Abstract
This study aimed to evaluate the efficacy of random-start controlled ovarian stimulation (COS) in cancer patients for emergency fertility preservation. In this retrospective comparative study, 22 patients diagnosed with cancer and 44 infertile women undergoing conventional in vitro fertilization (IVF) were included. In cancer patients, ovarian stimulation was started on the day of referral, irrespective of their menstrual cycle date. The control group was selected by age matching among women undergoing conventional IVF. COS outcomes were compared between groups. The number of total and mature oocytes retrieved and the oocyte maturity rate were higher in the random-start group than in the conventional-start group. However, duration of ovarian stimulation was longer in the random-start group (11.4 vs. 10.3 days, P = 0.004). The addition of letrozole to lower the estradiol level during COS did not adversely affect total oocytes retrieved. However, oocyte maturity rate was lower in cycles with letrozole than in cycles without letrozole (71.6% vs. 58.2%, P = 0.019). Our study confirms the feasibility and effectiveness of random-start COS in cancer patients.
Graphical Abstract
Keywords: Controlled Ovarian Stimulation, Random-start, Fertility Preservation, Emergency, Cancer, In Vitro Fertilization Outcomes
INTRODUCTION
Fertility preservation is a continually evolving and important component of the comprehensive care of cancer patients as the survival rates of cancer patients and the interest in quality of life after cancer therapy have increased. In female cancer patients, various strategies have been used for fertility preservation: ovarian stimulation followed by cryopreservation of embryo or oocytes, ovarian suppression using gonadotropin-releasing hormone (GnRH) analogues, and ovarian tissue cryopreservation and transplantation. Among these techniques, both embryo and oocyte cryopreservation are considered as clinically established fertility preservation methods.
Controlled ovarian stimulation (COS) cycles for embryo or oocyte cryopreservation require 2-5 weeks. In a conventional stimulation regimen, ovarian stimulation is started during the early follicular phase of the menstrual cycle, and approximately 2 weeks of ovulation induction is required from the beginning. This may require up to 5 weeks of delay in starting cancer treatments, depending on the menstrual cycle phase at first consultation. In some cases, this delay is unacceptable because of the need for early cancer treatment. Because of this delay, patients may forgo fertility preservation or consider more experimental approaches.
To decrease the time for COS, initiating ovarian stimulation at random has been suggested, and some researchers have reported successful oocyte retrieval using this protocol (1, 2, 3). However, few studies have demonstrated the efficacy of this protocol compared with conventional stimulation (4, 5). In the present study, we aimed to determine the efficacy of "random-start COS" in cancer patients for emergency fertility preservation by comparing outcomes achieved with conventional-start therapy.
MATERIALS AND METHODS
Study design
This retrospective comparative study included patients diagnosed with cancer and prepared for gonadotoxic therapy (chemotherapy or radiotherapy) between August 2012 and December 2013 and infertile women undergoing conventional in vitro fertilization (IVF) in our institution. During the study period, 22 women were referred for fertility preservation and agreed to undergo COS for fertility preservation. No patients had previously undergone gonadotoxic treatments. In these patients, ovarian stimulation was started on the day of referral, irrespective of their menstrual cycle date, without awaiting menstruation. In the control group, conventional-start cycles were selected by age matching in a 1:2 ratio among women underwent their first IVF cycles under the GnRH antagonist protocol because of male, tubal, or uterine factor in our institution. Because many patients were under 30 yr of age compared with the control group, exact 1:2 ratio age matching was not possible. Therefore matching was classified as less than 30 yr old.
COS parameters and outcomes were compared between cycles in the random-start and conventional-start groups. This study was approved by the institutional review board of Seoul National University Bundang Hospital (B-1304-200-102). Written consent was not obtained. Because this was a retrospective chart review, we had difficulty contacting the subjects, and we determined that the risk to study subjects was minimal. Patient records and information were anonymized and deidentified before analysis. All clinical investigations were conducted according to the principles expressed in the Declaration of Helsinki.
