Abstract
Background
Many patients with diabetes do not achieve target values. One of the reasons for this is clinical inertia. The correct explanation of clinical inertia requires a conjunction of patient with physician and health care system factors. Our aim was to determine the rate of clinical inertia in treating diabetes in primary care and association of patient, physician, and health care setting factors with clinical inertia.
Material/Methods
This was a national, multicenter, observational, cross-sectional study in primary care in Croatia. Each family physician (FP) provided professional data and collected clinical data on 15–25 type 2 diabetes (T2DM) patients. Clinical inertia was defined as a consultation in which treatment change based on glycated hemoglobin (HbA1c) levels was indicated but did not occur.
Results
A total of 449 FPs (response rate 89.8%) collected data on 10275 patients. Mean clinical inertia per FP was 55.6% (SD ±26.17) of consultations. All of the FPs were clinically inert with some patients, and 9% of the FPs were clinically inert with all patients. The main factors associated with clinical inertia were: higher percentage of HbA1c, oral anti-diabetic drug initiated by diabetologist, increased postprandial glycemia and total cholesterol, physical inactivity of patient, and administration of drugs other than oral antidiabetics.
Conclusions
Clinical inertia in treating patients with T2DM is a serious problem. Patients with worse glycemic control and those whose therapy was initiated by a diabetologist experience more clinical inertia. More research on causes of clinical inertia in treating patients with T2DM should be conducted to help achieve more effective diabetes control.
MeSH Keywords: Diabetes Mellitus, Type 2; Physicians, Family; Quality of Health Care
Background
Although the benefits of tight glycemic control are well known, many patients with diabetes still do not achieve target values. One of the reasons for this is clinical inertia of health care professionals, including those in primary care [1]. By definition, clinical inertia is failure of a health care provider to initiate or intensify therapy when indicated [2]. A study of the relationship between inertia and the outcome of diabetes care found that, on average, a 15% higher frequency of treatment intensification was associated with a 0.15% lower level of glycated hemoglobin (HbA1c) [3]. It is well accepted that glycemic control is an important indicator for quality of care, and clinical inertia may be one of the reasons why the level of HbA1c is worse than generally recommended. By defining the specific factors associated with clinical inertia, it is possible to develop other quality indicators for primary care diabetes control [4]. The phenomenon of clinical inertia has been difficult to study because of the paucity of data on the content of the patient-physician encounters [5]. A treatment decision based on the last HbA1c measurement in combination with recent history acknowledges the intrinsic variation of physiological measurement as well as other variation [6]. Studies conducted in the USA, Canada, and Europe showed widespread clinical inertia, with the percentage ranging from 30% to 68%. Clinical inertia has been assigned to both patient and physician characteristics. Some studies have linked clinical inertia to medication non-adherence, provider judgement, number of chronic conditions, severity of hypertension, and problems related to the implementation of guidelines [4,5,7–13]. Prior studies have investigated combined physician and patient characteristics and their relative contribution to clinical inertia. They reported that greater clinical inertia was associated with patient non-compliance, low level of diabetes knowledge, lack of motivation, the short time spent in consultation, absence of data in medical records, border-high limits measurements accepted as normal readings, lack of treatment goals, lack of teamwork, lack of alarm systems in the electronic medical record, and lack of feedback on performance [14–16].
In Croatia, the primary care system is currently organized as a list-based system in which patients register with a single physician who acts as a gatekeeper for other services and provides continuing and comprehensive personal care. According to official data from the Central Health Information System of Croatia, there were 234 457 persons with diabetes registered with their general practitioners in 2011 [17]. Annual reports from the Croatian National Diabetes Registry show a slow decline in percentage of patients not achieving good glycemic control (HbA1<7.5%) in primary care – 40.34% in year 2011 vs. 38.08% in year 2013 [18,19]. Persons with diabetes are seen by their doctor a mean of 6.2–16.2 times a year. The patient enablement score as a consultation measure in family practice in Croatia is relatively high (6.6) [20,21].
Although some progress has been made, our understanding of clinical inertia is still far from complete. More attention should be devoted to understanding and reducing factors that contribute to clinical inertia. Interventions to reduce clinical inertia should be properly designed and targeted; thus, it is important to assess the influence of patient factors in conjunction with physician factors on the probability of a patient experiencing clinical inertia. To the best of our knowledge, there are no published data on clinical inertia in Croatia. The aim of the present study was to assess the extent of clinical inertia in treating diabetes in primary care in Croatia and to investigate its association with patient, physician, and health care setting characteristics.
