Abstract
Osgood-Schlatter disease is a common cause of anterior knee pain in adolescents. In a good proportion of cases the pain is relieved through stopping sport alone, or by doing so in conjunction with undertaking physiotherapy. However, resolution of symptoms may take several years. A proportion of teenagers are prevented from participating in sport for a prolonged period as a result of the condition, and some have persisting knee pain into adulthood. We report the use of a new surgical treatment for this disease. We describe the case of a 12-year-old boy who was unable to play rugby for a year due to this pain. Following percutaneous fixation of the tibial tuberosity his symptoms entirely resolved and he returned to competitive sport 6 weeks after surgery. A year later the screw was removed. As soon as he resumed sport his symptoms immediately returned and he requested that the screw be replaced. Following replacement his symptoms once more resolved.
Background
Osgood-Schlatter disease was first described independently by Robert Osgood and Carl Schlatter in 1903.1 It is a traction apophysitis of the insertion of the patellar tendon onto the tibial tuberosity at the knee, with slippage of the patella tendon insertion over pathological fibrocartilage.2 It is more common in boys than girls and generally presents between the ages of 10 and 14 years. Up to 20% of adolescent athletes will be affected. It is often bilateral but symptoms are most commonly asymmetrical. Pain is usually relieved by a physical therapy regime of activity modification and stretching exercises, but over half take more than 2 years to fully recover.3 Use of extracorporeal shock wave therapy is also an option. The condition will often resolve completely when the physis closes at skeletal maturity, but up to 10% have on-going knee pain as adults. College-aged adults who previously had Osgood-Schlatter disease as teenagers have been shown to have impaired knee function compared with controls who never had the condition.4 Surgical treatment in adults with on-going pain includes excision of any accessory ossicles formed under or inside the patella tendon insertion, sometimes with tubercle reduction osteotomy.5
If a technique can be shown to safely stabilise the tibial apophysis and quickly remove the pain, this would be of great benefit to young athletes whose symptoms have failed to settle with non-operative treatment.
Case presentation
We report the case of a 12-year-old boy who presented with a 1-year history of pain and tenderness at both the lower pole of the patella and the tibial tuberosity. There was no family history of this condition. His social history showed that he was a keen sportsman. He played competitive rugby both at school and for a local club. This involved approximately 3 h of training and 90 min playing matches each week. His symptoms had failed to respond to activity modification as advised by his general practitioner. He was referred to the children's physiotherapy team, and pursued a 6-month course of withdrawal from sport and regular stretching exercises. This eased his symptoms. However, once restrictions on his activity were relaxed he returned to competitive rugby and his symptoms recurred, with bilateral tibial tuberosity pain. The pain on the right deteriorated to the extent that it prevented him from playing rugby. His pain was troublesome during physical activities, but not at rest. His functional limitation interfered with school and recreational activities.
Investigations
Plain radiographs of the knees demonstrated osteochondrotic tibial tuberosities with the incidental finding of an abnormal appearance to the lower pole of the patella. The appearance of the patella was identical on radiographs of the contralateral knee. In subsequent radiographs it was seen to entirely resolve. It was interpreted to represent either resolving Sinding-Larsen-Johansson syndrome or a type I bipartite patella.
Differential diagnosis
Diagnoses considered for his symptoms were Osgood-Schlatter disease, or an impending avulsion fracture of the tibial tuberosity. The chronicity of his symptoms, the absence of displacement of the tuberosity fragment, the lack of callus formation and the failure of the pain to settle with rest over many months made an avulsion fracture rather unlikely. Osgood-Schlatter disease was the diagnosis most consistent with his symptoms, signs and images.
Treatment
A decision was taken to stabilise the tibial tuberosity with a single percutaneous screw inserted through the tuberosity, just distal to the attachment of the patella tendon (figures 1 and 2). At his first postoperative review, some 6 weeks following surgery he declared that his pain had entirely resolved. He returned to full activity and was able to resume competitive rugby without any pain at that stage.
