Sir,
Pterygium surgery is typically performed in an outpatient setting with subconjunctival anesthesia.1 Owing to the short duration of action of local anesthesia, patients may experience considerable pain and discomfort following surgery once anesthesia has worn off. Wishaw et al2 showed that clinically significant postoperative pain (conjunctival and corneal origin) is reportedly experienced in 60% of patients undergoing pterygium surgery.
The purpose of this prospective randomized study was to compare the postoperative pain, and symptoms of photophobia, epiphora, and foreign body sensation, with overnight patching vs placement of a bandage lens for the management of postoperative pain following pterygium surgery.
Results
Of 30 eyes in each group, 15/30 in the patching group and 17/30 in the bandage lens group were male. All but one case in each group had nasal pterygia. The mean age of patients was 50.1±10.6 years in the patching group and 49.0±16.9 years in the bandage lens group. No statistically significant differences existed between the two groups with respect to age, laterality, pterygium location, gender, size of pterygium, size of conjunctival autograft required, or preoperative visual acuity (Table 1).
Table 1. Clinical characteristics in patients with primary pterygium undergoing excision followed by patching or bandage lens.
| Patching | Bandage lens | P-value | |
|---|---|---|---|
| No. of eyes | 30 | 30 | |
| Laterality (right:left) | 13:17 | 16:14 | 0.45 |
| Pterygium Location (nasal:temporal) | 29:1 | 29:1 | 1 |
| Age (years) | 50.1±10.6 | 49.0±16.9 | 0.77 |
| Gender (male:female) | 15:15 | 17:13 | 0.60 |
| Size of pterygium (mm2) | 12.29±7.65 | 15.9±12.76 | 0.19 |
| Size of CAU required | 43.83±16.86 | 49.67±24.48 | 0.29 |
| Preoperative visual acuity (logMAR) | 0.157±0.168 | 0.17±0.166 | 0.76 |
Abbreviation: CAU, conjunctival autograft.
Comment
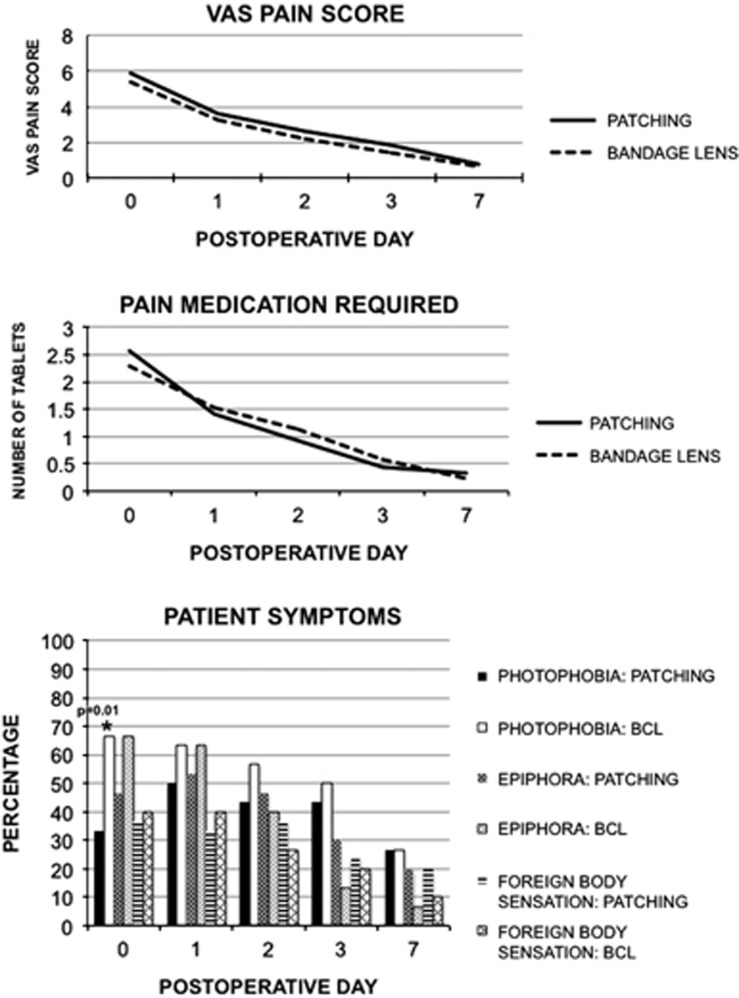
Figure 1 summarizes the results of the primary and secondary end points of the study. There was no statistically significant difference in VAS pain score or amount of pain medication taken between groups during the first week. Significantly more eyes were reported to be photophobic on POD 0 in the bandage lens group (P=0.01; odds ratio=4.0). Using linear logistic regression analysis, VAS pain score predicted the amount of pain medication taken on the same day (P<0.0001; no significant difference between groups). On POD 0 only, VAS pain score was statistically significantly related to the graft area required (P=0.023). Age was noted to be inversely correlated to the amount of pain medication taken; for every additional year of age, a given patient would have taken 0.13 less tablets (P=0.0009). None of the clinical symptoms (photophobia, epiphora, and foreign body sensation) were predicted by any of the baseline characteristic of the groups.
Figure 1.
VAS pain score, amount of pain medication taken, and clinical symptoms in patients following pterygium surgery with postoperative patching or bandage lens.
Interestingly, postoperative pain and requirement for pain medication (acetaminophen with codeine tablets) was similar after POD 1, when the patch was removed. The bandage lens during the first postoperative week did not appear to improve comfort. These results suggest that both modalities help in reducing the postoperative pain following pterygium excision, although overnight patching may provide further relief from the symptoms of photophobia.
Either overnight patching or the placement of a bandage contact lens is safe and effective in the management of postoperative pain following excision of primary pterygia with CAU. In cases where overnight patching would interfere with the visual needs of the patient, the placement of a bandage lens is preferable.
The authors declare no conflict of interest.
References
- Smith RB, Everett WG. Physiology and pharmacology of local anesthetic agents. Int Ophthalmol Clin. 1973;13 (2:35–60. [PubMed] [Google Scholar]
- Wishaw K, Billington D, O'Brien D, Davies P. The use of orbital morphine for postoperative analgesia in pterygium surgery. Anaesth Intensive Care. 2000;28 (1:43–45. doi: 10.1177/0310057X0002800107. [DOI] [PubMed] [Google Scholar]