Material and Methods
Study design, setting, and participants
This national, multicenter, cross-sectional study was conducted in primary care physician offices in Croatia between 2008 and 2010. For recruitment purposes, the following assumptions were made in determining the representative sample size of patients and physicians. The national standard is 1700 patients per family physician (FP) office, about 900 of whom are aged ≥40 years. The prevalence of adult T2DM in Croatia is 8.9%, so 80 T2DM patients per standard FP office are expected, about 15% of them on insulin therapy, with the remaining 85% on oral antidiabetics. A minimum of 15 T2DM patients per practice was set. To minimize practice bias, the maximum number of charts allowed per FP was set at 25. Based on these assumptions, at least 374 FPs were required for the study. To compensate for incomplete or incorrectly completed questionnaires, an FP oversampling of 20% was used. The study was approved by the Ethics Committee of the Medical Faculty in Zagreb.
Questionnaires
We used 2 standardized, validated questionnaires, designed for the study, which complied with ethics requirements. The questionnaire for physicians included physician sociodemographic and professional data: age, sex, years of working experience, specialty in family medicine, total number of patients enlisted, number of T2DM patients in care, average number of consultations per day, place of work, prescription of antidiabetic medications or referral to diabetologist, and diabetes complications record. The questionnaire for patients included data on lifestyle habits (physical activity, diet, alcohol consumption, and smoking) demographic audit, data on comorbidity, chronic medication, and micro- and macro-vascular complication of patients.
Physicians
The target population of FPs consisted of 2552 working in family medicine in 2007. A stratified proportional sample design was used to draw a random sample of 500 FPs; the 2 stratification criteria included practice size (≤1399 patients, 1400–1799 patients, and ≥1800 patients) and geographical distribution of the practices (21 Croatian counties). The selection of practices and FPs was made using data from the Croatian National Institute of Public Health and Croatian Institute of Health Insurance [22]. With a response rate of 89.8%, the 449 recruited FPs are a representative sample of all FPs in Croatia.
Patients
A total of 449 FPs from all Croatian regions recruited the first 15–25 participants of both sexes with T2DM (according to IDF criteria). Inclusion criteria were: diagnosed at least 3 years prior to study entry, no insulin in therapy, aged ≥40 years, and who had visited a practice for diabetes control during the last 3 months. Exclusion criteria were: secondary diabetes, including iatrogenic diabetes (steroid and/or olanzapine therapy); pancreatic disease (chronic pancreatitis, cystic fibrosis); known endocrine cause of diabetes (hypercortisolism or acromegaly); and severe diseases with less than 6 months life expectancy. For the measurement of HbA1c, an inhibition of latex immunoagglutination with DCA Vantage analyzer from Siemens Healthcare Diagnostics® was used and Bayer’s Contour® glucometer was used for the measurement of fasting and postprandial glycemia. Data on total cholesterol, triglyceride, and creatinine levels were collected from patient medical records if performed within the past year. Two consecutive measurements were made of blood pressure, body weight and height, and waist circumference. All medical data extraction and measurements were objectively carried out by FPs.
Clinical inertia
Clinical inertia was defined as a consultation in which treatment change based on HbA1c level was indicated but did not occur. Each included T2DM patient had continuity in care with their FP at least 3 years prior to the study. Based on complete patient data, each FP acts to encourage patients to take prescribed medication, increases the drug dosage, adds a second/third drug if indicated, changes previous therapy, and/or initiates insulin therapy. Each action is a factor relevant to clinical inertia. If HbA1c was <7.5% and the FP did not encourage the patient to receive regular therapy, clinical inertia was declared. In case HbA1c was 7.5–8.0%, if the FP increased the drug dosage or changed previous therapy, or added a second/third drug, there was no clinical inertia, otherwise clinical inertia was declared. In case HbA1c was 8.0–9.0%, there was no clinical inertia if the FP changed the previous therapy, added a second/third drug, or initiated insulin therapy, otherwise clinical inertia was declared. In case HbA1c was >9.0%, there was no clinical inertia only if insulin therapy was initiated, otherwise clinical inertia was declared. HbA1c levels as cut-off points to declare clinical inertia were in accordance with, but less restrictive than, Croatian T2DM guidelines, which state that HbA1c should be ≤6.5%, but HbA1c>7.5% after 3–6 months therapy with 2 or 3 oral antidiabetic drugs (OADs) is indication for initiation of insulin therapy [23].
Statistical analysis
Normality of distribution was tested using the Kolmogorov-Smirnov test. The mean and standard deviation were used to measure central tendency and dispersion. χ2 tests were used to assess associations between 2 nominal variables with contingency coefficient as a measure of the degree of relationship. In univariate analysis, we explored possible patient characteristics associated with clinical inertia, including sex, age, HbA1c%, anthropometry and laboratory measurements, lifestyle habits, microvascular and macrovascular diabetes complications, presence of other chronic diseases, and receiving drugs for diabetes and other diseases, as well as the FP’s sociodemographic and professional data. Significantly associated variables were entered into multivariate logistic regression models to determine adjusted odds ratios (ORs) for predictors of clinical inertia. A separate analysis with the practices as the unit of study was performed to determine the percentage of clinical inertia per FP. All statistical methods were performed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA).
