Abstract
IMPORTANCE
Serotonergic system dysfunction has been associated with increased lethal suicide attempts and suicide. Dysfunction includes higher binding of serotonin1A autoreceptor in the brainstem raphe of individuals who die by suicide.
OBJECTIVES
To determine the relationships between brain serotonin1A binding and suicidal behavior in vivo in major depressive disorder (MDD) using positron emission tomography and the serotonin1A antagonist radiotracer carbon C 11 [11C]–labeled WAY-100635.
DESIGN, SETTING, AND PARTICIPANTS
Cross-sectional positron emission tomography study at an academic medical center from 1999 through 2009. We compared serotonin1A binding between individuals with MDD who did not attempt suicide (nonattempters) (n = 62) and those who attempted suicide (attempters) (n = 29). We subdivided the attempters into those with lower (n = 16) and higher (n = 13) levels of lethality.
MAIN OUTCOMES AND MEASURES
The binding potential (BPF) of [11C]WAY-100635 (calculated as the number of receptors available divided by affinity) in the prefrontal cortex (PFC) and brainstem, estimated by kinetic modeling with an arterial input function; the severity of suicidal behaviors, including lethality and intent of suicide attempts; and suicidal ideation.
RESULTS
Using a linear mixed-effects model, we found no difference between attempters and nonattempters with MDD in serotonin1A BPF in the PFC regions (F1,88 = 0.03; P = .87) or in the raphe nuclei (F1,88 = 0.29; P = .59). Raphe nuclei serotonin1A BPF was 45.1% greater in higher-lethality attempters compared with lower-lethality attempters (F1,25 = 7.33; P = .01), whereas no difference was observed in the PFC regions (F1,25 = 0.12; P = .73). Serotonin1A BPF in the raphe nuclei of suicide attempters was positively correlated with the lethality rating (F1,25 = 10.56; P = .003) and the subjective lethal intent factor (F1,25 = 10.63; P = .003; R2 = 0.32) based on the most recent suicide attempt. Suicide ideation in participants with MDD was positively correlated with serotonin1A BPF in the PFC regions (F1,88 = 5.19; P = .03) and in the raphe nuclei (F1,87 = 7.38; P = .008; R2 = 0.12).
CONCLUSIONS AND RELEVANCE
Higher brainstem raphe serotonin1A BPF observed in higher-lethality suicide attempters with MDD is in agreement with findings in suicide studies and also with the finding of low cerebrospinal fluid levels of 5-hydroxyindoleacetic acid in higher-lethality suicide attempters. Higher brainstem raphe serotonin1A BPF would be consistent with lower levels of serotonin neuron firing and release and supports a model of impaired serotonin signaling in suicide and higher-lethality suicidal behavior. Severity of suicidal ideation in MDD is related to brainstem and prefrontal serotonin1A BPF, suggesting a role for both regions in suicidal ideation. Lower levels of serotonin release at key brain projection sites, such as the prefrontal regions, may favor more severe suicidal ideation and higher-lethality suicide attempts.
Suicide claimed the lives of more than 38 000 individuals in the United States in 2010.1 Although the majority of suicides occur in the setting of a current psychiatric disorder, most commonly major depressive disorder (MDD),2 most individuals with MDD never attempt suicide. Of those who do, fewer make higher-lethality attempts, confounding efforts to detect and mitigate suicide risk. Thus, an urgent need exists for in vivo biomarkers of suicide risk to assist clinical identification and management of such high-risk patients.
Biological studies of suicidal behaviors occurring within major depressive episodes repeatedly have identified evidence of central serotonin system hypofunction. Low cerebrospinal fluid (CSF) levels of 5-hydroxyindoleacetic acid (5-HIAA), serotonin’s primary metabolite within the central nervous system, have been associated with prior suicide attempts, particularly violent and/or highly lethal attempts, and the prospective risk for suicide.2–10 Serotonin release in response to the serotonergic agent fenfluramine hydrochloride also appears to be impaired in individuals with higher-lethality suicide attempts (attempters), as indicated by a blunted prolactin response.11 In higher-lethality suicide attempters, the suicidal intent is greater and the CSF levels of 5-HIAA are lower; a lifetime history of more severe aggression is also correlated with lower CSF levels of 5-HIAA.12–14 However, CSF measures and neuroendocrine challenge studies do not provide information about the anatomical location of brain abnormalities within the serotonergic system or offer an explanation of the mechanism responsible for lower-level functioning of the serotonin system.
Uptake of fludeoxyglucose F 18 (FDG) in positron emission tomography (PET) is lower in the ventral, medial, and lateral prefrontal cortex (PFC) in higher-lethality suicide attempters who are depressed compared with lower-lethality attempters who are depressed; these differences become more pronounced on challenge with fenfluramine and are related to higher levels of suicidal intent and lower levels of impulsiveness.9 Suicidal intent is also related to lower uptake of carbon C 11 [11C]–labeled methyltryptophan in the ventromedial PFC,15 whereas aggression is related to lower ventromedial FDG uptake in the PFC16,17 and lower serotonin transporter binding in the anterior cingulate.18 These findings provide some possible regional specificity to serotonergic abnormalities related to suicidality.
Postmortem studies of individuals who die by suicide (completers) find differences in serotonergic system markers in the brainstem and PFC regions. Findings include higher binding of serotonin1A autoreceptor in the dorsal raphe nucleus in suicides,19 particularly in the rostral dorsal raphe nucleus,20 and higher levels of serotonin1A autoreceptor binding in the ventrolateral PFC,21,22 although not all studies find the PFC difference.23
Cerebrospinal fluid 5-HIAA and PET FDG uptake studies in higher-lethality suicide attempters and serotonin1A binding in suicide completers post mortem suggest a common biological substrate between suicide and higher-lethality nonfatal suicide attempts in MDD. In contrast, serotonergic function in lower-lethality suicide attempters appears more similar to that of individuals who do not attempt suicide (hereinafter referred to as nonattempters). Therefore, we assessed the relationship between serotonin1A binding in vivo and a history of suicide attempts in a large cohort with current MDD using PET imaging and the serotonin1A antagonist radiotracer [11C]WAY-100635. We hypothesized that we would find higher levels of binding in the PFC and midbrain raphe nuclei in higher-lethality suicide attempters with MDD compared with lower-lethality attempters with MDD. We also explored correlations between serotonin1A autoreceptor binding and the severity of suicidal ideation and depression psychopathology.
Methods
Participants
The institutional review board of the New York State Psychiatric Institute approved the protocol. All participants provided written informed consent for study procedures.
We included 91 individuals who met DSM-IV criteria for a current major depressive episode and a diagnosis of MDD in this secondary analysis of data from a sample largely overlapping but expanded from previous reports.24–26 This sample included 29 suicide attempters (consisting of 16 lower-lethality and 13 higher-lethality suicide attempters defined by a median split based on the lethality rating of the most recent suicide attempt). Inclusion criteria were assessed through psychiatric interview, medical record review, the Structured Clinical Interview for DSM-IV, Patient Edition,27 physician-obtained medical history, review of systems, results of a physical examination, and results of laboratory tests. These tests included a complete blood cell count, chemistry panel, thyroid function tests, urinalysis, and urine screening for drugs; female participants also underwent pregnancy testing. The diagnosis of MDD based on the Structured Clinical Interview for DSM-IV was conducted by experienced research masters- and doctoral-level psychologists. A team of experienced clinical research psychologists and psychiatrists (G.M.S., M.A.O., and A.B.) reviewed all diagnoses. The scores for the MDD diagnosis were greater than 0.85. The Beck Depression Inventory,28 Hamilton Depression Rating Scale (the 17-item scale for screening and the 24-item scale for severity correlations with binding),29 and Global Assessment Scale30 assessed subjective and objective depression severity and functional impairment, respectively. Diagnoses of Axis II personality disorder were determined using the Structured Clinical Interview for DSM-IV Axis II Personality Disorders.31 The behavioral data reported on suicide attempts refer to the most recent attempt for participants reporting more than 1 attempt. All suicide attempt data were gathered using the Columbia Suicide History Form,32 which uses clinical probes and anchor points to identify suicide attempts chronologically that meet the Columbia Classification Algorithm of Suicide Assessment criteria33 and documents the method and medical damage of each suicide attempt. The Medical Lethality Scale34 scores medical damage caused by a suicide attempt on a scale ranging from 0 (no injury) to 8 (fatal), with anchor points dependent on the method of the attempt. The assessment also incorporates the Beck Scale for Suicide Ideation35 for all participants and the Beck Suicide Intent Scale34 for attempters. Ratings of suicidal intent components were based on a 2-factor solution resulting from a prior analysis of the Beck Suicide Intent Scale.36 Factor 1, termed lethal intent, is the sum of items pertaining to subjective intent. Factor 2, termed planning, is the sum of the items pertaining to the objective degree of planning for the attempt. Lifetime history of aggression was measured by the Brown-Goodwin Lifetime History of Aggression Scale.37
Inclusion criteria for all participants consisted of age 18 to 65 years, DSM-IV criteria for a current major depressive episode and MDD, a 17-item Hamilton Depression Rating Scale29 score greater than 16, and the capacity to provide informed consent. Exclusion criteria were a history of alcohol or substance abuse or dependence not in remission for at least the preceding 6 months; lifetime exposure to 3,4-methylenedioxymethamphetamine more than 2 times; significant unstable medical conditions; pregnancy; and a diagnosis of psychosis, bipolar disorder, or schizophrenia. All participants were free of psychotropic medications for at least 2 weeks (6 weeks for fluoxetine hydrochloride and 4 weeks for neuroleptics) with the exception of short-acting benzodiazepines, which could be used as needed up to 72 hours before PET scanning for treatment of anxiety or insomnia. Results of the urine toxicology screen were negative for all participants enrolled.