Clinical management of cancer patients for fertility preservation
All the patients were evaluated for infertility risk based on their age and gonadotoxic treatment regimen and were counseled by an attending reproductive endocrinologist regarding various fertility-preserving strategies. Informed consents were obtained. Pelvis ultrasound and hormonal profiles including follicle-stimulating hormone (FSH), luteinizing hormone, estradiol (E2), progesterone (P4), and anti-Mullerian hormone (AMH) were evaluated. The phase of the menstrual cycle was evaluated based on the onset of the last menstrual period, ultrasonographic findings, and serum P4 concentrations. The early follicular phase was defined as within day 5 of the menstrual cycle, and the late follicular phase as after day 5 of the menstrual cycle with the emergence of a dominant follicle and serum P4 level <3 ng/mL. The luteal phase was determined by serum P4 level ≥3 ng/mL. All patients referred to our clinic did not have sufficient time for conventional fertility preservation; therefore, we initiated ovarian stimulation immediately regardless of their menstrual phase. Thus, we designated these cycles as "random-start" cycles.
COS protocols
After baseline pelvic ultrasound and hormonal evaluation, ovarian stimulation with GnRH antagonist protocol was commenced with recombinant FSH (Gonal-F; Serono, Geneva, Switzerland). The initial dose of gonadotropins was determined based on the patient's age and an assessment of ovarian reserve as estimated by antral follicle count (AFC) and/or AMH level. In the case of estrogen-sensitive tumors, an aromatase inhibitor, letrozole (Femara, 5 mg/day; Novartis, Suffern, NY), was used concomitantly with recombinant FSH until the day of triggering and then continued for a week after oocyte retrieval or until E2 levels decreased to less than 100 pg/mL. Once ultrasound monitoring revealed a dominant follicle ≥14 mm, a GnRH antagonist (Cetrorelix, 0.25 mg; Serono) was initiated. When at least 2 follicles had a mean diameter of ≥18 mm, final oocyte maturation was achieved with recombinant human chorionic gonadotropin (hCG; Ovidrel, 250 or 500 µg; Serono) or GnRH agonist (Decapeptyl, 0.2 mg; Ferring, Malmo, Sweden, or Leuplin, 3.75 mg; Takeda, Japan) at the clinician's discretion.
Oocyte retrieval was performed with transvaginal ultrasound guidance 36 hr after hCG triggering. Oocyte maturity was evaluated by microscopic examination and graded as mature (metaphase II), intermature (metaphase I), and immature. Mature oocytes and in vitro-matured oocytes were cryopreserved. For embryo banking, intracytoplasmic sperm injection was performed using ejaculated sperm. None of the male partners had subfertile sperm parameters. Fertilization was assessed by the presence of 2 pronuclei and a second polar body 16 to 18 hr after intracytoplasmic sperm injection. The quality of embryos was evaluated by morphological criteria based on the fragmentation degree and the regularity of blastomeres on day 3 after fertilization. All embryos were cryopreserved on day 3.
Conventional-Start COS
In conventional stimulation cycles performed for infertility treatments, ovarian stimulation was started on the second or third menstrual cycle date. GnRH antagonist was added to prevent premature ovulation when the lead follicle reached a mean diameter of 14 or 15 mm; oocyte maturation was achieved with hCG triggering.
Outcome measures
The main outcome measure was the number of total and mature oocytes retrieved after ovarian stimulation was started randomly or conventionally. Secondary outcome measures included the total gonadotropin dose needed and the number of days needed for ovarian stimulation from the day the stimulation was started to the day of oocyte retrieval.
Statistical analysis
Data were analyzed using SPSS software (version 20.0, Chicago, IL, USA) and compared by Mann-Whitney U, Kruskal-Wallis, or Fisher's exact tests as indicated. Descriptive data are expressed as median and ranges. The result was considered significant when the P value was less than 0.05.
Ethics statement
This study was approved by the institutional review board of Seoul National University Bundang Hospital (B-1304-200-102). Informed consent was waived by the board.