Figure 1.

Lateral radiograph of right knee, November 2009, demonstrating an ostochondrotic appearance to the tibial tuberosity and either Sinding-Larsen-Johansson syndrome or a type I bipartite patella.
Figure 2.
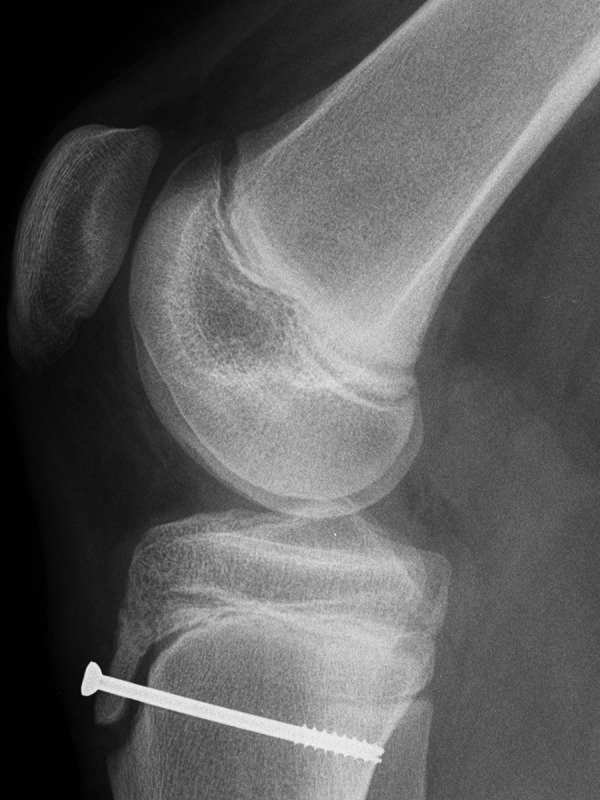
Lateral radiograph of right knee, April 2010, demonstrating the first screw passed across the tibial tuberosity.
Outcome and follow-up
Ten months following insertion of the screw, he remained entirely symptom free and was delighted with the result. A decision was then taken to remove the screw to avoid the potential for progressive recurvatum deformity that could theoretically result from tethering of the anterior part of the physis of the tibial plateau with on-going growth.
Unfortunately within weeks of removing this screw his original symptoms returned and indeed progressively worsened (figures 3 and 4). He was once more advised regarding activity modification and stretches. His symptoms were tolerable when he participated in low impact repetitive mobility exercises such as swimming and cycling, but whenever he tried to play rugby his pain became intolerable.
Figure 3.

Lateral radiograph of right knee, November 2011, following removal of the first screw.
Figure 4.

Sagittal MRI of the right knee, December 2011, demonstrating osteochondrosis of the tibial tuberosity consistent with Osgood-Schlatter disease.
For over a year he was very much restricted in his sporting activity and regularly requested to have the screw re-inserted. Fourteen months post removal the screw was replaced. An identical pattern of resolution occurred and he was able to return to rugby without restriction within 6 weeks. His proximal tibial physis has closed and he is entirely symptom free. The decision has been made not to remove the screw since it causes no problems. Clinical assessment shows no evidence for recurvatum as knee extension is symmetric and normal (5°), and plain radiographs again fail to show any evidence for recurvatum (figures 5 and 6).
Figure 5.
