Introduction
The ECG provides important diagnostic information in patients suspected of right ventricular cardiomyopathy/dysplasia. The clinician needs to be aware of the ECG abnormalities in ARVC/D to ascertain the likelihood of patients having this disease. Several reviews of the ECG findings in ARVC/D have been published.1, 2
The ECG changes in ARVC/D reflect the pathophysiology of ARVC/D that is characterized by progressive replacement of myocardial tissue in the free wall of the right ventricle by fibrous and fatty tissue. Normally the free wall of the right ventricle is the last part of the heart to undergo depolarization.3 If there is selective damage to the right ventricular free wall musculature there may be fragmentation and selective slowing and prolongation of the end of the QRS complex and this can be seen in the anterior precordial leads. The delay in depolarization may be extremely prolonged and may be visible as reproducible low frequency, low amplitude waves that extend beyond the QRS complex and before the T wave. These are known as postexcitation or epsilon waves.4 They are of low amplitude, and are usually visible only on the ECG leads overlying the right ventricle.
The diagnose of ARVC/D is based on a comprehensive evaluation of clinical, imaging, and ECG findings from the Task Force Criteria.5 Table 1 shows ECG parameters for the diagnosis of ARVC/D.
Table 1.
ECG-Based Task Force Criteria for Diagnosing ARVC/D
| Repolarization Abnormalities |
| Minor Criteria |
| Inverted T waves in precordial leads (V2 and V3) in absence of right bundle branch block |
| Deplorization/Conduction Abnormalities |
| Major Criteria |
| Epsilon waves or localized prolongation (>110 ms) of QRS in right precordial leads (V1 – V3) |
| Minor Criteria |
| Late potentials (signal-average ECG) |
| Arrhythmias |
| Minor Criteria |
| Left bundle branch block type VT (sustained & nonsustained) by ECG, Holter or exercise testing. |
| Frequent ventricular extrasystoles (>1000/24 hrs) (Holter) |
Anterior Precordial T Wave Inversion
T wave inversion is often a manifestation of myocardial injury. For example, in patients with an anterior myocardial infarction, T wave inversion is a common ECG finding. Likewise, this is an ECG feature in patients with ARVC/D who have right ventricular free wall musculature replaced by fibrous-fatty tissue.6
Data from the NIH Registry of ARVC/D showed that the mean age of diagnosis of ARVC/D was 38 ± 14 years; there was a slight majority of males. In this registry cohort of newly diagnosed patients with ARVC/D, T wave inversion beyond V1 was present in 56% of newly diagnosed patients. (Table 2) T wave inversion was limited to V1 and V2 in 6%, to V1, V2 and V3 in 16%, and extended beyond V3 in 31%. In addition T wave inversion was not found in V2 and V3 but in V4, V5 and V6 in 3%. In normal individuals age 19–45, T wave inversion in V1, V2 and V3 is present in less than 3% of apparently healthy subjects.7 Thus this ECG finding is quite specific and relatively sensitive for the diagnosis. (Figure 1) This pattern of T wave inversion in V1 – V3 or beyond is frequently recorded in normal individuals less than age 14 and has been termed “a juvenile pattern” but this pattern is infrequent in the age group in which ARVC/D usually presents.
Table 2.