RESULTS
Patients were diagnosed with breast cancer (n=11), lymphoma (n=2), recurrent rectal cancer (n=1), endometrial cancer (n=1), malignant fibrous histiocytoma (n=1), colon cancer (n=1), advanced gastric cancer (n=1), myelodysplastic syndrome (n=1), brain tumor (n=1), ovarian cancer (n=1), or lung cancer (n=1). Among the 22 cancer patients, 5 women (22.7%) were married. In all cycles, COS was followed by oocyte retrieval. Oocyte and embryo cryopreservation were performed in 17 and 5 cycles, respectively. Fertilization rate (2 pronuclei/metaphase II oocytes) was 100%, and good-quality embryos (defined as having at least ≥5 cells and less than 20% fragmentation on day 3) were obtained in all 5 cases. Ovarian tissue was obtained during the surgical procedure for the primary cancer and was cryopreserved in 2 patients.
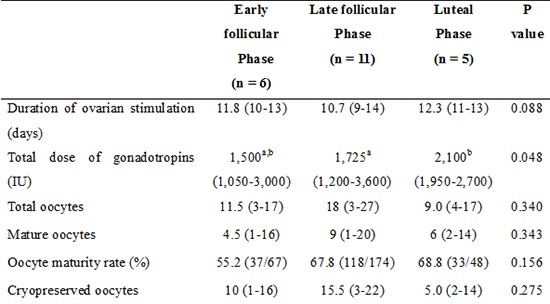
Table 1 compares the baseline characteristics, stimulation parameters, and outcomes in the random- (n=22) and conventional-start (n=44) groups. The age-matched conventional-start group consisted of women who had undergone tubal factor (n=27, 61.4%), male factor (n=15, 34.1%), and uterine factor infertility (n=2, 4.5%). There were no significant differences in age, body mass index (BMI), or AMH levels. The starting dose of gonadotropins and total gonadotropin dose were similar. However, duration of ovarian stimulation was 1 day longer in the random-start group (11.4 vs. 10.3 days, P=0.004). The number of total and mature oocytes retrieved and the oocyte maturity rate were higher in random-start cycles than in conventional-start COS cycles (11.5 vs. 7.4, P=0.030; 6.0 vs. 3.8, P=0.048; 65.1% vs. 51.0%, P<0.001, respectively).
Table 1.
Comparison of characteristics and outcomes of random-start and conventional-start GnRH antagonist IVF cycles
Data are presented as median (range). BMI body mass index; AMH anti-Mullerian hormone.
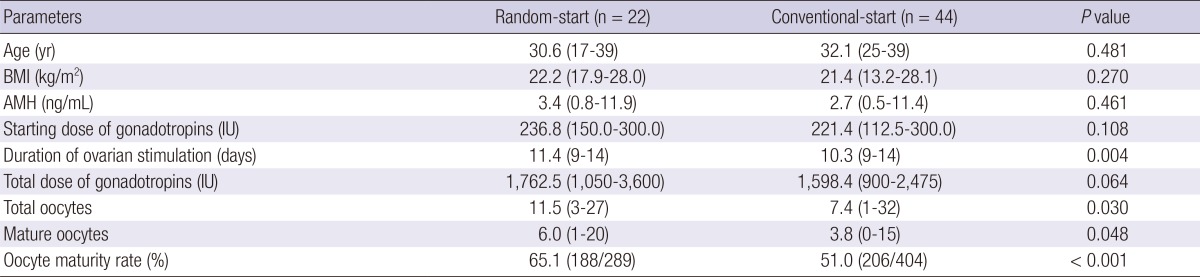
In random-start groups, ovarian stimulation was started in the early follicular (n=6), late follicular (n=11), and luteal phases (n=5). There were no significant differences in the age, BMI, AFC, or AMH in the 3 subgroups. Hormonal profiles on the day of initiation of ovarian stimulation are presented in Table 2. Although the starting dose of gonadotropins was similar in all groups, total gonadotropin dose was significantly higher in the luteal phase-start cycles than in late follicular phase-start cycles owing to longer stimulation (10.7 vs. 12.3 days). In luteal phase-start cycles, P4 levels decreased during COS from 12.4 ng/mL on the day of stimulation start to 0.9 ng/mL on the day of triggering. Two patients had their menses during COS. The number of total and mature oocytes retrieved and the oocyte maturity rates were similar irrespective of the start phase of ovarian stimulation.
