Abstract
Objectives
Substance use disorder (SUD) among women of reproductive age is a complex public health problem affecting a diverse spectrum of women and their families, with potential consequences across generations. The goals of this study were 1) to describe and compare the prevalence of patterns of injury requiring emergency department (ED) visits among SUD-positive and SUD-negative women and 2) among SUD-positive women, to investigate the association of specific categories of injury with type of substance used.
Methods
This study was a secondary analysis of a large, multisource health care utilization data set developed to analyze SUD prevalence, and health and substance abuse treatment outcomes, for women of reproductive age in Massachusetts, 2002 through 2008. Sources for this linked data set included diagnostic codes for ED, inpatient, and outpatient stay discharges; SUD facility treatment records; and vital records for women and for their neonates.
Results
Injury data (ICD-9-CM E-codes) were available for 127,227 SUD-positive women. Almost two-thirds of SUD-positive women had any type of injury, compared to 44.8% of SUD-negative women. The mean (±SD) number of events also differed (2.27 ± 4.1 for SUD-positive women vs. 0.73 ± 1.3 for SUD-negative women, p < 0.0001). For four specific injury types, the proportion injured was almost double for SUD-positive women (49.3% vs 23.4%), and the mean (±SD) number of events was more than double (0.72 ± 0.9 vs. 0.26 ± 0.5, p < 0.0001). The numbers and proportions of motor vehicle incidents and falls were significantly higher in SUD-positive women (22.5% vs. 12.5% and 26.6% vs. 11.0%, respectively), but the greatest differences were in self-inflicted injury (11.5% vs. 0.8%; mean ± SD events = 0.19 ± 0.9 vs. 0.009 ± 0.2, p < 0.0001) and purposefully inflicted injury (11.5% vs 1.9%, mean ± SD events = 0.18 ± 0.1 vs. 0.02 ± 0.2, p < 0.0001). In each of the injury categories that we examined, injury rates among SUD-positive women were lowest for alcohol disorders only and highest for alcohol and drug disorders combined. Among 33,600 women identified as using opioids, 2,132 (6.3%) presented to the ED with overdose. Multiple overdose visits were common (mean ± SD = 3.67 ± 6.70 visits). After adjustment for sociodemographic characteristics, psychiatric history, and complex/chronic illness, SUD remained a significant risk factor for all types of injury, but for the suicide/self-inflicted injury category, psychiatric history was by far the stronger predictor.
Conclusions
The presence of SUD increases the likelihood that women in the 15- to 49-year age group will present to the ED with injury. Conversely, women with injury may be more likely to be involved in alcohol abuse or other substance use. The high rates of injury that we identified among women with SUD suggest the utility of including a brief, validated screen for substance use as part of an ED injury treatment protocol and referring injured women for assessment and/or treatment when scores indicate the likelihood of SUD.
Substance use disorder (SUD), defined as illicit drug abuse, prescription drug misuse and dependence, and alcohol abuse and dependence, is a complex public health problem affecting a diverse spectrum of women and their children from all geographies, races, ethnicities, social classes, communities, and ages, with potential consequences across generations.1–7
Emergency departments (EDs) are both an important venue for providing services to patients with SUD and the site of entry for treatment of many injuries. Among respondents to the National Survey on Drug Use and Health and the National Epidemiologic Survey on Alcohol and Related Conditions, ED patients generally report higher rates of coexisting alcohol and drug use and spend more days using drugs and are more likely to have alcohol or drug use disorders compared with respondents who did not use the ED as a source of health care.8,9 The Drug Abuse Warning Network (DAWN) in 2011 estimated that 1.25 million ED visits were for illicit drugs, and 35% of those patients were identified as women.10
Injury rates are also high. In 2010, among 130 million ED visits for all presenting patients, almost one-third (38 million) were attributed to injury. Women overall represented nearly half of these injury visits,11 and among them, there were 7.4 million injured women aged 15 to 49 years (10% of U.S. women and 19% of ED visits in this age group).12
The data sets from which these estimates are drawn represent probability and weighted samples and do not link data on injury and alcohol and drug abuse. Moreover, most studies of substance use and injury are restricted to specific anatomic regions (e.g., traumatic brain, spinal, or orofacial),13–16 specific causes of injury (e.g., motor vehicle incidents or intimate partner or nonpartner violence),17–20 focus on the age outliers of adolescents or older adults,21,22 or on alcohol only23 or drugs only.24 These studies are limited by small sample sizes, single sites, or restricted numbers of settings and self-report of drug history or, in some cases, limitations of toxicology screening or lack of toxicology screening at the time of injury.24 Although most ED studies have focused on drug and alcohol use prior to injury to determine causal relationships, very few have had the capacity to determine the effect of preexisting SUD on the likelihood of injury presenting to the ED.25 Furthermore, no population-based studies to date have examined the risk of injury for women of reproductive age with SUD.
The goals of this study were 1) to describe and compare the prevalence of patterns of injury requiring ED visits among SUD-positive and SUD-negative women in a multisource, statewide data system, and 2) among SUD-positive women, to investigate the association of specific categories of injury with type of substance used.
METHODS
Study Design
This study was a secondary analysis of a large, multisource health care utilization data set designed to investigate SUD prevalence, and health and substance abuse treatment outcomes for women in Massachusetts. This study was approved by the Boston University Medical Campus, Massachusetts General Hospital Partners, and the Massachusetts Department of Public Health institutional review boards.
