Abstract
Burkholderia mallei are Gram-negative bacteria, responsible for the disease glanders. B. mallei has recently been classified as a Tier 1 agent owing to the fact that this bacterial species can be weaponised for aerosol release, has a high mortality rate and demonstrates multi-drug resistance. Furthermore, there is no licensed vaccine available against this pathogen. Lipopolysaccharide (LPS) has previously been identified as playing an important role in generating host protection against Burkholderia infection. In this study, we present gold nanoparticles (AuNPs) functionalised with a glycoconjugate vaccine against glanders. AuNPs were covalently coupled with one of three different protein carriers (TetHc, Hcp1 and FliC) followed by conjugation to LPS purified from a non-virulent clonal relative, B. thailandensis. Glycoconjugated LPS generated significantly higher antibody titres and compared with LPS alone. Further, they improved protection against a lethal inhalation challenge of B. mallei in the murine model of infection.
Keywords: Nanoparticles, glycoconjugate, glanders
1. Background
Bionanotechnology is an emerging field in which nano-sized materials are utilised to address biologically-relevant problems. The development of safe and effective vaccine delivery systems is an area where nanotechnology can provide new avenues of innovation. Studies into the use of nanoparticles for vaccine delivery have demonstrated great potential for improving vaccine efficacy, either by encapsulating antigens to improve their stability or promoting antigen-presentation by decorating antigens onto the nanoparticle surface (1–3). Gold nanoparticles (AuNPs), in particular, have generated a lot of interest due to their unique optical properties for imaging and site-directed release of drugs or antigens, as well as being non-toxic and biocompatible (4–7). Moreover, there are a number of established techniques for the fabrication of gold nanofibres (nanorods or nanotubes) and nanoparticles of various sizes with limited size dispersity (8). The versatility and structural diversity of gold nanomaterials allows for a variety of approaches towards their application in therapy, bio-sensing and diagnostics.
Glanders is one of the oldest known infectious diseases, having first being described in 350 BC by Aristotle (9). Glanders is caused by the non-motile, Gram-negative bacterium Burkholderia mallei, which usually infects equines whilst humans are considered accidental hosts. Furthermore, B. mallei has been identified by the CDC as a Category B Select Agent and has recently been included by the Federal Security Advisory Panel as a Tier 1 agent (10). Elevating B. mallei to a Tier 1 agent stems from the fact that this bacterial species: (i) can be weaponised for aerosol release; (ii) causes infection with a relatively low number of organisms; (iii) has a high mortality rate from inhalational infection and; (iv) lacks effective treatments and accurate diagnosis. Mortality rates for individuals with this disease vary significantly depending on the route of infection, but can be as high as 50% even with the correct antibiotic therapy (11). One factor contributing to this high mortality rate is the expression of lipopolysaccharide (LPS) on the outer membrane of the bacterium. The O-antigen moiety of LPS has been demonstrated to play an important role in bacterial resistance to hydrophobic antimicrobials as well as the bactericidal action of human serum (12–14). LPS is also an important antigen for generating protection against Burkholderia infection. For example, passive protection studies using monoclonal antibodies raised against B. mallei LPS O-antigen were shown to be protective against a lethal challenge of glanders in a murine model of infection (15). Immunisation with LPS purified from clonal relatives of B. mallei, B. thailandensis and B. pseudomallei, has been shown to protect mice against an intraperitoneal (16) or an aerosol challenge (17) with B. pseudomallei. Furthermore, immunological studies demonstrated structural similarity with LPS from these clonal relatives to B. mallei LPS suggesting a vaccine may be cross-protective (18). However, partial protection afforded by LPS is short-lived and the animals eventually succumb to infection. This is because LPS is a T-independent antigen, unable to induce long-term immunity (19). To induce a more favourable T-dependent response, polysaccharides can be conjugated to a protein carrier, which is subsequently presented on MHC I/II molecules for recognition by T cells. This has previously been shown with the Haemophilus influenzae type b (Hib) and meningococcal type C vaccines (20, 21).
The aim of this study was to improve the protection afforded by B. thailandensis E264 LPS by conjugating to a protein carrier. The protein carriers used included the Hc fragment (TetHc) of tetanus toxin (TeNT; produced by Clostridium tetani), which is the current choice of protein carrier for several licensed glycoconjugate vaccines (22–24). We also tested haemolysin co-regulated protein (Hcp1) which is produced by both B. mallei and B. pseudomallei, and flagellin (FliC) which is produced by B. pseudomallei but not by B. mallei, as carrier proteins. The glycoconjugates were covalently coupled onto the surface of AuNPs to evaluate their potential to generate a more favourable immune response.
2. Methods
2.1 Nanoparticle synthesis
AuNPs were synthesised using the Turkevich method (25). Briefly, 90 mL 1 mM Gold (III) chloride trihydrate (Sigma) was heated to 90 °C with stirring. Next, 10 ml 90 mM sodium citrate dihydrate (Sigma) was added. The colloidal solution was cooled to room temperature and stored in the dark. Particle characterisation was carried out using ultraviolet-visible spectroscopy and their diameters determined by transmission electron microscopy (TEM). Nanoparticle tracking analysis (NanoSight NS500) was used to determine the concentration of AuNPs.
2.2 Protein expression and purification
His-tagged recombinant TetHc was expressed in Escherichia coli BL21 (λDE3) containing plasmid pKS1, encoding the Hc fragment of TeNT, and cultured in Luria Bertani broth containing 50 μg/mL kanamycin (26). Cultures were grown to early log phase prior to induction with 1 mM isopropyl β-D-1-thiogalactopyranoside (IPTG) for 4 h at 37 °C, 250 rpm. Cultures were centrifuged at 14,000 × g for 20 min at 4 °C and the cell pellet and flocculant layer resuspended in 100 mL BugBuster® (Merck), 30 KU/μL lysozyme (Pierce), 25 U/μL benzonuclease (Merck) and 1 EDTA-free protease inhibitor tablet (Sigma) before incubating with gentle rolling at room temperature for 30 min. Insoluble cell debris were removed by centrifuging at 16,000 × g for 20 min at 4 °C and supernatant was added to a HisBind column (Novagen). The TetHc protein was desalted in a PD10 buffer exchange column (GE Healthcare) before concentrating in a Vivaspin 6 column (Sartorius) at 4,000 × g for 20 min at 4 °C. The resulting solution was collected and assayed for TetHc by SDS-PAGE, and Western blotting using a peroxidase conjugated anti-polyhistidine monoclonal antibody (mAb; Sigma).
An hcp1 coding sequence (BMAA0742; amino acid residues 1 – 169) was amplified by PCR from B. mallei ATCC 23344 genomic DNA. An fliC coding sequence (BPSL3319; amino acids 175 – 297) was amplified by PCR from B. pseudomallei K96243 genomic DNA. The amplified hcp1 gene was cloned in frame with a C-terminal 6 x His affinity tag (vector pET28a; Novagen). The amplified fliC gene was cloned with an N-terminal tag (vector pET15b; Novagen). E. coli (λDE3) Rosetta strains harbouring these constructs were cultured in Overnight Express instant TB medium (Novagen) and grown at 37 °C, 250 rpm for 18 – 20 h prior to harvesting by centrifugation: 8,000 × g for 15 min. Bacterial pellets were resuspended in 25 mL of Lysis buffer (50 mM NaH2PO4, 300 mM NaCl, 10 mM imidazole, pH 8.0) supplemented with EDTA-free protease inhibitor cocktail (Roche) and 1 mg/mL lysozyme (sigma). After 15 min on ice, bacteria were lysed by sonication using a Misonix 3000 sonicator with a flat tip probe (power level 3.5; 10 × 30 s pulses, 30 s delay). Cell lysates were centrifuged at 19,118 × g for 20 min and the supernatant added to 1 mL of washed Ni2+-NTA agarose resin (Qiagen). Samples were rotated at 4 °C for 1 h and the resin washed three times with wash buffer (Lysis buffer containing 25 mM imidazole) followed by centrifugation at 1,000 × g. Proteins were eluted with 750 μl of Elution buffer (Lysis buffer containing 250 mM imidazole) under gravity flow conditions through Poly-Prep chromatography columns (Bio-Rad). Eluted proteins were further purified by size exclusion chromatography using a Hiload 16/60 Superdex 200 preparatory grade column (GE Healthcare) connected to an ÄCTA FPLC (GE Healthcare). Running buffer was HEPES-buffered saline (10 mM HEPES, 150 mM NaCl, pH 7.4) used at a flow rate of 0.5 mL/min, 4 °C. Fractions containing protein were identified by SDS-PAGE and pooled prior to concentration with Amicon Ultra protein concentrators (Millipore). Protein concentrations were calculated using the BCA assay (Pierce) and confirmed by SDS-PAGE and Western blotting using a peroxidase conjugated anti-polyhistidine mAb (Sigma). Aliquots of proteins were stored at −80 °C.