Table 2.
Comparison of characteristics and outcomes according to the start phase of controlled ovarian stimulation
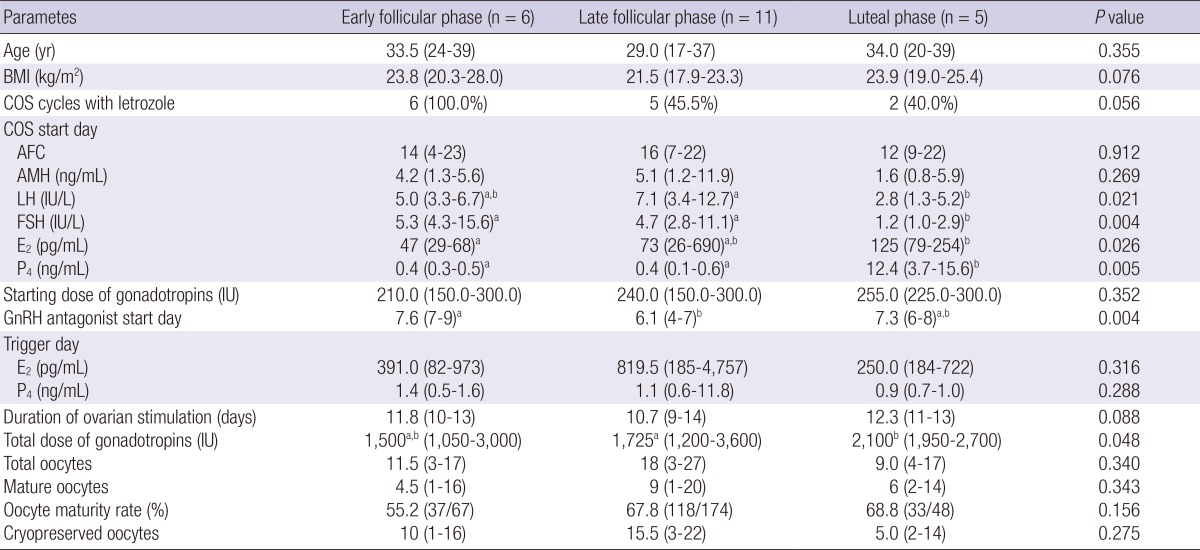
Data are presented as median (range). Data are compared by Kruskal Wallis and Mann Whitney U analysis. Different superscript means a statistical significance within the same row. BMI, body mass index; AFC, antral follicle count; AMH, anti-Mullerian hormone.
Letrozole was added to prevent a supraphysiologic E2 rise during COS in cases of estrogen-sensitive tumors such as breast or endometrial cancers. As shown in Table 3, patients undergoing ovarian stimulation with letrozole were nonsignificantly older (P=0.060) and had a nonsignificantly higher BMI (P=0.051) than did those without letrozole. As expected, the addition of letrozole resulted in significantly lower peak serum E2 levels. Use of letrozole did not affect the duration of ovarian stimulation, total dose of gonadotropins used, or the number of oocytes retrieved. However, the oocyte maturity rate was lower in cycles with letrozole than in those without letrozole (71.6% vs. 58.2%, P=0.019).
Table 3.