Study Setting and Population
We present here results from analysis of ED and inpatient discharge records, maternal delivery hospitalization records, birth certificates, and substance abuse treatment system admissions occurring between 2002 and 2008. This linked data system was used to identify the proportion of women identified with SUD who were subsequently injured during the study period, to compare injury prevalence by SUD identification (yes/no), and to describe injury rate by type of substance used. We examined six categories of injury: 1) total injuries of all types (“all e-coded injury’), 2) motor vehicle crashes (MVCs)/pedestrian injury, 3) falls, 4) suicide/self-inflicted injury, 5) homicide/purposefully inflicted injury, and 6) any of the four specific marker injuries (injury types 2–5).
Data Sources
We used three major data sources to capture documentation of SUD among women of reproductive age in Massachusetts: 1) the Massachusetts Center for Health Information and Analysis (CHIA), which provided International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) diagnostic codes for statewide hospital discharge data, including E-codes, from all inpatient, observational stay, and ED discharges for all women aged 15–49 years, including medical inpatient substance abuse treatment services; 2) the Massachusetts Pregnancy to Early Life Longitudinal (PELL) data system, which provided evidence of SUDs from both maternal and infant records and birth and fetal death records corresponding to hospital delivery discharge records; and 3) the Massachusetts Bureau of Substance Abuse Services (BSAS) treatment data set, which provided information about SUD treatment need and utilization in all publicly funded specialty programs.
Study Sample
The study sample included all women aged 15 to 49 years who received any inpatient, observational stay, ED services or SUD specialty treatment in Massachusetts hospitals or SUD treatment programs at any time from January 1, 2002, to December 31, 2008, and any infants born (live or stillborn) to them between January 1, 2003, and December 31, 2007.
Study Protocol
Data Linkage and Identification of Individual Women From Incident-level Data
A multistep linkage algorithm was developed to identify multiple treatment records belonging to individual women in the CHIA data set. The CHIA episodic-level hospital use data contained 6,347,310 discharge records from 2002 to 2008. All records from women who were aged 15 to 49 years at any point during the study period were included. The individual universal hospital identification number (an encryption of the patient’s social security number), date of birth, and hospital medical record number were used to link and aggregate multiple records belonging to the same woman, for a final sample of 1,748,748 unique women.
SUD Prevalence
The first phase of this investigation focused on the development of a gender-specific algorithm that uses ICD-9-CM codes for women and their neonates, along with vital statistics and substance abuse treatment admission records, to identify probable SUD among women of reproductive age (the Explicit Mention of Substance Abuse Need for Treatment in Women [EMSANT-W] unpublished data, see authors for details). EMSANT-W is built on a methodologically rigorous measure of variation in the rates of substance abuse/dependence and unmet treatment need among the general population, the Substance Need Index. This index was developed by McAuliffe and colleagues26–28 using multiple years of inpatient hospital discharge data mortality data and arrest records.
We specified three criteria for tailoring this algorithm to female gender: 1) the tool would be sensitive enough to capture discharge diagnoses strongly suggestive of an SUD in need of further assessment, 2) the tool would be specific enough to distinguish SUD from background mental health conditions, and 3) the tool would be tailored to women of reproductive age using indirect sources of information about substance use that are not usually included in gender-neutral grouping algorithms. Women were therefore classified as affected by SUD based on 1) specific ICD-9-CM codes for women or their neonates (ED, observational stay, and hospital discharge records), 2) birth certificate mention of a positive neonatal toxicology screen, or 3) a BSAS treatment system record (fuller details available on request). Women who appeared in the hospital data set for reasons unrelated to SUDs, who had no other evidence of SUD, were classified as “non-SUD.”
Substance Type
Use of specific substances was aggregated from several potential sources: 1) discharge ICD-9-CM codes from hospital admissions, ED visits, observation stays, and newborn hospital admissions; 2) the substance type data entry field from the BSAS admissions data set; and 3) the substance type data field from birth and fetal death records. For example, opiates were defined by codes 96500, 96501, 96502, 96509, 9701x, E8500, E8501, E8502, E9350, and E9800. Codes 3041x, 3054x, 9670x, 9671x, 9672x, 9673x, 9674x, 9675x, 9676x, 9678x, 9679x, 9682x, 9683x, E851x, E852x, E8551, and E9801 were grouped as “sedatives, barbiturates, hypnotics, anesthetics.” The cannabis category included 3043x, 3052x, and E8541. Alcohol abuse or dependence was defined by the 303 (dependence), 305 (abuse), and 291 (alcohol induced disorders) code series, with the exception of code 303.3 (in remission), which was excluded.
Injury Prevalence
The “all E-coded injury” category was based on any listing of ICD-9-CM codes E800 to E969 in conjunction with an ED visit following after the first identification of SUD in the data set, for SUD-positive women, and from the first injury-related ED visit for SUD-negative women. Hospital admissions and discharges for injury were not included in these counts, and we set a 72-hour interval between codes for the second ED visit to be eligible for counting as a separate injury.
We specified four types of injury as specific markers for the events most commonly associated with substance use: 1) MVCs and pedestrian injury (codes E810 to E825), 2) falls (codes E880 to E899), 3) suicide/self-inflicted injury (codes E951 to E959), and 4) homicide/purposefully inflicted injury (codes E960 to 969). We also further combined data for these four injury types to create an “any specific marker injury” variable for evidence of any one of these marker injuries. Because poisoning codes encompass drug overdose, we chose to include poisonings in criteria for identification of SUD and thus exclude them from the injury variables.