Results
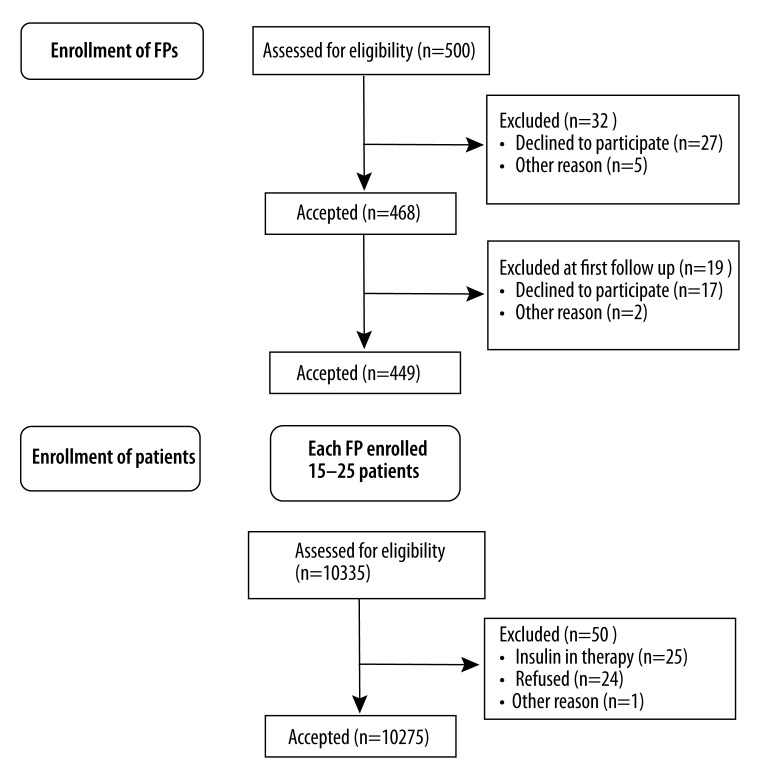
A total of 449 FPs collected data on 10 275 patients (Figure 1). Baseline characteristics of the patients are presented in Table 1. There was a slight predominance of female patients. Most (62.6%) male diabetics were 50–69 years old and most (66.6%) female diabetics were 60–79 years old. Most (41.3%) patients were overweight or obese (31.4%) with sedentary lifestyle, even though 76% of them reported healthy dietary habits. Mean HbA1c (7.6%) was above recommended target and most patients had 1 (46.1%) or 2 (43.6%) OADs prescribed. Most patients did not achieve treatment targets for blood pressure or lipids. Presence of other chronic diseases was found among 80% of patients and 81.5% of them had been prescribed other drugs beside OAD. Most participating FPs were female (84.4%) with relevant experience. Data on their characteristics can be seen in Table 2. Among procedures that FPs performed, encouraging patients to take prescribed medication was the most common, followed by increasing the dosage and adding a second or third drug. Initiation of insulin therapy or changing the previous therapy were the least common actions. Patients with lower levels of HbA1c were subject to all actions except for initiation of insulin therapy. Patients with HbA1c levels of 7.6–7.9% underwent the smallest number of procedures. Over half (52.1%) of all insulin initiation was for patients with HbA1c >9% (Table 3).
Figure 1.
Flow chart: Enrollment of participants.
Table 1.
Patients baseline characteristics.