Incidence of Electrical Abnormalities on ECG, SAECG, and 24 Hour Holter Monitor in Several Series of Patients with ARVC/D
| Publications | Nava (1) | Peters (10) | Dalal (12) | Cox (13) | NIH Registry Data |
|---|---|---|---|---|---|
| # of Patients | N=136 | N=265 | N=69 | N=42 | N=95 |
| 1) Depolarization and Conduction Abnormalities | |||||
| a) Epsilon Waves | 4% | 23% | 29% | 10% | 1% |
| b) Localized QRS >110msec in V1, V2, or V3 (In Absence of RBBB) | 70% | 58% | 26% | 24% | |
| c) QRS Duration Ratio | 98% | 35% | 17% | ||
| d) Prolonged S Wave Duration | 91%x | 52%x | 34% xx | ||
| Terminal Activation Delay (TAD) | 71%xxx | ||||
| 2) Repolarization Abnormalities | |||||
| Inverted T waves V1 | 18% | ||||
| V1 and V2 | 6% | ||||
| V1 + V2 + V3 | 19% | 31% | 81% xxxx | 67% | 16% |
| Beyond V3 | 18% | 23% | 31% | ||
| Only V4, V5, V6 | 3% | ||||
| 3) LBBB, VT on ECG Holter or Exercise Test | |||||
| a) Sustained VT | 77% | 42% | 35% | ||
| b) 1000 PVCs/24 Hours on Holter | 67% | 28% | 57% |
Prolonged S wave duration from nadir of S wave to isoelectric line >55 msec in leads V1 – V2
From nadir of S wave to end of depolarization (R’)
(TAD) from nadir of S wave to end of all depolarization including an epsilon wave
T ↓ V1 – V3 or beyond
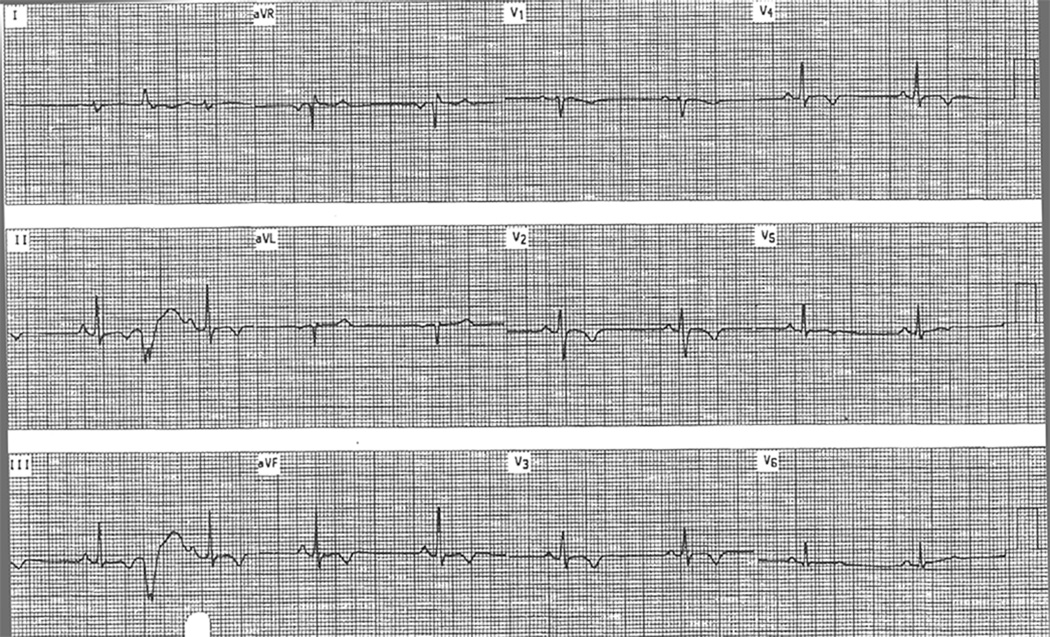
Figure 1.
An ECG from a patient with ARVC/D. The T waves are inverted in V1 –V5. The PVC recorded in leads AVR, AVL, AVF and lead II shows that this PVC is of LBBB configuration and has a superior QRS axis
The extent of the precordial T wave inversion provides an indication of the extent of right ventricular involvement and/or enlargement. In the first detailed clinical profile of this disease 6, T wave inversion in V1 – V4 was found in 86% (19 of 22 patients) in contrast to an incidence of 31% of T wave inversion in V1 – V3 of newly diagnosed patients in the above noted registry. The patients with a high incidence of T wave inversion in V1 – V4 had a more advanced stage of the disease since they were all referred to a tertiary care center because of ventricular tachycardia that was refractory to antiarrhythmic drugs. Nava et al. found that there was a direct correlation between the extent of T wave negativity in the precordial leads and right ventricular enlargement (r=0.89; p=<0.01) 8 Jadou et al noted that T wave inversion in V1 – V3 was observed in 37/74 (50%) of individuals with ARVC/D at time of initial diagnosis and this progressed to (65%) of patients over 9.5 ± 3.25 years.9
Delayed Activation of the Right Ventricle
It has long been recognized that there can be delayed repolarization of the right ventricle due to fibrous - fatty replacement of the cardiac chamber. In 1994 localized prolongation of the QRS complex >110 msec in V1–V3 was included as a minor Task Force Criteria. The frequency of this finding has been reported to range from 24% (23 of 95 ECGs) in the NIH registry to 97 % reported by Peters et al.10. Again, the difference in the incidence of these findings are likely related to the extent of right ventricular structural and functional abnormality.