2.2 LPS purification
LPS was extracted from Burkholderia thailandensis E264 using a modified hot-phenol extraction method (27). Briefly, bacterial cell pellets were lysed for 16 h at 4 °C using 15,000 U of lysozyme (Sigma) per mg of bacteria. DNase I (Promega) and RNase I (Promega) were added at 20 μg/mL each, stirred at room temperature for a further 16 h, prior to digestion with 50 μg/mL Proteinase K (Promega) for 6 h. An equal volume of 90% (w/v) aqueous phenol was added and the bacterial suspension heated to 70 °C for 30 min with vigorous stirring. The mixture was dialysed against dH2O for 3 days, with frequent changes, prior to lyophilisation. The dry material was subsequently digested with 50 μg/mL Proteinase K for 4 h at 45 °C and ultracentrifuged at 100,000 × g for 3 h. Gel-like pellets were resuspended in dH2O and lyophilised. The dry LPS was weighed, resuspended in dH2O, stored in aliquots at −80 °C. The quality of the purified LPS was verified using SDS-PAGE and silver-staining (Bio-Rad Silver Stain Plus kit).
2.3 Antigen coupling onto gold nanoparticles
Recombinant carrier proteins were immobilised onto AuNPs using carbodiimide chemistry. To an AuNP suspension, 0.1 mM 16-mercaptohexadecanoic acid (MHDA) was added followed by 0.1% (v/v) Triton® X-100 (Sigma) and incubated for 2 h at room temperature. The mixture was centrifuged at 13,000 × g for 10 min, the supernatant removed and the pellet re-suspended in phosphate buffered saline (PBS). N-(3-dimethylaminopropyl)-N′-ethylcarbodiimide hydrochloride (Sigma; EDC) and N-hydroxysuccinimide (NHS; Sigma), 0.15 mM and 0.6 mM, respectively, were added before further adding 20 μg/mL of carrier protein. The solution was incubated at room temperature for 2 h. Centrifugation was used to sediment the conjugated AuNPs which were resuspended in PBS.
To make a 1 mL solution of LPS coupled to AuNPs, 4.3 μL 40 mM EDC and 17.3 μL 10 mM NHS was added to 0.26 mg LPS in 50 mM MES buffer pH 5.5 and incubated at room temperature for 15 min. Following this, 10.9 μL 800 μM 6-maleimidocaproic acid hydrazide, trifluoroacetic acid salt (EMCH; Pierce) was added to the LPS solution and incubated at room temperature for a further 15 minutes. The pH of the LPS solution was adjusted to 7.0 using NaOH and left to incubate for an hour. Meanwhile, AuNPs coupled with a protein carrier of choice was suspended in 874.6 μL potassium phosphate buffer (pH 7.5) before adding 25.4 μL 250 mM S-acetylthioglycolic acid N-hydroxysuccinimide ester (SATA; Sigma) and incubating at room temperature for 60 minutes. Hydroxylamine and EDTA were then added to the AuNP solution to quench the reaction with SATA. LPS was centrifuged in a Vivaspin® 6 centrifugal concentrator (Sartorius) for 15 min at 3,220 × g and desalted into 5 mM EDTA in PBS pH 7. The AuNP solution was also centrifuged, at 13,366 × g for 10 minutes before resuspending into the LPS solution and incubating at room temperature for 4 h. The conjugation reaction was quenched with 5 mM N-ethylmaleimide; the nano-glycoconjugates were centrifuged and resuspended in PBS with or without 0.26% (w/v) alhydrogel.
2.4 Glycoconjugate quantification
Confirmation of nano-glycoconjugate formation was assessed by measuring the absorbance spectra using a UV-visible spectrometer (Bio-Rad 680 microplate reader) where a red-shift in λmax of AuNPs was indicative of coupling to the surface. A two-colour Western blot was also performed, where possible, using a rabbit polyclonal antibody (pAb) raised against TetHc and a mouse mAb against LPS before incubating with a goat secondary antibody raised against either rabbit or mouse, tagged with an infrared dye at 680 nm or 800 nm (LI-COR®), respectively. The two infrared channels could then be viewed simultaneously on an Odyssey® CLx imager. Protein concentrations were measured using the BCA assay. Conjugated protein was released from AuNPs by displacing the MHDA linker using 0.1 mM 11-mercapto-1-undecanol (MUD; Sigma) and incubating at room temperature for 4 h. The degree of AuNP separation was determined by measuring extinction at λmax of AuNPs (> 99.5%). A BCA assay was performed as before, using BSA as a standard.
A modified version of a phenol-sulphuric acid assay was performed to determine the concentration of LPS conjugated to AuNPs (28, 29). As previously described, the MHDA linker attached to the AuNP surface was displaced using MUD and the AuNPs removed by centrifugation. Next, 50 μL of cleaved LPS was added in triplicates to a 96-well micro-titre plate alongside a known concentration of LPS. To each sample, 150 μL concentrated H2SO4 was added followed by the rapid addition of 30 μL 5% (w/v) phenol. The plate was covered and carefully floated on a static water bath for 5 min at 90 °C before cooling to room temperature and reading on a micro-titre plate reader (Bio-Rad) at 490 nm.
2.5 Protection study
BALB/c female mice were purchased from Harlan Sprague Dawley, Inc. (Indianapolis, Indiana) and maintained in ABSL-2 or ABSL-3 laboratories. Animals were provided with rodent feed and water ad libitum and maintained on 12 h light cycle. All protocols were approved by the Animal Care and Use Committee of the University of Texas Medical Branch (protocol number 0503014) and carried out in accordance with the National Institutes of Health guidelines.
In the first immunisation study groups of 9 female 6 – 8 week old BALB/c mice were immunised three times at two-weekly intervals, receiving 0.05 mL per mouse by the intranasal (IN) route. Group 1 received AuNPs conjugated with 0.93 μg TetHc; group 2 received AuNPs conjugated with 0.93 μg TetHc and 0.93 μg LPS (TetHc-LPS); group 3 received AuNPs conjugated with 0.93 μg LPS; group 4 received 0.93 μg LPS and group 5 received PBS. All of the vaccine materials were formulated in PBS with 0.26% (w/v) alhydrogel. One week after the final boost, mice were bled from the lateral tail vein to obtain blood for antibody analysis. Three weeks after the final boost, the mice were challenged by the IN route with 2.27 × 105 CFU/50 μL (~3.5 × LD50 [expected was 3 × LD50]) of B. mallei strain ATCC 23344 (China 7).
