Abstract
Background
Ukraine is experiencing one of the most volatile HIV epidemics globally, fueled primarily by people who inject drugs (PWIDs), and a parallel incarceration epidemic. Opioid substitution therapy (OST) is internationally recognized as one of the most effective forms of treatment for opioid dependence and is among the most effective HIV prevention strategies available, yet efforts to adopt it in Ukraine’s Criminal Justice System (CJS) have been thwarted.
Methods
To understand the reluctance of the Ukrainian CJS to adopt OST despite the overwhelming evidence pointing to its health benefits and improved criminal justice outcomes, we conducted the first survey of Ukrainian prison administrative, medical and custodial staff (N=243) attitudes towards addiction in general, OST, and people living with HIV/AIDS (PLWHA) in representative regions of Ukraine.
Results
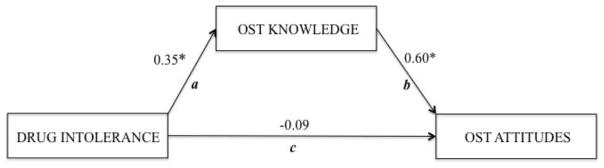
Results revealed that Ukrainian CJS workers’ attitudes toward OST, PLWHA, and drug addiction were universally negative, but differed substantially along geographic and occupational lines. Whereas geographic and cultural proximity to the European Union drove positive attitudes in the west, in the southern region we observed an identifiability effect, as workers who worked directly with prisoners held the most positive attitudes. We also found that knowledge mediated the effect of drug intolerance on OST attitudes.
Conclusion
In Ukraine, adoption of OST is more influenced by ideological biases and prejudices than by existing scientific evidence. By elucidating existing attitudes among CJS personnel, this assessment will help direct subsequent interventions to address the barriers to implementing evidence-based HIV prevention treatments.
Keywords: Attitudes, Prisons, Ukraine, Substance Abuse, opioid substitution therapy, methadone, buprenorphine, HIV/AIDS, healthcare providers
1. INTRODUCTION
HIV/AIDS incidence has decreased globally, but despite these encouraging trends, the epidemics in countries of the Former Soviet Union (FSU) in Eastern Europe and Central Asia continue to expand (Joint United Nations Programme on HIV/AIDS, 2014, UNAIDS, 2013). Ukraine is experiencing one of the most volatile HIV epidemics in the world, with an estimated 230,000 people living with HIV/AIDS (PLWHA), fueled primarily by people who inject drugs (PWIDs), although there is emerging evidence for a transition to the general population (Azbel et al., 2013; Bojko et al., 2013a; Joint United Nations Programme on HIV/AIDS (UNAIDS, 2014).
Opioid substitution therapy (OST) is one of the most effective and cost-effective strategies for curbing HIV transmission (Alistar et al., 2011) in community settings as well as in prisons (Stallwitz and Stover, 2007; Stover et al., 2006), resulting in reduced rates of drug use, infectious disease transmission, criminal activity, and recidivism (Altice et al., 2010). Community-based OST (first with buprenorphine and then with methadone) has been available in Ukraine for more than a decade. Expansion of OST, however, has been limited among the estimated 310,000 PWIDs and appears to differ regionally (Zaller et al., 2014). Efforts to improve entry and retention in OST have been thwarted by negative attitudes toward PWIDs, lack of knowledge about HIV and addiction treatment, and absence of integrated care (Degenhardt et al., 2013; Wolfe et al., 2010; Zaller et al., 2014). Furthermore, despite 2011 legislation allowing it, OST has not yet been introduced into the Ukrainian criminal justice system (CJS) despite evidence of its benefit to reduce the negative consequences of drug injection within prison (Larney et al., 2012), and to improve transitional care post-release (Kinlock et al., 2009; Springer et al., 2012). With almost 138,000 prisoners (305 prisoners per 100,000 population) in Ukraine (Walmsley, 2014), of which 48.7% are estimated to be PWIDs, HIV/AIDS and other infectious diseases are concentrated within Ukraine’s prisons (Azbel et al., 2013, 2014). As prisoners cycle in and out of criminal justice settings (CJS), access to and retention in treatment is disrupted (Maru et al., 2007). Without reentry initiatives to provide continuity of care upon release, prisoners are especially vulnerable to substantial risks including relapse to drug use, overdose, and death (Binswanger et al., 2013, 2007). In the absence of adequate alternatives to incarceration for PWIDs, the CJS serves as a sentinel place for screening and the initiation of disease prevention and treatment measures for a population that is otherwise missed by public health systems (DeBell and Carter, 2005; Flanigan et al., 2010; Izenberg and Altice, 2010).
The few published studies on the health status of prisoners in countries of the FSU, and Ukraine in particular, report on the burden of infectious diseases (Azbel et al., 2013, 2014) and numerous patient-centered barriers to adequate care and community reentry (Morozova et al., 2013). A review of substance use disorders and HIV in prisons available from government sources in Central Asia strongly suggests that the existing estimates of drug abuse and infectious diseases remain markedly under-reported (Vagenas et al., 2013). Research initiatives adhering to international standards in Ukraine are hampered by logistical, financial, and political constraints, as well as by skepticism toward change and concerns about transparency on the part of the CJS officials (UNODC, 2012).
It is well-documented that healthcare providers’ (Lev-Ran et al., 2013; Talal et al., 2013; Tracy et al., 2009) and prison personnel’s (Caplehorn et al., 1998; Springer and Bruce, 2008b; Stover et al., 2006) attitudes contribute to the quality of the care that patients ultimately receive. Globally and historically, treatment for opioid dependence has been more influenced by moral biases and prejudices than by scientific evidence (Torrens et al., 2013). In many settings, including high-income countries where OST is accepted in community settings, its extension to CJS remains controversial (Larney and Dolan, 2009). The opposition to OST is unsubstantiated, as research shows that commonly expressed concerns regarding the introduction of OST by prison administrators, such as drug diversion, security, and violent behaviors, disappear after the programs are implemented (Jurgens et al., 2011; Magura et al., 2009). Nevertheless, despite the explicit recommendation by WHO, UNODC, and UNAIDS (2007) to CJS authorities to urgently introduce and expand OST programs, negative attitudes toward and stigma against OST have persistently impeded its adoption in prison systems around the world.
This is particularly true in Ukraine’s neighboring Russia and in some FSU countries where OST is explicitly forbidden (Bojko et al., 2013b; Cohen, 2010; Samet, 2011). OST remains unavailable in Ukraine’s CJS despite legislation that does not restrict its introduction (Izenberg et al., 2013). Recent policies mandate provision of OST in pre-trial detention centers to ensure continuity of addiction treatment, yet OST introduction has been hampered by multi-level organizational constraints that conspire to sabotage or delay it.