Comparison of outcomes of random-start COS cycles with or without letrozole
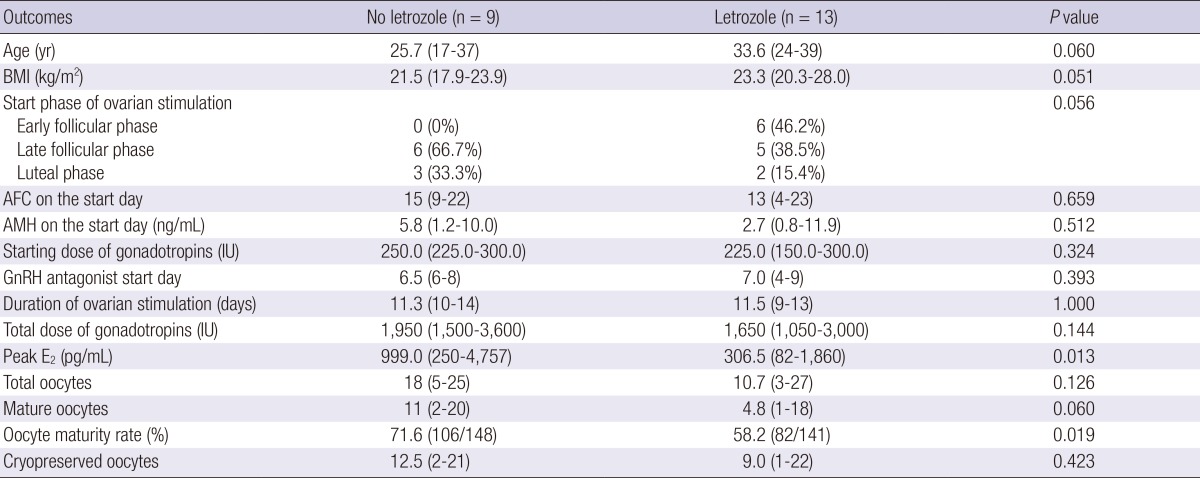
Data are presented as median (range). Data are compared by Mann Whitney U analysis. BMI, body mass index; AFC, antral follicle count; AMH, anti-Mullerian hormone.
Final oocyte maturation was induced with hCG (n=15) or GnRH agonist (n=7; triptorelin 0.2 mg in 2 patients and leuprorelin acetate 3.75 mg in 5 patients). Oocyte maturity was similar between cycles with hCG and GnRH agonist triggers (63.2% vs. 68.2%, P=0.444). Ovarian hyperstimulation syndrome (OHSS) developed in 2 patients. One patient developed severe OHSS with tense ascites and pleural effusion, despite the triggering that was achieved using GnRH agonist. Another patient developed moderate OHSS with the hCG trigger. They were hospitalized and managed conservatively.
DISCUSSION
In this study, we demonstrated that the random-start COS protocol was an effective method to overcome time constraints for fertility preservation. Oocytes were successfully retrieved regardless of the day of initiation of ovarian stimulation. The number of total and mature oocytes retrieved and oocyte maturity rates were not compromised in the random-start cycles. However, the duration of ovarian stimulation was longer in random-start cycles than in conventional-start cycles. The use of letrozole did not affect the number of oocytes retrieved, but the oocyte maturity rate was lower in letrozole cycles. Additionally, the GnRH agonist trigger did not adversely affect random-start COS outcomes.
To evaluate the efficiency of random-start COS cycles, we compared the outcomes of random-start cycles with those of conventional cycles in which ovarian stimulation was started on the second or third day of the menstrual cycle. Contrary to our expectations, the number of oocytes retrieved and oocyte maturity rate were lower in conventional cycles. It is generally assumed that infertile women have a reduced ovarian response for their age, despite the cause of infertility was neither ovulatory dysfunction nor decreased ovarian reserve. Our results suggest that at least the outcomes of random-start cycles were not compromised compared with those of conventional cycles.