In the second immunisation study, the same protocol as before was implemented with mice receiving 1.19 × 105 CFU/50 μL (~1.9 × LD50 [expected was 3 × LD50]) B. mallei strain ATCC 23344. The groups of mice were as follows: group 1 received AuNPs conjugated with 0.93 μg FliC and 0.93 μg LPS (FliC-LPS); group 2 received AuNPs conjugated with 0.93 μg Hcp1-antigen and 0.93 μg LPS (Hcp1-LPS); group 3 received AuNPs conjugated with 0.93 μg TetHc and 0.93 μg LPS (TetHc-LPS) and group 4 received PBS. All of the vaccine materials were formulated in PBS with 0.26% (w/v) alhydrogel. In both experiments, bacterial loads were determined in lungs and spleens of surviving animals.
In the third immunisation study the same protocol was followed as before, with mice receiving a higher dose of 4.2 × 105 CFU/50 μL (6.5 × LD50 [expected was 7 × LD50]) B. mallei strain ATCC 23344. The groups of mice were as follows: group 1 received AuNPs conjugated with 0.93 μg FliC and 0.93 μg LPS (FliC-LPS); group 2 received AuNPs conjugated with 0.93 μg Hcp1-antigen and 0.93 μg LPS (Hcp1-LPS); group 3 received AuNPs conjugated with 0.93 μg TetHc and 0.93 μg LPS (TetHc-LPS); group 4 received 0.93 μg LPS and group 5 received PBS. All of the vaccine materials were formulated in PBS with 0.26% (w/v) alhydrogel. In this study, a subset of mice was sacrificed 3 days post-infection to determine bacterial load in spleens and lungs during early stage of infection.
Mice were euthanized three weeks (first study) or five weeks (second study) after challenge with B. mallei. In the third study, mice were euthanized after 19 days to comply with Animal Research Committee regulations. In all the studies, blood was taken and spleens were removed.
2.6 Immunological analysis
Serum was collected from animals one week after the final boost and assayed for antibody isotypes and IgG subclasses by ELISA (30). Microtitre plate wells were incubated with 50 μL 5 μg/mL LPS overnight at 4 °C. The plate was washed with 0.05% (v/v) Tween 20 in TBS and wells blocked with 200 μL 3% (w/v) skimmed milk powder in TBS for 1 h at 37 °C before washing again with TBS/Tween. Serum samples were serially diluted from 1:100 to 1:12,800 in 1% (w/v) skimmed milk powder in TBS. Serum from mice given PBS plus alum was used as a negative control. The plate was incubated at 37 °C for 1 h before it was washed three times with TBS/Tween. An appropriate isotype or IgG subclass specific goat anti-mouse horseradish peroxidise conjugate was added to the wells at a dilution specified by the manufacturer (Abcam) followed by incubation at 37 °C for 1 h. The plate was washed a further three times with TBS/Tween before adding an ABTS substrate (Pierce). The absorbance from the wells was measured at 415 nm using a micro-titre plate reader. Antibody titres were defined as the lowest A450 value greater than three standard deviations above the mean absorbance of control wells. ELISA data is expressed as the geometric mean antigen-specific IgG antibody titre with a 95% confidence limit.
2.7 Statistical analysis
Statistical differences between mean values were calculated using an unpaired, two-tailed Student’s t-test or a one-way ANOVA with orthogonal contrast. A Mantel-Haenszel test was used to compare survival curve data. A p value of ≤ 0.05 was considered significant.
3. Results
3.1 Nano-glycoconjugate synthesis
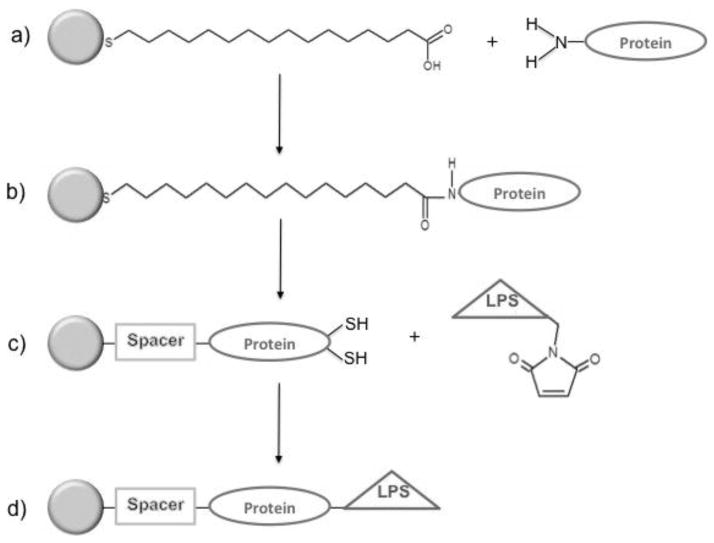
A citrate reduction of gold (III) chloride trihydrate was performed to generate near-monodisperse gold spheres, AuNPs, of approximately 15.6 ± 2.3 nm in diameter at 1.37 × 1012 particles/mL. Conjugation of protein antigens onto AuNPs was performed using carbodiimide coupling chemistry. LPS used in this study was purified from the lowly virulent B. thailandensis strain. Purified LPS was subsequently conjugated onto nanoparticle-immobilised protein carriers using thiol-maleimide coupling (Figure 1). Confirmation of nano-glycoconjugate synthesis was by measuring the absorbance spectra of AuNPs (Figure S1). An increase in the penetration depth of the AuNP plasmon, as indicated by red-shift in λmax of 9 nm from 532 nm for AuNP-TetHc to 541 nm, indicated an increase in the mean diameter of AuNP conjugates as a result of LPS conjugation. The extinction peak is also much broader for AuNP-TetHc-LPS, suggesting the size distribution of particles is much larger. This is likely to be due to variable lengths of the repeating O-antigen disaccharide on the particles. A two-colour Western blot was used to demonstrate the presence of both antigens and the retention of antigenicity after chemical conjugation (Figure S2). Using a phenol-sulphuric acid assay and nanoparticle tracking analysis, the amount of LPS measured on nano-glycoconjugates was determined to be approximately 6 molecules of LPS/NP.
Figure 1.
Glycoconjugate coupling chemistry to AuNPs. MHDA was added to a solution of AuNPs, forming a gold-thiol bond to generate a self-assembled monolayer (A). A protein carrier was coupled to the terminal carboxyl group of MHDA (spacer) using carbodiimide chemistry (B). Maleimide-modified LPS was conjugated onto the protein carrier using thiol maleimide coupling (C). AuNP-coupled glycoconjugate (D).