To better understand the reluctance of the Ukrainian CJS to introduce OST despite new laws promoting it, alongside the overwhelming evidence supporting its health benefits and improved criminal justice outcomes (Amato et al., 2005; Kermode et al., 2011), it is crucial to assess the prison personnel’s attitudes towards OST. As there are virtually no data on prison staff attitudes and knowledge about OST in Ukraine, we conducted the first survey of Ukrainian prison administrative, medical and custodial staff attitudes towards addiction in general, OST, and PLWHA in four distinct regions of Ukraine. Findings from this assessment are intended to elucidate lingering biases and help direct future educational training programs and organizational interventions to address the barriers to implementing evidence-based HIV prevention treatments in FSU prison systems.
2. MATERIALS AND METHODS
2.1 Setting
Ukraine is Europe’s second largest and seventh most populous country of 45 million, with diverse regional cultures and identities (Malik, 2013). To define the country’s regions, we employ the standard four-region approach (Arel, 1995; Kubicek, 2000; Zaller et al., 2014) that divides the country into west, east, north/center, and south. Ukraine first introduced OST with buprenorphine in 2004 (Bruce et al., 2007), followed by methadone’s introduction in 2007 (Lawrinson et al., 2008), which has since become the primary OST due to cost. Although OST reduces HIV risk behaviors (Altice et al., 2006; Metzger et al., 1993), increases ART access (Altice et al., 2011; Lucas et al., 2010; Uhlmann et al., 2010) and improves retention in HIV care and HIV treatment outcomes (Altice et al., 2011; Palepu et al., 2006), OST coverage in Ukraine remains inadequate, with only 2.6% of the estimated 310,000 PWIDs receiving treatment (Degenhardt et al., 2013; WHO, 2013; Zaller et al., 2014).
2.2 Recruitment and participants
As part of a nationally representative prisoner health survey, three medium-security prison facilities were chosen in each of Ukraine’s four regions for a total of 12 facilities (Azbel et al., 2013). In each region, the 3 facilities were comprised of a first-time and a recidivist offender men’s prison as well as a women’s prison, representing the three types of non-specialized prison facilities in Ukraine. Trained research assistants approached all daytime prison personnel, the ones who would be primarily involved in OST delivery, and encouraged them to anonymously complete a brief pen and paper survey after providing informed consent; only three personnel refused participation.
2.3 Definitions
Due to confidentiality constraints, personal identifiers, such as age and gender, were not included. Region was decided a priori based on the city region (oblast’), where the study participant worked: east (Donetsk); west (Lviv); north (Kiev) and south (Odessa). Personnel position was defined by one of four categories: medical administration; custodial administration; medical staff; and custodial staff. Medical and custodial personnel were those members who worked directly with inmates on a daily basis. The amount of experience working in the CJS was included and categorized as: 1) <1 year; 2) 1–5 years; 3) 6–10 years; 4) 11–15 years; 5) 16–20 years; and 6) >20 years.
2.4 Measures
Knowledge about and attitudes toward OST was derived from a 16-item survey (Springer and Bruce, 2008a), which uses a five-point Likert-type response where higher numbers reflect more positive attitudes. Principal component analysis with Varimax rotation suggested a two-factor solution for 16 items. The first factor consisted of 6 items (α=0.90), which collectively measured an individual’s favorable attitudes toward OST (OST attitudes). An example of a statement reflecting such attitudes is “OST services should be available in the community so that all people who suffer from opioid addiction and want substitution therapy can receive it.” The second factor (OST knowledge) used four items that measured an individual’s knowledge about the positive effects of OST on other health outcomes (α=0.89). An example of a knowledge item is “OST improves adherence to HIV medications in HIV-infected, opioid dependent individuals.”
To measure an individual’s intolerance toward PLWHA (PLWHA intolerance, α=0.72), we used the five-items Likert-type Attitudes Toward AIDS Scale (Goh et al., 1996), with increasing scores indicating higher intolerance. An example of a statement used in the scale is “I have little sympathy for people who get AIDS from sexual promiscuity.”
Tough mindedness about and intolerance toward drugs and drug users (Drug intolerance, α =0.76) was measured using seven Likert-type items (UNAIDS/WHO, 2006) with higher scores indicating more intolerance (e.g., “modern society is too tolerant towards drug addicts”). Finally, we asked the respondents how effective they perceived different methods of treating drug addiction to be (0=not effective and 1=effective). Specifically, the respondents were asked to rate the perceived effectiveness of each of the following addiction treatment modality: religion, incarceration, OST, folk medicine, addiction treatment without OST (primarily counseling), and detox (cold turkey).
2.5 Hypotheses
Because the surveyed population is from a nationally representative sample of prison personnel, representing diverse prison occupations and all regions and facility types in Ukraine, we proposed the following hypotheses pertaining specifically to the effects of region and occupation on relevant attitudinal outcomes:
Regional differences: HIV prevalence and drug use in Ukraine have been shown to differ geographically in prisons (Azbel et al., 2013) and communities (Zaller et al., 2014), and we expected to see regional differences in attitudes, especially between west and east—the regions that have been shown to substantially differ across a multitude of socio-cultural domains (Barrington and Faranda, 2009).
Occupational differences: We hypothesized that attitudes toward OST, PLWHA, and drug dependence will differ across occupational positions held by prison staff. Specifically, we hypothesized that medical workers, due to their educational focus on promoting improved health, are likely to hold more positive attitudes relative to non-medical workers. Similarly, staff members working directly with prisoners, due to their day-to-day involvement and identifiability with the client (Small and Loewenstein, 2003a), will hold more positive attitudes relative to administrative personnel who have virtually no direct contact. Identifiability evolves from the observation that people are more sympathetic and hence generous in attitude toward “specific” identified victims than toward “statistical” victims (i.e., abstract persons who are depicted solely through reports or data) who are yet to be identified (Schelling, 1968).
2.6 Analytic Plan
A multivariate general linear model (GLM) on SPSS version19 was used to examine multivariate relationships among variables and to address the research hypotheses with Turkey’s HSD post-hoc analysis that adjusts for multiple pairwise comparisons. Below we report the effects of independent variables by region and occupation, as well as their interaction for each of the dependent variables: (1) attitudes toward and (2) knowledge about OST; and intolerance toward (3) PLWHA and (4) drug addiction. The structural equation modeling program AMOS.22 was utilized to perform a bootstrapping indirect effects procedure.
3. RESULTS
3.1 Attitudes towards and knowledge about opioid substitution therapy
To investigate the variation in attitudes toward and knowledge about OST, we ran a multivariate GLM with OST attitudes and OST knowledge as dependent variables; region (east, west, south, north), and occupation (medical administration, custodial administration, medical staff, and custodial staff) as fixed factors; and experience in the field as a covariate. The Wilks Lambda multivariate test of overall differences among groups was significant (F(2, 220)=204, p<0.01; η2=0.65). The variance in the outcome variables explained by the analysis was 12% for OST attitudes and 20% for OST knowledge.