| Sex (N/%) | |
| Male | 4939/48.1 |
| Female | 533651.9 |
|
| |
| Age (years) | 65.7/10.05 |
|
| |
| Waist circumference (cm) | |
| Male | 104.1(12.04) |
| Female | 98.1(13.29) |
|
| |
| BMI (kg/m2) (N/%) | |
| 25–29.9 | 4247/41.3 |
| 30–34.9 | 3231/31.4 |
| 35–39.9 | 1106/10.8 |
| >40 | 370/3.6 |
|
| |
| Blood pressure <140/80 mmHg (N/%) | 1290/12.6 |
|
| |
| HbA1c | 7.6/1.58 |
|
| |
| Fasting glycemia (mmol/l) | 8.6/2.68 |
|
| |
| Postprandial glycemia (mmol/l)) | 10.7/3.73 |
|
| |
| Total cholesterol (mmol/l) | 5.5/1.12 |
|
| |
| Triglyceride (mmol/l) | 2.0/1.05 |
|
| |
| Creatinine (μmol/l) | 88.8/21.14 |
|
| |
| Diabetes complication (N/%) | |
| Retinopathy | 1242/12.6 |
| Polyneuropathy | 3142/32.4 |
| Coronary Disease | 1696/17.2 |
| Nefropathy | 557/5.6 |
|
| |
| OADs (N/%) | |
| None | 372/3.6 |
| One | 4737/46.1 |
| Two | 4483/43.6 |
| Three | 693/6.7 |
|
| |
| Comorbidities present (N/%) | 8229/80.0 |
|
| |
| Drugs other than OAD (N/%) | 8366/81.3 |
|
| |
| Current smokers (N/%) | 1969/19.4 |
|
| |
| Any alcohol consuming (N/%) | 5573/55.8 |
|
| |
| Unhealthy diet* (N/%) | 2398/24.0 |
|
| |
| Not physically active* (N/%) | 2146/21.1 |
All values, if not as%, are shown as means (SD). BMI – body mass index; OAD – oral antidiabetic drug.
European guidelines on cardiovascular prevention recommendation.
Table 2.
Family physician baseline characteristics.
| Sex (N/%) | |
| Male | 70/15.6 |
| Female | 379/84.4 |
|
| |
| Age, y | 49.2(7.64) |
|
| |
| Working experience, y | 22.7(7.83) |
|
| |
| Family medicine specialists (N/%) | 256/57.1 |
|
| |
| Patient in care | 1775(370.3) |
|
| |
| T2DM in care | 101(40.8) |
|
| |
| Daily visits | 66(22.9) |
|
| |
| Working status (N/%) | |
| Health care center employee | 77/17.1 |
| Private practice outside health care centres | 52/11.6 |
| Private practice inside health care centres | 320/71.3 |
|
| |
| Initiation of OAD prescribed (N/%) | 5058/51.0 |
All values, if not as%, are shown as means (SD).
Table 3.
HbA1c and treatment intensification.
| HbA1c | |||||
|---|---|---|---|---|---|
| ≤7.5 | 7.6–7.9 | 8.0–8.9 | ≥9.0 | Total | |
| Encourage towards taking prescribed medication | 3522 (60.4) | 629 (10.8) | 785 (13.5) | 893 (15.3) | 5829 (100.0) |
| Increase the drug dosage | 906 (47.6) | 280 (14.7) | 332 (17.4) | 386 (20.3) | 1904 (100.0) |
| Change previous therapy | 315 (38.9) | 117 (14.5) | 164 (20.3) | 213 (26.3) | 809 (100.0) |
| Add a second/third drug | 473 (43.9) | 136 (12.6) | 228 (21.2) | 240 (22.3) | 1077 (100.0) |
| Initiate an insulin | 14 (14.9) | 12 (12.8) | 19 (20.2) | 49 (52.1) | 94 (100.0) |
All values are shown as%.
Clinical inertia
We found clinical inertia in 57.7% of all clinical encounters. Mean clinical inertia per FP was 55.6% (SD ±26.17). All FPs were clinically inert with some patients, and 9% of FPs were clinically inert with all patients. Clinical inertia significantly increased (χ2=1753.984; ss=3; P<0.001; cc=0.382) along with the increase of HbA1c (Table 4).
Table 4.
Clinical inertia and HbA1c.
| Clinical inertia | p; cc | ||||
|---|---|---|---|---|---|
| Yes | No | ||||
| HbA1c | |||||
| ≤7.5 | 2616 | (42.6) | 3522 | (57.4) | <0.001; 0.382 |
| 7.6–7.9 | 726 | (64.1) | 406 | (35.9) | |
| 8.0–8.9 | 1025 | (74.5) | 350 | (25.5) | |
| ≥9.0 | 1542 | (96.9) | 49 | (3.1) | |
p<0.05; cc – contingency coefficient. All values are shown as%. All percentages refer to the total number of patients in each rows.
Significant associations were found in the univariate analysis of patient and physician characteristics associated with clinical inertia. Some of those associations were no longer found when analyzed with the multivariate model. This was the case with the following variables: fasting glycemia, blood pressure ≥140/80 mHg, triglycerides >1.7 mmol/l, unhealthy dietary habits, presence of other chronic diseases, number of patients in care, number of consultations per day, and FP-initiated OAD (Table 5). Of all the patient and physician factors included into multivariate analysis, HbA1c level had the highest association with clinical inertia and patients with worse glycemic control were more likely to experience clinical inertia. The analysis showed that the risk for clinical inertia increased when OADs were initiated by diabetologists, when patients had increased postprandial glycemia and total cholesterol, or were not sufficiently physically active. The presence of other chronic diseases was not associated with clinical inertia, but presence of drugs other than OADs was associated with clinical inertia. Male FPs were more likely to be inert than female FPs.