3.2 Immunoanalysis
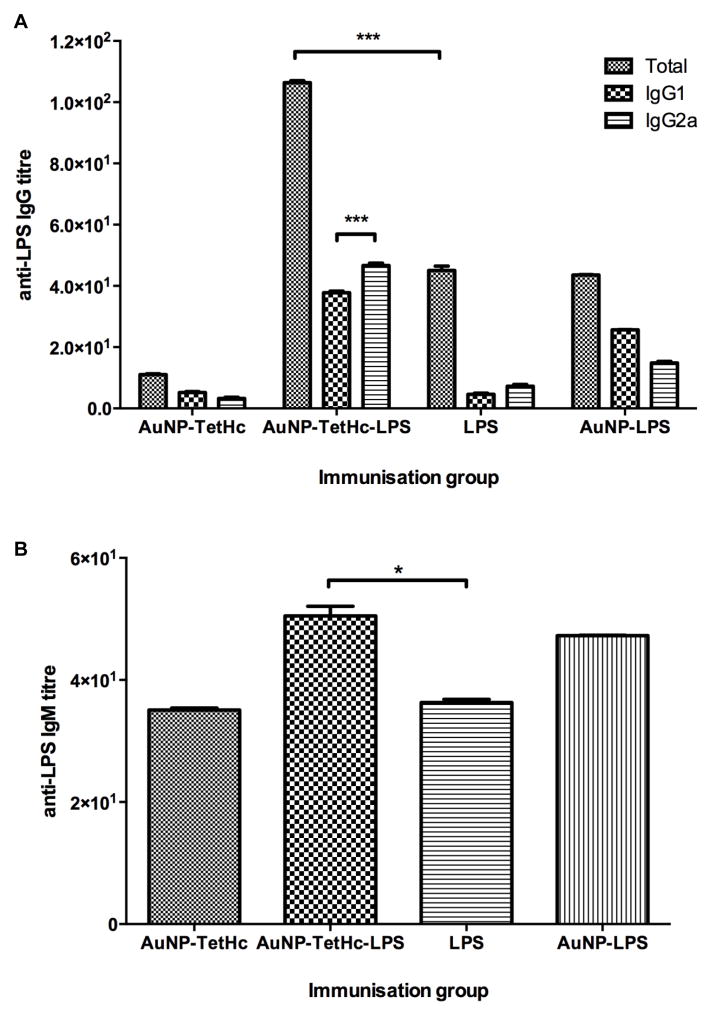
An immunisation and protection study was designed to evaluate the protective efficacy of nano-glycoconjugated LPS compared with free LPS. Groups of BALB/c mice were immunised with either LPS or TetHc-LPS coupled onto AuNPs. Control groups consisting of TetHc conjugated to AuNPs and AuNPs-LPS were also used. Antibody titres were measured one week after the final boost (five weeks post first immunisation) by ELISA. Animals immunised with AuNP-TetHc-LPS generated the highest LPS-specific IgG response, which was significantly higher than those immunised with LPS alone (p < 0.001; Figure 2A). IgG subclasses 1 and 2a were measured as determinants for the type of immune response induced. Mice immunised with AuNP-TetHc-LPS generated an IgG2a dominant response, accounting for almost half of the total IgG. In mice immunised with LPS alone, IgG1 and 2a titres accounted for approximately a third of the total IgG and there was no significant differences between the two isotype titres. Further investigation into the isotype profile of LPS immunised mice revealed that IgG3 is the dominant isotype present (Figure S3). Since LPS is a T-independent antigen, IgM responses were also measured (Figure 2B). Mice immunised with AuNP-TetHc-LPS generated the greatest IgM response, which was significantly higher than those given LPS alone (p < 0.05).
Figure 2.
LPS-specific IgG and IgG subclasses (A) and IgM titres (B) in sera collected from groups of eight mice, five weeks after the first immunisation with the antigen indicated and determined using ELISA. Error bars are calculated using the standard error of the mean. * p < 0.05, *** p < 0.001.
3.3 Protection study
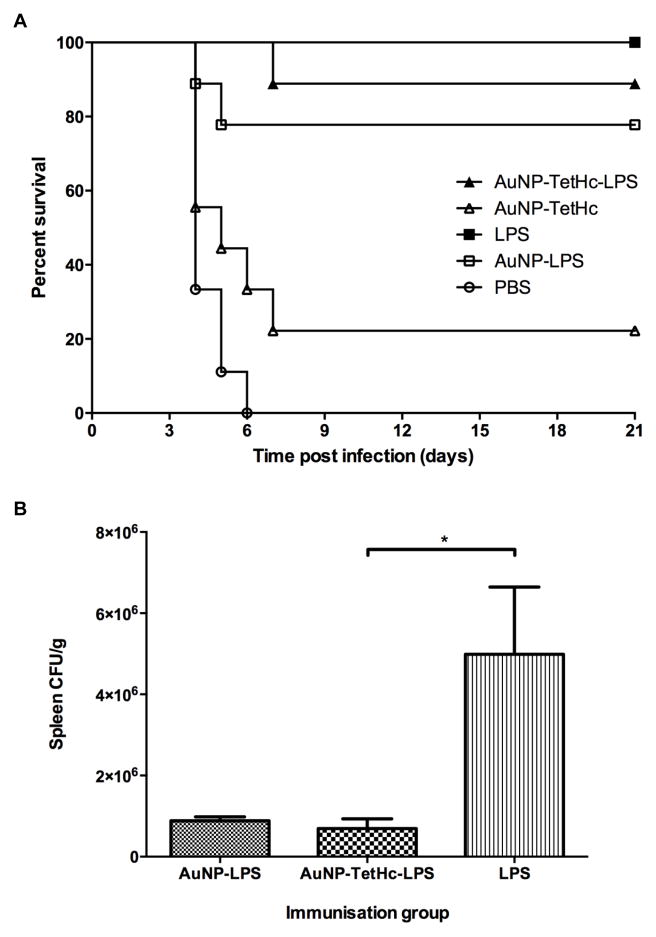
Three weeks after the final immunisation boost, mice were challenged IN with 3.5 × LD50 B. mallei ATCC 23344 and the mean time to death recorded. The protection study was terminated after 21 days, at which point the LPS-immunised mice demonstrated the highest level of survival (100%) (Figure 3A). There was no significant difference between the survival of mice immunised with LPS, AuNP-LPS or AuNP-TetHc-LPS. The colony counts in the spleens of challenged mice were significantly lower in mice that had been immunised with AuNP-TetHc-LPS or AuNP-LPS than in mice immunised with LPS alone (p < 0.05; Figure 3B). The bacterial loads in the lungs in mice were also measured (range 1.1×102 to 4.9×102 CFU / g). There was no significant difference in the lung burdens of B. mallei between any of the groups (data not shown).
Figure 3.
Survival curve for groups of 9 BALB/c mice challenged IN with 3 × LD50 B. mallei ATCC 23344, five weeks post-first IN immunisation with 3 × 50 μL doses of LPS or AuNP-TetHc-LPS (A). Colony counts of B. mallei in spleens three weeks post challenge. Each point is the mean of values from five mice. Error bars represent the standard error of the mean; asterisks indicate significant differences (p < 0.05) (B).
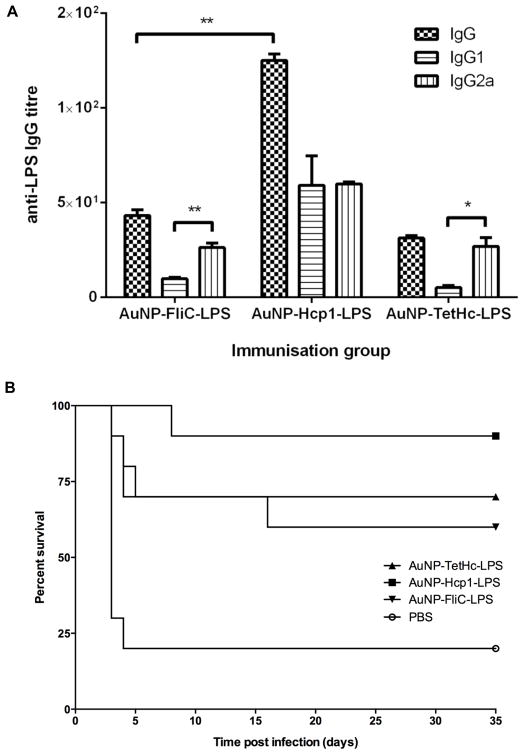
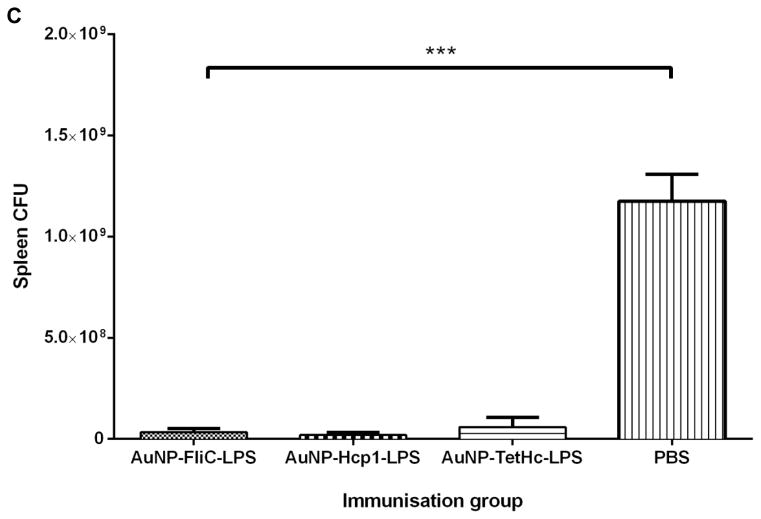
A second immunisation study was carried out to determine whether the efficacy of a glycoconjugate vaccine was influenced by the protein carrier and could extend the protection against B. mallei. Two additional protein carriers were included; Hcp1 and FliC. The LPS and AuNP-LPS groups were not included in this experiment because our previous study had shown that the glycoconjugate groups outperformed them. Antibody titres were measured as before and showed that animals immunised with AuNP-Hcp1-LPS generated a significantly higher IgG titre than mice immunised with AuNP-FliC-LPS or AuNP-TetHc-LPS (p < 0.01) (Figure 4A). Mice immunised with AuNP-FliC-LPS or AuNP-TetHc-LPS generated an IgG2a dominant immune response (p < 0.01 and p < 0.05, respectively). Three weeks after the final immunisation boost, mice were challenged IN with 1.9 × LD50 of B. mallei and their mean time to death was recorded. The protection study was terminated after 35 days, at which point AuNP-Hcp1-LPS immunised mice demonstrated the highest level of survival (90%; Figure 4B). However, there was no significant difference in survival between any of the nano-glycoconjugate immunised mice. There was a 20% survival rate from PBS immunised mice, however this was statistically lower than the three treatment groups (p < 0.01). Colony counts taken from the spleens of challenged mice were significantly reduced in mice immunised with nano-glycoconjugates compared with PBS (p < 0.05; Figure 4C).