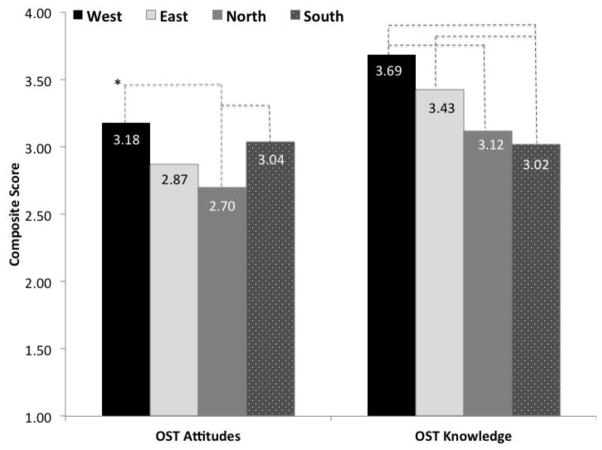
The analysis produced main effects for geographic region on OST attitudes (F=4.81, p<0.01; η2=0.06, see Figure 1), suggesting that prison personnel from western and southern Ukraine held more positive attitudes toward OST relative to CJS workers in the north; and on OST knowledge (F=3.17, p=0.02; η2=0.05,) reflecting the highest knowledge in the west and the lowest knowledge in the south.
Figure 1.
Geographic Region Effects on OST Attitudes and OST Knowledge.
*Connector lines indicate a statistically significant difference at p<0.05.
OST=opioid substitution therapy
There was no main effect for occupation for either of the two outcomes, but there was a significant region*occupation interaction effect on OST knowledge (F=2.48, p=0.01; η2=0.09). Planned pair-wise comparisons for the differences within geographic region, revealed the significantly different knowledge scores among CJS workers in the south, where administrative personnel (medical and custodial) possessed higher knowledge than staff working directly with prisoners (Table 1). Pair-wise comparisons for the differences within prison occupation revealed a rather complex interaction pattern, with geographic differences for each of the four occupation categories (Table 2). Results indicate that medical and custodial administrators from the west and south had higher knowledge than their counterparts in the north; however medical and custodial staff members from the south have reported the lowest knowledge scores. The experience covariate was not significant for OST attitudes (F=1.69, p=0.19), but was significant for OST knowledge (F=7.54, p<0.01; η2=0.04), showing that more years in the field led to higher knowledge about OST.
Table 1.
Mean Difference Pairwise Comparisons For Prison Personnel Position within Regions
| Variable | Region | Personnel Position | Medical Administration | Custodial Administratio | Medical Staff |
|---|---|---|---|---|---|
|
| |||||
| Opioid substitution therapy knowledge (OST knowledge) | South | Custodial Administration | .58a | ||
| Medical Staff | 1.49** | .91** | |||
| Custodial Staff | 1.30** | .72** | −.19 | ||
|
| |||||
| Intolerance toward people living with HIV/AIDS (PLWHA intolerance) | West | Custodial Administration | −1.26** | ||
| Medical Staff | −1.04* | .23 | |||
| Custodial Staff | −1.25** | .01 | −.21 | ||
|
| |||||
| East | Custodial Administration | −.50 | |||
| Medical Staff | −.30 | .20 | |||
| Custodial Staff | −1.03** | −.53* | −.73* | ||
|
| |||||
| South | Custodial Administration | .45 | |||
| Medical Staff | 1.11** | .66* | |||
| Custodial Staff | .61 | .17 | −.49* | ||
|
| |||||
| Intolerance toward drug addiction (Drug intolerance) | East | Custodial Administration | .65* | ||
| Medical Staff | .76* | .10 | |||
| Custodial Staff | .41 | −.24 | −.34 | ||
Mean difference = column – row.
p < .05;
p < .01
Table 2.
Mean Difference Pairwise Comparisons for Region within Prison Personnel Positions
| Variable | Personnel Position | Region | West Administratio | East Administratio | North Administratio |
|---|---|---|---|---|---|
|
| |||||
| Opioid substitution therapy knowledge (OST knowledge) | Medical Administration | East | .86a | ||
| North | 1.08** | .22 | |||
| South | −.10 | −.96 | −1.19** | ||
|
| |||||
| Custodial Administration | East | .20 | |||
| North | .50* | .30 | |||
| South | −.03 | −.23 | −.53* | ||
|
| |||||
| Medical Staff | East | .28 | |||
| North | −.04 | −.31 | |||
| South | 1.04** | .75 | 1.07** | ||
|
| |||||
| Custodial Staff | East | .11 | |||
| North | .50* | .38 | |||
| South | .76** | .64** | .26 | ||
|
| |||||
| Intolerance toward people living with HIV/AIDS (PLWHA intolerance) | Medical Administration | East | −.95* | ||
| North | −.1.75** | −.80* | |||
| South | −1.68** | −.73 | .07 | ||
|
| |||||
| Custodial Staff | East | −.73** | |||
| North | −.02 | .71** | |||
| South | .18 | .91** | .20 | ||
|
| |||||
| Intolerance toward drug addiction (Drug intolerance) | Medical Staff | East | −.38 | ||
| North | −.34 | .04 | |||
| South | .70** | 1.08** | 1.04** | ||
|
| |||||
| Custodial Staff | East | −.40* | |||
| North | −.22 | .18 | |||
| South | .25 | .65** | .47** | ||
Mean difference = column – row.
p < .05;
p < .01
3.2 Intolerance toward PLWHA and Drug Addiction
We ran a multivariate GLM with Drug intolerance and PLWHA intolerance as dependent variables, with region, and occupation as fixed factors and work experience as a covariate. The Wilks Lambda multivariate test of overall differences among groups was significant, (F(2, 220)=1774, p<0.01; η2=0.96). The model was significant for each of the dependent variables, explaining a satisfactory amount of variance: Drug intolerance (F=5.52, p<0.01; η2=0.28) and PLWHA intolerance (F=3.70, p<0.01; η2=0.21). The work experience covariate was not significant for either of the outcomes (F<0.3, p>0.05 in both cases).
3.3 Intolerance toward PLWHA
Results showed a main effect of geographic region on PLWHA intolerance (F=3.60, p=0.01; η2=0.05) with the lowest levels of intolerance reported in western Ukraine. Although our analysis did not reveal a main effect of occupation, there was a significant region*occupation interaction effect on PLWHA intolerance (F=3.05, p<0.01; η2=0.11). Within region, the differences were driven by comparatively lower intolerance reported by medical administrators from the west and medical staff from the south, as well as higher intolerance reported by custodial staff in the east (Table 1). Within CJS occupation, a significant interaction was determined by highly varying regional differences for medical administrators and custodial staff (Table 2); specifically, most negative attitudes toward PLWHA were reported by custodial staff from the east, whereas least negative attitudes were held by medical administrators in the west, followed by medical staff in the south (Table 2).
