 87 (2.41) | 8 (0.49) | 26 (1.25) | 4 (0.49) | 19 (0.97) | 2 (0.63) | 6 (0.80) |
| Social phobia | 66 (1.23) | 139 (1.62) | 40 (1.80) | 89 (2.45) | 14 (0.80) | 28 (1.31) | 11 (0.81) | 17 (0.85) | 1 (0.09) | 5 (0.70) |
| Specific phobia | 185 (3.75) | 581 (7.46) | 113 (5.34) | 319 (9.99) | 43 (2.47) | 157 (6.88) | 22 (2.04) | 84 (5.12) | 7 (3.12) | 21 (3.12) |
| Generalized anxiety disorder | 88 (1.51) | 265 (3.85) | 54 (2.10) | 152 (5.26) | 20 (1.01) | 64 (3.32) | 10 (0.82) | 35 (2.47) | 4 (1.64) | 14 (2.49) |
| Post-traumatic stress disorder | 140 (2.38) | 344 (4.38) | 82 (3.12) | 199 (6.12) | 30 (1.47) | 79 (3.79) | 21 (1.74) | 59 (3.20) | 7 (3.39) | 7 (0.92) |
| Any anxiety disorder | 417 (7.90) | 1092 (14.24) | 243 (10.76) | 588 (18.60) | 100 (5.56) | 279 (12.61) | 56 (4.73) | 183 (11.01) | 18 (7.51) | 42 (6.96) |
| Substance use disorders | ||||||||||
| Alcohol abuse/dependence | 326 (6.23) | 92 (1.22) | 211 (8.96) | 72 (2.42) | 81 (4.80) | 12 (0.43) | 32 (3.42) | 8 (0.53) | 2 (0.16) | 0 (0.00) |
| Any drug abuse/dependence | 33 (0.65) | 17 (0.24) | 29 (1.24) | 13 (0.46) | 3 (0.22) | 4 (0.17) | 0 (0.00) | 0 (0.00) | 1 (0.29) | 0 (0.00) |
| Any substance use disorder | 345 (6.62) | 105 (1.40) | 227 (9.64) | 81 (2.72) | 83 (5.00) | 16 (0.60) | 32 (3.42) | 8 (0.53) | 3 (0.45) | 0 (0.00) |
| Nicotine dependence | 534 (11.09) | 589 (7.82) | 349 (16.39) | 361 (11.80) | 146 (9.46) | 164 (7.70) | 34 (3.20) | 56 (3.12) | 5 (2.11) | 8 (0.96) |
| Personality disorders | ||||||||||
| Borderline | 195 (3.33) | 254 (3.03) | 116 (4.71) | 162 (4.62) | 49 (2.51) | 57 (2.56) | 25 (1.70) | 28 (1.49) | 5 (1.66) | 7 (0.95) |
| Antisocial | 142 (3.16) | 34 (0.40) | 91 (4.52) | 28 (0.78) | 38 (2.80) | 5 (0.15) | 11 (1.14) | 1 (0.20) | 2 (0.37) | 0 (0.00) |
| Avoidant | 47 (0.93) | 125 (1.60) | 30 (1.28) | 81 (2.59) | 13 (0.91) | 25 (0.96) | 2 (0.20) | 13 (0.86) | 2 (0.60) | 6 (1.01) |
| Dependent | 8 (0.11) | 29 (0.38) | 6 (0.16) | 16 (0.55) | 1 (0.03) | 7 (0.23) | 1 (0.13) | 5 (0.31) | 0 (0.00) | 1 (0.29) |
| Obsessive-compulsive | 335 (7.06) | 444 (6.10) | 173 (7.78) | 228 (7.50) | 89 (6.51) | 130 (6.19) | 58 (6.43) | 60 (3.80) | 15 (5.94) | 26 (5.11) |
| Paranoid | 116 (2.11) | 223 (2.46) | 73 (2.96) | 124 (3.36) | 27 (1.52) | 63 (2.42) | 13 (0.93) | 26 (1.46) | 3 (2.28) | 10 (0.86) |
| Schizoid | 127 (2.60) | 159 (1.87) | 66 (2.96) | 91 (2.71) | 34 (2.18) | 39 (1.49) | 24 (2.44) | 25 (1.29) | 3 (2.20) | 4 (0.58) |
| Histrionic | 47 (0.73) | 58 (0.67) | 30 (0.96) | 29 (0.82) | 9 (0.46) | 20 (0.84) | 5 (0.51) | 6 (0.30) | 3 (1.04) | 3 (0.34) |
| Schizotypal | 158 (2.49) | 206 (2.32) | 102 (3.81) | 120 (3.27) | 40 (1.89) | 34 (1.25) | 14 (0.84) | 39 (2.30) | 2 (0.18) | 13 (1.50) |
| Narcissistic | 299 (5.49) | 267 (2.61) | 162 (6.85) | 141 (3.07) | 80 (4.87) | 68 (2.26) | 43 (3.36) | 45 (2.66) | 14 (4.94) | 13 (1.41) |
| Any cluster A | 338 (5.95) | 471 (5.24) | 198 (7.92) | 260 (7.14) | 88 (4.69) | 112 (4.16) | 45 (3.94) | 76 (4.09) | 7 (2.88) | 23 (2.68) |
| Any cluster B | 525 (9.99) | 488 (5.47) | 291 (12.85) | 285 (7.53) | 145 (8.78) | 117 (4.59) | 68 (5.72) | 68 (4.01) | 21 (7.17) | 18 (2.25) |
| Any cluster C | 361 (7.58) | 529 (7.17) | 190 (8.54) | 281 (9.18) | 98 (7.09) | 144 (6.72) | 58 (6.43) | 73 (4.56) | 15 (5.94) | 31 (5.98) |
| Any personality disorder | 868 (16.79) | 1045 (12.68) | 466 (20.26) | 550 (16.09) | 240 (15.05) | 276 (11.58) | 126 (11.71) | 167 (9.35) | 36 (14.53) | 52 (8.66) |
