Abstract
Background
Although high rates of alcohol consumption and related problems have been observed among HIV-infected men who have sex with men (MSM), little is known about the long-term patterns of and factors associated with hazardous alcohol use in this population. We sought to identify alcohol use trajectories and correlates of hazardous alcohol use among HIV-infected MSM.
Methods
Sexually active, HIV-infected MSM participating in the Veterans Aging Cohort Study were eligible for inclusion. Participants were recruited from VA infectious disease clinics in Atlanta, Baltimore, New York, Houston, Los Angeles, Pittsburgh, and Washington, DC. Data from annual self-reported assessments and group-based trajectory models were used to identify distinct alcohol use trajectories over an eight-year study period (2002–2010). We then used generalized estimate equations (GEE) to examine longitudinal correlates of hazardous alcohol use (defined as an AUDIT-C score ≥4).
Results
Among 1,065 participants, the mean age was 45.5 (SD=9.2) and 606 (58.2%) were African American. Baseline hazardous alcohol use was reported by 309 (29.3%). Group-based trajectory modeling revealed a distinct group (12.5% of the sample) with consistently hazardous alcohol use, characterized by a mean AUDIT-C score of >5 at every time point. In a GEE-based multivariable model, hazardous alcohol use was associated with earning <$6,000 annually, having an alcohol-related diagnosis, using cannabis, and using cocaine.
Conclusions
More than 1 in 10 HIV-infected MSM US veterans reported consistent, long-term hazardous alcohol use. Financial insecurity and concurrent substance use were predictors of consistently hazardous alcohol use, and may be modifiable targets for intervention.
Keywords: alcohol, men who have sex with men, veterans, HIV infection, trajectories, trends
1. INTRODUCTION
Frequent alcohol use and heavy episodic drinking are common among gay, bisexual, and other men who have sex with men (MSM; Stall et al., 2001; Thiede et al., 2003). Findings from some nationally representative surveys suggest that MSM use alcohol more frequently than heterosexual men (Cochran et al., 2000; Dermody et al., 2014). Hazardous alcohol consumption (drinking that is associated with risk for alcohol problems) is a particular concern among MSM living with HIV, and is associated with poorer HIV treatment outcomes (Woolf-King et al., 2014). A recently published study of HIV-infected MSM in primary care found that hazardous alcohol use was associated with having a detectable viral load (Skeer et al., 2012a). Moreover, hazardous alcohol use is an established predictor of sexual risk behavior with HIV-negative or unknown status partners among HIV-positive MSM (Bruce et al., 2013; Parsons et al., 2005; Purcell et al., 2001). Among HIV positive persons generally, the sequelae of long-term hazardous alcohol use includes a range of adverse health outcomes, including medical and psychiatric comorbidities (Freiberg and Kraemer, 2010; Lim et al., 2014; Sullivan et al., 2011), liver disease (Salmon-Ceron et al., 2005), and poorer immune status (Skeer et al., 2012b).
Despite the individual and public health consequences related to alcohol use among HIV-infected MSM, few longitudinal studies have examined how patterns of drinking may change over time. The identification of distinct alcohol use “trajectories” (i.e., well-defined sub-groups of people who follow similar patterns of alcohol consumption over time) has a number of important public health implications. Such methods could improve the predictive capacity of screening tools to identify individuals at high risk of continued hazardous alcohol use, and may also result in better understanding of the adverse health outcomes associated with long-term, consistent hazardous alcohol use (compared to episodic hazardous drinking). The determination of hazardous drinking trajectories may also be useful for developing and focusing more intensive pharmacological and non-pharmacological treatment for subgroups of HIV-infected MSM at greatest risk of alcohol problems. Research to date has primarily focused on drinking trajectories during critical developmental periods of adolescence to emerging adulthood (Chassin et al., 2002; Hatzenbuehler et al., 2008; Marshal et al., 2009). Much less is known about alcohol use trajectories among adult MSM, particularly those living with HIV.
Not only are the longitudinal patterns of alcohol use in HIV-infected MSM poorly understood, the predictors of distinct alcohol use trajectories have not been well examined. However, in military populations, depression and posttraumatic stress disorder (PTSD) have been identified as key risk factors for the development and acceleration of alcohol-related problems (Jacobson et al., 2008; Marshall et al., 2012; Seal et al., 2011). A recent study observed significantly higher rates of hazardous alcohol use among gay and bisexual veterans compared to heterosexual males, as well as an increased prevalence of concurrent PTSD symptomatology and depression (Cochran et al., 2013). Further research is required to inform alcohol-focused prevention and risk reductions interventions for the over one million sexual minority veterans in the United States (Gates, 2004), including those who are HIV-infected.
The primary objective of this study was to identify long-term alcohol drinking trajectories among HIV-infected, sexually active MSM in a prospective cohort of veterans engaged in care in the United States. Additionally, we sought to examine the sociodemographic, behavioral, and clinical correlates of hazardous alcohol use in order to identify modifiable factors that may improve alcohol treatment interventions for this population.
2. MATERIAL AND METHODS
2.1. Study Design and Data Sources
The primary objectives, design, and methods of the Veterans Aging Cohort Study (VACS) have been described elsewhere (Conigliaro et al., 2004; Justice et al., 2006, 2001). This study utilizes data from the eight-site VACS, which enrolled HIV-infected participants receiving medical care at Veterans Health Administration (VHA) facilities in: Atlanta, Georgia; Baltimore, Maryland; Bronx, New York; Houston, Texas; Los Angeles, California; Manhattan, New York; Pittsburgh, Pennsylvania; and Washington, D.C. from 2002 to 2010 (Justice et al., 2006). At each assessment scheduled approximately annually (six waves of data collection in total), participants completed a comprehensive questionnaire, which solicits information regarding sociodemographic characteristics, general health status, health conditions, alcohol and substance use, sexual activity, and other behaviors. In addition to self-reported survey data, VACS extracted and linked information from electronic medical records, including diagnoses recorded using the International Classification of Diseases, Ninth Revision (ICD-9) codes (Centers for Disease Control and Prevention, 2013). The VACS was approved by the institutional review boards at each participating VHA Medical Center and affiliated academic institutions.
2.2. Study Sample
All HIV-infected male participants enrolled between June 1st, 2002 and September 30th, 2010 were eligible for inclusion. Of the 3,537 potentially eligible participants, we excluded 1,390 (39.3%) who reported sex with females only at baseline, 943 (26.7%) who reported no recent sexual activity in the past year, and 99 (2.8%) who refused to answer the sexual activity questions. We also excluded 40 (1.1%) who reported never consuming an alcoholic drink in their lifetime. The final analytic baseline sample was 1,065 sexually active, HIV-infected MSM. In all analyses (see below), we defined lost to follow-up as never returning to complete a follow-up assessment during the study period (i.e., date of recruitment until November 1st, 2011).
2.3. Measures
The primary outcomes for these analyses were scores on the AUDIT-C questionnaire (Bush et al., 1998). This screening test evaluates three measures of alcohol consumption, including frequency of alcohol use, quantity of alcohol consumed, and heavy episodic drinking (consumption of ≥6 drinks on ≥1 occasion) during the past year. The AUDIT-C has been found to be a reliable and valid screening instrument to assess risk of hazardous or harmful alcohol use among veterans (Bradley et al., 2003; Bush et al., 1998), including those enrolled in the VACS (McGinnis et al., 2013). The AUDIT-C was administered at baseline and at follow-up: in this longitudinal study, scores from all available assessments were examined. To be consistent with previous studies (Bradley et al., 2007; Saitz, 2005), we defined hazardous alcohol use dichotomously as a score of ≥4 on the AUDIT-C.