Sixteen of the 91 participants met criteria for past alcohol or substance abuse or dependence (with remission for >6 months before the PET studies). Six participants had past cannabis abuse; 1, past cannabis dependence; 3, past cocaine abuse; 1, past stimulant abuse; 1, past stimulant dependence; 8, past alcohol abuse; 3, past alcohol dependence; and 2, past hallucinogen abuse. None had a history of crack cocaine use disorder.
In this sample, the time from the most recent suicide attempt to PET imaging ranged from 9 days to 36.8 years. The mode was 1008 days, and the mean (SD) interval was 6.8 (9.5) years.
History of Medication Use
A previous study26 has shown that antidepressant-naive individuals with current MDD have higher [11C]WAY-100635 binding potential (BPF) values in the brain, indicating higher serotonin1A binding compared with healthy volunteers. In a comprehensive replication of this effect of MDD on serotonin1A binding,25 patients with MDD were categorized as not recently receiving medication (NRM) and recently receiving medication (RM), with NRM defined as no history of antidepressant exposure within the 4 years before the study. The NRM group included patients with MDD and no lifetime antidepressant exposure and patients with MDD who were not treated with antidepressants for at least the previous 4 years because those 2 groups did not differ in their composite binding data.
We used this classification in the present analyses, which include a larger sample of NRM (n = 49) and RM (n = 42) participants with MDD than in the previous studies.25,26 Those participants who could not recall the name or dose of a medication or the duration of therapy and for whom records of medication history were otherwise unavailable were classified as indeterminate (n = 13) and were not included. Because lower levels of binding were observed in the RM group,25 this potential medication effect was controlled for in all analyses.
The sample of NRM participants with MDD in the present study has 19 additional participants added to the previously described sample of 30 participants concerning the effect of MDD on serotonin1A binding.25 Sixty-three additional participants with MDD were added to the 28 participants with MDD in the previous report of an effect of MDD on serotonin1A binding.26
Radiochemistry and Input Function Measurement
Preparation of [11C]WAY-100635 and measurement of the arterial input function, metabolites, and plasma-free fraction (fP) have been described previously.38,39 Radioligand metabolite data were collected during the first 60 minutes; we were unable to quantify metabolites beyond this time point.
Image Acquisition and Analysis
The PET imaging was performed on a commercially available scanner (ECAT EXACT HR+; Siemens/CTI). Emission data were collected for 110 minutes as 20 successive frames of increasing duration. Image analysis was performed using graphics software (MATLAB 2006b; MathWorks) with extensions to the Functional Magnetic Resonance Imaging of the Brain’s Linear Image Registration Tool (FLIRT), version 5.240; the Brain Extraction Tool, version 1.241; Statistical Parametric Mapping normalization42; and segmentation routines.43 To correct for participant motion during the PET scan, denoising filter techniques were applied to all PET images starting at frame 5. All frames were aligned using rigid-body FLIRT to frame 8. A mean of motion-corrected frames 8 through 18 was registered to the magnetic resonance image (MRI) using FLIRT. Acquisition of the T1-weighted MRI for coregistration of PET images and identification of regions of interest (ROIs) was performed as previously described using a 1.5-T (Signa Advantage; General Electric) or a 3-T (Signa HDx; General Electric) system.39 The ROIs were hand drawn on the MRI by experienced technicians trained to reliably approximate these regions using brain atlases44,45 and published reports46,47 and who were blinded to the clinical data. The ROIs included the dorsolateral, medial, and ventral PFC and the anterior cingulate cortex. A fixed-volume elliptical ROI (2 cm3) was placed on the raphe nuclei in the dorsal midbrain on a mean PET image, as previously described.26 A cylindrical ROI was drawn in the cerebellar white matter (CWM), which served as the reference region.38 The ROI contours were processed using the segmented MRI to confine analyses in cortical regions to gray matter voxels.
Derivation of Regional Outcome Measures
The outcome measure of choice in PET neuroreceptor studies is the total number of receptors available (Bavail) in vivo to bind the radioligand divided by the receptor ligand affinity (KD). However, without multiple injections and occupancy of the receptors, current technology permits only measurement of BPF = Bavail/KD. Fortunately, no evidence exists for alterations in serotonin1A KD in depression.21 Regional distribution volumes (V) of [11C]WAY-100635 are derived from kinetic analysis using the arterial input function and a 2-tissue compartment model.39 The distribution volumes of the nondisplaceable (VND) and specific (VS) compartments were defined.48 The total regional equilibrium distribution volume (VT) was equal to the sum of VND and VS. Time activity curves were fit with a 2-tissue compartment model, with the K1:K2 ratio fixed to that of the CWM (the reference region with virtually no serotonin1A). For the CWM, a1-tissue compartment model was used.38 We calculated the BPF as (VT(ROI) − VT(CWM))/fP. The contribution of plasma total activity to the regional activity was calculated assuming a 5% blood volume in the ROI and subtracted from the regional activity before statistical analyses. Kinetic parameters were derived by nonlinear regression using software programmed in MATLAB. The BPF measures maximum specific binding divided by KD and involves the fewest assumptions about tracer delivery, clearance, and protein binding. Although some uncertainty remained in measuring fP, we expected that the extent of the participant-to-participant variability in fP relative to the noise in measuring it justifies adjusting for it on the participant level. Partial volume effects should be comparable for higher- and lower-lethality suicide attempters. To some degree, the effect of fP and any other index on measurement error is mitigated by the weightings that we used.
Statistical Analysis
To borrow strength across ROIs and to account for correlation among ROIs properly in the same participant, we fit linear mixed-effects models to the ROI-level BPF estimates, with region and group as fixed effects and participant as the random effect, providing a powerful test of our primary hypothesis without the need to correct for multiple comparisons. To stabilize variance across regions, adjust for slight skewness in distribution of binding measures, and allow a proportional change in binding across regions, we fit the model to log-transformed binding potentials. Log transformation has been used in multiple previous PET studies25,26,49–56 to address these issues. Other groups have used related statistical approaches, including linearizing transformation57 and nonparametric testing,58 to address these issues in analyzing PET data. Demonstrating a difference in log (BPF) is equivalent to demonstrating a difference in the same direction of raw BPF because the natural log is a monotone transformation. We computed estimated SEs using a bootstrap algorithm that takes into account errors in metabolite, plasma, and brain data,59 with observations weighted accordingly. Analyses controlled for recent (within 15-1460 days of PET) history of antidepressant use (RM vs NRM) and sex.25,60 Models were fit using the nlme package in the R software environment (http://www.r-project.org). Additional statistical analyses, including the t test, χ2 test, and Fisher exact test, were performed using commercially available software (SPSS Statistics, version 20.0 [IBM Corp, 2011] or R software). All tests were 2 tailed.