3.4 Intolerance toward Drug Addiction
Regarding Drug intolerance, results produced the main effect for geographic region (F=3.33, p=0.03; η2=0.04), indicating that east and north Ukraine’s participants reported higher intolerance toward illegal drugs, relative to their colleagues from Ukraine’s other two regions. There was also a main effect for occupation (F=6.40, p<0.01; η2=0.09), demonstrating that medical staff held the least intolerable views among the four examined employment positions. There was also a significant region*occupation interaction (F=2.16, p=0.02; η2=0.07, see Tables 1 & 2), which showed that regional variability between east and north versus west and south was particularly strong within custodial staff, and medical administrators in the east reported higher intolerance toward drugs than medical administrators in the west, and that the only favorable attitude was reported by medical staff in the south.
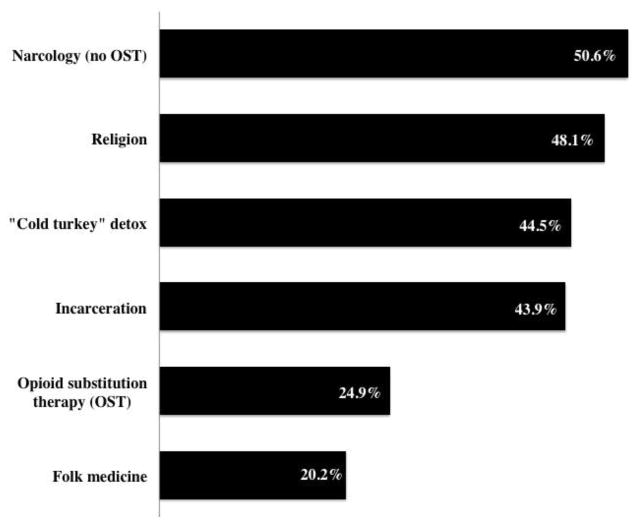
3.5 Perceived effectiveness
Figure 2 shows the perceived effectiveness of six methods to treat drug addiction, as reported cumulatively by our sample of Ukraine’s CJS personnel. It can be seen that non-OST narcology, a Soviet-era discipline characterized by pseudo-scientific assumptions about opioid dependence and criticized by international scientific community (Elovich and Drucker, 2008), that is also currently a preferred form of treatment in Russian Federation, superseded all treatment modalities, with half of the sample perceiving it to be effective. Compared to other common treatments for opioid dependence in Ukraine, OST was perceived to be effective by only a quarter of the surveyed personnel, which is in distinct contrast to narcology, incarceration, religion and “detox”, none of which are evidence-based treatments.
Figure 2.
Results for the mediation model for Drug Intolerance and OST Attitudes performed via AMOS Bootstrapping procedure with 2000 bootstrap samples and a bias-corrected accelerated confidence interval for ab. Indirect path through OST Knowledge (ab) was positive and significant, B(ab) = 0.212, p<0.001*, 95% CI = [.023, .629].
OST=opioid substitution therapy
3.6 Mediation Analysis
Presented in Table 3, OST attitudes significantly correlated only with OST knowledge that, in turn, positively correlated with the intolerance measures. The obtained correlations suggest that OST attitudes may be independent from other attitudinal constructs, and personnel’s intolerance toward drug addiction and PLWHA doesn’t imply the presence of negative attitudes toward OST. Next, although cross-sectional data doesn’t allow us to fully disentangle a puzzling positive correlation between OST knowledge and intolerance measures, we speculate that the existing intolerance toward drug addiction and PLWHA may have indirect effects on OST attitudes. To address this possibility, we tested for indirect effects among variables by using AMOS bootstrapping procedure (Bollen and Stine, 1992; Preacher et al., 2007), a recommended analytic strategy for avoiding measurement error and underestimation of the mediation significance, and found that there was a significant inconsistent mediation (MacKinnon et al., 2007), and that increased OST knowledge acted as a suppressor of the effects of Drug intolerance on OST attitudes. Specifically, the total indirect effect of drug intolerance on OST attitudes was fully mediated by OST knowledge (see Figure 3), which was positive and significant (B=0.212, p<0.01; 95% CI=[.023, .629]). Thus, higher intolerance toward drug addiction had a positive direct effect on knowledge about OST, and a fully mediated positive effect on attitudes toward OST. This mediation is inconsistent because the standardized direct effect of drug intolerance on OST attitudes is opposite in sign to its significant indirect effect (MacKinnon et al., 2000; Shrout and Bolger, 2002). This finding confirms the importance of mediation analyses in exploratory attitudinal studies in public health, because attitudinal constructs are rarely orthogonal and may relate to and interact with one another unexpectedly. The obtained inconsistent mediation revealed a surprising positive relationship between intolerance to drugs and drug addiction and the endorsement of OST. It can be reasoned that prison workers’ intolerance may lead to increased knowledge about OST, and ultimately to positive attitudes toward OST. Further investigation of this relationship is warranted.
Table 3.
Correlations among Attitudinal Constructs and Work Experience
| MEASURE | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Attitudes toward opioid substitution therapy | — | |||
| 2. Opioid substitution therapy knowledge | 0.62** | — | ||
| 3. Intolerance toward people living with HIV/AIDS | 0.12 | 0.22** | — | |
| 4. Intolerance toward drug addiction | 0.11 | 0.30** | 0.53** | — |
| 5. Work Experience | 0.06 | 0.24** | 0.14* | 0.14* |
p < .05;
p < .01
Figure 3.
Perceived Effectiveness for Drug Addiction Treatment Methods (%).
OST=opioid substitution therapy
4 DISCUSSION
The introduction and adoption of OST has been historically slow and difficult, but has been especially problematic in CJS populations (Friedmann et al., 2012; Jurgens et al., 2009; Oser et al., 2009) despite existing evidence supporting it (Stallwitz and Stover, 2007), with both patient and organizational issues impeding OST introduction and expansion. Research shows that such factors as the lack of knowledge, misinformation about, and negative attitudes toward OST have an impact on its use even in the US, where opioid-dependence has been treated with methadone for over 40 years. Our study was the first national survey to investigate attitudes toward OST, PLWHAs, and drug addiction of CJS personnel in Ukraine, a 23-year old country where OST was first introduced in 2004 as pilot programs.
At the policy level, there is a need for regulations, laws, public statements and funding to provide positive and supportive environment for organizational change. In Ukraine, such regulations allowing for OST introduction exist and there is funding from the Global Fund to support it. There are, however, many examples of where laws and regulations provide for the enactment of innovations (e.g., adoption or expansion of OST), but at the micro-level, the attitudes and personal opinions of managers (e.g., administrators) and/or line staff (e.g., medical staff or correctional officers) serve as a barrier to implementation. That is, the policy may allow for the innovation but the day-to-day operations within the facility impede progress. Moreover, there is extensive research shows that whenever therapeutic treatment programs are offered in prisons and jails by outside counselors or internal counselors, and the line staff do not support such programs, the result is disappointing: inmates do not enroll in programs, and correctional officers delay the delivery of the inmates to programs (Friedmann et al., 2007; Taxman et al., 2007). In fact, one of the key drivers of sound implementation is to ensure that line staff support the proposed initiative and understand the goals and objectives. One cannot “bypass” administrative personnel since they set the tone of the importance of an innovation in that environment (Taxman and Belenko, 2012). More generally, the idea that staff attitudes and values determine organizational change and shape organizational climate is well-documented in the literature on innovation implementation (Taxman and Belenko, 2012), which explicitly acknowledges staff members within an organization as a crucial implementation outcome (Fixsen et al., 2005; Klein and Sorra, 1996; Proctor et al., 2013; Rogers, 2003). Findings here provide important insights for future OST adoption and implementation in FSU countries.