In recognition of the fact that QRS prolongation selectively involves the right ventricle in this disease, it should primarily affect the terminal portion of the QRS complex. Nasir et al observed that the terminal part of the QRS, defined as the time from the nadir of the S wave to the isoelectric line, was prolonged to > 55 msec. in V1 – V3 in 95% of patients with ARVC/D, in 7% of patients with RVOT tachycardia and in 2% of normal controls.11 A more recent publication from the same center reported that 91% of patients with ARVC/D had a prolonged S wave duration. 12
Selective prolongation of the S wave duration in V1 – V3 has been verified by Cox et al. who reported this finding in 71% (30 of 42 patients). 13 This was defined as the longest value measured from the nadir of the S wave to the end of all depolarization deflections including epsilon waves and was called the terminal activation daily (TAD). Once again the incidence appears to be less in newly diagnosed patients. It was observed in 34% (32 of 95 patients) with ARVC/D in the NIH registry. Reports of the duration of the QRS or S wave has the inherent problem of error of measurement error of these parameters from the standard 12 lead electrocardiogram. Cox et al. reported that individual measurements varied 2.9±3.5 msec. with a range of 0–15 msec.
The epsilon wave may be defined as a reproducible low amplitude deflection on the ECG recording occurring between the end of the QRS complex and the onset of the T wave. This was well described by Fontaine et al. in 1978.4
Fontaine et al recognized that this was a delayed potential that resulted from slow conduction in localized areas of the right ventricle. It can be seen best in leads V1 – V3 since these leads are in close proximity to the right ventricle. When present in the 12 lead ECG it is invariably seen on the signal averaged electrocardiogram as a late potential. Nevertheless the signal averaged electrocardiogram may show late potentials that are not of sufficient amplitude to be visible on the 12 lead electrocardiogram. The presence of the epsilon wave also seems to reflect the extent of right ventricular involvement. It was observed in only one of 95 ECGs in the NIH registry. In patients with recurrent ventricular tachycardia reported in the original clinical description of ARVC/D these ventricular post excitation waves were present on the resting ECG in 7 of 22 patients and was recorded in 13 of 16 patients who had signal averaged electrocardiograms.6
The Electrocardiogram as an Aid to Differentiate Idiopathic VT (RVOT Tachycardia) from ARVC/D
It is important to differentiate individuals with RVOT (idiopathic) ventricular tachycardia from those who have ARVC/D since patients with RVOT tachycardia have an excellent prognosis and arrhythmic death is extremely rare. In contrast, ARVC/D is a progressive disease with frequent recurrence of ventricular tachycardias including the possibility of arrhythmic death. ECG findings that help to differentiate RVOT tachycardia from ARVC/D are shown in Table 3. The QRS morphology can assist in the differential diagnosis.
Table 3.
ECG Findings in RVOT Tachycardia and in ARVC/D
| RVOT | ARVC/D | |
|---|---|---|
| T↓ V1–V3 | 0 –6% | 37–81% |
| Prolonged S wave upstroke V1–V3 (>55 msec) | 4% | 34–91% |
| Epsilon Waves | 0% | 1–29% |
| Superior QRS axis Of LBBB-PVCs or VT (positive in AVL) | 0–4% | 37–67% |
| Multiple VT Morphologies | 0% | 64% |
| QRS Duration in Lead I ≥ 120 msec during VT | ||
| Positive SAECG | 0–12% | 50–80% |
Data from references #1,2,6 –8, 11, 13–17, 19 and from NIH Registry (Table 2)
Large % variation in categories may be due to centers who report data from patients with less or more advanced ARVC/D
The ECG abnormalities described as frequently present in ARVC/D are uncommon in patients with RVOT tachycardia. 14,15,16 This includes T wave inversion in V1, V2, V3 and beyond or evidence of a prolonged terminal portion of the QRS complex (S wave duration of >55 msec) as well as epsilon waves and late potentials. T wave inversion in V1, V2, and V3 was seen in 36% of 17 patients with ARVC/D and 6% of patients with RVOT tachycardia.16 In a recent study, Cox et al. reported T wave inversion in V1, V2, and V3 in 28 of 42 (67% of patients with ARVC/D) but in none (0 of 27) patients with RVOT tachycardia.13 Therefore the standard ECG is a valuable tool to assist in this differential diagnosis.