Results
Serotonin1A BPF in Nonattempters Compared With Attempters
Clinical and demographic characteristics of the nonattempters and attempters with MDD are summarized in Table 1. The nonattempters were older than the attempters by a mean of about 6 years. Attempters had higher levels of suicidal ideation in the 2 weeks before PET, lower Global Assessment Scale scores, and greater hopelessness and were younger at the onset of MDD. Otherwise, the nonattempter and attempter groups were comparable on educational level, clinician- and self-rated depression severity, lifetime aggression, and the Reasons for Living Scale score. We found no group differences in radioligand administration parameters, that is, specific activity or injected dose of [11C]WAY-100635, or in the injected mass of WAY-100635. In addition, we found no group differences in the radiotracer-free fraction (fP) in plasma or in the VT of the reference region (VT(CWM)). Age was not related to serotonin1A BPF in the raphe nuclei (P = .93) or the PFC (P = .62). The age at onset of MDD was not related to serotonin1A BPF in the raphe nuclei (P = .54) or the PFC (P = .20). No differences were found in brainstem raphe serotonin1A BPF in relation to lifetime history of suicide attempts (ie, attempters vs nonattempters with MDD) (F1,88 = 0.29; P = .59) or in the PFC BPF (F1,88 = 0.03; P = .87) between these 2 groups.
Table 1.
Demographic and Clinical Characteristics of the Attempter and Nonattempter MDD Groupsa
| Characteristic | Study Group
|
Group Comparison
|
|||
|---|---|---|---|---|---|
| Suicide Nonattempters (n = 62) | Suicide Attempters (n = 29) | Test Statistic | P Value | ||
| Age, y | 40.4 (12.4) | 34.6 (12.3) | t89 = 2.11 | .04 | |
|
| |||||
| Educational level, y | 14.9 (3.2) | 14.1 (4.3) | t89 = 1.03 | .31 | |
|
| |||||
| HDRS-24 score | 25.7 (6.7) | 27.6 (6.1) | t89 = −1.29 | .20 | |
|
| |||||
| Beck Depression Inventory score | 26.8 (9.6) | 30.7 (10.4) | t87 = −1.73 | .09 | |
|
| |||||
| Beck SSI score | 3.4 (5.5) | 9.7 (11.6) | t89 = −3.52 | .001 | |
|
| |||||
| Beck Suicide Intent Scale score | NA | 14.4 (5.0) | |||
|
| |||||
| Lethality of attempt score | NA | 1.6 (1.7) | |||
|
| |||||
| Lifetime aggression scoreb | 18.2 (4.9) | 19.2 (5.1) | t75 = −0.83 | .41 | |
|
| |||||
| Global Assessment Scale score | 54.0 (10.6) | 48.0 (10.9) | t89 = 2.52 | .01 | |
|
| |||||
| Reasons for Living Scale score | 2.2 (2.4) | 1.6 (1.9) | t89 = 1.03 | .30 | |
|
| |||||
| Beck Hopelessness Scale score | 9.9 (6.7) | 13.3 (5.3) | t89 = −2.39 | .02 | |
|
| |||||
| Age at onset of MDE, y | 23.5 (12.1) | 17.9 (10.3) | t89 = 2.17 | .03 | |
|
| |||||
| Female sex, % | 64.5 | 65.5 |
|
.93 | |
|
| |||||
| Cluster B personality disorder, % | 12.2 | 32.0 | Fisher exact test | .06 | |
|
| |||||
| Lifetime history of abuse, % | 56.7 | 60.7 |
|
.72 | |
|
| |||||
| History of abuse before 15 years of age, % | 45.0 | 46.4 |
|
.90 | |
|
| |||||
| SSI score >0 at baseline, %c | 37.1 | 48.3 |
|
.31 | |
|
| |||||
| Specific activity, mCi/nmol | 3.85 (1.80) | 3.55 (1.85) | t89 = 0.72 | .47 | |
|
| |||||
| Injected dose, mCi/kg | 0.09 (0.05) | 0.10 (0.04) | t89 = −0.96 | .34 | |
|
| |||||
| Injected mass, mg/kg | 0.02 (0.01) | 0.03 (0.02) | t89 = −1.69 | .09 | |
|
| |||||
| fP, % | 6.44 (2.26) | 6.21 (2.13) | t89 = 0.45 | .65 | |
|
| |||||
| VT(CWM), mL/cm3 | 0.29 (0.09) | 0.27 (0.10) | t89 = 0.89 | .38 | |
Abbreviations: fP, plasma-free fraction; HDRS-24, 24-item version of Hamilton Depression Rating Scale; MDD, major depressive disorder; MDE, major depressive episode; NA, not applicable; SSI, Scale for Suicide Ideation; VT(CWM), volume of distribution in cerebellar white matter.
SI conversion factor: To convert millicuries to millibecquerels, multiply by 3.7 × 1010.
Unless otherwise indicated, data are expressed as mean (SD).
Determined using the Brown-Goodwin Lifetime History of Aggression Scale for 51 nonattempters and 26 attempters.
Indicates some ideation is present at entry into the study.
Serotonin1A BPF in Lower- vs Higher-Lethality Attempters
Clinical and demographic characteristics of the lower- and higher-lethality attempters with MDD are summarized in Table 2. In addition to a higher mean lethality score of the most recent suicide attempt, the higher-lethality group also had greater suicidal intent. Otherwise, both attempter subgroups were comparable on demographic and clinical variables and the radiotracer administration parameters fP and VT(CWM).
Table 2.
Demographic and Clinical Characteristics of the Higher- and Lower-Lethality Attempter Subgroups With MDDa
| Characteristic | Study Subgroup
|
Group Comparison
|
|||
|---|---|---|---|---|---|
| Lower-Lethality Attempters (n = 16) | Higher-Lethality Attempters (n = 13) | Test Statistic | P Value | ||
| Age, y | 30.8 (13.0) | 39.2 (9.9) | t27 = −1.92 | .07 | |
|
| |||||
| Educational level, y | 13.0 (5.4) | 15.4 (1.8) | t27 = −1.53 | .14 | |
|
| |||||
| HDRS-24 score | 27.1 (6.2) | 28.2 (6.1) | t27 = −0.48 | .64 | |
|
| |||||
| Beck Depression Inventory score | 28.8 (10.5) | 32.9 (12.3) | t27 = −1.03 | .31 | |
|
| |||||
| Beck SSI score | 6.4 (10.5) | 13.7 (12.1) | t27 = −1.73 | .09 | |
|
| |||||
| Beck Suicide Intent Scale score | 12.1 (5.1) | 17.2 (3.2) | t27 = −3.12 | .004 | |
|
| |||||
| Lethality of attempt score | 0.3 (0.5) | 3.2 (1.3) | t14.644 = −7.68 | <.001 | |
|
| |||||
| Lifetime aggression scoreb | 20.1 (5.0) | 18.3 (5.4) | t27 = 0.87 | .39 | |
|
| |||||
| Global Assessment Scale score | 49.4 (10.8) | 46.2 (11.1) | t27 = 0.77 | .45 | |
|
| |||||
| Reasons for Living Scale score | 2.1 (2.2) | 1.1 (1.4) | t27 = 1.40 | .17 | |
|
| |||||
| Beck Hopelessness Scale score | 13.6 (4.5) | 13.0 (6.5) | t27 = 0.28 | .78 | |
|
| |||||
| Age at onset of MDE, y | 17.9 (12.2) | 17.9 (7.9) | t27 = 0.01 | .99 | |
|
| |||||
| Female sex, % | 62.5 | 69.2 | Fisher exact test | >.99 | |
|
| |||||
| Cluster B personality disorder, % | 46.2 | 16.7 | Fisher exact test | .20 | |
|
| |||||
| Lifetime history of abuse, % | 80.0 | 38.5 |
|
.03 | |
|
| |||||
| History of abuse before 15 years of age, % | 60.0 | 30.8 |
|
.12 | |
|
| |||||
| SSI score >0 at baseline, %c | 37.5 | 61.5 |
|
.20 | |
|
| |||||
| Specific activity, mCi/nmol | 3.48 (1.56) | 3.65 (2.21) | t27 = −0.25 | .80 | |
|
| |||||
| Injected dose, mCi/kg | 0.10 (0.04) | 0.10 (0.05) | t27 = −0.13 | .90 | |
|
| |||||
| Injected mass, mg/kg | 0.02 (0.01) | 0.03 (0.03) | t27 = −0.57 | .57 | |
|
| |||||
| fP, % | 6.36 (2.62) | 6.03 (1.39) | t27 = 0.42 | .68 | |
|
| |||||
| VT(CWM), mL/cm3 | 0.27 (0.10) | 0.28 (0.12) | t27 = −0.32 | .75 | |
Abbreviations: See Table 1.