With a population of 45 million people, Ukraine is characterized by diverse regional identities, which may rise above and beyond the effects of the demographic composition of a region and thus are important to account for in attitudinal studies. It is important to note that by revealing similarities between west and south, east and west, as well as interaction of region and occupation, our data doesn’t confirm the polarized view of Ukraine as being split into west and east. In fact, recoding the regions in our data into two categories to reflect the alleged divide, revealed no statistically significant difference between the regions for any of the outcome variables (t<1.63, p>0.10, for all cases). Our results reveal that Ukrainian CJS workers’ attitudes toward OST, PLWHA, and drug addiction are generally negative, with the average score for each of the constructs for the entire sample being below the neutral scale point. This overall negative sentiment was not ubiquitous, and was determined geographically and occupationally.
Specifically, workers in the west and south regions reported more positive attitudes toward OST, as well as a lower degree of intolerance toward PLWHA and drugs, relative to workers from the other two regions; however, the only significant difference between west and south was in OST knowledge (Figure 1). In turn, CJS personnel in the east and north regions did not differ in their attitudes toward and knowledge about OST, nor in their intolerance toward PLWHA, and drug addiction. The relatively positive attitudes in western region of the country are not entirely surprising. The most pronounced, documented, and historically salient cultural distinction is the difference between the Russian-influenced, urbanized, and industrial east, and pro-European, and largely agricultural west. Western Ukraine has been least influenced by Russia and by the USSR historically and ideologically, and has more closely aligned with Western Europe geographically and culturally. Such proximity may translate into concrete attitudinal and behavioral differences. Being under the Soviet rule for a shorter period of time, and therefore being distant from the inflexibility of Soviet planned economy, Western Ukrainians have traditionally travelled westward, traded with European neighbors, and thus may have embraced organizational habits and economic efficiency of western market economy after the collapse of the USSR quicker than their compatriots residing in other regions. Studies on economic transitions and privatization practices (Shulman, 2005; Tedstrom, 1995) and on voting behaviors of Ukrainians (Kubicek, 2000) report a nearly ubiquitous pro-market economy orientation of the western Ukrainians and suggests that due to its shorter shared history with the Soviet Union, western Ukraine endorses and pursues reforms more vigorously than eastern Ukraine, which gradually translates into tangible differences in performance. For example, a study of efficiency of Ukrainian hospitals (Pilyavsky et al., 2006) reports that hospitals in the west had demonstrated faster adoption of European management practices and improved efficiencies relative to those in the east.
The observed geographic effects indicate that people learn about and acquire solutions better when they are close to them. Therefore, the similarity of responses among CJS personnel from the west and south is particularly noteworthy because the southern region, arguably, has more in common with the east than the west. It is urbanized, industrial, densely-populated, and historically close to Russia. However, what sets Southern Ukraine apart is that drug use and HIV were introduced there and currently have the highest prevalence nationally. The highest Ukrainian HIV prevalence among prisoners (28.6%) is by far in the south (Azbel et al., 2013). This may in part explain a more progressive and solution-oriented attitudes of the local personnel: people may learn about and acquire solutions when they are close to the problem. With the south region having the highest HIV and drug use prevalence, CJS workers may be more motivated to seek out and learn about available solutions, more likely to lobby for and initiate reforms, and to notice the difference in their workplace and communities.
We also hypothesized that attitudes toward OST, PLWHA, and drug dependence will differ across occupational positions held by prison staff. Our results revealed that medical and custodial staff members report lower intolerance levels toward drug addiction, relative to administrators. Per our hypothesis, we suggest that staff members who work directly with prisoners are likely to sympathize, build relationships with, and ultimately identify with the client. This is particularly true for medical staff workers, who have reported the lowest intolerance toward drug addiction, as well as the lowest intolerance toward PLWHA relative to other investigated positions. Here we find support for our hypothesis of medical personnel holding less intolerable attitudes. Although our results showed that low intolerance was primarily reported by medical personnel in the west and in the south, it is important to point out that in the west it was reported by medical administrators, while in the south it was reported by medical staff workers, suggesting the presence of two different mechanisms of acceptance and tolerance: free market and European management orientation for medical administrators in the west, and identifiability effect for medical staff in the south. Research on identifiability shows that people react differently toward others in need, and even a weak form of identification, such as providing very basic impersonal information about an individual in a laboratory study, may increase caring (Kogut and Ritov, 2005; Small and Loewenstein, 2003b).
While the findings from this survey provide important insights into how the Ukrainian CJS must work differently and distinctly with various personnel within different regions, the epilogue now is mired by ineffectual governance of the CJS due to annexation of Crimea by Russia and ongoing conflicts in Eastern Ukraine. Although an in-depth review of these events is out of the scope of this paper, their relevancy to our work is hard to overstate. OST and needle exchange programs are forbidden in Russia, and such globally accepted concepts as harm reduction’ are seen as corrupting influences of the West, and are not endorsed by health professionals (Wolfe, 2007). Even though the situation in Ukraine is not as bleak, and the Ukrainian harm reduction programs have been fruitful (Alliance, 2012), Russian influence remains strong and pervasive. Therefore, any effective intervention will have to selectively differentiate regions that align most with Russia (i.e., East and North) where high levels of drug intolerance and negative attitudes toward OST prevail.
Our data suggest that adequate information and increased knowledge about the benefits of OST have a direct positive effect on positive attitudes toward and endorsement of OST, thereby highlighting the importance of educational interventions that would directly target perpetuated myths about and prejudices toward OST. Importantly, any ideology is a set of attitudes, which should be studied and comprehended before they can be targeted for transformation. To our knowledge, this is the first study of CJS workers’ attitudes, and its results are currently being used to develop an extensive attitude and behavior change intervention to ensure OST acceptance and sustainability for Ukrainian providers and patients alike.
In the absence of introducing OST within CJS, alternative strategies like using injectable long-acting opioid antagonists at the time of release may serve as a bridge to OST in settings where implementing OST in the CJS is presently unattainable (Kunoe et al., 2010; Lobmaier et al., 2010). Though preliminary data suggest that opioid antagonists may have some benefit for this population, concerns about cost, uncertainty about release dates and eventual overdose for those not remaining on opioid antagonists (Wolfe et al., 2011) or not transitioning to OST have limited this strategy until more evidence becomes available (Di Paola et al., 2014). Irrespective of whether OST or long-acting opioid antagonist therapies are deployed, both will require organizational change for adoption and expansion where innovations of using medications to treat addiction are counter-intuitive to the CJS (Friedmann et al., 2012; Friedmann et al., 2014; Springer et al., 2011).