We examined sociodemographic, behavioral, and clinical variables as correlates of hazardous alcohol use. These independent variables were chosen based on a priori hypotheses that were informed by previous studies examining factors associated with unhealthy alcohol use in male veterans and MSM (Cochran et al., 2013; Jakupcak et al., 2010; Kraemer et al., 2006; Stall et al., 2001; Sullivan et al., 2011; Wong et al., 2008). Sociodemographic self-reported variables included: age (in years); education (some college or greater, high school or less); race (African American, white, other); ethnicity (Hispanic/Latino, not Hispanic/Latino); marital status (married or living with partner, divorced/separated/widowed, never married); employment status (employed for wages or self-employed, unemployed/student/retired/unable to work/other); annual household income (<$6,000, $6,000 – $11,999, $12,000 – $24,999, $25,000 – $49,999, ≥$50,000); and ever homeless (yes, no). Behavioral self-reported variables referred to activities in the past year, and included: type of sex partner(s) (males only, males and females); cannabis use (yes, no); cocaine use (yes, no); and other stimulant use (yes, no), including amphetamines, speed, and crystal methamphetamine. Clinical variables assessed included: depressive symptomatology, measured using the Patient Health Questionnaire (PHQ-9) (Kroenke et al., 2001); baseline hepatitis C virus (HCV) status (positive, negative), defined as a positive HCV antibody test or an ICD-9 code for this diagnosis; and past year receipt of VHA outpatient services for substance abuse treatment (yes, no), defined using substance use disorder-specific outpatient clinic “stop codes” (i.e., unique identifiers for all inpatient and outpatient care services received in the VHA; Harris et al., 2010). Finally, we used ICD-9 codes to define diagnoses for the following conditions, recorded between 12 months prior to VACS enrollment and the end of each participant’s follow-up: alcohol-related diagnosis (yes, no), defined by ICD-9 codes 291.x, 303.x, and 305.0x; drug-related diagnosis (yes, no), defined by ICD-9 codes 292.x and 305.2–305.9; major depressive disorder diagnosis (yes, no), defined by ICD-9 codes 296.2x; and posttraumatic stress disorder (PTSD) (yes, no), defined by ICD-9 code 309.81.
2.4. Statistical Analyses
As a first step, we assessed differences in sociodemographic, behavioral, and clinical characteristics by baseline hazardous alcohol use. We used the Pearson χ2 test for categorical data and the Wilcoxon rank-sum test for continuous data. We then plotted the proportion reporting hazardous alcohol use at each assessment, and used the Cochran-Armitage trend to evaluate the presence of linear trends (Fleiss et al., 2003).
Next, we used a semi-parametric, group-based method (Jones et al., 2001) to fit AUDIT-C score trajectories. This approach has been used successfully in previous studies examining alcohol use trajectories among adolescents (Chassin et al., 2002) and HIV-infected women (Cook et al., 2013), as well as stimulant use trajectories among MSM (Lim et al., 2012). The procedure sorts each individual’s set of AUDIT-C scores from all surveys into “clusters”, and estimates a single model (consisting of distinct trajectories) from the data. The trajectory with the highest probability of membership is then assigned to each individual. Average posterior membership probabilities greater than 0.7 indicate adequate internal reliability (Andruff et al., 2009). Unlike latent class growth models, group-based trajectory modeling permits estimation of mean growth curves for each cluster, and captures the extent of individual variation around these group trajectories (Muthén and Muthén, 2000). Individuals with missing observations are included, since the procedure (PROC TRACJ) uses all values from each individual to estimate participants’ trajectories (Jones et al., 2001). We selected a zero-inflated Poisson outcome distribution for all trajectory-based models, based on visualization of the data (see Supplemental Material1).
Model selection requires determination of both the number of groups and the trajectory shapes which best describe the data (Jones and Nagin, 2007). To be consistent with published recommendations and previous studies employing PROC TRAJ (Nagin and Odgers, 2010; Østbye et al., 2011; Schmitz et al., 2013), we considered several factors to determine the number of groups and trajectory shapes. Specifically, we examined model fit statistics (i.e., the Bayesian information criterion [BIC], with BIC values closer to zero indicating a better fit), significance of polynomial terms, and the values of average posterior group membership probability, leaning towards parsimony in the number of trajectory groups. We aimed for models in which each group membership probability was greater than 5% (Jones and Nagin, 2007). We started with quadratic specifications for each trajectory shape, as models with cubic polynomial specifications failed to converge. We first compared whether an additional group was a better fit, based on the criteria described above. If so, we then dropped non-significant polynomial terms from each trajectory shape, until a final BIC for that number of groups was obtained. This procedure was conducted iteratively until a final “best fit” model was determined. Estimated trajectories and observed mean AUDIT-C scores at each visit for each trajectory group were then computed and plotted using TRAJPLOT(Jones, 2012). Finally, we examined baseline factors associated with membership in each trajectory.
In a second set of longitudinal analyses, we examined factors associated with hazardous alcohol use over the study period using generalized estimating equations (GEE; Liang and Zeger, 1986). The following independent variables were considered as time-varying measures in GEE analyses: type of sex partner(s), depressive symptomatology, receipt of outpatient VHA substance abuse treatment, and substance use (i.e., cannabis, cocaine, stimulants). Third, to determine factors independently associated with hazardous alcohol use over follow-up, we fit a multivariable logistic GEE model, including all variables found to be significantly associated with hazardous alcohol use in bivariable analyses (p < 0.05). To account for population-averaged changes in the prevalence of hazardous alcohol use over the study period, linear and higher-order time variables (years since baseline) were included in the final model.
In a series of sensitivity analyses and to account for possible differential loss to follow-up, we re-ran the GEE regression models with stabilized inverse probability of censoring weights (IPCW) (Robins and Finkelstein, 2000). In IPCW analyses, the sample is reweighted such that the contribution of participants who remain in the study, but who share characteristics of persons who drop out, is effectively inflated. We constructed IPCW using pooled logistic regression, conditional on baseline covariates, as described elsewhere (Cain and Cole, 2009). All statistical analyses were conducted in SAS version 9.3 (SAS Institute Inc., Cary, NC), and all p-values are two-sided.
3. RESULTS
3.1. Sample Characteristics
The 1,065 eligible study subjects contributed a total of 5,103 person-years of follow-up. The median number of completed assessments was 3 (interquartile range [IQR]: 1–4). The characteristics of the study sample are shown in Table 1. Among 1,065 eligible participants, the median age at baseline was 45 (interquartile range [IQR]: 39 – 52) and the majority (58.0%) were African American. At baseline, 309 (29.0%) were classified as hazardous drinkers. As shown in Table 1, those with hazardous alcohol use at baseline were more likely to have low annual income, report a history of homelessness, report both male and female sex partners in the past year, use cannabis, use cocaine, and be HCV positive (all p < 0.005). Hazardous drinkers were also more likely to: have an alcohol-related or drug-related diagnosis (both p < 0.001); have higher scores on the PHQ-9, indicating greater depressive symptomology (p = 0.002); and receive outpatient treatment for substance abuse in the past year (p = 0.031).
Table 1.