Figure 4.
LPS specific IgG and IgG subclass titres in sera collected from groups of eight mice, five weeks post-first immunisation with the antigen indicated and determined using ELISA (A). Survival curve for groups of 9 BALB/c mice challenged IN with 2.62 × LD50 B. mallei China7, 3 weeks post-last IN immunisation with 3 × 50 μL doses of AuNP-FliC-LPS, AuNP-Hcp1-LPS or AuNP-TetHc-LPS (B). Colony counts of B. mallei in spleens three days post challenge. Each point is the mean of values from five mice. (C). Error bars are calculated using the standard error of the mean. * p < 0.05, ** p < 0.01.
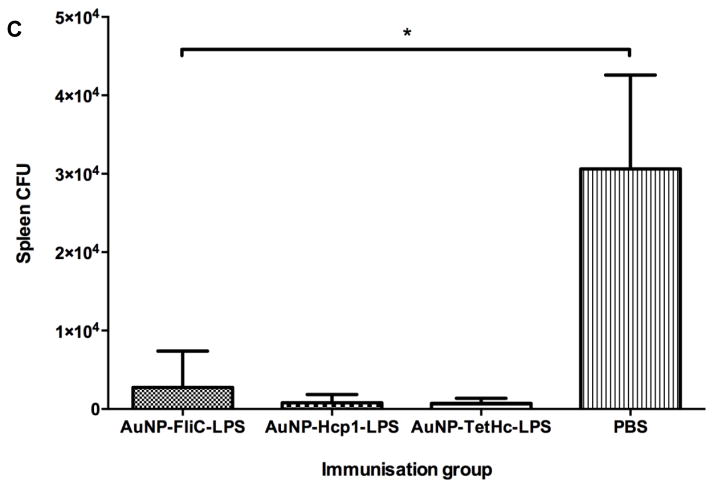
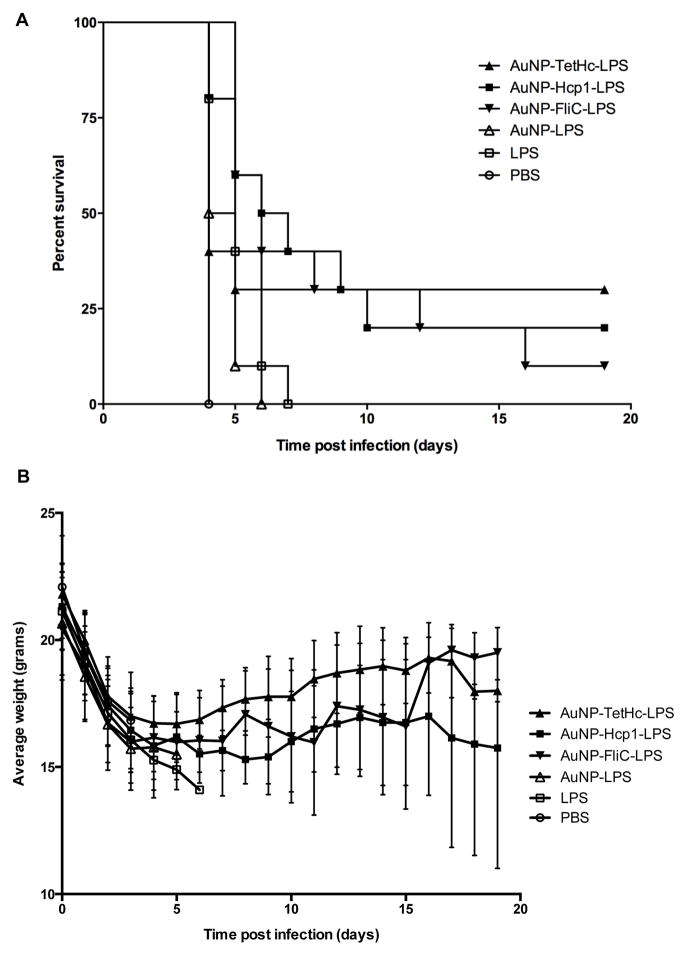
A final study was carried out to determine whether the glycoconjugate vaccines tested in the previous study could provide protection against a higher challenge dose. The immunisation procedure was repeated as before and three weeks after the final boost mice were challenged with 6.5 × LD50 of B. mallei and their mean time to death was recorded. The protection study was terminated after 19 days, at which point the only survivors were mice that had been immunised with AuNP-FliC-LPS, AuNP-Hcp1-LPS or AuNP-TetHc-LPS (Figure 5A). The survival times of mice immunised with the AuNP-glycoconjugates were significantly longer than the survival times of mice immunised with LPS or AuNP-LPS (p < 0.05). However, there was no significant difference in the survival times of mice in the three glycoconjugate immunisation groups. As with the first study, there was no significant difference in protection between mice immunised with LPS or AuNP-LPS. Body mass measurements of infected mice were also recorded which initially shows a sharp decline for all groups (Figure 5B). However, mice that were able to survive 7 days post infection showed a significant increase in body mass. Colony counts were also determined from 5 additional mice per group 3 days post-infection in the spleens and lungs. Bacterial loads of challenged mice that had been immunised with nano-glycoconjugates were significantly lower than those from the spleens of mice that had been dosed with PBS only (p < 0.001; Figure 5C)
Figure 5.
Survival curve for groups of 9 BALB/c mice challenged IN with 7 × LD50 B. mallei China7, 3 weeks post-last IN immunisation with 3 × 50 μL doses of AuNP-FliC-LPS, AuNP-Hcp1-LPS, AuNP-TetHc-LPS or LPS alone (A). Body mass of immunised animals during the course of infection. Only AuNP-glycoconjugate immunised mice survived past day 7 (B). Colony counts of B. mallei in spleens three days post challenge. Each point is the mean of values from five mice. (C). Error bars represent the standard error of the mean; asterisks indicate significant differences (p < 0.001)
4. Discussion
One of the major pitfalls in designing glycoconjugate vaccines is the poor efficiency associated with the bio-conjugation chemistry. In this study, AuNPs were used as a surface onto which the chemistry could be performed. Moreover, whilst reductive amination is traditionally used to couple polysaccharides onto protein carriers, this requires alkaline conditions owing to the high pKa of the ε amino group on lysine residues. This method of coupling is not only slow and inefficient, typically taking several days, but also forms reversible Schiff bases which require reduction to stabilise the linkage formed (31, 32). A borohydride salt is often used as the reducing agent for this chemistry, which is not only toxic but can hydrolyse or deacylate pH sensitive polysaccharides, such as the capsule from Neisseria meningitidis A, reducing the display of protective epitopes (31). We found that thiol-maleimide coupling chemistry could be used to couple B. thailandensis LPS onto a range of protein carriers to generate nano-glycoconjugates, which were then tested both for their abilities to induce antibody responses in mice and to provide protection against experimental glanders.