Patients with RVOT tachycardia invariably will have QRS complex of the ventricular ectopy that is of left bundle branch block morphology that is positive in the inferior leads 2, 3 and AVF and negative in AVL. Patients with ARVC/D may also have this morphology. However, if the ventricular ectopy has a left bundle branch block morphology with a superior QRS axis, this enhances the suspicion that the patient has this condition.
The importance of utilizing the morphology as well as the QRS axis of PVCs or ventricular tachycardia suggests that the physician should try to identify the morphology and the QRS axis from the Holter recording. Although one of the Task Force Criteria is that of the presence of ventricular arrhythmias by Holter monitor of > 1,000 per 24 hour, the recognition that the ventricular arrhythmias are of right bundle branch block rather than left bundle branch block morphology should decrease the suspicion of the presence of right ventricular cardiomyopathy/dysplasia.
The 12 lead electrocardiogram can also provide information to determine whether the left bundle branch block morphology of the ventricular tachycardia may be due to right ventricular outflow tachycardia or ARVC/D. A QRS duration > 120 msec in lead I has a sensitivity of 100%, specificity of 46%, positive predictive value of 61%, and negative predictive value of 100% for ARVC/D.17 The reason for this difference is undoubtedly related to the fact that the rate of depolarization of the right ventricle it slowed in patients with ARVC/D due to fibrous fatty tissue whereas the right ventricular structure and function is normal in patients with ARVC/D with resulting rapid ventricular depolarization.
The Signal Averaged ECG (SAECG) as an Aid in the Diagnosis of ARVC/D
A positive signal averaged electrocardiogram is another minor Task Force Criteria for this diagnosis. Recording of SAECG involves the use of special ECG equipment to markedly increase the amplitude of the QRS complex in order to accurately measure the duration of the QRS complex as well as to observe and measure the small electrical potentials that may occur after the end of the QRS complex.
For the 40 Hz high pass filter, the normal value for filtered QRS duration is ≤ 114 msec, the normal value of low amplitude signal duration below 40 uV (LAS 40) is ≤ 38 msec and the root – mean square voltage in the last 40 msec of the QRS (RMS 401) should be ≥ 20 uV.18 It has become common practice to classify the signal averaged ECG as positive if 2 of the 3 parameters are abnormal, although this categorization is not based on evidence. 18 The presence of abnormal signal averaged ECG may provide information with regard to the differential diagnosis of ARVC/D versus RVOT tachycardia since the incidence of a positive signal averaged ECG is only a few percent in patients with RVOT tachycardia and is in the range of 50–60% or greater in patients with ARVC/D. (Table 1). Late potentials correlate with the severity of the disease but there are conflicting reports as to whether there is a correlation between the presence of late potentials to predict inducibility to ventricular tachycardia in patients with sustained VT. 19,20,21
The ECG to Aid in the Diagnosis of ARVC/D in Family Members
The penetrance of ARVC/D is variable; therefore the expression of the electrical phenomenon would be expected to have a lower incidence and be less severe than in the probands. This was observed by Hamid et al. who suggested that the diagnosis of ARVC/D in family members may be present without their having to fulfill the Task Force Criteria established for the probands.22 One major Task Force Criteria in addition to an established diagnosis of ARVC/D in a family member has been proposed as a diagnostic criteria for family members. A modification of the Task Force Criteria suggested by Hamid et al. is a PVC frequency of >200 PVCs per 24 hours rather than 1,000 PVCs for probands. This is based on the observation that the frequency of PVCs in a normal individual < 40 years of age is generally less than 200 PVCs per 24 hours and is frequently < 50 PVCs per 24 hours in individuals below the age of 20. A positive signal averaged ECG is also a useful criteria to suspect the diagnosis of ARVC/D in family members.