Sociodemographic, behavioral, substance use, and clinical characteristics associated with hazardous alcohol use at baseline† among HIV-infected male VACS participants who have sex with men (n= 1065)
| Characteristic | All participants |
Hazardous Alcohol Use† | p-value | |
|---|---|---|---|---|
| Yes (n = 309)* |
No (n = 745)* |
|||
| Age at baseline, median (IQR) | 45 (39 – 52) | 44 (39 – 50) | 45 (39 – 52) | 0.063 |
| Race, n (%) | ||||
| African American | 598 (58.0) | 175 (58.6) | 423 (59.2) | 0.745 |
| White | 374 (36.3) | 109 (35.9) | 265 (36.5) | |
| Other | 59 (5.7) | 20 (6.5) | 39 (5.3) | |
| Hispanic/Latino ethnicity, n (%) | 91 (9.7) | 31 (34.4) | 59 (65.6) | 0.245 |
| Education, n (%) | ||||
| High school or less | 258 (24.5) | 84 (27.2) | 174 (23.4) | 0.188 |
| Some college or greater | 796 (75.5) | 225 (72.8) | 571 (76.6) | |
| Marital status at baseline, n (%) | ||||
| Married or living with partner | 218 (20.9) | 63 (20.7) | 155 (21.0) | 0.980 |
| Divorced/separated/widowed | 308 (29.6) | 89 (29.3) | 219 (29.7) | |
| Never married | 516 (49.5) | 152 (50.0) | 364 (49.3) | |
| Employment status at baseline, n (%) | ||||
| Employed or self-employed | 459 (43.5) | 128 (41.4) | 331 (44.4) | 0.370 |
| Unemployed/retired/other | 595 (56.5) | 181 (58.6) | 414 (55.6) | |
| Annual income at baseline, n (%) | ||||
| < $6,000 | 149 (14.4) | 68 (22.4) | 81 (11.1) | <0.001 |
| $6,000 – $11,999 | 237 (22.9) | 67 (22.1) | 170 (23.2) | |
| $12,000 – $24,999 | 269 (26.0) | 73 (24.1) | 196 (26.8) | |
| $25,000 – $49,999 | 256 (24.7) | 72 (23.8) | 184 (25.1) | |
| ≥$50,000 | 124 (12.0) | 23 (7.6) | 101 (13.8) | |
| Ever homeless, n (%) | 382 (36.3) | 133 (43.0) | 249 (33.5) | 0.003 |
| Sex partner(s)¶n (%) | ||||
| Males only | 923 (87.6) | 250 (80.9) | 673 (90.3) | <0.001 |
| Both males and females | 131 (12.4) | 59 (19.1) | 72 (9.7) | |
| Alcohol-related diagnosis§n (%) | 240 (22.8) | 123 (39.8) | 117 (15.7) | <0.001 |
| Drug-related diagnosis§n (%) | 282 (26.8) | 120 (38.8) | 162 (21.7) | <0.001 |
| Major depressive disorder diagnosis§n (%) | 264 (24.8) | 81 (26.2) | 183 (24.6) | 0.574 |
| PTSD diagnosis§n (%) | 88 (8.4) | 33 (10.7) | 55 (7.4) | 0.078 |
| PHQ-9 score‡ at baseline, median (IQR) | 4 (1 – 9) | 5 (1 – 9) | 3 (1 – 8) | 0.002 |
| Cannabis use¶n (%) | 427 (41.0) | 152 (49.7) | 275 (37.4) | <0.001 |
| Cocaine use¶n (%) | 220 (21.2) | 103 (33.6) | 117 (16.0) | <0.001 |
| Stimulant use¶n (%) | 90 (8.7) | 30 (9.8) | 60 (8.2) | 0.414 |
| Substance abuse treatment¶, n (%) | 107 (10.2) | 41 (13.3) | 66 (8.9) | 0.031 |
| Positive HCV status at baseline, n (%) | 342 (32.5) | 124 (40.1) | 218 (29.3) | <0.001 |
Hazardous alcohol use de ined as a score of ≥ 4 on AUDIT-C (Saitz, 2005) at baseline;
denotes use or experiences in the past-year, reported at baseline;
columns don’t add to 100% due to rounding and missing values;
PHQ-9 score ≥10 indicates moderate depression severity (Kroenke et al., 2001).
recorded ICD-9 diagnosis between 12 months before VACS enrollment and end of study period. Abbreviations: HCV = hepatitis C virus; PHQ-9 = Patient Health Questionnaire-9 (Kroenke et al., 2001); PTSD = posttraumatic stress disorder; VACS = Veterans Aging Cohort Study.
3.2. Hazardous Alcohol Use Over Time
Over the study period, 126 (11.8%) eligible participants were lost to follow-up. Persons lost to follow-up did not differ from those who remained in the study with respect to age, race, marital status, income, or baseline AUDIT-C score. Participants lost to follow-up were: more likely to have a high school or less education (33.3% vs. 23.6%); less likely to be employed (31.0% vs. 41.2%); and more likely to report ever experiencing homelessness (45.2% vs. 35.5%). We examined the extent to which these differences may have influenced our results in IPCW analyses (see below).
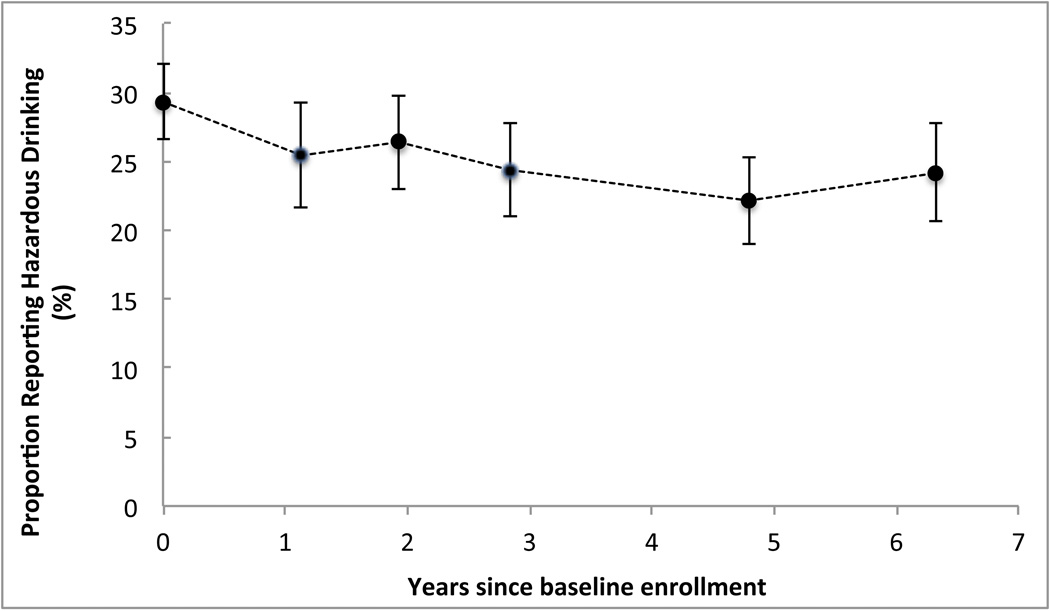
As shown in Figure 1, the proportion of participants classified with hazardous drinkers declined over subsequent years of follow-up (trend test p = 0.002). Between baseline enrollment and the final year of follow-up, the proportion scoring ≥4 on the AUDIT-C decreased from 29.0% to 24.2%. Results did not differ substantially in a weighted IPCW analysis to account for possible differential loss to follow-up (trend test p = 0.001).
Figure 1. Declining prevalence of hazardous alcohol use among HIV-infected men who have sex with men.
Hazardous alcohol use defined as a score of ≥4 on the AUDIT-C (Saitz, 2005). Note: data points represent average time (in years) since baseline enrollment for completion of follow-up assessments 1 through 5. Abbreviations: VACS = Veterans Aging Cohort Study.