The evidence is that B. mallei is a clonal derivative of B. pseudomallei (33) and these closely related pathogens share many surface antigens including LPS (33, 34). Both pathogens have similar facultative intracellular lifestyles, though B. mallei has a narrower host range (35). Previous workers have shown that antibody plays a major role in protection against experimental B. mallei and B. pseudomallei infection in mice (17, 36–41). In the case of human infection with B. pseudomallei there is also evidence that the level of IgG antibodies to LPS were significantly higher in patients who survived melioidosis compared to those who died, and also higher in patients with non-septic melioidosis compared to septic patients (42). Antibodies against LPS appear to be protective by promoting opsonisation-induced phagocytic killing of bacteria in vitro (36, 43). These studies in mouse models of disease also reveal that antibody-mediated protection is only effective against low challenge doses and one study showed a clear dependence of the level of protection on the level of antibody to LPS (38).
Previous studies have shown that monoclonal antibodies reactive with LPS, and belonging to subclasses IgG1, IgG2a, IgG2b or IgG3, are reported to provide protection against experimental B. mallei and B. pseudomallei infection (36–38, 41). These findings suggest that protection is not necessarily linked to the induction of one specific subclass of antibodies, though there are no reports of testing of the testing of IgM antibodies to LPS for protection. Our results show that immunisation with LPS linked to nanoparticles, or with LPS linked to a protein immobilised on AuNPs, increased the IgG1, IgG2a and IgM responses to LPS. The increased IgG1 and IgG2a responses were greatest in mice immunised with the nano-glycoconjugates. Since the coupling chemistry is selective for nucleophilic carbonyl groups in the LPS core region, this leaves the O-antigen and lipid A moieties exposed. Whilst the O-antigen provides epitopes for the development of antigen-specific antibodies, the lipid A region is a potent agonist for TLR4 and evokes a strong immune response from interaction with B memory cells (44). Additionally, the increased response from AuNP-TetHc-LPS may be due to the presentation of LPS in its coupled form and the high density of O-antigen epitopes localised on an AuNP surface compared with uncoupled LPS.
In the second immunisation study, two additional protein carriers were chosen alongside TetHc. The first was FliC, the major structural protein of Gram-negative flagella, which has been studied for its adjuvantal role in vaccine formulations (45, 46). While B. mallei strains are non-motile, FliC (flagellin) has a high affinity for TLR5, which plays a fundamental role in activating innate immunity (47, 48). Through the induction of cytokines and chemokines, flagellin increases the recruitment of B and T lymphocytes to draining lymph nodes resulting in enhanced activation of B cells and the generation of plasma and memory cells (49, 50). Additionally, sera raised against FliC provides partial protection against a lethal challenge of B. pseudomallei in a diabetic rat model (51). The second protein carrier was Hcp1, which is member of a family of haemolysin co-regulatory proteins (Hcp) that share homology to Vibrio cholerae Hcp (52). This family of proteins have been identified as interacting with valine-glycine repeat protein G (VgrG) to assemble into a structure which resembles the cell-penetrating needle of a bacteriophage tail (53). This molecular assembly, known as the type six secretion system (T6SS), uses Hcp proteins as both structural and secreted components in vivo as evidenced by sera from mice, horses and humans reacting with Hcp1 (54). The T6SS-1 protein Hcp1 has also been shown to provide significant protection against a lethal inhaled B. mallei and B. pseudomallei challenge in a murine model of infection (55).
The levels of the antibody responses, irrespective of subclass, that we have recorded can be related to the level of protection we have seen following challenge with B. mallei. At the lowest challenge dose tested, prior immunisation with LPS, AuNP-LPS or nano-glycoconjugates provided broadly similar levels of protection. At a higher challenge dose immunisation with LPS alone failed to provide any protection but protection was seen in mice which had been immunised with nano-glycoconjugates. Given that B. mallei is a facultative intracellular pathogen which can spread from cell-to-cell (35), it is likely that antibody is only able to protect against bacteria during the extracellular phase of infection. Antibody would therefore be expected to protect against the haematogenous spread of bacteria from the initial site of infection. This is consistent with our observation that bacterial loads in spleens were reduced in animals with the highest levels of antibodies to LPS. The inability to reduce the bacterial burden in the lungs may reflect the need to induce immunity at the lung mucosal surface to eliminate bacteria before they gain entry into cells. A previous study with a live attenuated mutant of B. pseudomallei has shown that protection against an IN challenge was dependent on IN immunisation (56). Others have found that dosing with killed cell vaccines by the IN route did not improve protection against an aerosol challenge (57). Additional work would be needed to determine whether protective immunity in the lungs could be achieved using alternate immunisation routes.
Thus, our results have shown that coupling a glycoconjugate vaccine derived from B. thailandensis LPS onto AuNPs can markedly increase both the levels of antibody and reduce the bacterial loads in spleens of mice subsequently challenged with B. mallei. Our data suggest that the protection elicited is mostly mediated by antibody against LPS. Our results also support the suggestions that antibodies against LPS and belonging to a range of subclasses plays a key role in protecting against B. mallei infection. They also indicate that protection can be enhanced by stimulating higher levels of antibody to LPS but suggest that it will be difficult to achieve sterile immunity against glanders using vaccines which rely on LPS as the major immunogen.
Supplementary Material
Acknowledgments
Funding: This work was supported by grants U54 AI057156 and U01 AI078008 from National Institute of Allergy and Infectious Diseases (NIAID)/NIH.
Footnotes
The contents are solely the responsibility of the authors and do not necessarily represent the official views of the RCE Programs office, NIAID, or NIH.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Prasad S, Cody V, Saucier-Sawyer J, Fadel T, Edelson R, Birchall M, et al. Optimization of Stability, Encapsulation, Release, and Cross-Priming of Tumor Antigen-Containing PLGA Nanoparticles. Pharmaceutical Research. 2012;29(9):2565–77. doi: 10.1007/s11095-012-0787-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zaric M, Lyubomska O, Touzelet O, Poux C, Al-Zahrani S, Fay F, et al. Skin Dendritic Cell Targeting via Microneedle Arrays Laden with Antigen-Encapsulated Poly-d,l-lactide-co-Glycolide Nanoparticles Induces Efficient Antitumor and Antiviral Immune Responses. ACS Nano. 2013;7(3):2042–55. doi: 10.1021/nn304235j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nembrini C, Stano A, Dane KY, Ballester M, van der Vlies AJ, Marsland BJ, et al. Nanoparticle conjugation of antigen enhances cytotoxic T-cell responses in pulmonary vaccination. Proc Natl Acad Sci U S A. 2011;108(44):E989–97. doi: 10.1073/pnas.1104264108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsoli M, Kuhn H, Brandau W, Esche H, Schmid G. Cellular uptake and toxicity of Au55 clusters. Small. 2005;1(8–9):841–4. doi: 10.1002/smll.200500104. [DOI] [PubMed] [Google Scholar]
- 5.Connor EE, Mwamuka J, Gole A, Murphy CJ, Wyatt MD. Gold nanoparticles are taken up by human cells but do not cause acute cytotoxicity. Small. 2005;1:325–7. doi: 10.1002/smll.200400093. [DOI] [PubMed] [Google Scholar]
- 6.Bhattacharya R, Mukherjee P. Biological properties of “naked” metal nanoparticles. Advanced Drug Delivery Reviews. 2008;60(11):1289–306. doi: 10.1016/j.addr.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 7.Li T, Guo L, Wang Z. Gold Nanoparticle-based Surface Enhanced Raman Scattering Spectroscopic Assay for the Detection of Protein–Protein Interactions. Analytical Sciences. 2008;24:907–10. doi: 10.2116/analsci.24.907. [DOI] [PubMed] [Google Scholar]
- 8.Schmid G. Large clusters and colloids. Metals in the embryonic state. Chemical Reviews. 1992;92(8):1709–27. [Google Scholar]
- 9.Wajanarogana S, Sonthayanon P, Wuthiekanun V, Panyim S, Simpson AJ, Tungpradabkul S. Stable marker on flagellin gene sequences related to arabinose non-assimilating pathogenic Burkholderia pseudomallei. Microbiology and Immunology. 1999;43(11):995–1001. doi: 10.1111/j.1348-0421.1999.tb01238.x. [DOI] [PubMed] [Google Scholar]
- 10.Korch G, Parham G. Services USDoAHaH, editor. Federal experts security advisory panel, recommendations concerning the select agent program. https://orise.orau.gov/emi/scapa/files/biosafety/fesap-recommendations-101102.pdf2011.