SI conversion factor: To convert millicuries to millibecquerels, multiply by 3.7 × 1010.
Unless otherwise indicated, data are expressed as mean (SD).
Determined using the Brown-Goodwin Lifetime History of Aggression Scale for 13 higher- and 13 lower-lethality attempters.
Indicates some ideation is present at entry into the study.
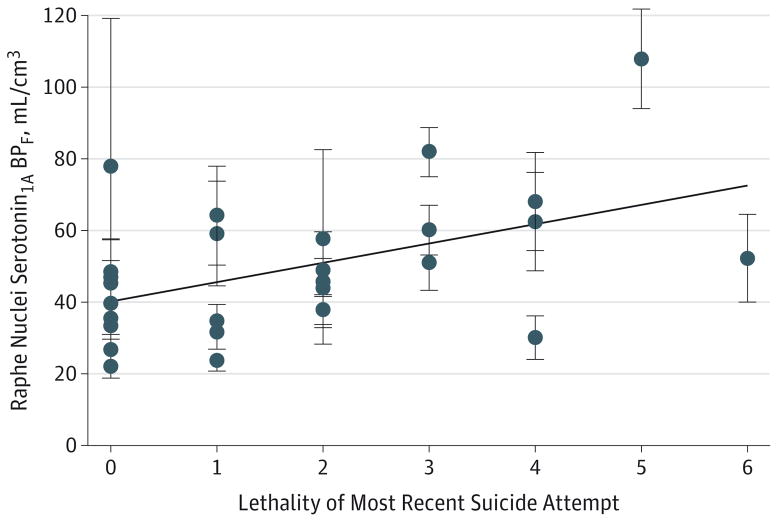
The higher-lethality attempters with MDD had higher serotonin1A BPF in the raphe nuclei compared with the lower-lethality attempters with MDD (F1,25 = 7.33; P = .01). Binding of the serotonin1A autoreceptor was 45.1% higher in the higher-lethality attempters. In all attempters with MDD, the lethality rating and serotonin1A BPF binding in the raphe nuclei were positively correlated (F1,25 = 10.56; P = .003; R2 = 0.32) (Figure 1). In contrast in the PFC, serotonin1A BPF did not differ between the higher- and lower-lethality attempter groups (X vs X; F1,25 = 0.12; P = .73). We found no relationship between lethality and the PFC serotonin1A BPF (F1,25 = 1.70; P = .20). No effects of sex (F1,25 = 0.04; P = .85) or prior anti-depressant status (F1,25 = 1.04; P = .32) on raphe nuclei binding were observed.
Figure 1. Bivariate Plot of the Relationship Between Raphe Nuclei Serotonin1A Binding Potential (BPF) and Lethality Rating of the Most Recent Suicide Attempt.
Participants include the 29 suicide attempters with major depressive disorder (MDD). Error bars depict associated SE; diagonal line, the fitted curve; and slope, the correlation. Lethality of the attempt was measured using the Beck Medical Lethality Scale (scores range from 0 to 6, and the scale scores to 8, which designates a fatal attempt) (F1,25 = 10.56; P = .003; R2 = 0.32). Displayed serotonin1A BPF estimates have been adjusted for sex and prior antidepressant use derived from the specific linear mixed-effects model examining the relationship of raphe nuclei serotonin1A BPF with lethality for all suicide attempters with MDD. For display purposes, 1 lower-lethality attempter with a very high serotonin1A BPF and SE is not included in this plot but was included in all the statistical analyses.
When the presence of a cluster B personality disorder diagnosis was considered as a predictor in the model, the effect of lethality on the raphe nuclei serotonin1A BPF remained significant (F1,24 = 7.84; P = .01), and no effect of cluster B personality disorder diagnosis on binding was found (F1,24 = 0.01; P = .93). The degree of intent to attempt suicide or the degree of planning correlates with the lethality of the attempt (29 participants; R2 = 0.617; P < .001). This finding may reflect the lower lethality observed in more impulsive, less planned attempts. Similarly, considering lifetime aggression severity as measured by the Brown-Goodwin Lifetime History of Aggression Scale as a predictor in the model, the effect of lethality remained significant (F1,24 = 7.29; P = .01), and no effect of aggression history was observed (F1,24 = 0.08; P = .78).
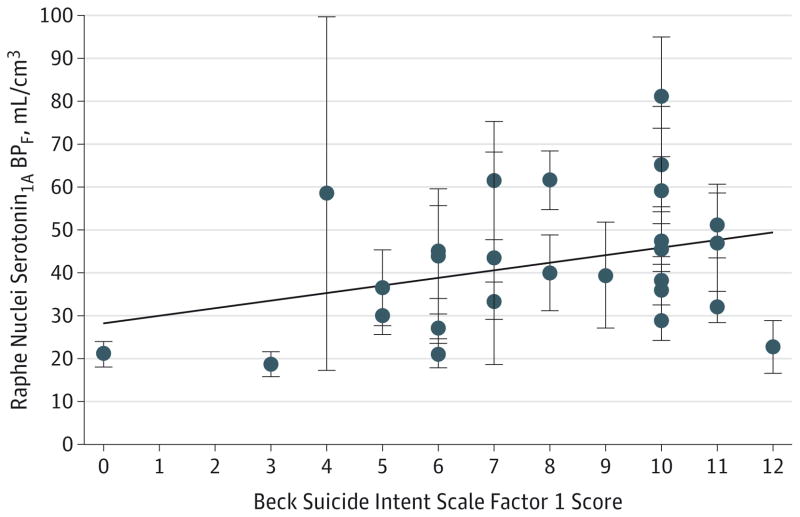
Serotonin1A BPF and Suicide Intent Rating in Attempters
Total Beck Suicide Intent Scale score and the raphe nuclei serotonin1A BPF were positively correlated (F1,25 = 7.89; P < .01), which post hoc analyses showed was accounted for by factor 1 (subjective lethal intent) (F1,25 = 10.63; P = .003; R2 = 0.32) (Figure 2) and not factor 2 (objective planning) (F1,25 = 2.05; P = .16). No relationship was found between the PFC region serotonin1A BPF and the Beck Suicide Intent Scale score (F1,25 = 0.09; P = .76) or with either factor score.
Figure 2. Bivariate Plot of the Relationship Between Raphe Nuclei Serotonin1A Binding Potential (BPF) and the Beck Suicide Intent Scale Factor 1 Score in Suicide Attempters.
Participants include the 29 suicide attempters with major depressive disorder (MDD). Error bars depict associated SE; diagonal line, best fit; and slope, correlation. Factor 1 indicates lethal intent (scores range from 0 to 12) (F1,25 = 10.63; P = .003; R2 = 0.32). Displayed serotonin1A BPF estimates have been adjusted for sex and prior antidepressant medication status derived from the specific linear mixed-effects model examining the relationship of raphe nuclei serotonin1A BPF with the factor 1 score in all suicide attempters with MDD. For display purposes, 1 lower-lethality attempter with a very high serotonin1A BPF and SE is not included in this plot but was included in all the statistical analyses.