Table 5.
Patient and physician characteristics associated with clinical inertial.
| Raw Association (univariate) | Adjusted model | |||
|---|---|---|---|---|
| ORuv | (95% CI) | ORmv | (95% CI) | |
| HbA1c (%) level | ||||
| ≤7.5 | 1 | 1 | ||
| 7.6–7.9 | 2.4 | (2.11–2.75) | 2.6 | (2.18–3.00) |
| 8.0–8.9 | 3.9 | (3.46–4.50) | 4.6 | (3.86–5.38) |
| ≥9.0 | 42.4 | (31.74–56.56) | 47.2 | (33.60–66.40) |
| Fasting glycemia (cut off value 7 mmol/l) | ||||
| ≤7.0 | 1 | 1 | ||
| > 7.0 | 2.3 | (2.05–2.43) | 1.0 | (0.89–1.14) |
| Postprandial glycemia (cut off value 7.5 mmol/l) | ||||
| ≤7.5 | 1 | 1 | ||
| >7.5 | 2.5 | (2.23–2.75) | 1.2 | (1.06–1.39) |
| Waist circumference | ||||
| Normal* | 1 | 1 | ||
| Increased** | 0.9 | (0.84–0.99) | 0.9 | (0.79–0.99) |
| Blood pressure (mmHg) | ||||
| <140/80 | 1 | 1 | ||
| ≥140/80 | 1.2 | (1.07–1.35) | 1.0 | (0.85–1.16) |
| Total cholesterol (cut off value 4.5 mmol) | ||||
| Normal (<4.5) | 1 | 1 | ||
| Increased (≥4.5) | 1.4 | (1.24–1.52) | 1.3 | (1.12–1.47) |
| Triglicerides (cut off value 1.7 mmol) | ||||
| Normal (<1.7) | 1 | 1 | ||
| Increased (≥1.7) | 1.3 | (1.20–1.41) | 1.0 | (0.92–1.14) |
| Creatinin | ||||
| Normal# | 1 | 1 | ||
| Moderate increase## | 0.8 | (0.66–0.91) | 0.7 | (0.55–0.86) |
| Increased### | 1.1 | (0.91–1.36) | 0.8 | (0.66–1.14) |
| Current smoking | ||||
| No | 1 | 1 | ||
| Yes | 0.9 | (0.77–0.94) | 0.9 | (0.76–0.99) |
| Any alcohol consuming | ||||
| No | 1 | 1 | ||
| Yes | 0.8 | (0.73–0.86) | 0.8 | (0.76–0.95) |
| Anyone advised to stop alcohol consuming | ||||
| No | 1 | 1 | ||
| Yes | 1.4 | (1.23–.49) | 1.0 | (0.83–1.10) |
| Anyone advised to increase physical activity | ||||
| No | 1 | 1 | ||
| Yes | 1.7 | (1.51–1.81) | 1.2 | (1.09–1.36) |
| Dietary habits‡ | ||||
| Healthy | 1 | 1 | ||
| Unhealthy | 0.9 | (0.79–0.95) | 1.0 | (0.84–1.08) |
| Other chronic diseases (total) | ||||
| No | 1 | 1 | ||
| Yes | 0.6 | (0.54–0.66) | 1.0 | (0.84–1.19) |
| Other drugs (total) | ||||
| No | 1 | 1 | ||
| Yes | 0.7 | (0.66–0.81) | 1.2 | (0.98–1.40) |
| FP sex | ||||
| Female | 1 | 1 | ||
| Male | 1.2 | (1.03–1.29) | 1.2 | (1.00–1.35) |
| Years of working expirience (M; SD) | 1.01 | (1.00–1.01) | 1.009 | (1.001–1.016) |
| Total number of patients in care (M; SD) | 0.992 | (0.991–0.995) | 1.0 | (0.998–1.000) |
| Total number of T2DM (M; SD) | 0.996 | (0.995–0.997) | 0.998 | (0.996–1.001) |
| Average daily visits (M; SD) | 0.994 | (0.992–0.996) | 1.0 | (0.994–1.006) |
| Working status | ||||
| Health care center employee | 1 | 1 | ||
| Private practice outside health care centres | 1.0 | (0.87–1.19) | 1.1 | (0.86–1.34) |
| Private practice inside health care centres | 0.8 | (0.73–0.90) | 0.8 | (0.66–0.90) |
| FP initiated OAD | ||||
| No | 1 | 1 | ||
| Yes | 0.5 | (0.49–0.58) | 1.1 | (0.89–1.49) |
| Diabetologist initiated OAD | ||||
| No | 1 | 1 | ||
| Yes | 2.0 | (1.81–2.14) | 1.9 | (1.48–2.49) |
Male ≤102 cm, female ≤88 cm;
male >102 cm, female >88 cm;
male <115 μmol/l, female <107 μmol/l;
male 115–132 μmol/l, female 107–123 μmol/l;
male >132 μmol/l, female >123 μmol/l.