Independent Predictors
Standard categories for race (African American, Asian/Pacific Islander, white, and other), ethnicity (Hispanic vs. non-Hispanic), age, and insurance type were obtained from hospital discharge data (CHIA) and treatment system (BSAS) discharge data at first admission. Insurance status was characterized as public versus private. The complex/chronic illness variable was derived from CHIA data using the schema developed by Mertens et al.29 for tracking alcohol- and drug-related conditions and tested using matched controls in a Kaiser Health Maintenance Organization system database. The psychiatric history variable included codes for mood disorders, psychoses, paranoid and anxiety states, personality disorders, adjustment disorders, posttraumatic stress disorder, and stress reactions. It excluded codes from either end of the age spectrum (developmental disorders at one end and delirium, dementia, and organic brain disease at the other), drug-related conditions (alcohol abuse and dependence, drug abuse and dependence, because these codes were included in the definition of SUD), and unspecified disorders. Similarly, codes for suicide gesture, attempt, or suicidal ideation were not included in the psychiatric history variable because they were measured within the definition of the suicide/self-inflicted injury outcome variable.
Data Analysis
We initially conducted descriptive analyses to 1) estimate the prevalence of SUD among women of reproductive age in Massachusetts, across categories of race/ethnicity, age, and insurance status; 2) establish the prevalence of injury among SUD-affected and non–SUD-affected women; and 3) describe injury rates by types of drugs used by women positive for SUD. In unadjusted descriptive analyses, we computed means, standard deviations (SDs), 95% confidence intervals (CIs), medians, and interquartile ranges (IQRs). In adjusted descriptive analyses, we computed means, SDs, and 95% CIs. Chi-square tests of significance were performed to identify differences by SUD identification and by type of drug used. For normally distributed continuous variables, t-test statistics were used to identify differences by SUD status, and Wilcoxon rank-sum testing was used for nonparametric distributions.
We planned a retrospective cohort study with 82,811 SUD-positive women (exposed subjects) and 799,141 SUD-negative women (unexposed subjects), representing the total number of women in the final data set who had evidence for an ED visit. We estimated the probability of injury exposure among unexposed women was 0.4. With a true probability of injury exposure among exposed women of 0.6, we had statistical power of 100% at a two-sided alpha of 0.05 in the analysis sample of over 800,000. Moreover, when comparing exposed and unexposed women in terms of an incident rate ratio (IRR), the study sample size supports IRRs computed in a Poisson model less than 0.10 with 100% power at a two-sided alpha of 0.05. We performed these power computations using nQuery Advisor version 7 and GPower version 3.1.
We performed both unadjusted and adjusted analyses to estimate the association of a documented SUD diagnosis with the frequency of injury during the study period. Poisson regression was used to estimate the IRR of specific types of injury associated with SUD (model 1, adjusted only for time). Our Poisson models incorporated a scaled deviance adjustment for the standard errors of the model coefficients.
For SUD-negative women, we counted the number of months from the first appearance of an injury-related code until the last clinical encounter in the data set. For SUD-positive women, we counted the number of months from the first injury-related episode after appearance of an SUD indicator to the last clinical encounter. Adjusting for time in model 1 prevented confounding from potentially unequal number of injury-possible months (exposure) between groups.
Model 2 additionally controlled for covariates of women’s race, Hispanic ethnicity, private insurance, region of residence in Massachusetts, history of psychiatric illness, and complex/chronic illness along with time. White race, non-Hispanic ethnicity, and absence of psychiatric history or complex/chronic illness served as the reference groups. Data were analyzed using SAS 9.2.
RESULTS
Prevalence of SUDs Among Women of Reproductive Age
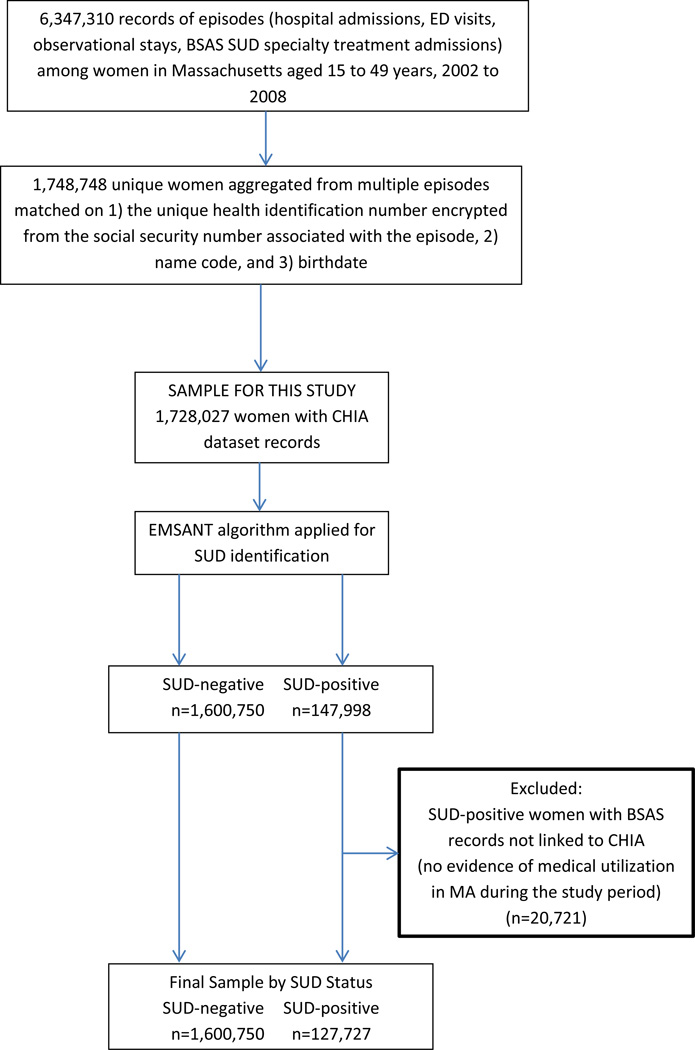
Altogether, 1,748,748 individual women who received medical or SUD treatment services in Massachusetts were identified in the linkage of CHIA, PELL, and BSAS data sources spanning 2002 to 2008. Among them, 8.5% (n = 147,998) were SUD-positive based on ICD-9-CM codes for themselves and their neonates, BSAS admissions for SUD treatment, and birth and death certificate data, while 1,600,750 women had no indication of SUD. ED, observational stay, and hospital discharge records were available for 127,227 women who were SUD-positive. An additional 20,771 SUD-positive women had records solely in the SUD treatment system with no linkage to hospital discharge data and were excluded from the sample for this investigation because no injury information was available (no use of ED services, observational stays, or hospital admissions during the study period). The sample for this investigation thus consists of the 1,728,027 women who were identified in CHIA data (see Figure 1).