3.3. Group-Based Drinking Trajectory Models
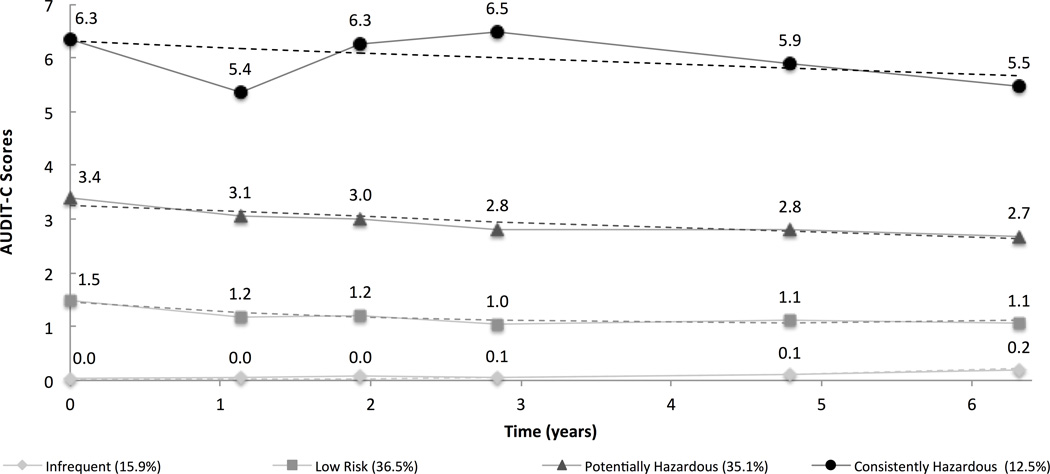
The estimated and observed mean AUDIT-C scores at each time point for the final group-based trajectory model are shown in Figure 2. The final four-group solution (which had the lowest BIC, see Supplemental Material2) produced AUDIT-C score trajectories that were either stable or gradually decreasing over time. We classified the four trajectories as: infrequent drinkers (15.9% of the sample); low-risk drinkers (36.5%); potentially hazardous drinkers (37.6%); and consistently hazardous drinkers (12.0%). Infrequent, potentially hazardous, and consistently hazardous drinkers were best characterized by intercept and linear terms, while the low-risk drinking trajectory was best characterized by intercept, linear, and quadratic terms. The mean probability of membership in each group was 0.91, 0.86, 0.82, and 0.89, respectively, indicating acceptable internal reliability. The proportion of participants missing more than three waves of data (the median number of completed assessments) did not vary significantly by group (p = 0.157).
Figure 2. Group-based AUDIT-C score trajectories among HIV-infected men who have sex with men (2002–2011).
Note: dashed lines (---) represent estimated trajectories; solid lines (−) represent observed mean AUDIT-C score values for each trajectory group. Note: x-axis values represent average time (in years) since baseline enrollment for completion of waves 2 through 6, Note: model selected based on BIC values shown in Figure S2 (see Supplemental Material3). The final model includes intercept and linear terms for infrequent, potentially hazardous, and unhealthy drinkers, and an intercept, linear, and quadratic term for low risk drinkers. Abbreviations: AUDIT-C = Alcohol Use Disorders Identification Test-Consumption questionnaire; VACS = Veterans Aging Cohort Study.
Baseline factors that were associated with trajectory group membership are shown in Table 2. As expected, the baseline AUDIT-C scores varied significantly across the groups: the mean score was 0.0 (standard deviation [SD] = 0.1), 1.5 (SD = 1.2), 3.4 (SD = 2.0), and 6.3 (2.6) for infrequent drinkers, low-risk drinkers, potentially hazardous drinkers, and consistently hazardous drinkers, respectively. Other baseline factors significantly associated with group membership included age, education, race, employment status, annual income, history of homelessness, having diagnoses of an alcohol use disorder or drug use disorder, cannabis use, and cocaine use.
Table 2.
Sociodemographic, behavioral, substance use, and clinical factors associated with membership in group-based drinking trajectories among HIV-infected men who have sex with men(n= 1065).
| Characteristic | Infrequent Drinkers (n= 109) |
Low Risk (n= 364) |
Potentially Hazardous (n= 353) |
Consistently Hazardous (n= 113) |
p-value* |
|---|---|---|---|---|---|
| mean, SD | |||||
| Age at baseline | 47.5 (9.3) | 45.8 (8.8) | 44.5 (9.8) | 45.0 (7.2) | 0.014 |
| AUDIT-C score at baseline | 0.0 (0.1) | 1.5 (1.2) | 3.4 (2.0) | 6.3 (2.6) | <0.001 |
| Depressive symptomology (PHQ-9 score) at baseline | 5.7 (6.4) | 5.7 (6.3) | 5.1 (5.3) | 6.8 (6.4) | 0.066 |
|
n, % | |||||
| Unhealthy drinking (AUDIT-C ≥ 4) at baseline | 0 (0.0) | 17 (4.7) | 151 (42.8) | 102 (91.1) | <0.001 |
| High school education or greater | 74 (67.9) | 286 (78.6) | 281 (79.6) | 76 (67.3) | 0.006 |
| African American race | 58 (54.2) | 228 (64.6) | 189 (54.0) | 54 (49.5) | 0.012 |
| Married or common law at baseline | 57 (52.3) | 182 (50.4) | 183 (52.1) | 50 (45.9) | 0.785 |
| Employed/self-employed at baseline | 38 (34.9) | 168 (46.2) | 172 (48.7) | 46 (40.7) | 0.057 |
| <$6,000 annual income at baseline | 15 (14.2) | 36 (10.0) | 50 (14.4) | 27 (25.0) | 0.014 |
| Ever homeless | 40 (37.0) | 94 (26.0) | 93 (26.4) | 44 (38.9) | 0.009 |
| Male and female sex partners¶ | 13 (11.9) | 41 (11.3) | 40 (11.3) | 21 (18.6) | 0.184 |
| Alcohol-related diagnosis§ | 14 (12.8) | 60 (16.5) | 74 (21.0) | 59 (62.2) | <0.001 |
| Drug-related diagnosis§ | 25 (22.9) | 94 (23.1) | 93 (26.4) | 49 (43.4) | <0.001 |
| Major depressive disorder diagnosis§ | 30 (27.5) | 91 (25.0) | 90 (25.5) | 30 (26.6) | 0.954 |
| PTSD diagnosis§ | 15 (13.8) | 19 (5.2) | 32 (9.1) | 12 (10.6) | 0.020 |
| Cannabis use¶ | 17 (16.5) | 147 (41.0) | 162 (46.2) | 58 (52.3) | <0.001 |
| Cocaine use¶ | 10 (9.8) | 68 (19.0) | 73 (21.0) | 37 (33.0) | <0.001 |
| Stimulant use¶ | 8 (7.8) | 30 (8.4) | 33 (9.5) | 11 (9.7) | 0.921 |
| Substance abuse treatment¶ | 9 (8.3) | 35 (9.6) | 32 (9.1) | 16 (14.2) | 0.399 |
| Positive HCV status at baseline | 35 (32.1) | 117 (32.1) | 111 (31.4) | 42 (37.2) | 0.722 |
Derived from F ratio (continuous values) or chi-square statistic (categorical variables);
Denotes use or experiences in the past-year, reported at baseline;
recorded ICD-9 diagnosis between 12 months before VACS enrollment and end of study period. Abbreviations: AUDIT-C = Alcohol Use Disorders Identification Test-Consumption questionnaire (Bush et al., 1998); HCV = hepatitis C virus; PHQ-9 = Patient Health Questionnaire-9 (Kroenke et al., 2001); PTSD = posttraumatic stress disorder; VACS = Veterans Aging Cohort Study.