European guidelines on cardiovascular prevention recommendation.
OR – odds ratio; 95% CI – 95% confidence interval; uv – univariate logistic regression, mv – multivariate logistic regression.
Discussion
Our study, in a very large sample, found widespread clinical inertia and, unexpectedly, that patients with worse glycemic control were more likely to experience clinical inertia. Most participating patients with poor glycemic control did not receive proper treatment intensification. The frequency of clinical inertia (57.7%) in our study was comparable with that found in previous studies [12]. Most studies on clinical inertia were performed in the USA, with only a few in Europe and none in Croatia. In a study performed by Berlowitz, inertia occurred in 68% of the visits made by US Veterans Administration patients with an HbA1c>8% over 16 months [4], with similar percentages found in academic centers and outpatient clinics among patients with poor glycemic, blood pressure, or cholesterol control [13,24,25]. We found that all FPs were clinically inert with some patients and that 9% of FPs were clinically inert with all patients, which is concerning. We also found major differences in FP intervention and clinical inertia based on HbA1c. In contrast to the results reported by Mata-Cases, clinical inertia increased as HbA1c values increased and most inertia was found above HbA1c 9.0%, while lowest inertia was found with HbA1c below 7.6% [5]. The reluctance of FPs to make treatment changes in those patients could be explained by the insufficient experience and clinical knowledge about intensification of treatment. For decades, the health care system in Croatia encouraged referral to diabetologists. Until recently, FPs were encouraged by the Croatian Institute for Health Insurance to provide most of the antidiabetic treatment needed by patients. This is probably why clinical inertia was mostly associated with the initiation of OAD therapy by a diabetologist, which in fact represents an early referral from the FP. Both of these results could indicate the need for different educational strategies to help family practitioners initiate treatment intensification once the first signs of poor glycemic control are detected in order to prevent disease progression. Failure to intensify oral diabetes treatment is common in diabetes care, with only 22% of patients receiving intensified oral diabetes treatment in hyperglycemic visits [26]. One might expect that increased HbA1c indicates a patient who is more difficult to treat, with more comorbidities and complex clinical background, which could partly explain clinical inertia. In contrast, we found that comorbidities were not associated with the likelihood of clinical inertia, but rather that the presence of other drugs beside OADs was associated with increased likelihood of clinical inertia. Medication burden was not a barrier for treatment modification for GIANTT group investigators [6]. This favors the concept that clinical inertia does not adequately characterize the complexity of the primary care encounter, which involves a complex web of patient factors that modifies the impact of pharmacotherapy on HbA1c [27]. Our finding that encouraging patients to take prescribed medication was the most utilized strategy among FPs may imply that they preferred improvement of patient self-management education rather than treatment intensification. Clinicians are advised to consider all benefits and risks of intensifying glucose-lowering treatment carefully because the most sensible treatment strategy will vary substantially between patients [28]. In addition, current guidelines for antidiabetic treatment are not relevant for most elderly people, who were the majority of investigated patients in this study. Similar to other investigators, we also found that sedentary lifestyle, being a traditional cardiovascular risk factor, did not lead to action by FPs [25]. It may be that FP time constraints in handling competing demands is an important factor in physician decision-making and that other concerns take priority over interventions to change unhealthy behavior. A Croatian study found 2.1±1.1 reasons for encounter per visit and 2.6±1.5 procedures per visit of persons with diabetes to FPs [29]. Another of our findings – that FPs working in private practice are less likely to be inert – could be in line with Phillips et al’s definition of clinical inertia [2], that clinical inertia is not a patient-centered problem but is rather a problem of health care systems. One of possible reasons for private practice FPs to be less inert is that in Croatia they are paid more than health care center employees. Aside from financial issues, we believe that dealing with clinical inertia in primary care probably requires a patient-centered rather than a concept-oriented approach. Addressing individual needs while integrating various disease perspectives with continuity in care is at the root of family practice and determines its effectiveness [30].