Figure 1.
Strobe diagram: sample selection. BSAS = Bureau of Substance Abuse Services; CHIA = Center for Health Information and Analysis; EMSANT = Explicit Mention of Substance Abuse Need for Treatment; SUD = substance use disorder.
Comparison of Injury Incidence by SUD Status (Table 1)
Table 1.
Prevalence and Incidence of Injury in Massachusetts Women of Reproductive Age, 2002–2008 by SUD, Among 4,839,706 ED visits
| Number (%) of Women With E-code Indicating Injury |
Mean (±SD) Number of Injuries (95% CI) |
|||
|---|---|---|---|---|
| Variable | SUD-positive | SUD-negative | SUD-positive | SUD-negative |
| All E-coded injury (n = 800,763) | 82,811 (65.1) | 717,952 (44.8) | 2.27 (4.1) (2.25–2.29) |
0.73 (1.3) (0.73–0.73) |
| Any of the four specified marker injuries (n = 437,501) | 62,691 (49.3) | 374,810 (23.4) | 0.72 (0.9) (0.72–0.73) |
0.26 (0.5) (0.26–0.26) |
| Motor vehicle injuries (n = 228,721) | 28,650 (22.5) | 200,071 (12.5) | 0.34 (0.8) (0.34–0.35) |
0.15 (0.5) (0.15–0.15) |
| Falls (n = 209,924) | 33,855 (26.6) | 176,069 (11.0) | 0.52 (1.5) (0.51–0.53) |
0.13 (0.1) (0.13–0.14) |
| Suicide/self-inflicted injury (n = 27,690) | 14,645 (11.5) | 13,045 (0.8) | 0.19 (0.9) (0.18–0.19) |
0.01 (0.2) (0.01–0.01) |
| Homicide/purposeful injury (n = 45,522) | 14,636 (11.5) | 30,886 (1.9) | 0.18 (0.7) (0.17–0.18) |
0.02 (0.2) (0.02–0.02) |
SUD = substance use disorder.
Among these 1,728,027 women, the proportion of records that were injury-related differed by SUD identification. In the “any E-coded injury” category, 65.1% of SUD-positive women had injuries compared to 44.8% of women who were SUD-negative. On average, women with SUD had more events than SUD-negative women (mean ± SD = 2.27 ± 4.1 for SUD-positive women vs. 0.73 ± 1.3 for SUD-negative women, p < 0.0001). In the “any specific marker injury” category, the proportion injured was more than double for SUD-positive women (49.3% vs. 23.4%), and the mean number of events was more than double (mean ± SD = 0.72 ± 0.9 vs. 0.26 ± 0.50, p < 0.0001). The proportions of women injured in motor vehicle incidents and falls were significantly higher in SUD-positive women versus SUD-negative women (22.5% vs. 12.5% and 26.6% vs. 11.0%, respectively), but the greatest differences were observed in suicide/self-inflicted injury (11.5% vs. 0.8%; mean ± SD = 0.19 ± 0.9 events, p < 0.0001) and homicide/purposefully inflicted injury (11.5% vs 1.9%; mean ± SD = 0.18 ± 0.7 events vs. 0.02 ± 0.2 events, p < 0.0001).
Variations in Injury Incidence by Type of Drug Identified (Table 2)
Table 2.