Summary
The electrical manifestations of right ventricular dysplasia are important to aid in the diagnosis of ARVC/D and also in the differential diagnosis of ARVC/D versus RVOT tachycardia. The findings are based on the pathophysiology of right ventricular free wall replacement of musculature by fibrous and fatty tissue causing abnormal repolarization as well as slow and delayed conduction.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nava A, Buja G, Corrado D. In: Electrocardiographic features in Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia. Nava A, Rossi G, Thiene G, editors. The Netherlands: Elsevier Science; 1997. pp. 186–196. [Google Scholar]
- 2.Zareba W, Piotrowicz K, Turrini P. In: Electrocardiographic manifestations in Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia. Marcus FI, Nava A, Thiene G, editors. Italia: Springer-Verlag; 2007. pp. 121–128. [Google Scholar]
- 3.Durrer D, Van Dam THR, Freud GE, Janse MJ, Meijler FL, Arzbaecher RC. Total excitation of the isolated human heart. Circulation. 1970;16:899–912. doi: 10.1161/01.cir.41.6.899. [DOI] [PubMed] [Google Scholar]
- 4.Fontaine G, Guiraudon G, Frank R. Intramyocardial conduction defects in patients prone to chronic ventricular tachycardia.I. The postexcitation syndrome in sinus rhythm. In: Sandoe E, Julian DG, Bell JW, editors. Management of ventricular tachycardia – role of mexilitine. Amsterdam-Oxford: Exerpta Medica; 1978. pp. 39–55. [Google Scholar]
- 5.McKenna WJ, Thiene G, Nava A, Fontaliran F, Blomstrom-Lundquist C, Fontaine G, Camerini F. Diagnosis of arrhythmogenic right ventricular dysplasia, cardiomyopathy. Br. Heart. J. 71:215–218. doi: 10.1136/hrt.71.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcus FI, Fontaine GH, Guiraudon G, Frank R, Laurenceau JL, Malergue C, Grosgogeat Y. Right ventricular dysplasia: A report of 24 adult cases. Circulation. 1982;65:384–398. doi: 10.1161/01.cir.65.2.384. [DOI] [PubMed] [Google Scholar]
- 7.Marcus FI. Prevalence of T wave inversion beyond V1 in young normal individuals and usefulness for the diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia. Am. J. Cardiol. 2005;95:1070–1071. doi: 10.1016/j.amjcard.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 8.Nava A, Canciani B, Buja G, Martini B, Daliento L, Scognamiglio R, Thiene G. Electrovectorcardiographic study of negative T waves on precordial leads in arrhythmogenic right ventricular dysplasia: Relationship with right ventricular volumes. J. Electrocardiology. 1988;21:239–245. doi: 10.1016/0022-0736(88)90098-2. [DOI] [PubMed] [Google Scholar]
- 9.Jaoude SA, Leclercq JF, Coumel P. Progressive ECG changes in arrhythmogenic right ventricular disease. Evidence for an evolving disease. Eur Heart J. 1996;17:1717–1722. doi: 10.1093/oxfordjournals.eurheartj.a014756. [DOI] [PubMed] [Google Scholar]
- 10.Peters S, Trummel M. Diagnosis of arrhythmogenic right ventricular dysplasia-cardiomyopathy: Value of standard ECG revisited. A.N.E. 2003;8:238–245. doi: 10.1046/j.1542-474X.2003.08312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nasir K, Bomma C, Tandri H, Roquin A, Dalal D, Prakasa K, Tichnell C, James C, Jspevak P, Marcus F, Calkins H. Electrocardiographic features of arrhythmogenic right ventricular dysplasia/cardiomyopathy according to disease severity. A need to broaden diagnostic criteria. Circulation. 2004;110:1527–1534. doi: 10.1161/01.CIR.0000142293.60725.18. [DOI] [PubMed] [Google Scholar]