Strengths and limitations of the study
The cross-sectional design of the study limits ability to draw conclusions. A longer study period would be optimal. Also, we did not investigate patient adherence to treatment or reluctance to have their antidiabetes treatment intensified, which could force physicians into clinical inertia. Although practices were randomly selected, all FPs participated voluntarily and the FPs may have been selected with a particular interest in diabetes. Therefore, we may have underestimated the prevalence of clinical inertia. However, given that the rates of clinical inertia found in this study are consistent with those of other studies, it is likely that the selected FPs are representative of other practices throughout Croatia. There is a great imbalance between variable numbers related to patients and those related to physicians and the health care setting, as well as a great imbalance in the number of patients and physicians included into the survey and possible variates inside each group. It is only correct to associate separate parameters with a physician’s clinical inertia.
One of the strengths of our study is the large number of participating patients and FPs. Furthermore, this study was conducted among insured patients who had no financial barriers to care. This design helps to isolate the relationship between clinical inertia and all predictors investigated, but may limit generalizability to other populations.
This study is the first to explore clinical inertia in Croatia and shows that the extent of clinical inertia in treating diabetes in primary care in Croatia is essential and associated with patient, physician, and health care setting characteristics. Repeated assessment of diabetes care delivery could improve diabetes treatment in Croatia.
Conclusions
This study demonstrates that clinical inertia in treating patients with T2DM is an important problem. This is particularly concerning given that patients with worse glycemic control and those whose therapy was initiated by a diabetologist experience more clinical inertia. These findings may also indicate a problem in the health care system. Proper monitoring of quality of care and feedback on specific clinical outcomes with tailored interventions like educational courses, decisional aids, reminders, peer influence, and even incentives/sanctions could help in reducing clinical inertia. More research on causes of clinical inertia in treating patients with T2DM should be conducted to help achieve more effective diabetes control in primary care.
Acknowledgements
We are grateful to all who participated in the study.
Footnotes
Competing interest
There are no financial or other conflicts of interest.
Source of support: Association of Teachers in General Practice/Family Medicine (ATGP/FM) in Croatia
References
- 1.Shah BR, Hux JE, Laupacis A, Walraven C. Clinical Inertia in Response to Inadequate Glycemic Control Do specialists differ from primary care physicians? Diabetes Care. 2005;28:600–6. doi: 10.2337/diacare.28.3.600. [DOI] [PubMed] [Google Scholar]
- 2.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–34. doi: 10.7326/0003-4819-135-9-200111060-00012. [DOI] [PubMed] [Google Scholar]
- 3.Ziemer DC, Miller CD, Rhee MK, et al. Clinical inertia contributes to poor diabetes control in a primary care setting. Diabetes Educ. 2005;31:564–71. doi: 10.1177/0145721705279050. [DOI] [PubMed] [Google Scholar]
- 4.Berlowitz DR, Ash AS, Glickman M, et al. Developing a Quality of Measure for Clinical Inertia in Diabetes Care. Health Serv Res. 2005;40(6 Pt1):1836–53. doi: 10.1111/j.1475-6773.2005.00436.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mata-Cases M, Benito-Badorrey B, Roura-Olmeda P, et al. Clinical inertia in the treatment of hyperglycemia in type 2 diabetes patients in primary care. Curr Med Res Opin. 2013;11(29):1495–502. doi: 10.1185/03007995.2013.833089. [DOI] [PubMed] [Google Scholar]
- 6.Voorham J, Haaijer-Ruskamp FM, Wolffenbuttel BHR, et al. Groningen Initiative to Analyse Type 2 Diabetes Treatment (GIANTT) Group. Cardiometabolic treatment decisions in patients with type 2 diabetes: the role of repeated measurements and medication burden. Qual Saf Health Care. 2010;19:411–15. doi: 10.1136/qshc.2008.030106. [DOI] [PubMed] [Google Scholar]
- 7.Grant R, Adams AS, Trinacty CM, et al. Relationship between patient medication adherence and subsequent clinical inertia in type 2 diabetes glycemic management. Diabetes Care. 2007;30:807–12. doi: 10.2337/dc06-2170. [DOI] [PubMed] [Google Scholar]
- 8.Crowley MJ, Smith VA, Olsen MK, et al. Treatment intensification in a hypertension telemanagement trial: clinical inertia or good clinical judgement? Hypertension. 2011;58:552–58. doi: 10.1161/HYPERTENSIONAHA.111.174367. [DOI] [PubMed] [Google Scholar]
- 9.Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–63. doi: 10.1056/NEJM199812313392701. [DOI] [PubMed] [Google Scholar]
- 10.Hyman DJ, Pavlik VN, Vallbona C. Physician role in lack of awareness and control of hypertension. J Clin Hypertens. 2000;2:324–30. [PubMed] [Google Scholar]
- 11.Oliveria SA, Lapuerta P, McCarthy BD, et al. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–20. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 12.Parchman ML, Pugh JA, Romero RL, Bowers KW. Competing demands or clinical inertia: the case of elevated glycosylated hemoglobin. Ann Fam Med. 2007;5:196–201. doi: 10.1370/afm.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Bruggen R, Gorter K, Stolk R, et al. Clinical inertia in general practice: widespread and related to the outcome of diabetes care. Family Practice. 2009;26:428–36. doi: 10.1093/fampra/cmp053. [DOI] [PubMed] [Google Scholar]
- 14.Carratalá-Munuera MC, Gil-Guillen VF, Orozco-Beltran D, et al. Barriers associated with poor control in Spanish diabetic patients. A consensus study. Int J Clin Pract. 2013;67(9):888–94. doi: 10.1111/ijcp.12160. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz FL, Marling CR, Shubrook J. Automated glycemic pattern analysis: overcoming diabetes clinical inertia. J Diabetes Sci Technol. 2013;7(1):167–69. doi: 10.1177/193229681300700121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes (IPCAAD) 8. Arch Intern Med. 2006;166(5):507–13. doi: 10.1001/archinte.166.5.507. [DOI] [PubMed] [Google Scholar]
- 17.Croatian National Institute of Public Health. Croatian Health Service Yearbook. 2011. [cited 2014 Jul 14]. Web edition. Available from: URL: http://hzjz.hr/wp-content/uploads/2013/11/Ljetopis_2011.pdf.