Prevalence of Injuries among Massachusetts Women of Reproductive Age, 2002–2008, by Type of Drug Use, Among 4,839,706 ED Visits, n = 1,728,027
| Injuries Among SUD-positive Women with Known Type of Substance Use |
n | Number (%) of Women with E- code Indicating Injury |
Mean Number of Events (95% CI) |
|---|---|---|---|
| Any E-coded injury | |||
| By substance category | |||
| Alcohol only | 40,786 | 21,925 (53.7) | 1.3 (1.25–1.30) |
| Drugs only | 39,653 | 26,992 (68.0) | 2.5 (2.46–2.55) |
| Alcohol and drugs | 44,319 | 32,272 (72.8) | 4.0 (2.95–3.04) |
| By use of specific drugs | |||
| Marijuana | 25,036 | 16,713 (66.7) | 2.4 (2.38–2.48) |
| Cocaine | 30,207 | 21,770 (72.0) | 3.0 (2.99–3.10) |
| Opioids | 33,600 | 24,400 (72.6) | 3.3 (3.24–3.36) |
| Other drugs | 55,173 | 41,671 (75.5) | 3.0 (3.26–3.35) |
| Specified marker injury | 437,501 | ||
| Alcohol only | 40,786 | 16,107 (39.5) | 0.50 (0.50–0.51) |
| Drugs only | 39,653 | 19,739 (49.8) | 0.72 (0.72–0.73) |
| Alcohol and drugs | 44,319 | 25,917 (58.5) | 0.92 (0.92–0.94) |
| Motor vehicle injuries | 228,721 | ||
| Alcohol only | 40,786 | 7,048 (17.3) | 0.23 (0.23–0.24) |
| Drugs only | 39,653 | 9,772 (24.6) | 0.39 (0.38–0.40) |
| Alcohol and drugs | 44,319 | 11,354 (25.6) | 0.40 (0.40–0.41) |
| Falls | 209,924 | ||
| Alcohol only | 40,786 | 8,661 (21.2) | 0.31 (0.31–0.32) |
| Drugs only | 39,653 | 10,490 (26.5) | 0.55 (0.53–0.57) |
| Alcohol and drugs | 44,319 | 14,209 (32.1) | 0.68 (0.67–0.70) |
| Suicide/self-inflicted injury | 27,690 | ||
| Alcohol only | 40,786 | 1,927 (4.7) | *0.06 (0.06–0.06) |
| Drugs only | 39,653 | 4,222 (10.7) | 0.16 (0.16–0.17) |
| Alcohol and drugs | 44,319 | 8,402 (19.0) | 0.50 (0.33–0.35) |
| Homicide/purposeful injury | 45,522 | ||
| Alcohol only | 40,786 | 2,979 (7.3) | *0.09 (0.09–0.10) |
| Drugs only | 39,653 | 4,276 (10.8) | *0.15 (0.15–0.16) |
| Alcohol and drugs | 44,319 | 7,219 (16.3) | *0.27 (0.27–0.28) |
CIs are narrow because the sample is large and estimates are precise.
SUD = substance use disorder.
Point estimates for several variables differ but appear similar because of rounding.
In each injury category, injury rates among SUD-positive women were lowest for alcohol disorders only, higher for drug disorders only, and highest for alcohol and drug disorders combined. Marijuana use disorder was the least likely to be associated with injury (mean ± SD = 2.4 ± 4.1 events) and opioids the most likely (mean ± SD = 3.3 ± 5.6 events). The range in injury prevalence among types of drugs was narrow (66.7% to 75.5%), but differences were statistically significant (p < 0.0001).
Opioid Overdose
During the study period, there were 7,824 ED visits for opioid overdoses. Among 33,600 women who were identified as using opioids, 2,132 (6.3%) presented to the ED with overdoses. Multiple overdose visits were common; the mean (±SD)number of visits among those with an ED visit for overdose was 3.67 (±6.70) visits per woman during the study period.
Contribution of SUD to the Likelihood of Injury
Time in Months of Potential Injury
SUD-positive women had a mean (±SD) of 28.7 (±27.4) months in the CHIA data set and a median of 41.0 months (IQR = 5.6 to 65.2 months), compared to a mean (±SD) of 19.0 (±24.4) months and a median of 2 months (IQR = 0.3 to 36.5 months) for women with no SUD (p < 0.0001).
Model 1, Adjusted Only for Differences in Time (Table 3)
Table 3.
Model 1—The Association of SUD With Categories of Injury, Adjusting for the Number of Injury-possible Months in the Data System (Time): IRRs
| Outcome | IRR | 95% CI |
|---|---|---|
| Any E-coded injury | 0.96 | 0.95–0.96 |
| MVC | 1.19 | 1.17–1.20 |
| Falls | 1.59 | 1.57–1.61 |
| Suicide/self-inflicted injury | 9.30 | 9.08–9.52 |
| Homicide/purposefully inflicted injury | 3.93 | 3.85–4.00 |
| Any of the specific marker injuries | 1.39 | 1.37–1.40 |
MVC = motor vehicle crash; IRR = incident rate ratio; SUD = substance use disorder
Women identified with SUD at any time in the study period were slightly less likely to experience any type of injury (yes/no) than non-SUD women, but more likely to have any one of the four specific marker injuries. The risk of suicide/self-inflicted injury was highest, at nine times the rate for women with indication of SUD, followed by a threefold risk for homicide/injury inflicted by others. The risk of falls was also greater among SUD-positive women. The risk of MVCs and pedestrian injuries was the lowest of the four, but still elevated among women with SUD.
Model 2, Adjusted for Time of Exposure, Demographic, and Health Care Variables (Table 4)
Table 4.
Model 2—The Association of SUD With Categories of Injury, Adjusted for Time, Demographic Factors, and Psychiatric and Medical History* With IRRs
| Outcome | Variable | IRR | 95% CI |
|---|---|---|---|
| Any E-coded injury | SUD | 1.22 | 1.21–1.23 |
| MVC | SUD | 1.50 | 1.48–1.52 |
| Falls | SUD | 1.69 | 1.67–1.71 |
| Suicide/self-inflicted injury | SUD | 3.90 | 3.80–4.00 |
| Homicide/purposefully inflicted injury | SUD | 3.30 | 3.23–3.38 |
| Any of the specific marker injuries | SUD | 1.59 | 1.58–1.61 |
IRR = incident rate ratio; MVC = motor vehicle crash; SUD = substance use disorder.
Adjusted for number of injury possible months, age, race, health insurance status, psychiatric history, and chronic/complex medical conditions.
Substance use disorder remained a significant risk factor for all E-coded injuries after adjusting for demographic factors, type of insurance, and psychiatric and medical history, as well as number of months of exposure (details in Data Supplement S1, available as supporting information in the online version of this paper). For MVC/pedestrian injury, the IRR increased after adjustment. The relative risk for falls also increased slightly. In both of these cases, SUD identification was the strongest of the predictors included in the analysis. For suicide/self-inflicted injury, the IRR was substantial, but a non–suicide-related psychiatric history was by far the stronger predictor. SUD identification remained the strongest predictor of homicide after adjustment, but public insurance and psychiatric history were still important factors. SUD was also the strongest predictor of both “any e-coded injury” and “any of the specific-marker injuries” after adjustment.