- 12.Dalal D, Nasir K, Bomma C, Prakasa K, Tandri H, Piccini J, Roquin A, Tichnell C, James C, Russell SD, Judge DP, Abraham T, Spevak PJ, Bluemke DA, Calkins H. Arrhythmogenic right ventricular dysplasia: A United States experience. Circulation. 2005;112:3823–3832. doi: 10.1161/CIRCULATIONAHA.105.542266. [DOI] [PubMed] [Google Scholar]
- 13.Cox MGPJ, Nelen MR, Wilde AAM, Wiesfeld ANSC, Van Der Smagt J, Loh P, Cramer MJ, Doevendans PA, Van Tintelen JP, De Bakker JMT. Hauer RNW. Activation delay and VT parameters in arrhythmogenic right ventricular dysplasia/cardiomyopathy: Toward improvement of diagnostic ECG criteria. J. Cardiovasc Electrophysiol. 2008;19:775–781. doi: 10.1111/j.1540-8167.2008.01140.x. [DOI] [PubMed] [Google Scholar]
- 14.Niroomand F, Carbucicchio C, Tondo C, Riva S, Fassini G, Apostolo A, Trevisi N, Della Bella P. Electrophysiological characteristics and outcome in patients with idiopathic right ventricular arrhythmia compared with arrhythmogenic right ventricular dysplasia. Heart. 2002;87:41–47. doi: 10.1136/heart.87.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Donnell D, Cox D, Bourke J, Mitchell L, Furniss S. Clinical and electrophysiological differences between patients with arrhythmogenic right ventricular dysplasia and right ventricular outflow tract tachycardia. European Heart Journal. 2003;24:801–810. doi: 10.1016/s0195-668x(02)00654-1. [DOI] [PubMed] [Google Scholar]
- 16.Proclemer A, Ciani R, Feruglio GA. Right ventricular tachycardia with left bundle branch block and inferior axis morphology: Clinical and arrhythmological characteristics in 15 patients. PACE. 1989;12:977–988. doi: 10.1111/j.1540-8159.1989.tb05035.x. [DOI] [PubMed] [Google Scholar]
- 17.Ainsworth CD, Skanes AC, Klein GJ, Gula LJ, Yee R, Krahn AD. Differentiating arrhythmogenic right ventricular cardiomyopathy from right ventricular outflow tract ventricular tachycardia using multilead QRS duration and axis. Heart Rhythm. 2006;3:416–432. doi: 10.1016/j.hrthm.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 18.Marcus FI, Zareba W, Sherrill D. Evaluation of the normal values for signal averaged electrocardiogram. J. Cardiovasc Electrophysiol. 2007;18:231–233. doi: 10.1111/j.1540-8167.2006.00685.x. [DOI] [PubMed] [Google Scholar]
- 19.Nava A, Folino AF, Bauce B, Turrini P, Buja GF, Daliento L, Thiene G. Signal averaged electrocardiogram in patients with arrhythmogenic right ventricular dysplasia. Prevalence, diagnostic and prognostic values. Eur Heart J. 1993;14(Suppl E):80–83. doi: 10.1053/euhj.1999.1733. [DOI] [PubMed] [Google Scholar]
- 20.Nasir K, Tandri H, Rutberg J, Tichnell C, Spevak P, Crossan J, Baughman KL, Kasper EK, Tomaselli GF, Berger R, Calkins H. Filtered QRS duration on signal averaged electrocardiographic predicts inducibility of ventricular tachycardia in arrhythmogenic right ventricle dysplasia. PACE. 2003;26:1055–1960. doi: 10.1046/j.1460-9592.2003.00302.x. [DOI] [PubMed] [Google Scholar]
- 21.Turrini P, Corrado D, Basso C, Nava A, Thiene G. Noninvasive risk stratification in arrhythmogenic right ventricular cardiomyopathy. A.N.E. 2003;8:161–169. doi: 10.1046/j.1542-474X.2003.08212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamid MS, Norman M, Quraishi A, Firoozi S, Thaman R, Gimeno JR, Sachdev B, Rowland E, Elliot PM, McKenna WJ. Prospective evaluation of relatives for familial arrhythmogenic right ventricular cardimyopathy/dysplasia reveals a need to broaden diagnostic criteria. J. Am Coll Cardiol. 2002;40:1445–1450. doi: 10.1016/s0735-1097(02)02307-0. [DOI] [PubMed] [Google Scholar]