3.4. Factors Associated with Hazardous Alcohol Use Over Time
Factors associated with hazardous alcohol use in longitudinal analyses are shown in Table 3. In the final multivariable model, hazardous alcohol use was positively and independently associated with: <$6,000 in annual income, having an alcohol-related diagnosis, past year cannabis use, and past year cocaine use. Linear and quadratic time terms were significant in the final model, indicating a decreasing prevalence of unhealthy drinking earlier in the study period that stabilized over time. Results were not meaningfully different in a weighted GEE model using IPCW (data not shown).
Table 3.
Factors associated with hazardous alcohol use† over follow-up among HIV-infected men who have sex with men, 2002–2011 (n= 1,065).
| Characteristics | OR | 95% CI | p-value | AOR | 95%CI | p-value |
|---|---|---|---|---|---|---|
| Time (per year) | 0.95 | 0.93 – 0.97 | <0.001 | 0.85 | 0.76 – 0.95 | 0.006 |
| Time2 (per year2) | - | - | - | 1.02 | 1.00 – 1.03 | 0.024 |
|
Sociodemographic and Behavioral Characteristics | ||||||
| Age at baseline (per 10 years) | 0.81 | 0.73 – 0.90 | <0.001 | 0.92 | 0.80 – 1.05 | 0.219 |
| Education (ref: high school or less) | ||||||
| Some college or greater | 1.17 | 1.02 – 1.34 | 0.026 | 0.90 | 0.73 – 1.11 | 0.334 |
| Race (ref: white) | ||||||
| African American | 0.83 | 0.66 – 1.06 | 0.133 | |||
| Other | 1.11 | 0.67 – 1.85 | 0.683 | |||
| Hispanic/Latino Ethnicity (ref: not H/L) | 1.31 | 0.83 – 2.08 | 0.246 | |||
| Marital Status (ref: married, living with partner) | ||||||
| Divorced/separated/widowed | 0.95 | 0.69 – 1.31 | 0.756 | |||
| Never married | 1.12 | 0.84 – 1.51 | 0.444 | |||
| Employment status at baseline (ref: employed) | ||||||
| Unemployed/retired/other | 1.01 | 0.81 – 1.26 | 0.935 | |||
| Annual income at baseline (ref: ≥$50,000) | ||||||
| < $6,000 | 2.43 | 1.57 – 3.76 | <0.001 | 1.74 | 1.08 – 2.79 | 0.022 |
| $6,000 – $11,999 | 1.47 | 0.96 – 2.25 | 0.074 | 1.28 | 0.81 – 2.01 | 0.292 |
| $12,000 – $24,999 | 1.26 | 0.83 – 1.91 | 0.283 | 1.13 | 0.73 – 1.74 | 0.586 |
| $25,000 – $49,999 | 1.34 | 0.88 – 2.04 | 0.170 | 1.27 | 0.83 – 1.96 | 0.272 |
| Ever homeless (ref: no) | 1.38 | 1.10 – 1.73 | 0.005 | 0.77 | 0.58 – 1.02 | 0.071 |
| Sex partner(s)¶* (ref: males only) | ||||||
| Both males and females | 1.17 | 0.90 – 1.52 | 0.231 | |||
|
Clinical and Substance Use Factors | ||||||
| Alcohol-related diagnosis§ (ref: no) | 2.93 | 2.30 – 3.73 | <0.001 | 2.71 | 2.00 – 3.66 | <0.001 |
| Drug-related diagnosis§ (ref: no) | 1.41 | 1.16 – 1.70 | <0.001 | 0.86 | 0.68 – 1.09 | 0.216 |
| Major depressive disorder diagnosis § (ref: no) | 1.13 | 0.93 – 1.38 | 0.216 | |||
| PTSD diagnosis§ (ref: no) | 1.41 | 1.01 – 1.98 | 0.045 | 1.03 | 0.71 – 1.50 | 0.865 |
| PHQ-9 score* (per unit increase) | 1.02 | 1.00 – 1.03 | 0.026 | 1.01 | 0.99 – 1.02 | 0.391 |
| Cannabis use¶* (ref: no use) | 1.68 | 1.43 – 1.98 | <0.001 | 1.47 | 1.22 – 1.76 | <0.001 |
| Cocaine use¶* (ref: no use) | 2.01 | 1.63 – 2.47 | <0.001 | 1.55 | 1.24 – 1.95 | <0.001 |
| Stimulant use¶* (ref: no use) | 1.61 | 1.20 −2.17 | 0.002 | 1.17 | 0.85 – 1.61 | 0.334 |
| Substance abuse treatment¶* (ref: no) | 1.24 | 1.00 – 1.55 | 0.054 | |||
| Positive HCV status at baseline (ref: negative) | 1.22 | 0.97 – 1.54 | 0.087 | |||
Hazardous alcohol use de ined as ≥ 4 on AUDIT-C (Saitz, 2005);
Denotes use or experiences in the past year;
time-updated variable;
recorded ICD-9 diagnosis between 12 months before VACS enrollment and end of study period.
Abbreviations: AOR = adjusted odds ratio; AUD = alcohol use disorder; DUD = drug use disorder; HCV = hepatitis C virus; PHQ-9 = Patient Health Questionniare-9 (Kroenke et al., 2001); PTSD = posttraumatic stress disorder; OR = odds ratio.
4. DISCUSSION
This study demonstrated that the majority of HIV-infected male US military veterans in the VACS who have sex with men exhibited drinking trajectories congruous with stable alcohol consumption patterns. The proportion reporting hazardous alcohol use decreased over time, consistent with other studies (Dearing et al., 2013; Delucchi et al., 2004), and likely reflecting the tendency for total alcohol intake to decrease in older age (Ferreira and Weems, 2008). Approximately one-third reported hazardous drinking at a given time point, and in longitudinal trajectory-based analyses, more than one in ten participants were classified as consistently hazardous drinkers. Compared to other groups, participants in this trajectory were most likely to report a history of homelessness and low annual income, have a prior drug-related diagnosis, and report concurrent use of cannabis and cocaine. Similarly, in a separate population-based model, hazardous alcohol use was independently associated with low annual income, having an alcohol-related diagnosis, concurrent cannabis use, and concurrent cocaine use.
The results of this study have a number of clinical and research implications. First, these analyses support the value of the AUDIT-C as a screening instrument for hazardous alcohol use among male veterans with HIV (Bradley et al., 2004; Bush et al., 1998; Crawford et al. 2013). The group-based trajectory modeling identified a distinct group of individuals who reported consistently high AUDIT-C scores (i.e., ≥6). Importantly, over 90% of these participants had a baseline AUDIT-C score ≥4. These results suggest that scores from the AUDIT-C may predict not only current hazardous drinking, but also continued, ongoing unhealthy alcohol use in the future. Finally, our finding that the consistently hazardous drinkers were most likely to use cannabis and cocaine, as well as have a drug-related diagnosis, suggests that integrated treatments, which simultaneously address alcohol and other drug use, may be beneficial.
The two longitudinal methods employed in this study (trajectory-based and marginal models) provide complementary yet distinct insights into the phenomenon of hazardous alcohol use among HIV-infected MSM. Specifically, the GEE model “pools” data from both consistent and episodic hazardous drinkers (i.e., those with continued AUDIT-C scores ≥4 and those with scores above and below this cut-off) to identify population-based correlates of hazardous alcohol use. These findings provide clinicians and policymakers with insights into the characteristics of individuals who are likely to be hazardous drinkers at any given time point. In contrast, the trajectory-based models demonstrated that participants tended not to deviate substantially from their hazardous drinking patterns recorded at baseline (e.g., those who had AUDIT-C score ≥4 at baseline very likely to remain above this threshold). These results suggest that HIV-infected MSM reporting hazardous alcohol use may require comprehensive programs (rather than brief interventions) to mitigate the adverse health consequences of continued unhealthy alcohol consumption over many years.