| Number of mental disorders (mean, SE) | 0.84 (0.04) | 0.85 (0.03) | 0.48 (0.03) | 0.52 (0.03) | 0.34 (0.03) | 0.37 (0.03) | 0.38 (0.07) | 0.26 (0.03) | ||
Figure 1.
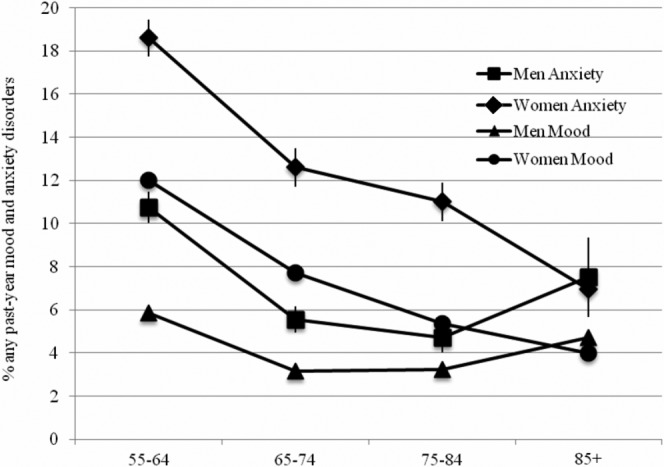
Percentage of respondents with any past-year mood disorder and any past-year anxiety disorder by age group and gender. Error bars represent 95% confidence intervals
DISCUSSION
To the best of our knowledge, this is the largest and most comprehensive study of the prevalence of psychiatric disorders in U.S. older adults to date. The large sample size allowed us to examine, for the first time, gender differences in the prevalence of psychiatric disorders across older adult age groups. The primary contribution of this paper is that it supports the view that disorders become less prevalent across age among older adults, with a leveling off among the oldest age group and a narrowing of gender differences with increasing age.
Our findings regarding the prevalence of psychiatric disorders among older adults are consistent with previous research (15,32). Our pattern of results demonstrating a decrease in the prevalence of psychiatric disorders across the older adult lifespan is supported by previous epidemiological research showing a decrease in psychiatric disorders across both the adult lifespan and specifically among late-life age groups (11–15). However, to the best of our knowledge, the current study is the first to identify a leveling off in the prevalence of specific psychiatric disorders among the oldest-old age group.
The overall pattern of decreased rates of psychiatric disorders with increased age can be explained by the socioemotional selectivity theory (SST) (33), and the leveling off in prevalence rates among adults aged 85 and older can be explained by the strength and vulnerability integration theory (SAVI) (34). SST posits that older adults adopt a limited perception of time and a present-focused state of awareness, seek the fulfillment of emotionally meaningful goals, and select the company of familiar social partners, which decreases the likelihood that stressful social situations will occur, and increases the likelihood of experiencing positive emotions (33). Building on the components of SST, SAVI suggests a pattern of increased positivity and well-being until approximately the late 60s and a slight decrease thereafter (34). The slight decrease in well-being may be attributable to older adults' decreased physiological tolerance to stress, which can result in compromised immune functioning when strategies associated with the aforementioned strengths are not applied successfully (34). These theories support the pattern of results observed in this study whereby prevalence rates of psychiatric disorders decline throughout the late-life span, until approximately the age of 85+, where a slight, albeit non-significant increase in prevalence of several psychiatric disorders was observed. Given medical advances and increases in life expectancy rates, it is possible that the vulnerabilities described in SAVI are occurring at a later age for older adults. It could also be the case that older adults who are experiencing more of the vulnerabilities of old age do not participate in survey research such as the NESARC due to illness and institutionalization.
