Abstract
We present the case of a 48-year-old man with an extensive cannabis smoking history who presented with pleuritic chest pain. A chest X-ray revealed multiple large, apical lung bullae with fluid levels, an appearance consistent with infection. Lung function tests showed moderate airflow obstruction and decreased gas transfer. The infection was treated with a prolonged course of antimicrobials, and the patient followed up by respiratory physicians.
Background
There have been at least 36 case reports of bullous lung disease1 in young adults with a heavy cannabis smoking history. The apical regions of the lungs are the areas most consistently affected.2 3 Most of these cases have had unremarkable chest X-rays and lung function tests. We present the case of a man with a heavy cannabis smoking history, a remarkable chest X-ray appearance, and significantly abnormal gas transfer on lung function testing (figure 1).
Figure 1.
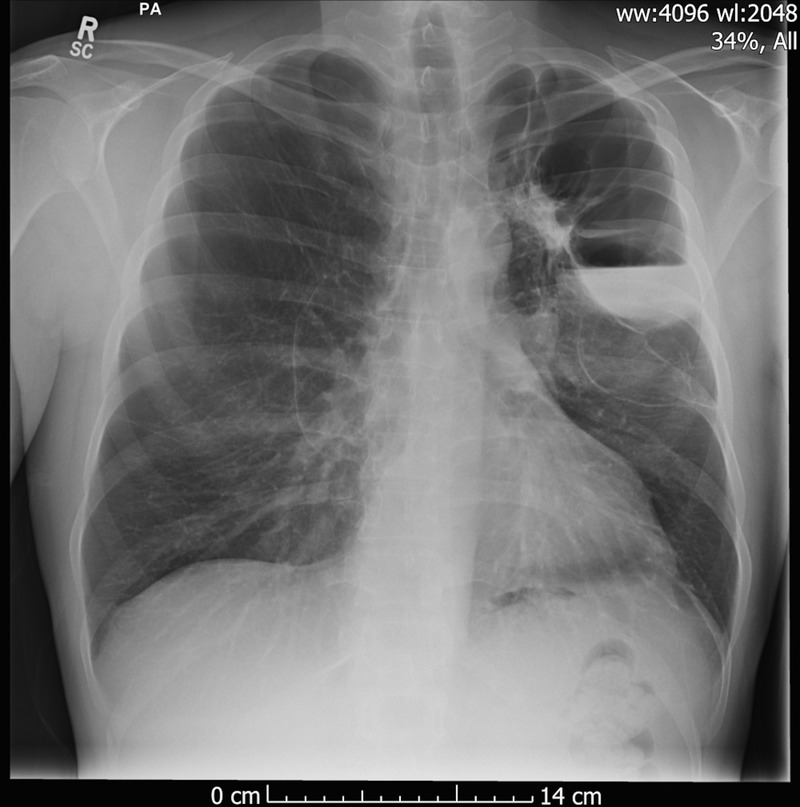
The presenting chest X-ray showing hyperexpanded lungs, with left-sided bullae with fluid zones.
Case presentation
A 48-year-old unemployed Caucasian man with a history of schizophrenia presented with left-sided, posterior, mid-thoracic pleuritic chest pain. He had no other respiratory symptoms. At the time a chest X-ray showed multiple, large lung bullae with fluid levels, consistent with infection. The patient had no history of lung disease, or recent traumatic injury. On further questioning, he divulged a 25-pack-year smoking history and an 86-joint-year cannabis smoking history.4 Examination of the respiratory system revealed mild crepitations of the left mid-zone.
Investigations
Investigation revealed a raised C reactive protein (CRP), consistent with infection. The patient was found to have a normal α1-antitrypsin level. Chest X-rays during admission showed persistent fluid levels in the large apical bullae. A CT of the thorax (figure 2) showed extensive upper and mid-zone bullous disease, with some bronchiectasis. Two of the large bullae showed air-fluid levels. No additional pulmonary, mediastinal or pleural lesion was identified. Blood cultures taken on admission were negative after 5 days, and a sputum culture grew only Candida. The patient's lung function tests showed moderate airflow obstruction, with a forced expiratory volume in 1 s of 2.61, 67% of predicted. The alveolar volume was 68% of predicted, but lung diffusion capacity test results were markedly low at 35% of predicted.
Figure 2.