- 11.Whitlock GC, Mark Estes D, Torres AG. Glanders: off to the races with Burkholderia mallei. FEMS Microbiology Letters. 2007;277(2):115–22. doi: 10.1111/j.1574-6968.2007.00949.x. [DOI] [PubMed] [Google Scholar]
- 12.DeShazer D, Brett PJ, Woods DE. The type II O-antigenic polysaccharide moiety of Burkholderia pseudomallei lipopolysaccharide is required for serum resistance and virulence. Molecular Microbiology. 1998;30(5):1081–100. doi: 10.1046/j.1365-2958.1998.01139.x. [DOI] [PubMed] [Google Scholar]
- 13.Burtnick MN, Brett PJ, Woods DE. Molecular and physical characterization of Burkholderia mallei O antigens. J Bacteriol. 2002;184(3):849–52. doi: 10.1128/JB.184.3.849-852.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamad MA, Di Lorenzo F, Molinaro A, Valvano MA. Aminoarabinose is essential for lipopolysaccharide export and intrinsic antimicrobial peptide resistance in Burkholderia cenocepacia †. Molecular Microbiology. 2012;85(5):962–74. doi: 10.1111/j.1365-2958.2012.08154.x. [DOI] [PubMed] [Google Scholar]
- 15.Treviño SR, Permenter AR, England MJ, Parthasarathy N, Gibbs PH, Waag DM, et al. Monoclonal Antibodies Passively Protect BALB/c Mice against Burkholderia mallei Aerosol Challenge. Infect Immun. 2006;74(3):1958–61. doi: 10.1128/IAI.74.3.1958-1961.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ngugi SA, Ventura VV, Qazi O, Harding SV, Kitto GB, Estes DM, et al. Lipopolysaccharide from Burkholderia thailandensis E264 provides protection in a murine model of melioidosis. Vaccine. 2010;28(47):7551–5. doi: 10.1016/j.vaccine.2010.08.058. [DOI] [PubMed] [Google Scholar]
- 17.Nelson M, Prior JL, Lever MS, Jones HE, Atkins TP, Titball RW. Evaluation of lipopolysaccharide and capsular polysaccharide as subunit vaccines against experimental melioidosis. Journal of Medical Microbiology. 2004;53(12):1177–82. doi: 10.1099/jmm.0.45766-0. [DOI] [PubMed] [Google Scholar]
- 18.Qazi O, Prior JL, Judy BM, Whitlock GC, Kitto GB, Torres AG, et al. Sero-characterization of lipopolysaccharide from Burkholderia thailandensis. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2008;102 (Suppl 1):S58–60. doi: 10.1016/S0035-9203(08)70016-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ngugi SA, Ventura VV, Qazi O, Harding SV, Kitto GB, Estes DM, et al. Lipopolysaccharide from Burkholderia thailandensis E264 provides protection in a murine model of melioidosis. Vaccine. 2010;28(47):7551–5. doi: 10.1016/j.vaccine.2010.08.058. [DOI] [PubMed] [Google Scholar]
- 20.Makela PH. Conjugate vaccines--a breakthrough in vaccine development. Southeast Asian J Trop Med Public Health. 2003;34(2):249–53. [PubMed] [Google Scholar]
- 21.Kandil AA, Chan N, Klein M, Chong P. Chemical synthesis of Haemophilus influenzae glycopeptide conjugates. Glycoconjugate Journal. 1997;14:13–7. doi: 10.1023/a:1018500712733. [DOI] [PubMed] [Google Scholar]
- 22.Kaplan SL, Lauer BA, Ward MA, Wiedermann BL, Boyer KM, Dukes CM, et al. Immunogenicity and safety of Haemophilus influenzae type b-tetanus protein conjugate vaccine alone or mixed with diphtheria-tetanus-pertussis vaccine in infants. Journal of Pediatrics. 1994;124(2):323–7. doi: 10.1016/s0022-3476(94)70328-0. [DOI] [PubMed] [Google Scholar]
- 23.Robbins JB, Schneerson R. Polysaccharide-Protein Conjugates: A New Generation of Vaccines. Journal of Infectious Diseases. 1990;161(5):821–32. doi: 10.1093/infdis/161.5.821. [DOI] [PubMed] [Google Scholar]
- 24.Sigurdardottir ST, Vidarsson G, Gudnason T, Kjartansson S, Kristinsson KG, Jonsson S, et al. Immune responses of infants vaccinated with serotype 6B pneumococcal polysaccharide conjugated with tetanus toxoid. Pediatric Infectious Disease Journal. 1997;16(7):667–74. doi: 10.1097/00006454-199707000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Turkevich J, Stevenson PC, Hillier J. A study of the nucleation and growth processes in the synthesis of colloidal gold. Discuss Faraday Soc. 1951;11:55–75. [Google Scholar]
- 26.Sinha K, Box M, Lalli G, Schiavo G, Schneider H, Groves M, et al. Analysis of mutants of tetanus toxin HC fragment: ganglioside binding, cell binding and retrograde axonal transport properties. Molecular Microbiology. 2000;37(5):1041–51. doi: 10.1046/j.1365-2958.2000.02091.x. [DOI] [PubMed] [Google Scholar]
- 27.Chart H. Methods in practical laboratory bacteriology. CRC Press; 1994. [Google Scholar]
- 28.DuBois M, Gilles KA, Hamilton JK, Rebers PA, Smith F. Colorimetric Method for Determination of Sugars and Related Substances. Analytical Chemistry. 1956;28(3):350–6. [Google Scholar]
- 29.Masuko T, Minami A, Iwasaki N, Majima T, Nishimura S-I, Lee YC. Carbohydrate analysis by a phenol–sulfuric acid method in microplate format. Analytical Biochemistry. 2005;339(1):69–72. doi: 10.1016/j.ab.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 30.Williamson DE, Sharp GJE, Eley SM, Vesey PM, Pepper TC, Titball RW, et al. Local and systemic immune response a microencapsulated sub-unit vaccine to for plague. Vaccine. 1996;14:1613–9. doi: 10.1016/s0264-410x(96)00151-x. [DOI] [PubMed] [Google Scholar]
- 31.Lees A, Sen G, LopezAcosta A. Versatile and efficient synthesis of protein-polysaccharide conjugate vaccines using aminooxy reagents and oxime chemistry. Vaccine. 2006;24(6):716–29. doi: 10.1016/j.vaccine.2005.08.096. [DOI] [PubMed] [Google Scholar]
- 32.Gildersleeve JC, Oyelaran O, Simpson JT, Allred B. Improved Procedure for Direct Coupling of Carbohydrates to Proteins via Reductive Amination. Bioconjugate Chemistry. 2008;19(7):1485–90. doi: 10.1021/bc800153t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nierman WC, DeShazer D, Kim HS, Tettelin H, Nelson KE, Feldblyum T, et al. Structural flexibility in the Burkholderia mallei genome. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(39):14246–51. doi: 10.1073/pnas.0403306101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holden MTG, Titball RW, Peacock SJ, Cerdeno-Tarraga AM, Atkins T, Crossman LC, et al. Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(39):14240–5. doi: 10.1073/pnas.0403302101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Galyov EE, Brett PJ, DeShazer D. Molecular insights into Burkholderia pseudomallei and Burkholderia mallei pathogenesis. Annu Rev Microbiol. 2010;64:495–517. doi: 10.1146/annurev.micro.112408.134030. [DOI] [PubMed] [Google Scholar]