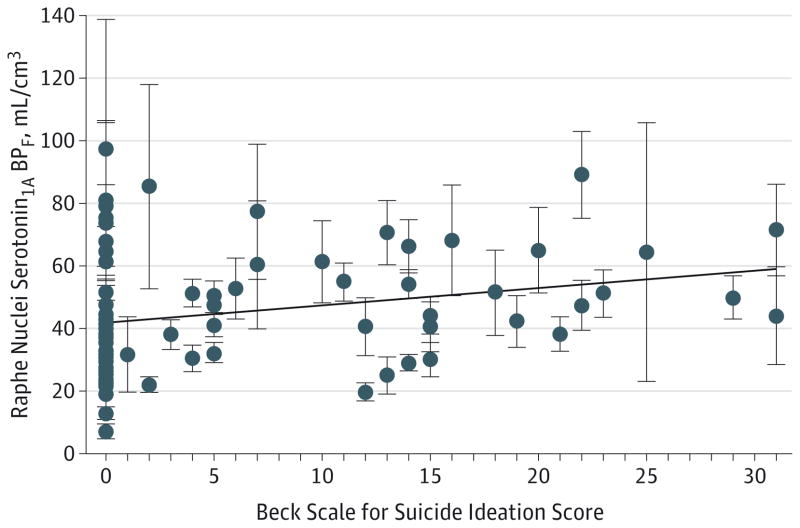
Relationships Among Serotonin1A BPF, Suicide Ideation, and Depression Severity
In the entire MDD group, the Beck Scale for Suicide Ideation score was positively correlated with serotonin1A BPF in PFC regions (F1,88 = 5.19; P = .03), with a significant effect of prior antidepressant status (F1,88 = 7.28; P < .01). The Beck Scale for Suicide Ideation score was also related to serotonin1A BPF in the raphe nuclei (F1,87 = 7.38; P = .008; R2 = 0.12) (Figure 3), but raphe nuclei binding was not significantly related to prior anti-depressant status (F1,87 = 3.86; P = .053). Depression severity, as rated on the 24-item version of the Hamilton Depression Rating Scale,29 was not related to raphe nuclei (F1,87 = 1.65; P = .20) or to PFC (F1,88 = 0.18; P = .67) binding.
Figure 3. Bivariate Plot of the Relationship Between Raphe Nuclei Serotonin1A Binding Potential (BPF) and the Beck Scale for Suicide Ideation Score in All Participants.
Participants include the 91 patients with major depressive disorder (MDD). Error bars depict associated SE; diagonal line, best fit; and slope, correlation. Suicidal ideation scores in the 2 weeks before positron emission tomography range from 0 to 30 (F1,87 = 7.38; P = .008; R2 = 0.12). Displayed serotonin1A BPF estimates have been adjusted for sex and prior antidepressant use derived from the specific linear mixed-effects model examining the relationship of raphe nuclei serotonin1A BPF with the Beck Scale for Suicide Ideation score in all participants with MDD. For display purposes, 1 lower-lethality attempter with a very high serotonin1A BPF and SE is not included in this plot but was included in all the statistical analyses.
Discussion
Consistent with postmortem studies showing higher dorsal raphe nuclei serotonin1A binding in individuals who die by committing suicide19,20 and with our hypothesis, we found that higher-lethality suicide attempters with MDD have higher raphe nuclei serotonin1A BPF compared with lower-lethality attempters with MDD. In contrast, serotonin1A BPF did not differ when all attempters with MDD were compared with all nonattempters with MDD. Within both suicide attempter groups with MDD (higher and lower lethality), lethality of the most recent suicide attempt was positively correlated with raphe nuclei binding; the Beck Suicide Intent Scale score34–36 was also positively correlated with binding. The degree of suicide intent correlated moderately with the lethality of suicide attempts, as has been reported.34,35 Thus, higher serotonin1A binding in vivo in higher-lethality attempters and in postmortem examination of individuals who complete suicide may represent a common biological marker of risk for higher lethality and intent or more serious suicidal behavior. Such a biological commonality between suicide and more lethal suicide attempts is also apparent in the demographic similarities (more men and older individuals) and in the clinical picture of more depression and less impulsiveness. Less lethal suicide attempts are more characteristic of women and younger individuals and are more impulsive.
Somatodendritic serotonin1A autoreceptors in the raphe nuclei inhibit raphe serotonergic neuron firing and thus the frequency of serotonin release from terminals.61,62 Therefore, higher raphe nuclei serotonin1A binding in higher-lethality attempters with MDD may indicate less neuronal firing and less serotonin release at terminal projection regions in the forebrain,63,64 favoring higher-lethality suicide attempts. We also find greater suicide intent correlated with higher raphe nuclei serotonin1A binding, and suicide intent correlates with more lethal suicidal behavior.65–67 This observation is also consistent with prior work in young suicide attempters15 showing that less [11C]methyltryptophan uptake in the medial ventral PFC correlates with greater suicide intent. Higher raphe nuclei serotonin1A autoreceptor binding in higher-lethality attempters would be expected to be associated with less serotonin neuron firing at PFC terminals, which in turn may result in less tryptophan uptake for production of serotonin at these PFC terminals.
Our finding of higher serotonin1A binding in higher-lethality suicide attempters with MDD is consistent with low CSF 5-HIAA levels in higher-lethality attempters with MDD and future suicide completers with MDD and is consistent with a blunted prolactin response to a fenfluramine-stimulated serotonergic challenge in higher-lethality suicide attempters.11,68 These results further indicate that higher raphe nuclei serotonin1A binding may be a marker of more serious suicidal behavior in those at risk for suicide attempts.
Serotonin1A binding is 17% to 30% higher in PFC regions post mortem in individuals who complete suicide compared with those with nonsuicide deaths assayed using the serotonin1A agonist 8-OH-DPAT. Agonists bind to the subset of receptors in the agonist high-affinity state.69 The antagonist radiotracer [11C]WAY-100635 binds to agonist high- and low-affinity states of serotonin1A. Nonhuman primate PET imaging comparing a serotonin1A agonist tracer and [11C]WAY-100635 indicates that only about half of the total binding of [11C]WAY-100635 in the PFC regions is attributable to high–agonist affinity receptors.70 In serotonin1A BPF in the raphe nuclei, we detected more than 45.1% higher binding in higher-lethality attempters, a difference that is comparable to that reported in individuals who complete suicide. Our median split for dividing attempters into higher- and lower-lethality groups was a score between 1 and 2, whereas prior CSF studies had a cut point between 2 and 3.7,11 We had fewer higher-lethality attempters in our study, which limited our power to detect binding differences associated with greater lethality.
Among all 91 participants with MDD, suicidal ideation in the 2 weeks before PET imaging was positively correlated, albeit weakly (R2 = 0.12), with serotonin1A BPF in the raphe nuclei and PFC regions. This finding suggests a more general role for serotonin1A signaling in determining suicidal ideation severity, and severity of suicidal ideation can predict risk for future suicide.71
Cluster B personality disorders are typically associated with more impulsive behaviors.72 The lower-lethality attempter group had about 3 times the rate of cluster B personality disorders (46.2%) compared with the higher-lethality attempter group (16.7%). This difference suggests that the higher raphe nuclei serotonin1A binding in higher-lethality attempters represents a biomarker for suicide attempts that are associated with more intent and with less impulsive traits or fewer personality disorders. Consistent with this model, we find better planned, less impulsive suicide attempts are more lethal. Objective and subjective depression severity and hopelessness were comparable between the higher- and lower-lethality attempter groups, and, as previously reported, serotonin1A binding was not related to depression severity.25,26
In terms of the causes of higher serotonin1A binding that we observed in higher-lethality attempters with MDD, there are a few possibilities. The first is the C(−1019)G genetic variant in the promoter of the serotonin1A gene (HTR1A [HGNC 5286]), where the G allele is associated with greater expression in the brainstem serotonin neurons,73 and higher raphe nuclei autoreceptor binding is seen on PET imaging.26 Second, animal studies of developmental adversity report that maternal deprivation in rodent models can upregulate binding in some brain regions, such as the hippocampus, although not the raphe nuclei autoreceptors.74 In the non-human primate, peer rearing is associated with in vivo serotonin1A binding differences by PET that are sex dependent.75 We did not detect an effect on binding of reported childhood (younger than 15 years) adversity. In fact, we found no effect of abuse at any age. Considering abuse in our model did not alter the significance of the lethality effect on binding. Therefore, we found no evidence that adversity explained the higher raphe nuclei binding or that it contributed to the effect of lethality.
Diminished serotonin activity could be caused by other factors, such as lower tryptophan hydroxylase 2 activity or expression. However, postmortem studies in depressed individuals who complete suicide have found greater tryptophan hydroxylase 2 expression and more serotonin neurons within raphe nuclei76–78; therefore, other mechanisms, such as serotonin1A autoreceptor overexpression, must be responsible for the hyposerotonergic state we observed in our sample of higher-lethality attempters.