DISCUSSION
Substance use disorder is a very important contributor to injury among women of childbearing age. Massachusetts women aged 15 to 49 years with indicators for SUD had twice the proportion of injured women and more than double the mean number of ED injury visits in the “any specified marker injury” category, compared to women with no evidence for SUD. Differences were greater for self and purposefully inflicted injuries compared to MVC- and fall-related injuries. This finding was not unexpected, because impairments in perception, cognition, and psychosocial functioning associated with SUD are also likely to predispose to increased likelihood of these four injury types. Injury rates among SUD-positive women varied by patterns of alcohol and drug use and were lowest for alcohol only and highest for alcohol in combination with other drugs, a finding that may be surprising to emergency physicians, who have been exposed more broadly to risks associated with alcohol than those associated with other substances of abuse.
Among drug types identified in the study, marijuana had the lowest association with injury and opioids had the highest. After adjustment for the number of months of exposure, demographic characteristics, prior psychiatric history, and chronic disease status, SUD continued to be a substantial risk factor for injury. SUD-positive women had an elevated risk of MVC/pedestrian and falls injuries compared to SUD-negative women, but the risk for suicide/self-inflicted injury and homicide/purposefully inflicted injury was more than double the risk for MVC/pedestrian and fall-related injuries. For suicide/self-inflicted injuries, however, a psychiatric history was a stronger predictor of risk than SUD. These findings, while not unexpected, underscore the importance of identifying drug and alcohol disorders as predictors of injury.
We did not find differences in our data for the “any E-coded injury category” in model 1, which adjusted only for time. However, the increase in prevalence for all E-coded injury among women with SUD was again demonstrated in model 2, which adjusted for major known demographic and psychosocial predictors of injury. This finding suggests that unadjusted analyses of injury prevalence in particular population subgroups may not be sufficiently nuanced to produce results that can be used for program and policy development. If we had not run an adjusted model for all E-coded injury, we would not have appreciated a small but significant difference between SUD-positive and SUD-negative women.
This statewide population-based study represents a novel opportunity to look broadly at the association of SUD with key types of injury among women of reproductive age. There are a number of studies that examine alcohol and drug use related to motor vehicle trauma, falls, and violence, but these studies are limited by small samples, self-report data, or weighted samples. Studies of injury do not generally have comprehensive information available about SUDs or the methodologies to differentiate SUD effects from medical care episode data, and studies of women with SUD often lack good information about injury.24 Studies focused on individuals in substance abuse treatment programs may also have problems with generalizability.25 Single-focus studies (violence-related injury, intentional injury, anatomic region-specific injury, or trauma setting studies, for example)13–20,25,30–32 may be biased by sample selection and circumstances of injury. Broad studies of injury often lack specificity by gender and age. There is much information, for example, about falls in adolescents33 and in older adults,21,34 but very little about the combined effects of age, sex, SUD, and injury for women in the reproductive age group. National plans to drop the DAWN reporting mechanism for substance abuse and include SUD in the National Ambulatory Medical Care/Emergency Department Survey may provide a more robust data source in the future for measuring the association of SUD with injury on the national level.
In our multisource Massachusetts-wide study, we were able to distinguish a group of women with likely SUD diagnoses, based on ICD-9-CM coding, and use that categorization to describe differences in injury risk based on alcohol and drug use disorders. In any population perspective, there is a trade-off; with our method, we do not approach the detail and depth possible in a small sample or more focused study based on interviews or primary data, nor can we say anything from these data about causality or motivation, determinants of behavior, or mediating factors. On the other hand, this type of secondary analysis attempts to include every woman who sought care in a Massachusetts hospital (ED visits, outpatient stays, and inpatient admissions), and these data are not limited by selective sampling of records or insurance company data sets, or selection bias in subject recruitment. The Massachusetts requirement that all injuries be recorded using the E-code system provided an opportunity to measure injury more completely.
The findings we report here for women aged 15 to 49 years are important for what they tell us about an age group that receives much attention for its reproductive health needs, but less attention than younger girls or older women receive for injury and associated sequelae.35 Yet an injury to a woman in her middle years can have many concentric circles of impact beyond her immediate diagnostic condition, since this is typically the time of life that society relies on women to manage household and job and care for both children and elders.36 Both incapacity due to injury and unaddressed SUD that may be a factor in that injury can contribute significantly to a large social cost. Falls among women in this age group, for example, involve 1.4 million ED visits and carry a mean cost of $771 for the visit at a total societal cost of $1.1 billion. Work loss expenses account for an additional $4.2 billion, and the extra expense of paying substitutes for caregiving responsibilities after falls means the total cost of this type of injury is even greater.12 Efforts to identify and address the drug and alcohol use that increases the risk of falls among adult women could make a significant contribution to reducing health care costs.
LIMITATIONS
Potential sources for sampling bias include missing data, miscoding errors, miscategorization of substance use or injury type, and restriction of the sample to women who used hospital-based services or substance abuse services. This multisource data set is the largest resource for analysis of women with identified SUD, but several groups of women may have been undercounted: 1) women who did not seek any health care from EDs, hospitals, or Massachusetts substance abuse treatment facilities that accept some publically funded clients; 2) women who had health care encounters in Massachusetts, but SUD was missed; and 3) women who received medical care in Massachusetts but went outside the state to seek substance abuse services or were treated within Massachusetts in private facilities that did not contract with BSAS. Our results therefore are likely somewhat undercounted.