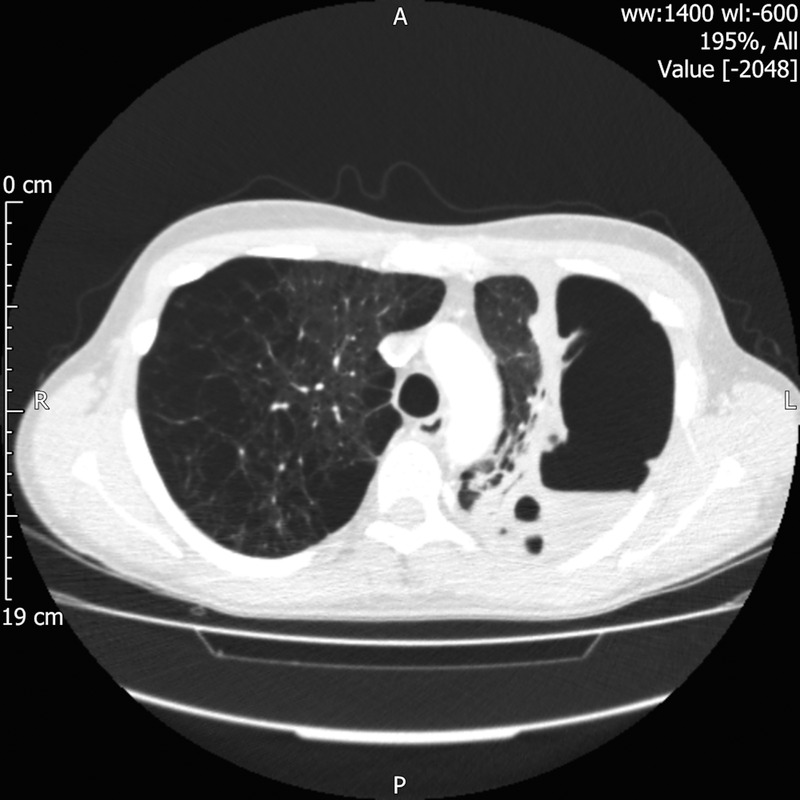
CT of the thorax showing bilateral bullous changes.
Differential diagnosis
A lung abscess was considered as a differential diagnosis.
Treatment
The patient received 10 days of intravenous ertapenem, followed by 9 days of intravenous meropenem. As the pleuritic chest pain resolved and the CRP fell, the antibiotics were subsequently switched to oral metronidazole and doxycycline. These antibiotic choices were influenced by the patient's penicillin allergy. Inhaled aclidinium bromide was introduced in light of the moderate chronic obstructive pulmonary disease, as detected by spirometry.
Outcome and follow-up
During the patient's stay in hospital, the intrabulla fluid initially worsened, before beginning to improve. However, it did not resolve fully during admission.
The patient is being followed up in clinic under the respiratory team. The clinic encounters that have taken place to date have revealed no return of clinical or laboratory signs of infection, and continuing slow resolution of the intrabulla fluid.
The patient will continue to be under the care of the respiratory team, with the potential for future surgical intervention and bullectomy.
Discussion
Lee and Hancox1 summarised the 36 case reports that they found in the English literature attributing bullous lung disease to heavy cannabis smoking. Most reported cases of cannabis-related bullous lung disease have relatively normal chest X-ray appearances,3 unlike the multiple large bullae with fluid levels seen in the discussed patient. It is also far more common for such patients to present with dyspnoea or infective symptoms than with pleuritic chest pain alone.2 3
The exact mechanism behind the development of apical bullous lung disease in cannabis smokers is not clear. However, it is thought that there may be some link between the manoeuvre used in cannabis smoking, namely a larger inspiratory effort and longer breath holding, and the pattern of pulmonary disease seen in this population.3 Additionally, there is a significant lack of longitudinal data on cannabis smoking and its effects on health.5 6 Furthermore, cannabis smokers also commonly smoke tobacco, and the combination of tobacco and cannabis smoke is also thought to be harmful.2
Learning points.
Pleuritic chest pain presents a wide range of differentials in a young patient.
Cannabis smoking can be associated with significant lung damage.
It is important to take a cannabis smoking history alongside a tobacco smoking history.
Infected bullous lung disease may require long courses of antimicrobial therapy.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lee MHS, Hancox RJ. Effects of smoking cannabis on lung function. Expert Rev Respir Med 2011;5:537–46. quiz 547 10.1586/ers.11.40 [DOI] [PubMed] [Google Scholar]
- 2.Johnson MK, Smith RP, Morrison D et al. . Large lung bullae in marijuana smokers. Thorax 2000;55:340–2. 10.1136/thorax.55.4.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hii SW, Tam JDC, Thompson BR et al. . Bullous lung disease due to marijuana. Respirology 2008;13:122–7. 10.1111/j.1440-1843.2007.01186.x [DOI] [PubMed] [Google Scholar]
- 4.Hall W, Solowij N. Adverse effects of cannabis. Lancet 1998;352:1611–16. 10.1016/S0140-6736(98)05021-1 [DOI] [PubMed] [Google Scholar]
- 5.Howden ML, Naughton MT. Pulmonary effects of marijuana inhalation. Expert Rev Respir Med 2011;5:87–92. 10.1586/ers.10.87 [DOI] [PubMed] [Google Scholar]
- 6.Taylor DR, Fergusson DM, Milne BJ et al. . A longitudinal study of the effects of tobacco and cannabis exposure on lung function in young adults. Addiction 2002;97:1055–61. 10.1046/j.1360-0443.2002.00169.x [DOI] [PubMed] [Google Scholar]