In Ukraine, ideological biases and persisting negative attitudes toward OST restrict its adoption and expansion in CJS, despite the evidence supporting its introduction. By elucidating existing attitudes among CJS personnel, understanding better the relationships between drug addiction, OST attitudes and accurate knowledge will help direct subsequent interventions to address the barriers to implementing evidence-based HIV prevention treatments. Future strategies should include designing effective interventions for CJS personnel that incorporate identifiability and accurate information. In the absences of such interventions with prison personnel, staff may collectively undermine introduction of evidence-based treatments on ideological rather than informed principles.
Highlights.
Ukranian Criminal Justice System workers’ attitudes were universally negative
Attitudes differed along geographic and occupational lines
Proximity to the European Union drove positive attitudes in the west
An identifiability effect in the southern region
Knowledge mediated the effect of drug intolerance on opioid substitution therapy attitudes.
Acknowledgments
Role of Funding Source
This research received funding from the National Institute on Drug Abuse for research (R01 DA029910, Altice, PI and R01 DA033679), career development (K24 DA017072 for Altice and K01 DA038529 for Wickersham), and the NIH Fogarty Research Training Grant (R25 TW009338, Polonsky). These funding agencies had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Contributors
MP: researched literature, analyzed data, wrote paper; LA: designed survey, collected data, wrote paper; JW: designed survey, edited paper; FT: interpreted results, edited paper; EG: designed survey, collected data; SD: designed survey, collected data; FA: designed survey, interpreted results, wrote paper. All authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alistar SS, Owens DK, Brandeau ML. Effectiveness and cost effectiveness of expanding harm reduction and antiretroviral therapy in a mixed HIV epidemic: a modeling analysis for Ukraine. PLoS Med. 2011;8:e1000423. doi: 10.1371/journal.pmed.1000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International HIV/AIDS Alliance. Analytical Report: Behavioral Monitoring And HIV-Prevalence Among Injecting Drug Users As A Component Of Second Generation Surveillance. Kyiv; Ukraine: 2012. [Google Scholar]
- Altice FL, Bruce RD, Lucas GM, Lum PJ, Korthuis PT, Flanigan TP, Cunningham CO, Sullivan LE, Vergara-Rodriguez P, Fiellin DA, Cajina A, Botsko M, Nandi V, Gourevitch MN, Finkelstein R, Collaborative B. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: results from a multisite study. J Acquir Immune Defic Syndr. 2011;56:S22–32. doi: 10.1097/QAI.0b013e318209751e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376:59–79. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Sullivan LE, Smith-Rohrberg D, Basu S, Stancliff S, Eldred L. The potential role of buprenorphine in the treatment of opioid dependence in HIV-infected individuals and in HIV infection prevention. Clin Infect Dis. 2006;43(Suppl 4):S178–183. doi: 10.1086/508181. [DOI] [PubMed] [Google Scholar]
- Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abuse Treat. 2005;28:321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Arel D. Language politics in independent Ukraine: towards one or two state languages? Natl Pap. 1995;23:597–622. [Google Scholar]
- Azbel L, Wickersham JA, Grishaev Y, Dvoryak S, Altice FL. Burden of infectious diseases, substance use disorders, and mental illness among Ukrainian prisoners transitioning to the community. PLoS One. 2013;8:e59643. doi: 10.1371/journal.pone.0059643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Wickersham JA, Grishaev Y, Dvoryak S, Altice FL. Correlates of HIV infection and being unaware of HIV status among soon-to-be-released Ukrainian prisoners. J Int AIDS Soc. 2014;17:19005. doi: 10.7448/IAS.17.1.19005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington L, Faranda R. Reexamining region, ethnicity, and language in Ukraine. Post Sov Affairs. 2009;25:232–256. [Google Scholar]
- Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159:592–600. doi: 10.7326/0003-4819-159-9-201311050-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD. Release from prison--a high risk of death for former inmates. N Engl J Med. 2007;356:157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojko MJ, Dvoriak S, Altice FL. At the crossroads: HIV prevention and treatment for people who inject drugs in Ukraine. Addiction. 2013a;108:1697–1699. doi: 10.1111/add.12243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA, Stine RA. Bootstrapping goodness-of-fit measures in structural equation models. Sociol Methods Res. 1992;21:205–229. [Google Scholar]
- Bruce RD, Dvoryak S, Sylla L, Altice FL. HIV treatment access and scale-up for delivery of opiate substitution therapy with buprenorphine for IDUs in Ukraine--programme description and policy implications. Int J Drug Policy. 2007;18:326–328. doi: 10.1016/j.drugpo.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caplehorn JR, Lumley TS, Irwig L. Staff attitudes and retention of patients in methadone maintenance programs. Drug Alcohol Depend. 1998;52:57–61. doi: 10.1016/s0376-8716(98)00047-7. [DOI] [PubMed] [Google Scholar]
- Cohen J. No opiate substitutes for the masses of IDUs. Science. 2010;329:165–167. doi: 10.1126/science.329.5988.165. [DOI] [PubMed] [Google Scholar]
- DeBell D, Carter R. Impact of transition on public health in Ukraine: case study of the HIV/AIDS epidemic. BMJ. 2005;331:216–219. doi: 10.1136/bmj.331.7510.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Mathers BM, Wirtz AL, Wolfe D, Kamarulzaman A, Carrieri MP, Strathdee SA, Malinowska-Sempruch K, Kazatchkine M, Beyrer C. What has been achieved in HIV prevention, treatment and care for people who inject drugs, 2010–2012? A review of the six highest burden countries. Int J Drug Policy. 2013;25:53–60. doi: 10.1016/j.drugpo.2013.08.004. [DOI] [PubMed] [Google Scholar]
- Di Paola A, Lincoln T, Skiest DJ, Desabrais M, Altice FL, Springer SA. Design and methods of a double blind randomized placebo-controlled trial of extended-release naltrexone for HIV-infected, opioid dependent prisoners and jail detainees who are transitioning to the community. Contemp Clin Trials. 2014 doi: 10.1016/j.cct.2014.09.002. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. FMHI Publication #231. University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network; Tampa, FL: 2005. Implementation Research: A Synthesis of the Literature. [Google Scholar]