Secondary data analysis depends on coding accuracy, but is limited by both human error and reluctance of physicians to introduce stigmatized diagnoses into patient records. This concern is balanced, however, by the benefit to reimbursement of documenting a complex diagnosis to justify patient billing time.
The years 2002 through 2008, concluding just prior to implementation of health care reform in Massachusetts, provide an important baseline for future comparison. Generalizability of results from this time frame may be limited by subsequent changes in health care delivery and policy and by variation in the socioeconomic context of injury.
CONCLUSIONS
Use of a large, multisource, statewide data set permits characterization of women of reproductive age who are likely to meet clinical criteria for substance use disorder, identification of injury rates, and comparison of injury prevalence by substance use disorder identification and by type of drug use. Among women of reproductive age who sought medical treatment in Massachusetts hospitals between 2002 and 2008, those with substance use disorder had a greater likelihood of injury, and among women with an substance use disorder, those who combined alcohol and drugs, had the greatest likelihood of any injury.
The strength of the association between substance use disorder and injury in women of reproductive age suggests the importance of targeted screening for drug and alcohol use disorders when injured women present to the ED. Positive scores for validated short-form instruments, such as the three-question form of the Alcohol Use Disorders Identification Test (AUDIT-C)37 and the 10-question Drug Abuse Screen Test (DAST-10)38 indicate a risk for reinjury if substance use is not addressed with brief intervention, referral for assessment, or treatment.
Supplementary Material
Acknowledgments
Supported in part by NIH NIAAA R21AA018395, NIH NIDA R21DA027181 and supplemental funding from the Massachusetts Department of Public Health and the Department of Emergency Medicine, Boston University School of Medicine.
Footnotes
The authors have no relevant financial information or potential conflicts to disclose.
Supporting Information:
The following supporting information is available in the online version of this paper:
Data Supplement S1. Detailed results from model 2. The association of substance use disorders with categories of injury, adjusted for time, demographic factors, and psychiatric and medical history: incident rate ratios (IRRs).
The document is in PDF format.
Please note: Wiley Periodicals Inc. is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- 1.Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings. [Accessed Sep 7, 2014]; NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. Available at: http://www.samhsa.gov/data/NSDUH/2k11Results/NSDUHresults2011.htm.
- 2.Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatr Clin North Am. 2010;33:339–355. doi: 10.1016/j.psc.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clin Psychol Rev. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Ouimette PC, Kimmerling R, Shaw J, Moos R. Physical and sexual abuse among women and men with substance use disorders. Alcohol Treat Q. 2000;18:7–17. [Google Scholar]
- 5.Zilberman ML, Tavares H, Blume SB, el-Guebaly N. Substance use disorders: sex differences and psychiatric comorbidities. Can J Psychiatr. 2003;48:5–13. doi: 10.1177/070674370304800103. [DOI] [PubMed] [Google Scholar]
- 6.Pan IJ, Yi HY. Prevalence of hospitalized live births affected by alcohol and drugs and parturient women diagnosed with substance abuse at live born delivery: United States, 1999–2008. Matern Child Health J. 2013;17:667–676. doi: 10.1007/s10995-012-1046-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madras B, Kuhar MJ. The Effects of Drug Abuse on the Human Nervous System. Waltham, MA: Elsevier Academic Press; 2014. p. 16. [Google Scholar]
- 8.Wu LT, Swartz MS, Wu Z, Mannelli P, Yang C, Blazer DG. Alcohol and drug use disorders among adults in emergency department settings in the United States. Ann Emerg Med. 2012;60:172–180. doi: 10.1016/j.annemergmed.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perron BE, Bohnert AS, Monsell SE, Vaughn MG, Epperson M, Howard MO. Patterns and correlates of drug-related ED visits: results from a national survey. Am J Emerg Med. 2011;29:704–710. doi: 10.1016/j.ajem.2010.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network. National Estimates of Drug-Related Emergency Department Visits. [Accessed Sep 7, 2014]; (HHS Pub. No. (SMA) 13-4760, DAWN Series D-39. Available at: http://www.samhsa.gov/data/2k13/DAWN2k10ED/DAWN2k10ED.htm.
- 11.Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2010 Emergency Department Summary Tables. [Accessed Sep 7, 2014]; Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2010_ed_web_tables.pdf.
- 12.Centers for Disease Control and Prevention. The WISQARS Nonfatal Injury Reports 2001 – 2013. [Accessed Sep 7, 2014]; Available at: http://webappa.cdc.gov/sasweb/ncipc/nfirates2001.html.