In both GEE-based and trajectory modeling analyses, persons classified as consistently hazardous drinkers were more likely than other participants to report low annual income. These findings are consistent with an earlier analysis from our group demonstrating that heavy multiple substance users have lower incomes (Green et al., 2010). Collectively, these results suggest that financial stability may be a modifiable factor that, if intervened upon, may help to reduce unhealthy drinking behavior. A recently published randomized controlled trial demonstrated that individual placement and support (IPS) programs (i.e., individualized rapid job searches, community-based job placement) were effective at increasing competitive employment among veterans with PTSD (Davis et al., 2012). Another study demonstrated that the IPS model improves work outcomes of dually diagnosed veterans (Mueser et al., 2011). More research is needed to determine whether employment-based programs can have positive effects on other health outcomes among veterans, including reductions in alcohol use. In particular, given that employment status was not found to be a correlate of hazardous alcohol use in this study, IPS programs that primarily provide access to low-paying jobs may not be sufficient to reduce unhealthy alcohol and substance use in this population.
Although depressive symptomatology was positively associated with hazardous drinking in bivariable analyses, this variable lost significance in the final adjusted model. It is possible that sociodemographic factors such as age or history of homelessness may have confounded this association. Alternatively, the relationship between hazardous alcohol use and depression among HIV-infected MSM may be nonlinear and/or vary by social and environmental context. One recently published study of over 500 gay-identified men in Australia found that men with major depression were more likely than non-depressed men to abstain from alcohol use, but among users, major depression was associated with heavier alcohol consumption patterns (Holt et al., 2012). Given ongoing concerns regarding depression and high rates of suicidality among sexual minority veterans (Blosnich et al., 2012), further work is required to elucidate these relationships among HIV-infected male US veterans who have sex with men.
Our study has several important limitations. First, the study population was restricted to veterans receiving VHA medical care, and therefore the results may not necessarily be generalizable to all HIV-infected, MSM veterans or HIV-infected MSM in general. Second, most data were collected via self-report, which could be subject to under-reporting or recall bias. However, the instrument used to assess alcohol consumption is well validated (Bush et al., 1998; Frank et al., 2008), and the primary outcomes were highly correlated with measures of alcohol-related problems based on administrative data (i.e., ICD-9 diagnoses). Therefore, we do not expect these biases, if present, to influence our results. Third, although ICD-9 diagnostic codes have been shown to be a reasonable proxy for estimating the burden of some diseases (Borzecki et al., 2004; Tu et al., 2007), some misclassification with respect to these variables is likely. For example, veterans with less severe disease may not seek care, and hence would not have corresponding ICD codes recorded. Additionally, we were unable to analyze precise dates of clinical diagnosis, and thus relied on time-invariant indicator variables representing the presence or absence of an alcohol-related diagnosis, drug-related diagnosis, major depression, or PTSD spanning the period 12 months prior to the date of the baseline interview and the end of each participant’s follow-up. Finally, the selection and post hoc classification of the final set of drinking trajectories were ultimately subjective processes. However, we relied on established recommendations for group-based trajectory modeling (Jones and Nagin, 2007), and our classifications were informed by previously identified trajectories of alcohol consumption over the lifecourse (Chassin et al., 2002; Cook et al., 2013; Jacob et al., 2013, 2009).
In summary, we have demonstrated that group-based trajectory analysis is a promising method to identify patterns and correlates of long-term drinking trajectories among HIV-infected MSM. Further work is needed to identify whether participants classified as consistently hazardous drinkers are at greater risk of adverse HIV-related and other health outcomes than individuals who screen positive for hazardous drinking at one time point. In particular, future research should investigate the association of membership in long-term hazardous drinking trajectories with the development of chronic multi-morbidities, hospitalization, and mortality. These findings support the need for the continued expansion of screening and treatment of alcohol use disorders in the VHA (The Management of Substance Use Disorders Working Group, 2009), specifically to increase the engagement and treatment of HIV-infected MSM who are consistently hazardous alcohol users.
Supplementary Material
Highlights.
In this eight-year prospective cohort study, approximately 1 in 10 HIV-infected male veterans who have sex with men reported consistently hazardous alcohol use
Hazardous alcohol consumption was associated with low annual income, cannabis use, cocaine use, and having an alcohol-related diagnosis
Addressing concurrent substance use and improving financial security may be modifiable targets for intervention to reduce hazardous drinking in this population
Acknowledgements
We would like to acknowledge the Veterans who participate in the Veterans Aging Cohort Study (VACS) and the study coordinators and staff at each VACS site and at the West Haven Coordinating Center. We would also like to thank Melissa Skanderson for her assistance and support during data acquisition.
Role of the funding source
This work was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA: U24-AA022000, U10-AA013566, U01-AA020795, U01-AA020790, U24-AA020794, U10-AA013566, and P01-AA019072), the National Institute of Allergy and Infectious Diseases (P30-AI042853), and in kind by the US Department of Veterans Affairs. Dr. Robert Cook is supported by the NIAAA (U24-AA022002). Dr. Julie Gaither is supported by the National Institute on Drug Abuse (F31-DA035567). Dr. Stephen Maisto is supported by the NIAAA (K05-AA16928). E. Jennifer Edelman is a Yale-Drug Abuse, Addiction, and HIV Research Scholar (K12-DA033312). The sponsors had no role in the study design; the collection, analysis and interpretation of data; the writing of the report; and in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplemental Material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplemental Material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplemental Material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Author disclosures
Contributors
All authors made significant contributions to the study’s design and conduct. Author BDLM led the statistical analysis, with significant input from RLC, KAM, and DAF. Author BDLM wrote the first draft of the manuscript, and all other authors participated in its preparation and critical revision for important intellectual content. All authors contributed to and have approved the final manuscript.
Conflict of interest
No conflicts declared.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
REFERENCES
- Andruff H, Carraro N, Thompson A, Gaudreau P, Louvet B. Latent class growth modelling: A tutorial. Tutor. Quant. Methods Psychol. 2009;5:11–24. [Google Scholar]
- Blosnich JR, Bossarte RM, Silenzio VM. Suicidal ideation among sexual minority veterans: Results from the 2005–2010 Massachusetts Behavioral Risk Factor Surveillance Survey. Am. J. Public Health. 2012;102:S44–S47. doi: 10.2105/AJPH.2011.300565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borzecki AM, Wong AT, Hickey EC, Ash AS, Berlowitz DR. Identifying hypertension-related comorbidities from administrative data: what's the optimal approach? Am. J. Med. Qual. 2004;19:201–206. doi: 10.1177/106286060401900504. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, et al. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female Veterans Affairs patient population. Arch. Intern. Med. 2003;163:821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol. Clin. Exp. Res. 2007;31:1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Kivlahan DR, Zhou XH, Sporleder JL, Epler AJ, McCormick KA, et al. Using alcohol screening results and treatment history to assess the severity of at-risk drinking in Veterans Affairs primary care patients. Alcohol. Clin. Exp. Res. 2004;28:448–455. doi: 10.1097/01.alc.0000117836.38108.38. [DOI] [PubMed] [Google Scholar]
- Bruce D, Kahana S, Harper GW, Fernandez MI and the ATN. Alcohol use predicts sexual risk behavior with HIV-negative or partners of unknown status among young HIV-positive men who have sex with men. AIDS Care. 2013;25:559–565. doi: 10.1080/09540121.2012.720363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA for the Ambulatory Care Quality Improvement Project (ACQUIP) The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Arch. Intern. Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Cain LE, Cole SR. Inverse probability-of-censoring weights for the correction of time-varying noncompliance in the effect of randomized highly active antiretroviral therapy on incident AIDS or death. Stat. Med. 2009;28:1725–1738. doi: 10.1002/sim.3585. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) [[accessed on: Apr 1, 2014]];National Center for Health Statistics (NCHS) 2013 < http://www.cdc.gov/nchs/icd/icd9cm.htm>.
