Description
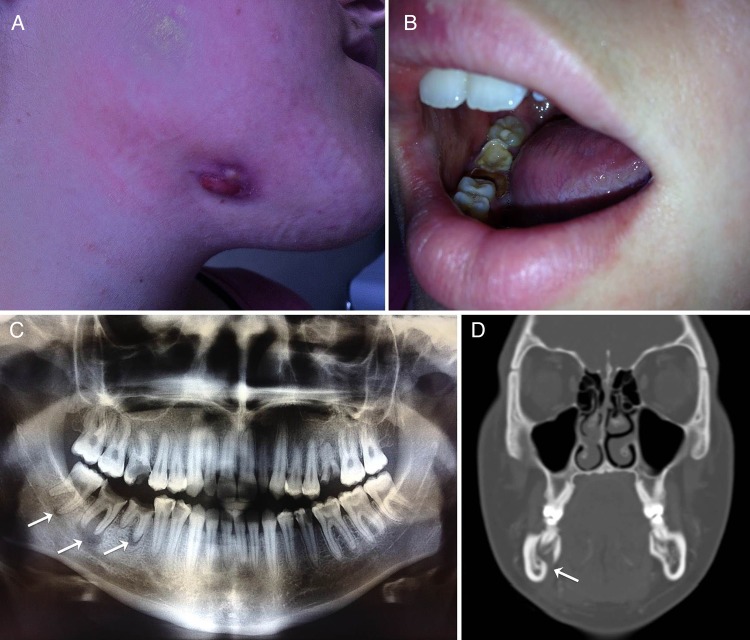
A 22-year-old woman attended the infectious diseases consultation for a 2-week history of painless afebrile submaxillary tumefaction with continuous serous exudate (figure 1A). Oral examination revealed multiple carious teeth (figure 1B). Panoramic dental radiography disclosed multiple periapical tooth abscesses (figure 1C, arrows). CT scan highlighted signs of chronic osteomyelitis of the lower mandible (figure 1D, arrows). Although actinomycosis was not proven, a regimen of amoxicillin (6 g/day) and clindamycin (1800 mg/day) was initiated, associated to dental avulsion, providing rapid improvement of symptoms.
Figure 1.
Submaxillary tumefaction with a continuous serous exudate (A), associated with multiple carious teeth (B), multiple periapical tooth abscesses (dental panoramic radiograph, (C), arrows) and chronic osteomyelitis of the lower mandible (CT scan, (D), arrows).
Lumpy jaw syndrome is well known by veterinarians, as it is frequent in cattle, swine, horses and dogs. It consists of a large unilateral abscess that grows on the head and neck of the infected animal, following dental disease and mandibular osteomyelitis. In humans, this syndrome is particularly associated with poor dental hygiene, periodontal disease and periapical dental abscess.1 Lumpy jaw syndrome is mainly due to anaerobic polymicrobial infection, including Actinomyces spp (filamentous Gram-positive bacilli belonging to the human commensal flora).2 Lumpy jaw syndrome is the most frequent clinical form of actinomycosis and can be associated with fistula, as in the our case. Treatment of dental disease (mainly dental avulsion) is essential, and antimicrobial therapy with high-dose amoxicillin is the treatment of choice. Association of a companion such as clavulanate or clindamycin is controversial, but may help target copathogens.1 3
Learning points.
Lumpy jaw syndrome associates unilateral head and neck abscess, mandibular osteomyelitis and dental infection.
Actinomyces spp are the main oropharyngeal commensals involved in lumpy jaw syndrome.
Dental avulsion and high doses of amoxicillin are usually the treatment of choice.
Footnotes
Collaborators: Lyon Bone and Joint Infection Study Group: Physicians – Tristan Ferry, Thomas Perpoint, André Boibieux, François Biron, Florence Ader, Julien Saison, Florent Valour, Fatiha Daoud, Johanna Lippman, Evelyne Braun, Marie-Paule Vallat, Patrick Miailhes, Christian Chidiac, Dominique Peyramond; Surgeons – Sébastien Lustig, Philippe Neyret, Olivier Reynaud, Caroline Debette, Adrien Peltier, Anthony Viste, Jean-Baptiste Bérard, Frédéric Dalat, Olivier Cantin, Romain Desmarchelier, Thibault Vermersch, Michel-Henry Fessy, Cédric Barrey, Francesco Signorelli, Emmanuel Jouanneau, Timothée Jacquesson, Pierre Breton, Ali Mojallal, Fabien Boucher, Hristo Shipkov; Microbiologists – Frederic Laurent, François Vandenesch, Jean-Philippe Rasigade, Céline Dupieux; Nuclear Medicine – Isabelle Morelec, Marc Janier, Francesco Giammarile; PK/PD specialists – Michel Tod, Marie-Claude Gagnieu, Sylvain Goutelle; Clinical Research Assistant – Eugénie Mabrut.
Contributors: FV wrote the case. FV, CC and TF performed the literature review and participated to the revision of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
on behalf of the Lyon Bone and Joint Infection Study Group:
Tristan Ferry, Thomas Perpoint, André Boibieux, François Biron, Florence Ader, Julien Saison, Florent Valour, Fatiha Daoud, Johanna Lippman, Evelyne Braun, Marie-Paule Vallat, Patrick Miailhes, Christian Chidiac, Dominique Peyramond, Sébastien Lustig, Philippe Neyret, Olivier Reynaud, Caroline Debette, Adrien Peltier, Anthony Viste, Jean-Baptiste Bérard, Frédéric Dalat, Olivier Cantin, Romain Desmarchelier, Thibault Vermersch, Michel-Henry Fessy, Cédric Barrey, Francesco Signorelli, Emmanuel Jouanneau, Timothée Jacquesson, Pierre Breton, Ali Mojallal, Fabien Boucher, Hristo Shipkov, Frederic Laurent, François Vandenesch, Jean-Philippe Rasigade, Céline Dupieux, Isabelle Morelec, Marc Janier, Francesco Giammarile, Michel Tod, Marie-Claude Gagnieu, Sylvain Goutelle, and Eugénie Mabrut
Collaborators: on behalf of the Lyon Bone and Joint Infection Study Group
References
- 1.Lerner PI. The lumpy jaw. Cervicofacial actinomycosis. Infect Dis Clin North Am 1988;2:203–20. [PubMed] [Google Scholar]
- 2.Valour F, Sénéchal A, Dupieux C et al. Actinomycosis: etiology, clinical features, diagnosis, treatment and management. Infect Drug Resist 2014:183–97 doi:10.2147/IDR.S39601.eCollection2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oostman O, Smego RA. Cervicofacial actinomycosis: diagnosis and management. Curr Infect Dis Rep 2005;7:170–4 doi:10.1007/s11908-005-0030-0 [DOI] [PubMed] [Google Scholar]