SST and SAVI support the current study's finding of decreased mental health-related quality of life among older adults aged 75-85+. The pattern of narrowing gender differences in the prevalence of psychiatric disorders with increasing age can also be explained by SAVI, with both genders experiencing similar vulnerabilities with increasing age. Furthermore, the decreased gender gap in life expectancy suggests that more men are now living into older age, increasing the likelihood that they will experience the vulnerabilities of old age.
Results of this study must be viewed in light of several limitations. First, the NESARC is a survey of community-dwelling individuals and our findings do not generalize to institutionalized older adults. Second, as is typically the case in epidemiologic surveys, psychiatric disorders were not diagnosed using hierarchical rules. As a result, it is possible that prevalence rates were inflated based on DSM-IV criteria. Third, given the recently published DSM-5, the diagnostic criteria for several of the DSM-IV psychiatric disorders examined in the current study have been modified to various extents. The most prominent change that may affect current findings is the removal of PTSD from the anxiety disorders category and its inclusion in the revised trauma and stress-related disorders category, which would affect our prevalence estimate for any anxiety disorder.
Notwithstanding these limitations, findings of this study make a unique contribution to the literature by highlighting the prevalence of mood, anxiety, substance use, and personality disorders in addition to mental health-related quality of life across the older adult lifespan, and by examining differences in prevalence of these disorders by late-life age groups and gender. Given the relatively high rates of psychiatric disorders among older adults and the leveling off in prevalence rates in older adults ages 85+, these results underscore the importance of prevention, diagnosis, and treatment of psychiatric disorders in this population.
Future research is needed to further examine the reasons why the prevalence of psychiatric disorders decreases across late-life age groups. Moreover, additional research is needed to examine gender-specific psychiatric comorbidity profiles, as well as to develop and evaluate personalized treatments for the oldest-old age group of adults (85+).
Acknowledgments
K. Reynolds is supported by a Canadian Institutes of Health Research Doctoral Research Award and a Manitoba Graduate Scholarship; R.H. Pietrzak is supported by the U.S. Department of Veterans Affairs National Center for PTSD and a private donation; R. El-Gabalawy is supported by a Manitoba Health Research Council Doctoral Studentship and a Manitoba Graduate Scholarship; J. Sareen is supported by a Manitoba Health Research Council Chair Award. The aforementioned funding sources did not have a role in the writing of the manuscript or the decision to submit it for publication. The NESARC was conducted and funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), with supplemental support from the National Institute on Drug Abuse. The authors thank the NIAAA and the U.S. Census Bureau field representatives who administrated the NESARC interviews and made data available to researchers.
References
- Department of Economic and Social Affairs, United Nations. World population aging 2009. New York: United Nations; 2010. [Google Scholar]
- Beekman ATF, Deeg DJH, van Tilburg T, et al. Major and minor depression in later life: a study of prevalence and risk factors. J Affect Disord. 1995;36:65–75. doi: 10.1016/0165-0327(95)00061-5. [DOI] [PubMed] [Google Scholar]
- Forsell Y, Jorm AF, von Strauss E, et al. Prevalence and correlates of depression in a population of nonagenarians. Br J Psychiatry. 1995;167:61–4. doi: 10.1192/bjp.167.1.61. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Reynolds JR. Age, depression, and attrition in the National Survey of Families and Households. Sociol Methods Res. 2000;28:476–504. [Google Scholar]
- Kessler RC, Foster C, Webster PS, et al. The relationship between age and depressive symptoms in two national surveys. Psychol Aging. 1992;7:119–26. doi: 10.1037//0882-7974.7.1.119. [DOI] [PubMed] [Google Scholar]
- Newmann J. Aging and depression. Psychol Aging. 1989;4:150–65. doi: 10.1037//0882-7974.4.2.150. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross CE. Age and depression. J Health Soc Behav. 1992;33:187–205. [PubMed] [Google Scholar]