This study has some limitations. Although this study has, to our knowledge, the largest sample size for a published PET study of this receptor, the numbers in the MDD attempter subgroups were too small to determine whether higher binding was associated with the G allele or reported childhood adversity. We detected lower serotonin1A binding in participants reporting use of antidepressants within 4 years of PET scanning, in agreement with a previous report.25 All analyses therefore controlled for this factor. Recruiting a sample of antidepressant-naive participants is challenging logistically and is not representative of most clinical populations. The mean age of the attempters with MDD was about 6 years younger than that of the nonattempters with MDD, but previous studies have not identified an effect of age on the binding of [11C]WAY100635 in the age range of this study.25,61
Conclusions
Other serotonin system findings on brain scanning include low brainstem serotonin transporter binding in attempters with MDD compared with nonattempters with MDD and healthy volunteers,79 low serotonin-related lower FDG uptake in the PFC in higher-lethality attempters with MDD,9 and lower [11C]methyltryptophan uptake in ventromedial PFC in higher-intent suicide attempters.15 Taken together with our findings of higher raphe nuclei serotonin1A binding in higher-lethality suicide attempters, these studies indicate key pathologic differences in serotonin system functioning in suicide attempters and particularly those at risk for more lethal and serious forms of suicidal behaviors.
Acknowledgments
Funding/Support: This study was supported by grants MH40695, MH62185, and MH074813 from the US Public Health Service and a grant from the American Foundation for Suicide Prevention.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: Dr Oquendo receives royalties from the Research Foundation for Mental Hygiene (RFMH) for commercial use of the Columbia Suicide Severity Rating Scale (C-SSRS); received financial compensation from Pfizer for the safety evaluation of a clinical facility; and has received unrestricted educational grants and/or lecture fees from AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Janssen, Otsuko, Pfizer, Sanofi, and Shire. Dr Oquendo’s family owns stock in Bristol-Myers Squibb. Dr Miller has received financial compensation for psychiatric evaluations of participants enrolled in medication studies sponsored by Pfizer and Orexigen Therapeutics. Dr Miller’s family owns stock in Johnson & Johnson. Drs Burke and Mann receive royalties from the RFMH for commercial use of the C-SSRS. Dr Mann has stock options from Qualitas Medical. No other disclosures were reported.
Author Contributions: Dr Sullivan had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Sullivan, Oquendo, Parsey, Mann.
Acquisition, analysis, or interpretation of data: Sullivan, Oquendo, Milak, Miller, Burke, Ogden, Mann.
Drafting of the manuscript: Sullivan, Oquendo, Parsey.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Sullivan, Oquendo, Ogden.
Obtained funding: Oquendo, Parsey, Mann.
Administrative, technical, or material support: Oquendo, Miller, Parsey, Mann.
Study supervision: Sullivan, Oquendo, Milak, Burke, Parsey, Mann.
References
- 1.Centers for Disease Control and Prevention. Control NCfIPa. [Accessed October 19, 2012];Web-based Injury Statistics Query and Reporting System (WISQARS) http://www.cdc.gov/injury/wisqars/leading_causes_death.html.
- 2.Mann JJ. A current perspective of suicide and attempted suicide. Ann Intern Med. 2002;136(4):302–311. doi: 10.7326/0003-4819-136-4-200202190-00010. [DOI] [PubMed] [Google Scholar]
- 3.Åsberg M, Träskman L, Thorén P. 5-HIAA in the cerebrospinal fluid: a biochemical suicide predictor? Arch Gen Psychiatry. 1976;33(10):1193–1197. doi: 10.1001/archpsyc.1976.01770100055005. [DOI] [PubMed] [Google Scholar]
- 4.Cooper SJ, Kelly CB, King DJ. 5-Hydroxyindoleacetic acid in cerebrospinal fluid and prediction of suicidal behaviour in schizophrenia. Lancet. 1992;340(8825):940–941. doi: 10.1016/0140-6736(92)92819-2. [DOI] [PubMed] [Google Scholar]
- 5.Mann JJ, Arango V, Marzuk PM, Theccanat S, Reis DJ. Evidence for the 5-HT hypothesis of suicide: a review of post-mortem studies. Br J Psychiatry Suppl. 1989;(8):7–14. [PubMed] [Google Scholar]
- 6.Mann JJ, Currier D, Stanley B, Oquendo MA, Amsel LV, Ellis SP. Can biological tests assist prediction of suicide in mood disorders? Int J Neuropsychopharmacol. 2006;9(4):465–474. doi: 10.1017/S1461145705005687. [DOI] [PubMed] [Google Scholar]
- 7.Mann JJ, Malone KM. Cerebrospinal fluid amines and higher-lethality suicide attempts in depressed inpatients. Biol Psychiatry. 1997;41(2):162–171. doi: 10.1016/s0006-3223(96)00217-x. [DOI] [PubMed] [Google Scholar]
- 8.Nordström P, Samuelsson M, Åsberg M, et al. CSF 5-HIAA predicts suicide risk after attempted suicide. Suicide Life Threat Behav. 1994;24(1):1–9. [PubMed] [Google Scholar]
- 9.Oquendo MA, Placidi GP, Malone KM, et al. Positron emission tomography of regional brain metabolic responses to a serotonergic challenge and lethality of suicide attempts in major depression. Arch Gen Psychiatry. 2003;60(1):14–22. doi: 10.1001/archpsyc.60.1.14. [DOI] [PubMed] [Google Scholar]
- 10.Roy A, De Jong J, Linnoila M. Cerebrospinal fluid monoamine metabolites and suicidal behavior in depressed patients: a 5-year follow-up study. Arch Gen Psychiatry. 1989;46(7):609–612. doi: 10.1001/archpsyc.1989.01810070035005. [DOI] [PubMed] [Google Scholar]
- 11.Malone KM, Corbitt EM, Li S, Mann JJ. Prolactin response to fenfluramine and suicide attempt lethality in major depression. Br J Psychiatry. 1996;168(3):324–329. doi: 10.1192/bjp.168.3.324. [DOI] [PubMed] [Google Scholar]
- 12.Linnoila M, Virkkunen M. Biologic correlates of suicidal risk and aggressive behavioral traits. J Clin Psychopharmacol. 1992;12(2 suppl):19S–20S. [PubMed] [Google Scholar]
- 13.Placidi GP, Oquendo MA, Malone KM, Huang YY, Ellis SP, Mann JJ. Aggressivity, suicide attempts, and depression: relationship to cerebrospinal fluid monoamine metabolite levels. Biol Psychiatry. 2001;50(10):783–791. doi: 10.1016/s0006-3223(01)01170-2. [DOI] [PubMed] [Google Scholar]
- 14.Stanley B, Molcho A, Stanley M, et al. Association of aggressive behavior with altered serotonergic function in patients who are not suicidal. Am J Psychiatry. 2000;157(4):609–614. doi: 10.1176/appi.ajp.157.4.609. [DOI] [PubMed] [Google Scholar]
- 15.Leyton M, Paquette V, Gravel P, et al. a-[11C]Methyl-L-tryptophan trapping in the orbital and ventral medial prefrontal cortex of suicide attempters. Eur Neuropsychopharmacol. 2006;16 (3):220–223. doi: 10.1016/j.euroneuro.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 16.Siever LJ, Buchsbaum MS, New AS, et al. d,l-Fenfluramine response in impulsive personality disorder assessed with [18F]fluorodeoxyglucose positron emission tomography. Neuropsychopharmacology. 1999;20(5):413–423. doi: 10.1016/S0893-133X(98)00111-0. [DOI] [PubMed] [Google Scholar]
- 17.Soloff PH, Meltzer CC, Greer PJ, Constantine D, Kelly TM. A fenfluramine-activated FDG-PET study of borderline personality disorder. Biol Psychiatry. 2000;47(6):540–547. doi: 10.1016/s0006-3223(99)00202-4. [DOI] [PubMed] [Google Scholar]
- 18.Frankle WG, Lombardo I, New AS, et al. Brain serotonin transporter distribution in subjects with impulsive aggressivity: a positron emission study with [11C]McN 5652. Am J Psychiatry. 2005;162(5):915–923. doi: 10.1176/appi.ajp.162.5.915. [DOI] [PubMed] [Google Scholar]