Several case reports and comparative studies have described the outcomes of random-start cycles in cancer patients (1, 2, 3, 4, 5). Von Wolff et al. (5) reported a comparative study regarding outcomes of ovarian stimulation during the follicular versus luteal phases. In that study, 28 patients underwent stimulation in the follicular phase and 12 patients underwent stimulation in the luteal phase with GnRH antagonists and recombinant FSH. The luteal phase group and the follicular phase group showed similar stimulation outcomes such as duration of stimulation (10.6 days vs. 11.4 days), total dose of gonadotropins (2,255 IU vs. 2,720 IU), number of retrieved oocytes (13.1 vs. 10.0), maturation rates (83.7% vs. 80.4%), and fertilization rates (61.0% vs. 75.6%). Recently, Cakmak et al. (4) compared the outcomes of random-start COS with those of conventional COS. The number of total and mature oocytes retrieved (14.4 vs. 14.5 and 9.7 vs. 9.9), oocyte maturity rate (66% vs. 67%), and fertilization rates (72% vs. 87%) were not different between random- and conventional-start COS cycles. In addition, no difference was observed when comparing COS initiation in the late follicular and luteal phases. In line with the findings of earlier studies, we found that outcomes are similar between random-start COS and conventional-start COS.
In some centers, ovarian stimulation has been started with gonadotropins during the luteal phase at the same time with the use of a GnRH antagonist to downregulate luteinizing hormone and induce immediate luteolysis (1, 5). This protocol seems to be based on the concept of the local inhibitory effects of the corpus luteum and a high P4 level in the luteal phase of follicular development (6). However, our study revealed that presence of corpus luteum and a high P4 level at the beginning of ovarian stimulation in the luteal phase did not affect follicle development or oocyte quality. Our results and those of previous studies (2, 3, 4) indicate that in patients undergoing random-start IVF in the luteal phase, simultaneous initiation of GnRH antagonist and gonadotropins may not be necessary.
The traditional concept of folliculogenesis supports the recruitment of a single wave of antral follicles during the late luteal phase of the preceding menstrual cycle (7). A single follicle is selected during the beginning or middle stage of the follicular phase while the others undergo atresia (8). However, recent studies indicate multiple waves of follicle recruitment within a single interovulatory period (9, 10, 11). Moreover, the antral follicles observed in the late follicular or luteal phase may not necessarily be atretic, but rather may be in the early stages of follicular development (12). These findings are supported by the similar numbers of retrieved immature oocytes, maturation and fertilization rates, and total number of cryopreserved oocytes and embryos in in vitro maturation cycles performed during the follicular and luteal phases of the cycle (13, 14). In agreement with this newer concept of ovarian physiology, we demonstrated that ovarian stimulation can be started at a random cycle date.
In the present study, we added daily letrozole administration during ovarian stimulation to prevent supraphysiologically high E2 level in patients with estrogen-sensitive tumors (15). Thus far, the limited prospective data regarding the risk of breast cancer recurrence within 2 yr in patients undergoing COS are reassuring when compared with the data for women who do not undergo COS (16). We showed that the number of total oocytes retrieved, length of ovarian stimulation, and gonadotropin requirements were similar between cycles with and without letrozole. However, oocyte maturity rate was lower in the letrozole cycles, similar to an earlier report (15). The authors stated that considering the high percentage of immature oocytes in letrozole cycles, the triggering time should be delayed until the follicle reaches a mean diameter of >20 mm (15). On the contrary, recent report demonstrated that the use of letrozole in patients with estrogen-sensitive cancers did not adversely affect COS outcomes, including oocyte maturity (4). In our study, we cannot rule out the possibility that nonsignificantly older and higher BMI of the patients using letrozole negatively affect maturation rate. However, all of the 3 studies including the present study have too small number of subjects to make a solid conclusion of this issue.
The GnRH agonist trigger has previously been described for final oocyte maturation to prevent OHSS, but the problem of luteal-phase deficiency needed to be resolved (17). For COS cycles performed for fertility preservation or a donor in whom embryos are not transferred, a GnRH agonist can be a good alternative for hCG. In addition, especially for cancer patients, a GnRH agonist trigger for final oocyte maturation should be considered to avoid OHSS. The need to minimize the OHSS risk is particularly important in cancer patients, because OHSS could not only result in a delay of cancer treatment but also amplify the baseline risk for coagulopathy and other cancer-related morbidities (2, 18). Nonetheless, a GnRH agonist trigger cannot prevent OHSS entirely; therefore, ovarian stimulation should be performed with caution. We had a patient, aged 33, who experienced severe OHSS with tense ascites and pleural effusion despite the GnRH agonist trigger. Her AMH level was 11.92 ng/mL, and pelvic ultrasound revealed 22 AFCs on initial presentation. For this patient, ovarian stimulation was started in the late follicular phase using letrozole with 225 IU of gonadotropin as a starting dose. The gonadotropin dose was adjusted to 150 IU during cycles. Peak E2 level was 1,860 pg/mL, and 27 oocytes were retrieved. Considering that this COS cycle may be the only opportunity to preserve oocytes and that a GnRH agonist trigger could reduce the risk of OHSS, we suggest not lowering the starting dose of gonadotropins, with great care.