- Flanigan T, Zaller N, Beckwith CG, Bazerman LB, Rana A, Gardner A, Wohl DA, Altice FL. Testing for HIV, sexually transmitted infections, and viral hepatitis in jails: still a missed opportunity for public health and HIV prevention. J Acquir Immune Defic Syndr. 2010;55:S78–S83. doi: 10.1097/QAI.0b013e3181fbc94f. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, Hoskinson R, Gordon M, Schwartz R, Kinlock T, Knight K, Flynn PM, Welsh WN, Stein LA, Sacks S, O’Connell DJ, Knudsen HK, Shafer MS, Hall E, Frisman LK Mat Working Group Of C.J. Dats. Medication-assisted treatment in criminal justice agencies affiliated with the criminal justice-drug abuse treatment studies (CJ-DATS): availability, barriers, and intentions. Subst Abuse. 2012;33:9–18. doi: 10.1080/08897077.2011.611460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Taxman FS, Henderson CE. Evidence-based treatment practices for drug-involved adults in the criminal justice system. J Subst Abuse Treat. 2007;32:267–277. doi: 10.1016/j.jsat.2006.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Wilson D, Knudsen HK, Ducharme LJ, Welsh WN, Frisman L, Knight K, Lin HJ, James A, Albizu-Garcia CE, Pankow J, Hall EA, Urbine TF, Abdel-Salam S, Duvall JL, Vocci FJ. Effect of an organizational linkage intervention on staff perceptions of medication-assisted treatment and referral intentions in community corrections. J Subst Abuse Treat. 2014 doi: 10.1016/j.jsat.2014.10.001. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh DS, Primavera C, Bartalini G. Risk behaviors, self-efficacy, and AIDS prevention among adolescents. J Psychol. 1996;130:537–546. doi: 10.1080/00223980.1996.9915020. [DOI] [PubMed] [Google Scholar]
- Izenberg J, Altice FL. Next steps for Ukraine abolition of HIV registries, implementation of routine human immunodeficiency virus testing and expansion of services. Addiction. 2010;105:568–570. doi: 10.1111/j.1360-0443.2009.02881.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izenberg J, Bachireddy C, Soule M, Kiriazova T, Dvoryak S, Altice FL. High rates of police detention among recently released HIV-infected prisoners in Ukraine: implications for health outcomes. Drug Alcohol Depend. 2013;133:154–160. doi: 10.1016/j.drugalcdep.2013.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS) The Gap Report. Geneva, Switzerland: 2014. [Accessed on 24 August 2014]. at: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2014/unaids_gap_report_en.pdf. [Google Scholar]
- Jurgens R, Ball A, Verster A. Interventions to reduce HIV transmission related to injecting drug use in prison. Lancet Infect Dis. 2009;9:57–66. doi: 10.1016/S1473-3099(08)70305-0. [DOI] [PubMed] [Google Scholar]
- Jurgens R, Nowak M, Day M. HIV and incarceration: prisons and detention. J Int AIDS Soc. 2011;14:26. doi: 10.1186/1758-2652-14-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kermode M, Crofts N, Kumar MS, Dorabjee J. Opioid substitution therapy in resource-poor settings. Bull WHO. 2011;89:243. doi: 10.2471/BLT.11.086850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT, O’Grady KE. A randomized clinical trial of methadone maintenance for prisoners: results at 12 months postrelease. J Subst Abuse Treat. 2009;37:277–285. doi: 10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein KJ, Sorra JS. The challenge of innovation implementation. Acad Manage Rev. 1996;21:1055–1080. [Google Scholar]
- Kogut T, Ritov I. The “identified victim” effect: an identified group, or just a single individual? J Behav Decis Mak. 2005;18:157–167. [Google Scholar]
- Kubicek P. Regional polarisation in Ukraine: public opinion, voting and legislative behaviour. Eur Asia Stud. 2000;52:273–294. [Google Scholar]
- Kunoe N, Lobmaier P, Vederhus JK, Hjerkinn B, Hegstad S, Gossop M, Kristensen O, Waal H. Retention in naltrexone implant treatment for opioid dependence. Drug Alcohol Depend. 2010;111:166–169. doi: 10.1016/j.drugalcdep.2010.03.021. [DOI] [PubMed] [Google Scholar]
- Larney S, Dolan K. A literature review of international implementation of opioid substitution treatment in prisons: equivalence of care? Eur Addict Res. 2009;15:107–112. doi: 10.1159/000199046. [DOI] [PubMed] [Google Scholar]
- Larney S, Toson B, Burns L, Dolan K. Effect of prison-based opioid substitution treatment and post-release retention in treatment on risk of re-incarceration. Addiction. 2012;107:372–380. doi: 10.1111/j.1360-0443.2011.03618.x. [DOI] [PubMed] [Google Scholar]
- Lawrinson P, Ali R, Buavirat A, Chiamwongpaet S, Altice FL, Dvoryak S, Habrat B, Jie S, Mardiati R, Mokri A, Moskalewicz J, Newcombe D, Poznyak V, Subata E, Uchtenhagen A, Utami DS, Vial R, Zhao C. Key findings from the WHO collaborative study on substitution therapy for opioid dependence and HIV/AIDS. Addiction. 2008;103:1484–1492. doi: 10.1111/j.1360-0443.2008.02249.x. [DOI] [PubMed] [Google Scholar]
- Lev-Ran S, Adler L, Nitzan U, Fennig S. Attitudes towards nicotine, alcohol and drug dependence among physicians in Israel. J Subst Abuse Treat. 2013;44:84–89. doi: 10.1016/j.jsat.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Lobmaier PP, Kunoe N, Gossop M, Katevoll T, Waal H. Naltrexone implants compared to methadone: outcomes six months after prison release. Eur Addict Res. 2010;16:139–145. doi: 10.1159/000313336. [DOI] [PubMed] [Google Scholar]
- Lucas GM, Chaudhry A, Hsu J, Woodson T, Lau B, Olsen Y, Keruly JC, Fiellin DA, Finkelstein R, Barditch-Crovo P, Cook K, Moore RD. Clinic-based treatment of opioid-dependent HIV-infected patients versus referral to an opioid treatment program: a randomized trial. Ann Intern Med. 2010;152:704–711. doi: 10.1059/0003-4819-152-11-201006010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Ann Rev Psychol. 2007;58:593. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magura S, Lee JD, Hershberger J, Joseph H, Marsch L, Shropshire C, Rosenblum A. Buprenorphine and methadone maintenance in jail and post-release: a randomized clinical trial. Drug Alcohol Depend. 2009;99:222–230. doi: 10.1016/j.drugalcdep.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik K. The Rise Of The South: Human Progress In A Diverse World. UNDP; New York: 2013. Human Development Report 2013. [Google Scholar]
- Maru DS, Basu S, Altice FL. HIV control efforts should directly address incarceration. Lancet Infect Dis. 2007;7:568–569. doi: 10.1016/S1473-3099(07)70190-1. [DOI] [PubMed] [Google Scholar]
- Metzger DS, Woody GE, McLellan AT, O’Brien CP, Druley P, Navaline H, DePhilippis D, Stolley P, Abrutyn E. Human immunodeficiency virus seroconversion among intravenous drug users in- and out-of-treatment: an 18-month prospective follow-up. J Acquir Immune Defic Syndr. 1993;6:1049–1056. [PubMed] [Google Scholar]