- 19.Stockmeier CA, Shapiro LA, Dilley GE, Kolli TN, Friedman L, Rajkowska G. Increase in serotonin-1A autoreceptors in the midbrain of suicide victims with major depression: postmortem evidence for decreased serotonin activity. J Neurosci. 1998;18 (18):7394–7401. doi: 10.1523/JNEUROSCI.18-18-07394.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boldrini M, Underwood MD, Mann JJ, Arango V. Serotonin-1A autoreceptor binding in the dorsal raphe nucleus of depressed suicides. J Psychiatr Res. 2008;42(6):433–442. doi: 10.1016/j.jpsychires.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arango V, Underwood MD, Gubbi AV, Mann JJ. Localized alterations in pre- and postsynaptic serotonin binding sites in the ventrolateral prefrontal cortex of suicide victims. Brain Res. 1995;688(1–2):121–133. doi: 10.1016/0006-8993(95)00523-s. [DOI] [PubMed] [Google Scholar]
- 22.Lowther S, De Paermentier F, Cheetham SC, Crompton MR, Katona CL, Horton RW. 5-HT1A receptor binding sites in post-mortem brain samples from depressed suicides and controls. J Affect Disord. 1997;42(2–3):199–207. doi: 10.1016/s0165-0327(96)01413-9. [DOI] [PubMed] [Google Scholar]
- 23.Stockmeier CA, Dilley GE, Shapiro LA, Overholser JC, Thompson PA, Meltzer HY. Serotonin receptors in suicide victims with major depression. Neuropsychopharmacology. 1997;16(2):162–173. doi: 10.1016/S0893-133X(96)00170-4. [DOI] [PubMed] [Google Scholar]
- 24.Miller JM, Hesselgrave N, Ogden RT, et al. Brain serotonin 1A receptor binding as a predictor of treatment outcome in major depressive disorder. Biol Psychiatry. 2013;74(10):760–767. doi: 10.1016/j.biopsych.2013.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parsey RV, Ogden RT, Miller JM, et al. Higher serotonin 1A binding in a second major depression cohort: modeling and reference region considerations. Biol Psychiatry. 2010;68(2):170–178. doi: 10.1016/j.biopsych.2010.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parsey RV, Oquendo MA, Ogden RT, et al. Altered serotonin 1A binding in major depression: a [carbonyl-C-11]WAY100635 positron emission tomography study. Biol Psychiatry. 2006;59(2):106–113. doi: 10.1016/j.biopsych.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 27.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-I/P), Version 2.0. New York: Biometrics Research, New York State Psychiatric Institute; 1994. [Google Scholar]
- 28.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 29.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33(6):766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- 31.First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Washington, DC: American Psychiatric Press Inc; 1997. [Google Scholar]
- 32.Oquendo MA, Halberstam B, Mann JJ. Risk factors for suicidal behavior: the utility and limitations of research instruments. In: First MB, editor. Standardized Evaluation in Clinical Practice. Vol. 22. Washington, DC: American Psychiatric Publishing; 2003. pp. 103–130. [Google Scholar]
- 33.Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164(7):1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beck AT, Beck R, Kovacs M. Classification of suicidal behaviors, I: quantifying intent and medical lethality. Am J Psychiatry. 1975;132(3):285–287. doi: 10.1176/ajp.132.3.285. [DOI] [PubMed] [Google Scholar]
- 35.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 36.Mieczkowski TA, Sweeney JA, Haas GL, Junker BW, Brown RP, Mann JJ. Factor composition of the Suicide Intent Scale. Suicide Life Threat Behav. 1993;23(1):37–45. [PubMed] [Google Scholar]
- 37.Brown GL, Goodwin FK, Ballenger JC, Goyer PF, Major LF. Aggression in humans correlates with cerebrospinal fluid amine metabolites. Psychiatry Res. 1979;1(2):131–139. doi: 10.1016/0165-1781(79)90053-2. [DOI] [PubMed] [Google Scholar]
- 38.Parsey RV, Arango V, Olvet DM, Oquendo MA, Van Heertum RL, John Mann J. Regional heterogeneity of 5-HT1A receptors in human cerebellum as assessed by positron emission tomography. J Cereb Blood Flow Metab. 2005;25 (7):785–793. doi: 10.1038/sj.jcbfm.9600072. [DOI] [PubMed] [Google Scholar]
- 39.Parsey RV, Slifstein M, Hwang DR, et al. Validation and reproducibility of measurement of 5-HT1A receptor parameters with [carbonyl-11C]WAY-100635 in humans: comparison of arterial and reference tissue input functions. J Cereb Blood Flow Metab. 2000;20(7):1111–1133. doi: 10.1097/00004647-200007000-00011. [DOI] [PubMed] [Google Scholar]
- 40.Jenkinson M, Smith S. A global optimisation method for robust affine registration of brain images. Med Image Anal. 2001;5(2):143–156. doi: 10.1016/s1361-8415(01)00036-6. [DOI] [PubMed] [Google Scholar]
- 41.Smith SM. Fast robust automated brain extraction. Hum Brain Mapp. 2002;17(3):143–155. doi: 10.1002/hbm.10062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ashburner J, Friston KJ. Nonlinear spatial normalization using basis functions. Hum Brain Mapp. 1999;7(4):254–266. doi: 10.1002/(SICI)1097-0193(1999)7:4<254::AID-HBM4>3.0.CO;2-G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ashburner J, Friston KJ. Unified segmentation. Neuroimage. 2005;26(3):839–851. doi: 10.1016/j.neuroimage.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 44.Duvernoy HM. The Human Brain: Surface, Three-Dimensional Sectional Anatomy and MRI. Wien, Austria: Springer-Verlag; 1991. [Google Scholar]
- 45.Talairach J, Tournoux P. Co-planar Stereotaxic Atlas of the Human Brain: 3-Dimensional Proportional System: An Approach to Cerebral Imaging. Stuttgart, Germany: Thieme; 1988. [Google Scholar]
- 46.Kates WR, Abrams MT, Kaufmann WE, Breiter SN, Reiss AL. Reliability and validity of MRI measurement of the amygdala and hippocampus in children with fragile X syndrome. Psychiatry Res. 1997;75(1):31–48. doi: 10.1016/s0925-4927(97)00019-x. [DOI] [PubMed] [Google Scholar]
- 47.Killiany RJ, Moss MB, Nicholson T, Jolesz F, Sandor T. An interactive procedure for extracting features of the brain from magnetic resonance images: the lobes. Hum Brain Mapp. 1997;5(5):355–363. doi: 10.1002/(SICI)1097-0193(1997)5:5<355::AID-HBM4>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 48.Innis RB, Cunningham VJ, Delforge J, et al. Consensus nomenclature for in vivo imaging of reversibly binding radioligands. J Cereb Blood Flow Metab. 2007;27(9):1533–1539. doi: 10.1038/sj.jcbfm.9600493. [DOI] [PubMed] [Google Scholar]
- 49.Parsey RV, Hastings RS, Oquendo MA, et al. Effect of a triallelic functional polymorphism of the serotonin-transporter–linked promoter region on expression of serotonin transporter in the human brain. Am J Psychiatry. 2006;163(1):48–51. doi: 10.1176/appi.ajp.163.1.48. [DOI] [PubMed] [Google Scholar]
- 50.Hirvonen J, Karlsson H, Kajander J, et al. Decreased brain serotonin 5-HT1A receptor availability in medication-naive patients with major depressive disorder: an in-vivo imaging study using PET and [carbonyl-11C]WAY-100635. Int J Neuropsychopharmacol. 2008;11(4):465–476. doi: 10.1017/S1461145707008140. [DOI] [PubMed] [Google Scholar]
- 51.Oquendo MA, Hastings RS, Huang YY, et al. Brain serotonin transporter binding in depressed patients with bipolar disorder using positron emission tomography. Arch Gen Psychiatry. 2007;64(2):201–208. doi: 10.1001/archpsyc.64.2.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Parsey RV, Hastings RS, Oquendo MA, et al. Lower serotonin transporter binding potential in the human brain during major depressive episodes. Am J Psychiatry. 2006;163(1):52–58. doi: 10.1176/appi.ajp.163.1.52. [DOI] [PubMed] [Google Scholar]