One case report demonstrated that a 3.75-mg triptorelin depot formulation efficiently promotes ovulation trigger because of the initial flare-up effect, leading to mature oocyte retrieval, with the advantage of initiating ovarian suppression for fertility preservation during adjuvant chemotherapy (19). We tried a depot GnRH agonist trigger (leuprorelin, 3.75 mg) for inducing final oocyte maturation and initiating ovarian suppression for ovarian protection against subsequent chemotherapy. Mature oocytes were retrieved successfully in all 5 patients. Oocyte maturity rate was 68%, comparable with the outcomes of the hCG trigger.
There have been concerns regarding the developmental competence of oocytes obtained after random-start cycles. A recent clinical study revealed promising results (20). A total of 242 infertile women started ovarian stimulation using hMG and letrozole during the luteal phase. The mean number of oocytes retrieved was 13.1, producing a mean of 4.8 highest quality embryos. The clinical pregnancy rate, ongoing pregnancy rate, and implantation rate of frozen embryo transfer were 55.46% (127/229), 48.91% (112/229), and 40.37% (174/431), respectively. The results of this study suggest that random-start ovarian stimulation can produce competent oocytes with optimal pregnancy outcomes. Nonetheless, additional clinical studies are needed to assess the outcomes of a random-start protocol, especially in cancer patients.
The limitations of this study are that it is a retrospective design and that a relatively small number of cases were included. Our findings would be strengthened by a prospective study with a larger number of cases.
In summary, this study confirmed the feasibility and effectiveness of random-start COS. This protocol allowed oocyte retrieval in cancer patients within 2 weeks, irrespective of the day of menstrual cycle on first consultation, without compromising IVF outcomes. This would minimize delays in treatment and enable more patients to achieve fertility preservation.
Footnotes
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI12C0055).
The authors have no conflicts of interest to declare in relation to this article.
Conception and coordination of the study: Lee JR. Design of ethical issues: Kim JH, Lee JR. Acquisition of data: Kim JH, Kim SK, Lee HJ, Lee JR. Data review: Kim SK, Lee HJ, Jee BC, Suh CS, Kim SH. Statistical analysis: Kim JH, Kim SK. Manuscript preparation: Kim JH, Kim SK, Lee HJ, Lee JR. Manuscript approval: all authors.