- 13.Hwang M, Chlan KM, Vogel LC, Zebracki K. Substance use in young adults with pediatric-onset spinal cord injury. Brain Inj. 2012;50:497–501. doi: 10.1038/sc.2012.8. [DOI] [PubMed] [Google Scholar]
- 14.Corrigan JD, Bogner J, Holloman C. Lifetime history of traumatic brain injury among persons with substance use disorders. Brain Inj. 2012;26:139–150. doi: 10.3109/02699052.2011.648705. [DOI] [PubMed] [Google Scholar]
- 15.Talving P, Plurad D, Barmparas G, et al. isolated severe traumatic brain injuries: association of blood alcohol levels with the severity of injuries and outcomes. J Trauma. 2010;68:357–362. doi: 10.1097/TA.0b013e3181bb80bf. [DOI] [PubMed] [Google Scholar]
- 16.Murphy DA, Shetty V, Resell J, Zigler C, Yamashita DD. Substance use in vulnerable patients with orofacial injury: prevalence, correlates, and unmet service needs. J Trauma. 2009;66:477–484. doi: 10.1097/TA.0b013e318164773a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davis CS, Esposito TJ, Palladino-Davis AG, et al. Implications of alcohol intoxication at the time of burn and smoke inhalation injury: an epidemiologic and clinical analysis. J Burn Care Res. 2013;34:120–126. doi: 10.1097/BCR.0b013e3182644c58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaysen DL, Lindgren KP, Lee CM, Lewis MA, Fossos N, Atkins DC. Alcohol-involved assault and the course of PTSD in female crime victims. J Trauma Stress. 2010;23:523–527. doi: 10.1002/jts.20542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cherpitel CJ, Ye Y, Greenfield TK, Bond J, Kerr WC, Midanik LT. Alcohol-related injury and driving while intoxicated: a risk function analysis of two alcohol-related events in the 2000 and 2005 National Alcohol Surveys. Am J Drug Alcohol Abuse. 2010;36:168–174. doi: 10.3109/00952991003793851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Danks RR, Wibbenmeyer LA, Faucher LD, et al. Methamphetamine-associated burn injuries: a retrospective analysis. J Burn Care Rehabil. 2004;25:425–429. doi: 10.1097/01.bcr.0000138298.30449.aa. [DOI] [PubMed] [Google Scholar]
- 21.Haaz S, Gache P. Medical stakes and prospects in alcohol use amongst the elderly. Rev Med Suisse. 2007;3:1673–1676. [PubMed] [Google Scholar]
- 22.Delcher C, Johnson R, Maldonado-Molina MM. Driving after drinking among young adults of different race/ethnicities in the United States: unique risk factors in early adolescence? J Adolesc Health. 2013;52:584–591. doi: 10.1016/j.jadohealth.2012.10.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weinsheimer RL, Schermer CR, Malcoe LH, Balduf LM, Bloomfield LA. Severe intimate partner violence and alcohol use among female trauma patients. J Trauma. 2005;58:22–29. doi: 10.1097/01.ta.0000151180.77168.a6. [DOI] [PubMed] [Google Scholar]
- 24.Vitale S, van de Mheen D. Illicit drug use and injuries: a review of emergency room studies. Drug Alcohol Depend. 2006;82:1–9. doi: 10.1016/j.drugalcdep.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 25.Soderstrom C, Smith GS, Dischinger PC, et al. Psychoactive substance use disorders among seriously injured trauma center patients. JAMA. 1997;277:1769–1774. [PubMed] [Google Scholar]
- 26.McAuliffe WE, Woodworth R, Zhang CH, et al. Identifying substance abuse treatment gaps in substate areas. J Subst Abuse Treat. 2002;23:199–208. doi: 10.1016/s0740-5472(02)00263-5. [DOI] [PubMed] [Google Scholar]
- 27.McAuliffe WE, LaBrie R, Lomuto N, et al. Measuring interstate variations in drug problems. Drug Alcohol Depend. 1999;53:125–145. doi: 10.1016/s0376-8716(98)00123-9. [DOI] [PubMed] [Google Scholar]
- 28.McAuliffe WE, LaBrie RA, Lomuto N, et al. Measuring interstate variations in problems related to alcohol use disorders. In: Wilson RA, Dufour MC, editors. The Epidemiology of Alcohol Problems in Small Geographic Areas. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1999. [Google Scholar]
- 29.Mertens JR, Lu YW, Parthasarathy S, Moore C, Weisner CM. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: comparison with matched controls. Arch Intern Med. 2003;163:2511–2517. doi: 10.1001/archinte.163.20.2511. [DOI] [PubMed] [Google Scholar]
- 30.Council CL, editor. Health Services Utilization by Individuals with Substance Abuse and Mental Disorders. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2004. (DHHS Publication No. SMA 04-3949, Analytic Series A-25). [Google Scholar]
- 31.Korcha RA, Cherpitel CJ, Witbrodt J, et al. Violence-related injury and gender: the role of alcohol and alcohol combined with illicit drugs. Drug Alcohol Rev. 2014;33:43–50. doi: 10.1111/dar.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cherpitel CJ, Martin G, Macdonald S, Brubacher JR, Stenstrom R. Alcohol and drug use as predictors of intentional injuries in two emergency departments in British Columbia. Am J Addict. 2013;22:87–92. doi: 10.1111/j.1521-0391.2013.00316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Colantonia A, Mar W, Escobar M, et al. Women’s health outcomes after traumatic brain injury. J Womens Health. 2010;19:1–8. doi: 10.1089/jwh.2009.1740. [DOI] [PubMed] [Google Scholar]
- 34.Lea S, Black K, Asbridge M. An overview of injuries to adolescents and young adults related to substance use: data from Canadian emergency departments. Can J Emerg Med. 2009;11:330–336. doi: 10.1017/s1481803500011374. [DOI] [PubMed] [Google Scholar]
- 35.Sex, gender, and health: the need for a new approach. BMJ. 2001;323:1061–1063. doi: 10.1136/bmj.323.7320.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.National Alliance for Caregiving, American Association of Retired Persons. [Accessed Sep 7, 2014];Caregiving in the U.S., 2009. Available at: http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf. [Google Scholar]
- 37.Frank D, DeBenedetti BA, Volk RJ, Williams EC, Kivlahan DR, Bradley KA. Effectiveness of the AUDIT-C as a screening test for alcohol misuse in three race/ethnic groups. J Gen Intern Med. 2008;23:781–787. doi: 10.1007/s11606-008-0594-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gavin DR, Ross HE, Skinner HA. Diagnostic validity of the DAST in the assessment of SDM-III drug disorders. Br J Addiction. 1989:301–371. doi: 10.1111/j.1360-0443.1989.tb03463.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.