- 53.Parsey RV, Olvet DM, Oquendo MA, Huang YY, Ogden RT, Mann JJ. Higher 5-HT1A receptor binding potential during a major depressive episode predicts poor treatment response: preliminary data from a naturalistic study. Neuropsychopharmacology. 2006;31(8):1745–1749. doi: 10.1038/sj.npp.1300992. [DOI] [PubMed] [Google Scholar]
- 54.Sullivan GM, Oquendo MA, Simpson N, Van Heertum RL, Mann JJ, Parsey RV. Brain serotonin1A receptor binding in major depression is related to psychic and somatic anxiety. Biol Psychiatry. 2005;58(12):947–954. doi: 10.1016/j.biopsych.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 55.Miller JM, Brennan KG, Ogden TR, et al. Elevated serotonin 1A binding in remitted major depressive disorder: evidence for a trait biological abnormality. Neuropsychopharmacology. 2009;34 (10):2275–2284. doi: 10.1038/npp.2009.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Miller JM, Kinnally EL, Ogden RT, Oquendo MA, Mann JJ, Parsey RV. Reported childhood abuse is associated with low serotonin transporter binding in vivo in major depressive disorder. Synapse. 2009;63(7):565–573. doi: 10.1002/syn.20637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rabiner EA, Wilkins MR, Turkheimer F, et al. 5-Hydroxytryptamine1A receptor occupancy by novel full antagonist 2-[4-[4-(7-chloro-2,3-dihydro-1, 4-benzdioxyn-5-yl)-1-piperazinyl]butyl]-1,2-benzisothiazol-3-(2H)-one-1,1-dioxide: a[11C][O-methyl-3H]-N-(2-(4-(2-methoxyphenyl)-1-piperazinyl)ethyl)-N-(2-pyridinyl)cyclohexanecarboxamide trihydrochloride (WAY-100635) positron emission tomography study in humans. J Pharmacol Exp Ther. 2002;301(3):1144–1150. doi: 10.1124/jpet.301.3.1144. [DOI] [PubMed] [Google Scholar]
- 58.Meltzer CC, Price JC, Mathis CA, et al. Serotonin 1A receptor binding and treatment response in late-life depression. Neuropsychopharmacology. 2004;29(12):2258–2265. doi: 10.1038/sj.npp.1300556. [DOI] [PubMed] [Google Scholar]
- 59.Ogden RT, Tarpey T. Estimation in regression models with externally estimated parameters. Biostatistics. 2006;7(1):115–129. doi: 10.1093/biostatistics/kxi044. [DOI] [PubMed] [Google Scholar]
- 60.Parsey RV, Oquendo MA, Simpson NR, et al. Effects of sex, age, and aggressive traits in man on brain serotonin 5-HT1A receptor binding potential measured by PET using [C-11]WAY-100635. Brain Res. 2002;954(2):173–182. doi: 10.1016/s0006-8993(02)03243-2. [DOI] [PubMed] [Google Scholar]
- 61.Kelly JS, Larkman P, Penington NJ, Rainnie DG, McAllister-Williams H, Hodgkiss J. Serotonin receptor heterogeneity and the role of potassium channels in neuronal excitability. Adv Exp Med Biol. 1991;287:177–191. doi: 10.1007/978-1-4684-5907-4_15. [DOI] [PubMed] [Google Scholar]
- 62.McAllister-Williams RH, Kelly JS. The modulation of calcium channel currents recorded from adult rat dorsal raphe neurones by 5-HT1A receptor or direct G-protein activation. Neuropharmacology. 1995;34(11):1491–1506. doi: 10.1016/0028-3908(95)00131-o. [DOI] [PubMed] [Google Scholar]
- 63.Hjorth S, Sharp T. Effect of the 5-HT1A receptor agonist 8-OH-DPAT on the release of 5-HT in dorsal and median raphe-innervated rat brain regions as measured by in vivo microdialysis. Life Sci. 1991;48 (18):1779–1786. doi: 10.1016/0024-3205(91)90216-x. [DOI] [PubMed] [Google Scholar]
- 64.Jacobsen JP, Siesser WB, Sachs BD, et al. Deficient serotonin neurotransmission and depression-like serotonin biomarker alterations in tryptophan hydroxylase 2 (Tph2) loss-of-function mice. Mol Psychiatry. 2012;17(7):694–704. doi: 10.1038/mp.2011.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Horesh N, Levi Y, Apter A. Medically serious versus non-serious suicide attempts: relationships of lethality and intent to clinical and interpersonal characteristics. J Affect Disord. 2012;136(3):286–293. doi: 10.1016/j.jad.2011.11.035. [DOI] [PubMed] [Google Scholar]
- 66.Kumar CT, Mohan R, Ranjith G, Chandrasekaran R. Characteristics of high intent suicide attempters admitted to a general hospital. J Affect Disord. 2006;91(1):77–81. doi: 10.1016/j.jad.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 67.Zhang J, Xu H. Degree of suicide intent and the lethality of means employed: a study of Chinese attempters. Arch Suicide Res. 2007;11(4):343–350. doi: 10.1080/13811110701541889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mann JJ, McBride PA, Brown RP, et al. Relationship between central and peripheral serotonin indexes in depressed and suicidal psychiatric inpatients. Arch Gen Psychiatry. 1992;49 (6):442–446. doi: 10.1001/archpsyc.1992.01820060022003. [DOI] [PubMed] [Google Scholar]
- 69.Hamon M, Bourgoin S, Gozlan H, et al. Biochemical evidence for the 5-HT agonist properties of PAT (8-hydroxy-2-(di-n-propylamino) tetralin) in the rat brain. Eur J Pharmacol. 1984;100(3–4):263–276. doi: 10.1016/0014-2999(84)90002-5. [DOI] [PubMed] [Google Scholar]
- 70.Kumar JS, Milak MS, Majo VJ, et al. Comparison of high and low affinity serotonin 1A receptors by PET in vivo in nonhuman primates. J Pharmacol Sci. 2012;120(3):254–257. doi: 10.1254/jphs.12100sc. [DOI] [PubMed] [Google Scholar]
- 71.Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68(3):371–377. [PubMed] [Google Scholar]
- 72.Fossati A, Barratt ES, Borroni S, Villa D, Grazioli F, Maffei C. Impulsivity, aggressiveness, and DSM-IV personality disorders. Psychiatry Res. 2007;149(1–3):157–167. doi: 10.1016/j.psychres.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 73.Lemonde S, Turecki G, Bakish D, et al. Impaired repression at a 5-hydroxytryptamine 1A receptor gene polymorphism associated with major depression and suicide. J Neurosci. 2003;23(25):8788–8799. doi: 10.1523/JNEUROSCI.23-25-08788.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vázquez DM, López JF, Van Hoers H, Watson SJ, Levine S. Maternal deprivation regulates serotonin 1A and 2A receptors in the infant rat. Brain Res. 2000;855(1):76–82. doi: 10.1016/s0006-8993(99)02307-0. [DOI] [PubMed] [Google Scholar]
- 75.Spinelli S, Chefer S, Carson RE, et al. Effects of early-life stress on serotonin1A receptors in juvenile Rhesus monkeys measured by positron emission tomography. Biol Psychiatry. 2010;67(12):1146–1153. doi: 10.1016/j.biopsych.2009.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bach-Mizrachi H, Underwood MD, Tin A, Ellis SP, Mann JJ, Arango V. Elevated expression of tryptophan hydroxylase-2 mRNA at the neuronal level in the dorsal and median raphe nuclei of depressed suicides. Mol Psychiatry. 2008;13(5):507–513. doi: 10.1038/sj.mp.4002143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Boldrini M, Underwood MD, Mann JJ, Arango V. More tryptophan hydroxylase in the brainstem dorsal raphe nucleus in depressed suicides. Brain Res. 2005;1041(1):19–28. doi: 10.1016/j.brainres.2005.01.083. [DOI] [PubMed] [Google Scholar]
- 78.Underwood MD, Khaibulina AA, Ellis SP, et al. Morphometry of the dorsal raphe nucleus serotonergic neurons in suicide victims. Biol Psychiatry. 1999;46(4):473–483. doi: 10.1016/s0006-3223(99)00043-8. [DOI] [PubMed] [Google Scholar]
- 79.Miller JM, Hesselgrave N, Ogden RT, et al. Positron emission tomography quantification of serotonin transporter in suicide attempters with major depressive disorder. Biol Psychiatry. 2013;74 (4):287–295. doi: 10.1016/j.biopsych.2013.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]