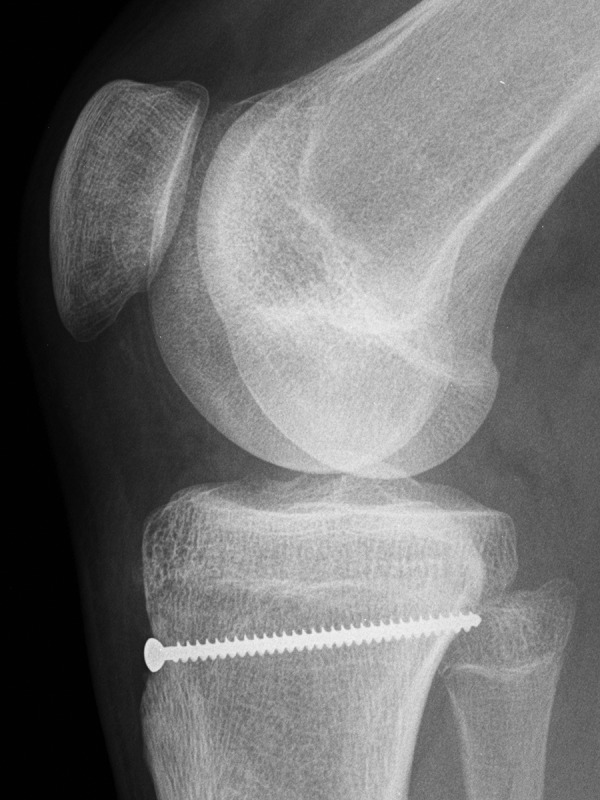
Lateral radiograph of the right knee, June 2013, demonstrating the second screw passed across the tibial tuberosity. There was no radiographic evidence of recurvatum at the tibial plateau.
Figure 6.

Lateral radiograph of the left knee, June 2013, for comparison.
Discussion
Osgood-Schlatter disease may respond well to conservative treatments such as stopping sports, physiotherapy and extracorporeal shock wave therapy.6 However, it can take several years for the symptoms to settle. This prevents adolescents from participating in the sports they enjoy. A proportion of accomplished junior athletes can find sporting activity is severely restricted by this condition. For this group it may be reasonable to consider tibial tuberosity stabilisation. The surgery can be performed through a 1 cm incision. In the case, surgery was highly effective and there were no long-term complications. We plan a prospective trial on a larger patient group to ensure the efficacy and safety of this treatment.
Learning points.
This is a new treatment for persistent Osgood-Schlatter disease of the knee.
It should only be used in children reaching the end of their skeletal growth.
In this case, symptoms completely resolved within 6 weeks of surgery.
Footnotes
Twitter: Follow Mark Latimer at @MDLatimer
Contributors: MDL operated on the patient and followed his progress in clinic. The idea for this novel surgery was his. The idea to write a report was his. The case report was first written by NN. The report was substantially revised by PDM.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Weiler R, Ingram M, Wolman R. 10-Minute consultation. Osgood-Schlatter disease. BMJ 2011;343:d4534 10.1136/bmj.d4534 [DOI] [PubMed] [Google Scholar]
- 2.Falciglia F, Giordano M, Aulisa AG et al. Osgood Schlatter lesion: histologic features of slipped anterior tibial tubercle. Int J Immunopathol Pharmacol 2011;24(1 Suppl 2):25–8. [DOI] [PubMed] [Google Scholar]
- 3.Kaya DO, Toprak U, Baltaci G et al. Long term functional and sonographic outcomes in Osgood-Schlatter disease. Knee Surg Sports Traumatol Arthrosc 2013;21:1131–9. 10.1007/s00167-012-2116-1 [DOI] [PubMed] [Google Scholar]
- 4.Ross MD, Villard D. Disability levels of college-aged men with a history of Osgood-Schlatter disease. J Strength Cond Res 2003;17:659–63. [DOI] [PubMed] [Google Scholar]
- 5.El-Husseini TF, Abdelgawad AA. Results of surgical treatment of unresolved Osgood-Schlatter disease in adults. J Knee Surg 2010;23:103–7. 10.1055/s-0030-1267474 [DOI] [PubMed] [Google Scholar]
- 6.Lohrer H, Nauk T, Scholl J et al. Extracorporeal shock wave therapy for patients suffering from recalcitrant Osgood-Schlatter disease. Sportverl Sportschad 2012;26:218–22. 10.1055/s-0032-1325478 [DOI] [PubMed] [Google Scholar]