- Chassin L, Pitts SC, Prost J. Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: predictors and substance abuse outcomes. J. Consult. Clin. Psychol. 2002;70:67–78. [PubMed] [Google Scholar]
- Cochran BN, Balsam K, Flentje A, Malte CA, Simpson T. Mental health characteristics of sexual minority veterans. J. Homosex. 2013;60:419–435. doi: 10.1080/00918369.2013.744932. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Keenan C, Schober C, Mays VM. Estimates of alcohol use and clinical treatment needs among homosexually active men and women in the U.S. population. J. Consult. Clin. Psychol. 2000;68:1062–1071. doi: 10.1037//0022-006x.68.6.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conigliaro J, Madenwald T, Bryant K, Braithwaite S, Gordon A, Fultz SL, Maisto S, Samet J, Kraemer K, Cook R, Day N, Roach D, Richey S. The Veterans Aging Cohort Study: observational studies of alcohol use, abuse, and outcomes among human immunodeficiency virus-infected veterans. Alcohol. Clin. Exp. Res. 2004;28:313–321. doi: 10.1097/01.alc.0000113414.73220.21. [DOI] [PubMed] [Google Scholar]
- Cook RL, Zhu F, Belnap BH, Weber KM, Cole SR, Vlahov D, Cook JA, Hessol NA, Wilson TE, Plankey M, Howard AA, Sharp GB, Richardson JL, Cohen MH. Alcohol consumption trajectory patterns in adult women with HIV infection. AIDS Behav. 2013;17:1705–1712. doi: 10.1007/s10461-012-0270-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford EF, Fulton JJ, Swinkels CM, Beckham JC, the VA Mid-Atlantic MIRECC OEF/OIF Registry Workgroup, Calhoun, P.S. Diagnostic efficiency of the AUDIT-C in U.S. veterans with military service since September 11, 2001. Drug Alcohol Depend. 2013;132:101–106. doi: 10.1016/j.drugalcdep.2013.01.012. [DOI] [PubMed] [Google Scholar]
- Davis LL, Leon AC, Toscano R, Drebing CE, Ward LC, Parker PE, Kashner TM, Drake E. A randomized controlled trial of supported employment among veterans with posttraumatic stress disorder. Psychiatr. Serv. 2012;63:464–470. doi: 10.1176/appi.ps.201100340. [DOI] [PubMed] [Google Scholar]
- Dearing RL, Witkiewitz K, Connors GJ, Walitzer KS. Prospective changes in alcohol use among hazardous drinkers in the absence of treatment. Psychol. Addict. Behav. 2013;27:52–61. doi: 10.1037/a0028170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delucchi KL, Matzger H, Weisner C. Dependent and problem drinking over 5 years: a latent class growth analysis. Drug Alcohol Depend. 2004;74:235–244. doi: 10.1016/j.drugalcdep.2003.12.014. [DOI] [PubMed] [Google Scholar]
- Dermody SS, Marshal MP, Cheong J, Burton C, Hughes T, Aranda F, Friedman MS. Longitudinal disparities of hazardous drinking between sexual minority and heterosexual individuals from adolescence to young adulthood. J. Youth Adolesc. 2014;43:30–39. doi: 10.1007/s10964-013-9905-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira MP, Weems MKS. Alcohol consumption by aging adults in the United States: health benefits and detriments. J. Am. Diet. Assoc. 2008;108:1668–1676. doi: 10.1016/j.jada.2008.07.011. [DOI] [PubMed] [Google Scholar]
- Fleiss L, Levin B, Paik MC. Statistical Methods for Rates and Proportions. New York: Wiley-Interscience; 2003. [Google Scholar]
- Frank D, DeBenedetti AF, Volk RJ, Williams EC, Kivlahan DR, Bradley KA. Effectiveness of the AUDIT-C as a screening test for alcohol misuse in three race/ethnic groups. J. Gen. Intern. Med. 2008;23:781–787. doi: 10.1007/s11606-008-0594-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freiberg MS, Kraemer KL. Focus on the heart: alcohol consumption, HIV infection, and cardiovascular disease. Alcohol Res. Health. 2010;33:237–246. [PMC free article] [PubMed] [Google Scholar]
- Gates G. Gay Men And Lesbians In The US Military: Estimates From Census 2000. Washington, DC: The Urban Institute; 2004. [Google Scholar]
- Green TC, Kershaw T, Lin H, Heimer R, Goulet JL, Kraemer KL, Gordon AJ, Maisto SA, Day NL, Bryant K, Fiellin DA, Justice AC. Patterns of drug use and abuse among aging adults with and without HIV: a latent class analysis of a US Veteran cohort. Drug Alcohol Depend. 2010;110:208–220. doi: 10.1016/j.drugalcdep.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris AH, Reeder RN, Ellerbe L, Bowe T. Are VHA administrative location codes valid indicators of specialty substance use disorder treatment? J. Rehabil. Res. Dev. 2010;47:699–708. doi: 10.1682/jrrd.2009.07.0106. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, Fromme K. Trajectories and determinants of alcohol use among LGB young adults and their heterosexual peers: results from a prospective study. Dev. Psychol. 2008;44:81–90. doi: 10.1037/0012-1649.44.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt M, Bryant J, Newman CE, Paquette DM, Mao LM, Kidd MR, Saltman DC, Kippax SC. Patterns of alcohol and other drug use associated with major depression among gay men attending general practices in Australia. Int. J. Ment. Health Ad. 2012;10:141–151. [Google Scholar]
- Jacob T, Blonigen DM, Upah R, Justice AC. Lifetime drinking trajectories among veterans in treatment for HIV. Alcohol. Clin. Exp. Res. 2013;37:1179–1187. doi: 10.1111/acer.12071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob T, Koenig LB, Howell DN, Wood PK, Haber JR. Drinking trajectories from adolescence to the fifties among alcohol-dependent men. J. Stud. Alcohol Drugs. 2009;70:859–869. doi: 10.15288/jsad.2009.70.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson IG, Ryan MA, Hooper TI, Smith TC, Amoroso PJ, Boyko EJ, Gackstetter GD, Wells TS, Bell NS. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA. 2008;300:663–675. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakupcak M, Tull MT, McDermott MJ, Kaysen D, Hunt S, Simpson T. PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addict. Behav. 2010;35:840–843. doi: 10.1016/j.addbeh.2010.03.023. [DOI] [PubMed] [Google Scholar]
- Jones BL. [[accessed on: April 1, 2014]];TRAJ: Group-based modeling of longitudinal data. 2012 < http://www.andrew.cmu.edu/user/bjones/index.htm>.
- Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol. Methods Res. 2007;35:542–571. [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol. Methods Res. 2001;29:374–393. [Google Scholar]
- Justice AC, Dombrowski E, Conigliaro J, Fultz SL, Gibson D, Madenwald T, Goulet J, Simberkoff M, Butt AA, Rimland D, Rodriguez-Barradas MC, Gilbert CL, Oursler KA, Brown S, Leaf DA>, Goetz MB, Bryant K. Veterans Aging Cohort Study (VACS): overview and description. Med. Care. 2006;44:S13–S24. doi: 10.1097/01.mlr.0000223741.02074.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice AC, Landefeld CS, Asch SM, Gifford AL, Whalen CC, Covinsky KE. Justification for a new cohort study of people aging with and without HIV infection. J. Clin. Epidemiol. 2001;54:S3–S8. doi: 10.1016/s0895-4356(01)00440-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer KL, McGinnis KA, Skanderson M, Cook R, Gordon A, Conigliaro J, Shen Y, Fiellin DA, Justice AC. Alcohol problems and health care services use in human immunodeficiency virus (HIV)-infected and HIV-uninfected veterans. Med. Care. 2006;44:S44–S51. doi: 10.1097/01.mlr.0000223703.91275.78. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Lim JK, Tate JP, Fultz SL, Goulet JL, Conigliaro J, Bryant KJ, Gordon AJ, Gibert C, Rimland D, Goetz MB, Klein MB, Fiellin DA, Justice AC, Lo Re V. Relationship between alcohol use categories and noninvasive markers of advanced hepatic fibrosis in HIV-infected, chronic hepatitis C virus-infected, and uninfected patients. Clin. Infect. Dis. 2014;58:1449–1158. doi: 10.1093/cid/ciu097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SH, Ostrow D, Stall R, Chmiel J, Herrick A, Shoptaw S, Kao U, Carrico A, Plankey M. Changes in stimulant drug use over time in the MACS: evidence for resilience against stimulant drug use among men who have sex with men. AIDS Behav. 2012;16:151–158. doi: 10.1007/s10461-010-9866-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R, Thompson AL. Individual trajectories of substance use in lesbian, gay and bisexual youth and heterosexual youth. Addiction. 2009;104:974–981. doi: 10.1111/j.1360-0443.2009.02531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall BDL, Prescott MR, Liberzon I, Tamburrino MB, Calabrese JR, Galea S. Coincident posttraumatic stress disorder and depression predict alcohol abuse during and after deployment among Army National Guard soldiers. Drug Alcohol Depend. 2012;124:193–199. doi: 10.1016/j.drugalcdep.2011.12.027. [DOI] [PubMed] [Google Scholar]
- McGinnis KA, Justice AC, Kraemer KL, Saitz R, Bryant KJ, Fiellin DA. Comparing alcohol screening measures among HIV-infected and -uninfected men. Alcohol. Clin. Exp. Res. 2013;37:435–442. doi: 10.1111/j.1530-0277.2012.01937.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueser KT, Campbell K, Drake RE. The effectiveness of supported employment in people with dual disorders. J. Dual Diagn. 2011;7:90–102. doi: 10.1080/15504263.2011.568360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol. Clin. Exp. Res. 2000;24:882–891. [PubMed] [Google Scholar]
- Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu. Rev. Clin. Psychol. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- Østbye T, Malhotra R, Landerman LR. Body mass trajectories through adulthood: results from the National Longitudinal Survey of Youth 1979 Cohort (1981–2006) Int. J. Epidemiol. 2011;40:240–250. doi: 10.1093/ije/dyq142. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Kutnick AH, Halkitis PN, Punzalan JC, Carbonari JP. Sexual risk behaviors and substance use among alcohol abusing HIV-positive men who have sex with men. J. Psychoactive Drugs. 2005;37:27–36. doi: 10.1080/02791072.2005.10399746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell DW, Parsons JT, Halkitis PN, Mizuno Y, Woods WJ. Substance use and sexual transmission risk behavior of HIV-positive men who have sex with men. J. Subst. Abuse. 2001;13:185–200. doi: 10.1016/s0899-3289(01)00072-4. [DOI] [PubMed] [Google Scholar]
- Robins JM, Finkelstein DM. Correcting for noncompliance and dependent censoring in an AIDS Clinical Trial with inverse probability of censoring weighted (IPCW) log-rank tests. Biometrics. 2000;56:779–788. doi: 10.1111/j.0006-341x.2000.00779.x. [DOI] [PubMed] [Google Scholar]
- Saitz R. Clinical practice. Unhealthy alcohol use. N. Engl. J. Med. 2005;352:596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- Salmon-Ceron D, Lewden C, Morlat P, Bevilacqua S, Jougla E, Bonnet F, Heripret L, Costagliola D, May T, Chene G Mortality 2000 Study Group. Liver disease as a major cause of death among HIV infected patients: role of hepatitis C and B viruses and alcohol. J. Hepatol. 2005;42:799–805. doi: 10.1016/j.jhep.2005.01.022. [DOI] [PubMed] [Google Scholar]
- Schmitz N, Gariepy G, Smith KJ, Malla A, Boyer R, Strychar I, Lesage A, Wang J. Trajectories of self-rated health in people with diabetes: associations with functioning in a prospective community sample. PLoS One. 2013;8:e83088. doi: 10.1371/journal.pone.0083088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116:93–101. doi: 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- Skeer MR, Mimiaga MJ, Mayer KH, O'Cleirigh C, Covahey C, Safren SA. Patterns of substance use among a large urban cohort of HIV-infected men who have sex with men in primary care. AIDS Behav. 2012a;16:676–689. doi: 10.1007/s10461-011-9880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeer MR, Mimiaga MJ, Mayer KH, O'Cleirigh C, Safren SA. The effect of heavy alcohol use on HIV viremia detectability and CD4 count among a clinical cohort of HIV-infected men who have sex with men (MSM) Alcohol. Clin. Exp. Res. 2012b;36:140A. [Google Scholar]
- Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, Mills TC, Binson D, Coates TJ, Catania JA. Alcohol use, drug use and alcohol-related problems among men who have sex with men: the Urban Men's Health Study. Addiction. 2001;96:1589–1601. doi: 10.1046/j.1360-0443.2001.961115896.x. [DOI] [PubMed] [Google Scholar]
- Sullivan LE, Goulet JL, Justice AC, Fiellin DA. Alcohol consumption and depressive symptoms over time: a longitudinal study of patients with and without HIV infection. Drug Alcohol Depend. 2011;117:158–163. doi: 10.1016/j.drugalcdep.2011.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Management of Substance Use Disorders Working Group. Secondary VA/DoD Clinical Practice Guideline for Management of Substance Use Disorders (SUD) Washington, DC: Department of Veterans Affairs & The Department of Defense; 2009. VA/DoD Clinical Practice Guideline for Management of Substance Use Disorders (SUD) [Google Scholar]
- Thiede H, Valleroy LA, Mackellar DA, Celentano DD, Ford WL, Hagan H, Koblin BA, LaLota M, McFarland W, Shehan DA, Torian LV Young Men's Survey Study Group. Regional patterns and correlates of substance use among young men who have sex with men in 7 US urban areas. Am. J. Public Health. 2003;93:1915–1921. doi: 10.2105/ajph.93.11.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu K, Campbell NR, Chen ZL, Cauch-Dudek KJ, McAlister FA. Accuracy of administrative databases in identifying patients with hypertension. Open Med. 2007;1:e18–e26. [PMC free article] [PubMed] [Google Scholar]
- Wong CF, Kipke MD, Weiss G. Risk factors for alcohol use, frequent use, and binge drinking among young men who have sex with men. Addict. Behav. 2008;33:1012–1020. doi: 10.1016/j.addbeh.2008.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf-King SE, Neilands TB, Dilworth SE, Carrico AW, Johnson MO. Alcohol use and HIV disease management: the impact of individual and partner-level alcohol use among HIV-positive men who have sex with men. AIDS Care. 2014;26:702–708. doi: 10.1080/09540121.2013.855302. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.