- Blanchflower DG, Oswald AJ. Is well-being U-shaped over the life cycle? Soc Sci Med. 2008;66:1733–49. doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- Stone AA, Schwartz JE, Broderick JE, et al. A snapshot of the age distribution of psychological well-being in the United States. Proc Natl Acad Sci USA. 2010;107:9985–90. doi: 10.1073/pnas.1003744107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karel MJ, Gatz M, Smyer MA. Aging and mental health in the decade: what psychologists need to know. Am Psychol. 2012;67:184–98. doi: 10.1037/a0025393. [DOI] [PubMed] [Google Scholar]
- Hybels CF, Blazer DG. Epidemiology of late-life mental disorders. Clin Geriatr Med. 2003;19:663–96. doi: 10.1016/s0749-0690(03)00042-9. [DOI] [PubMed] [Google Scholar]
- Gum AM, King-Kallimanis B, Kohn R. Prevalence of mood, anxiety, and substance-abuse disorders for older Americans in the National Comorbidity Survey – Replication. Am J Geriatr Psychiatry. 2009;17:769–81. doi: 10.1097/JGP.0b013e3181ad4f5a. [DOI] [PubMed] [Google Scholar]
- Schuster JP, Hoertel N, Le Strat Y, et al. Personality disorders in older adults: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Am J Geriatr Psychiatry. 2013;21:757–68. doi: 10.1016/j.jagp.2013.01.055. [DOI] [PubMed] [Google Scholar]
- Streiner D, Cairney J, Veldhuizen S. Epidemiology of psychological problems in the elderly. Can J Psychiatry. 2006;52:185–91. doi: 10.1177/070674370605100309. [DOI] [PubMed] [Google Scholar]
- Byers AL, Yaffe K, Covinsky KE, et al. High occurrence of mood and anxiety disorders among older adults: the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2010;67:489–96. doi: 10.1001/archgenpsychiatry.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bebbington PE, Dunn G, Jenkins R, et al. The influence of age and sex on the prevalence of depressive conditions: report from the National Survey of Psychiatric Morbidity. Psychol Med. 1988;28:9–19. doi: 10.1017/s0033291797006077. [DOI] [PubMed] [Google Scholar]
- Bland RC, Newman SC, Orn H. Period prevalence of psychiatric disorders in Edmonton. Acta Psychiatr Scand. 1988;77(Suppl. 338):33–43. doi: 10.1111/j.1600-0447.1988.tb08545.x. [DOI] [PubMed] [Google Scholar]
- Gurland BJ. The comparative frequency of depression in various adult age groups. J Gerontol. 1976;31:283–92. doi: 10.1093/geronj/31.3.283. [DOI] [PubMed] [Google Scholar]
- Jorm AF. Sex and age differences in depression: a quantitative synthesis of published research. Aust N Zeal J Psychiatry. 1987;21:46–53. doi: 10.3109/00048678709160898. [DOI] [PubMed] [Google Scholar]
- Robins LN, Regier DA. Psychiatric disorders in America. New York: Free Press; 1991. [Google Scholar]
- Cairney J, McCabe L, Veldhuizen S, et al. Epidemiology of social phobia in later life. Am J Geriatr Psychiatry. 2007;15:224–33. doi: 10.1097/01.JGP.0000235702.77245.46. [DOI] [PubMed] [Google Scholar]
- Corna LM, Cairney J, Herrmann N, et al. Panic disorder in later life: results from a national survey of Canadians. Int Psychogeriatr. 2007;19:1084–96. doi: 10.1017/S1041610207004978. [DOI] [PubMed] [Google Scholar]
- Mackenzie CS, Reynolds K, Chou KL, et al. Prevalence and correlates of generalized anxiety disorder in a national sample of older adults. Am J Geriatr Psychiatry. 2011;19:305–15. doi: 10.1097/JGP.0b013e318202bc62. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan K. Source and accuracy statement for the Wave 2 National Epidemiological Survey on Alcohol and Related Conditions (NESARC) Bethesda: National Institute on Alcohol Abuse and Alcoholism; 2005. [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69:533–45. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Clara IP, Worobec LM, et al. An empirical evaluation of the structure of DSM-IV personality disorders in a nationally representative sample: results of confirmatory factor analysis in the National Epidemiologic Survey on Alcohol and Related Conditions Wave 1 and 2. J Pers Disord. 2012;26:890–901. doi: 10.1521/pedi.2012.26.6.890. [DOI] [PubMed] [Google Scholar]
- Ware J, Kosinski M, Keller SD. 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Shah BV, Barnswell BG, Bieler GS. SUDAAN User's Manual: Release 10.0. Research Triangle Park: Research Triangle Institute; 2009. [Google Scholar]
- Levy PS, Lemeshow S. Sampling of populations. New York: Wiley; 1999. [Google Scholar]
- Wang YP, Andrade LH. Epidemiology of alcohol and drug use in the elderly. Curr Opin Psychiatry. 2013;26:343–8. doi: 10.1097/YCO.0b013e328360eafd. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: a theory of socioemotional selectivity. Am Psychol. 1999;54:165–81. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- Charles ST. Strength and vulnerability integration: a model of emotional well-being across adulthood. Psychol Bull. 2010;136:1068–91. doi: 10.1037/a0021232. [DOI] [PMC free article] [PubMed] [Google Scholar]