- Morozova O, Azbel L, Grishaev Y, Dvoryak S, Wickersham JA, Altice FL. Ukrainian prisoners and community reentry challenges: implications for transitional care. Int J Prison Health. 2013;9:5–19. doi: 10.1108/17449201311310760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oser CB, Knudsen HK, Staton-Tindall M, Taxman F, Leukefeld C. Organizational-level correlates of the provision of detoxification services and medication-based treatments for substance abuse in correctional institutions. Drug Alcohol Depend. 2009;103(Suppl 1):S73–81. doi: 10.1016/j.drugalcdep.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palepu A, Tyndall MW, Joy R, Kerr T, Wood E, Press N, Hogg RS, Montaner JS. Antiretroviral adherence and HIV treatment outcomes among HIV/HCV co-infected injection drug users: the role of methadone maintenance therapy. Drug Alcohol Depend. 2006;84:188–194. doi: 10.1016/j.drugalcdep.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Pilyavsky AI, Aaronson WE, Bernet PM, Rosko MD, Valdmanis VG, Golubchikov MV. East-west: does it make a difference to hospital efficiencies in Ukraine? Health Econ. 2006;15:1173–1186. doi: 10.1002/hec.1120. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behav Res. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139. doi: 10.1186/1748-5908-8-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers E. Diffusion of Innovations. 5. Free Press; New York, NY: 2003. [Google Scholar]
- Samet JH. Russia and human immunodeficiency virus--beyond crime and punishment. Addiction. 2011;106:1883–1885. doi: 10.1111/j.1360-0443.2011.03523.x. [DOI] [PubMed] [Google Scholar]
- Schelling TC. The Life You Save May Be Your Own. The Brookings Institute; Washington, DC: 1968. [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7:422. [PubMed] [Google Scholar]
- Shulman S. National identity and public support for political and economic reform in Ukraine. Slavic Rev. 2005;64:59–87. [Google Scholar]
- Small D, Loewenstein G. Helping a victim or helping the victim: altruism and identifiability. J Risk Uncertain. 2003a;26:5–16. [Google Scholar]
- Springer SA, Azar MM, Altice FL. HIV, alcohol dependence, and the criminal justice system: a review and call for evidence-based treatment for released prisoners. Am J Drug Alcohol Abuse. 2011;37:12–21. doi: 10.3109/00952990.2010.540280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer SA, Bruce RD. A pilot survey of attitudes and knowledge about opioid substitution therapy for HIV-infected prisoners. J Opioid Manage. 2008a;4:81. doi: 10.5055/jom.2008.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer SA, Qiu J, Saber-Tehrani AS, Altice FL. Retention on buprenorphine is associated with high levels of maximal viral suppression among HIV-infected opioid dependent released prisoners. PLoS One. 2012;7:e38335. doi: 10.1371/journal.pone.0038335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallwitz A, Stover H. The impact of substitution treatment in prisons--a literature review. Int J Drug Policy. 2007;18:464–474. doi: 10.1016/j.drugpo.2006.11.015. [DOI] [PubMed] [Google Scholar]
- Stover H, Casselman J, Hennebel L. Substitution treatment in European prisons: a study of policies and practices in 18 European countries. Int J Prison Health. 2006;2:3–12. [Google Scholar]
- Talal AH, Dimova RB, Seewald R, Peterson RH, Zeremski M, Perlman DC, Des Jarlais DC. Assessment of methadone clinic staff attitudes toward hepatitis C evaluation and treatment. J Subst Abuse Treat. 2013;44:115–119. doi: 10.1016/j.jsat.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taxman FS, Belenko S. Implementing Evidence-Based Practices in Community Corrections and Addiction Treatment. Springer; New York, NY: 2012. [Google Scholar]
- Taxman FS, Perdoni ML, Harrison LD. Drug treatment services for adult offenders: the state of the state. J Subst Abuse Treat. 2007;32:239–254. doi: 10.1016/j.jsat.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedstrom JE. Ukraine: a crash course in economic transition. Comp Econ Stud. 1995;37:49–67. [Google Scholar]
- Torrens M, Fonseca F, Castillo C, Domingo-Salvany A. Methadone maintenance treatment in Spain: the success of a harm reduction approach. Bull WHO. 2013;91:136–141. doi: 10.2471/BLT.12.111054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy K, Brown LS, Kritz S, Alderson D, Robinson J, Bini EJ, Levy M, Calsyn D, Rieckmann T, Fuller B, McAuliffe P, Rotrosen J. Substance abuse treatment clinician opinions and infectious disease service delivery. J Addict Dis. 2009;28:8–12. doi: 10.1080/10550880802544625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlmann S, Milloy MJ, Kerr T, Zhang R, Guillemi S, Marsh D, Hogg RS, Montaner JS, Wood E. Methadone maintenance therapy promotes initiation of antiretroviral therapy among injection drug users. Addiction. 2010;105:907–913. doi: 10.1111/j.1360-0443.2010.02905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. Joint United Nations Programme on HIV/AIDS (UNAIDS) Global report: UNAIDS report on the global AIDS epidemic 2013. UNAIDS; Geneva, Switzerland: 2013. [Google Scholar]
- UNAIDS/WHO. AIDS Epidemic Update. Geneva: 2006. United Nations Programme on HIV/AIDS/World Health Organization. [Google Scholar]
- United Nations Office on Drug Control (UNODC) Analysis of HIVAIDS response in penitentiary system of Ukraine. New York: 2012. [Google Scholar]
- Vagenas P, Azbel L, Polonsky M, Kerimi N, Mamyrov M, Dvoryak S, Altice FL. A review of medical and substance use co-morbidities in Central Asian prisons: implications for HIV prevention and treatment. Drug Alcohol Depend. 2013;132(Suppl 1):S25–31. doi: 10.1016/j.drugalcdep.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walmsley R. World Prison Population List. 10. University of Essex; London, England: 2014. [Accessed on July 14 2014]. at: http://www.prisonstudies.org/sites/prisonstudies.org/files/resources/downloads/wppl_2010.pdf. [Google Scholar]
- World Health Organization (WHO) World health statistics 2013: a wealth of information on global public health. World Health Organization; Geneva: 2013. [Google Scholar]
- Wolfe D. Paradoxes in antiretroviral treatment for injecting drug users: access, adherence and structural barriers in Asia and the former Soviet Union. Int J Drug Policy. 2007;18:246–254. doi: 10.1016/j.drugpo.2007.01.012. [DOI] [PubMed] [Google Scholar]
- Wolfe D, Carrieri MP, Dasgupta N, Wodak A, Newman R, Bruce RD. Concerns about injectable naltrexone for opioid dependence. Lancet. 2011;377:1468–1470. doi: 10.1016/S0140-6736(10)62056-9. [DOI] [PubMed] [Google Scholar]
- Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet. 2010;376:355–366. doi: 10.1016/S0140-6736(10)60832-X. [DOI] [PubMed] [Google Scholar]
- Zaller N, Mazhnaya A, Larney S, Islam Z, Shost A, Prokhorova T, Rybak N, Flanigan T. Geographic variability in HIV and injection drug use in Ukraine: implications for integration and expansion of drug treatment and HIV care. Int J Drug Policy. 2014 doi: 10.1016/j.drugpo.2014.09.004. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]