- 18.Croatian National Diabetes Registry. [cited 2014 Jul 14]. Available from: URL: http://www.idb.hr/CDN_2011.pdf.
- 19.Croatian National Diabetes Registry. [cited 2014 Jul 14]. Available from: URL: http://www.idb.hr/CDN_2013.pdf.
- 20.Vrca Botica M, Kovacic L, Katic M, et al. Chronic Patients – Persons with Diabetes Frequent Attenders in Croatian Family Practice. Coll Antropol. 2007;2:509–16. [PubMed] [Google Scholar]
- 21.Ozvacic Adzic Z, Katic M, Kern J, et al. Patient, Physician, and Practice Characteristics Related to Patient Enablement in General Practice in Croatia: Cross-sectional Survey Study. Croat Med J. 2008;49:813–23. doi: 10.3325/cmj.2008.49.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Croatian National Institute of Public Health. Croatian Health Service Yearbook. 2007. [cited 2014 Jul 22]. Web edition. Available from URL: http://hzjz.hr/wp-content/uploads/2013/11/Ljetopis_2007.pdf.
- 23.Croatian Guidelines on Type 2 Diabetes Mellitus. Croatian Association for Diabetes and Metabolic Disorders; [cited 2014 Jul 15]. Available from: URL: http://cro-endo.com/wp-content/uploads/2013/02/HR-smjernice-SBT2-Medix_Medilab-2011-k1.pdf. [Google Scholar]
- 24.Grant RW, Cagliero E, Dubey AK, et al. Clinical inertia in the management of Type 2 diabetes metabolic risk factors. Diabet Med. 2004;21:150–55. doi: 10.1111/j.1464-5491.2004.01095.x. [DOI] [PubMed] [Google Scholar]
- 25.Lázaro P, Murga N, Aguilar D, Hernández-Presa MA on behalf of the INERTIA Study investigators. Therapeutic Inertia in the Outpatient Management of Dyslipidemia in Patients With Ischemic Heart Disease. The Inertia Study. Rev Esp Cardiol. 2010;63(12):1428–37. doi: 10.1016/s1885-5857(10)70277-2. [DOI] [PubMed] [Google Scholar]
- 26.Bolen SD, Bricker E, Samuels TA, et al. Factors Associated With Intensification of Oral Diabetes Medications in Primary Care Provider-Patient Dyads: A Cohort Study. Diabetes Care. 2009;32:25–31. doi: 10.2337/dc08-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Connor PJ. Commentary – improving diabetes care by combating clinical inertia. Health Serv Res. 2005;40:1854–61. doi: 10.1111/j.1475-6773.2005.00437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Preiss D, Ray KK. Intensive glucose lowering treatment in type 2 diabetes. BMJ. 2011;343:d4243. doi: 10.1136/bmj.d4243. [DOI] [PubMed] [Google Scholar]
- 29.Vrca Botica M, Zelic I, Pavlic Renar I, et al. Structure of Visits Persons with Diabetes in Croatian Family Practice – Analysis of Reasons for Encounter and Treatment Procedures using the ICPC-2. Coll. Antropol. 2006;3:495–99. [PubMed] [Google Scholar]
- 30.Starfield B, Lemke KW, Bernhardt T, et al. Comorbidity: implications for the importance of primary care in ‘case’ management. Ann Fam Med. 2003;1:8–14. doi: 10.1370/afm.1. [DOI] [PMC free article] [PubMed] [Google Scholar]