- 36.Zhang S, Feng SH, Li B, Kim HY, Rodriguez J, Tsai S, et al. In vitro and In vivo studies on monoclonal antibodies with prominent bactericidal activity against Burkholderia pseudomallei and Burkholderia mallei. Clin Vaccine Immunol. 2011;2011:30. doi: 10.1128/CVI.00533-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jones SM, Ellis JF, Russell P, Griffin KF, Oyston PC. Passive protection against Burkholderia pseudomallei infection in mice by monoclonal antibodies against capsular polysaccharide, lipopolysaccharide or proteins. J Med Microbiol. 2002;51:1055–62. doi: 10.1099/0022-1317-51-12-1055. [DOI] [PubMed] [Google Scholar]
- 38.AuCoin DP, Reed DE, Marlenee NL, Bowen RA, Thorkildson P, Judy BM, et al. - Polysaccharide specific monoclonal antibodies provide passive protection against intranasal challenge with Burkholderia pseudomallei. PLoS One. 2012;7(4):17. doi: 10.1371/journal.pone.0035386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nieves W, Asakrah S, Qazi O, Brown KA, Kurtz J, Aucoin DP, et al. A naturally derived outer-membrane vesicle vaccine protects against lethal pulmonary Burkholderia pseudomallei infection. Vaccine. 2011;29(46):8381–9. doi: 10.1016/j.vaccine.2011.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peddayelachagiri BV, Paul S, Makam SS, Urs RM, Kingston JJ, Tuteja U, et al. Functional characterization and evaluation of in vitro protective efficacy of murine monoclonal antibodies BURK24 and BURK37 against Burkholderia pseudomallei. PLoS One. 2014;9(3) doi: 10.1371/journal.pone.0090930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Trevino SR, Permenter AR, England MJ, Parthasarathy N, Gibbs PH, Waag DM, et al. Monoclonal antibodies passively protect BALB/c mice against Burkholderia mallei aerosol challenge. Infect Immun. 2006;74(3):1958–61. doi: 10.1128/IAI.74.3.1958-1961.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Charuchaimontri C, Suputtamongkol Y, Nilakul C, Chaowagul W, Chetchotisakd P, Lertpatanasuwan N, et al. Antilipopolysaccharide II: An antibody protective against fatal melioidosis. ClinInfectDis. 1999;29:813–8. doi: 10.1086/520441. [DOI] [PubMed] [Google Scholar]
- 43.Ho M, Schollaardt T, Smith M, Perry M, Brett P, Chaowagul W, et al. Specificity and functional activity of anti-Burkholderia pseudomallei polysaccharide antibodies. Infect Immun. 1997;65(9):3648–53. doi: 10.1128/iai.65.9.3648-3653.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.West TE, Ernst R, Jansson-Hutson M, Skerrett S. Activation of Toll-like receptors by Burkholderia pseudomallei. BMC Immunology. 2008;9(1):46. doi: 10.1186/1471-2172-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Honko AN, Sriranganathan N, Lees CJ, Mizel SB. Flagellin Is an effective adjuvant for immunization against lethal respiratory challenge with Yersinia pestis. Infect Immun. 2006;74(2):1113–20. doi: 10.1128/IAI.74.2.1113-1120.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Song L, Zhang Y, Yun NE, Poussard AL, Smith JN, Smith JK, et al. Superior efficacy of a recombinant flagellin:H5N1 HA globular head vaccine is determined by the placement of the globular head within flagellin. Vaccine. 2009;27(42):5875–84. doi: 10.1016/j.vaccine.2009.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith KD, Andersen-Nissen E, Hayashi F, Strobe K, Bergman MA, Barrett SL, et al. Toll-like receptor 5 recognizes a conserved site on flagellin required for protofilament formation and bacterial motility. Nature immunology. 2003;4(12):1247–53. doi: 10.1038/ni1011. [DOI] [PubMed] [Google Scholar]
- 48.McDermott PF, Ciacci-Woolwine F, Snipes JA, Mizel SB. High-Affinity Interaction between Gram-Negative Flagellin and a Cell Surface Polypeptide Results in Human Monocyte Activation. Infect Immun. 2000;68(10):5525–9. doi: 10.1128/iai.68.10.5525-5529.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bates JT, Honko AN, Graff AH, Kock ND, Mizel SB. Mucosal adjuvant activity of flagellin in aged mice. Mechanisms of Ageing and Development. 2008;129(5):271–81. doi: 10.1016/j.mad.2008.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gewirtz AT, Navas TA, Lyons S, Godowski PJ, Madara JL. Cutting edge: bacterial flagellin activates basolaterally expressed TLR5 to induce epithelial proinflammatory gene expression. Journal of immunology (Baltimore, Md: 1950) 2001;167(4):1882–5. doi: 10.4049/jimmunol.167.4.1882. [DOI] [PubMed] [Google Scholar]
- 51.Brett PJ, Mah DC, Woods DE. Isolation and characterization of Pseudomonas pseudomallei flagellin proteins. Infect Immun. 1994;62:1914– 9. doi: 10.1128/iai.62.5.1914-1919.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Williams SG, Varcoe LT, Attridge SR, Manning PA. Vibrio cholerae Hcp, a secreted protein coregulated with HlyA. Infect Immun. 1996;64(1):283–9. doi: 10.1128/iai.64.1.283-289.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pukatzki S, Ma AT, Revel AT, Sturtevant D, Mekalanos JJ. Type VI secretion system translocates a phage tail spike-like protein into target cells where it cross-links actin. Proc Natl Acad Sci U S A. 2007;104(39):15508–13. doi: 10.1073/pnas.0706532104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Galyov EE, Brett PJ, DeShazer D. Molecular insights into Burkholderia pseudomallei and Burkholderia mallei pathogenesis. Annual Review of Microbiology. 2010;64:495–517. doi: 10.1146/annurev.micro.112408.134030. [DOI] [PubMed] [Google Scholar]
- 55.Whitlock GC, Deeraksa A, Qazi O, Judy BM, Taylor K, Propst KL, et al. Protective response to subunit vaccination against intranasal Burkholderia mallei and B. pseudomallei challenge. Procedia in Vaccinology. 2010;2(1):73–7. doi: 10.1016/j.provac.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Easton A, Haque A, Chu K, Patel N, Lukaszewski RA, Krieg AM, et al. Combining Vaccination and Postexposure CpG Therapy Provides Optimal Protection Against Lethal Sepsis in a Biodefense Model of Human Melioidosis. Journal of Infectious Diseases. 2011;204(4):636–44. doi: 10.1093/infdis/jir301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sarkar-Tyson M, Smither SJ, Harding SV, Atkins TP, Titball RW. Protective efficacy of heat-inactivated B. thailandensis, B. mallei or B. pseudomallei against experimental melioidosis and glanders. Vaccine. 2009;27(33):4447–51. doi: 10.1016/j.vaccine.2009.05.040. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.