References
- 1.Bedoschi GM, de Albuquerque FO, Ferriani RA, Navarro PA. Ovarian stimulation during the luteal phase for fertility preservation of cancer patients: case reports and review of the literature. J Assist Reprod Genet. 2010;27:491–494. doi: 10.1007/s10815-010-9429-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nayak SR, Wakim AN. Random-start gonadotropin-releasing hormone (GnRH) antagonist-treated cycles with GnRH agonist trigger for fertility preservation. Fertil Steril. 2011;96:e51–e54. doi: 10.1016/j.fertnstert.2011.04.079. [DOI] [PubMed] [Google Scholar]
- 3.Sönmezer M, Türkçüoğlu I, Coşkun U, Oktay K. Random-start controlled ovarian hyperstimulation for emergency fertility preservation in letrozole cycles. Fertil Steril. 2011;95:2125.e9–2125.e11. doi: 10.1016/j.fertnstert.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 4.Cakmak H, Katz A, Cedars MI, Rosen MP. Effective method for emergency fertility preservation: random-start controlled ovarian stimulation. Fertil Steril. 2013;100:1673–1680. doi: 10.1016/j.fertnstert.2013.07.1992. [DOI] [PubMed] [Google Scholar]
- 5.von Wolff M, Thaler CJ, Frambach T, Zeeb C, Lawrenz B, Popovici RM, Strowitzki T. Ovarian stimulation to cryopreserve fertilized oocytes in cancer patients can be started in the luteal phase. Fertil Steril. 2009;92:1360–1365. doi: 10.1016/j.fertnstert.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 6.McNatty KP, Hillier SG, van den Boogaard AM, Trimbos-Kemper TC, Reichert LE, Jr, van Hall EV. Follicular development during the luteal phase of the human menstrual cycle. J Clin Endocrinol Metab. 1983;56:1022–1031. doi: 10.1210/jcem-56-5-1022. [DOI] [PubMed] [Google Scholar]
- 7.Pache TD, Wladimiroff JW, de Jong FH, Hop WC, Fauser BC. Growth patterns of nondominant ovarian follicles during the normal menstrual cycle. Fertil Steril. 1990;54:638–642. doi: 10.1016/s0015-0282(16)53821-7. [DOI] [PubMed] [Google Scholar]
- 8.Hodgen GD. The dominant ovarian follicle. Fertil Steril. 1982;38:281–300. [PubMed] [Google Scholar]
- 9.Baerwald AR, Adams GP, Pierson RA. A new model for ovarian follicular development during the human menstrual cycle. Fertil Steril. 2003;80:116–122. doi: 10.1016/s0015-0282(03)00544-2. [DOI] [PubMed] [Google Scholar]
- 10.Baerwald AR, Adams GP, Pierson RA. Characterization of ovarian follicular wave dynamics in women. Biol Reprod. 2003;69:1023–1031. doi: 10.1095/biolreprod.103.017772. [DOI] [PubMed] [Google Scholar]
- 11.de Mello Bianchi PH, Serafini P, Monteiro da Rocha A, Assad Hassun P, Alves da Motta EL, Sampaio Baruselli P, Chada Baracat E. Review: follicular waves in the human ovary: a new physiological paradigm for novel ovarian stimulation protocols. Reprod Sci. 2010;17:1067–1076. doi: 10.1177/1933719110366483. [DOI] [PubMed] [Google Scholar]
- 12.Baerwald AR, Adams GP, Pierson RA. Ovarian antral folliculogenesis during the human menstrual cycle: a review. Hum Reprod Update. 2012;18:73–91. doi: 10.1093/humupd/dmr039. [DOI] [PubMed] [Google Scholar]
- 13.Demirtas E, Elizur SE, Holzer H, Gidoni Y, Son WY, Chian RC, Tan SL. Immature oocyte retrieval in the luteal phase to preserve fertility in cancer patients. Reprod Biomed Online. 2008;17:520–523. doi: 10.1016/s1472-6483(10)60239-8. [DOI] [PubMed] [Google Scholar]
- 14.Maman E, Meirow D, Brengauz M, Raanani H, Dor J, Hourvitz A. Luteal phase oocyte retrieval and in vitro maturation is an optional procedure for urgent fertility preservation. Fertil Steril. 2011;95:64–67. doi: 10.1016/j.fertnstert.2010.06.064. [DOI] [PubMed] [Google Scholar]
- 15.Oktay K, Hourvitz A, Sahin G, Oktem O, Safro B, Cil A, Bang H. Letrozole reduces estrogen and gonadotropin exposure in women with breast cancer undergoing ovarian stimulation before chemotherapy. J Clin Endocrinol Metab. 2006;91:3885–3890. doi: 10.1210/jc.2006-0962. [DOI] [PubMed] [Google Scholar]
- 16.Azim AA, Costantini-Ferrando M, Oktay K. Safety of fertility preservation by ovarian stimulation with letrozole and gonadotropins in patients with breast cancer: a prospective controlled study. J Clin Oncol. 2008;26:2630–2635. doi: 10.1200/JCO.2007.14.8700. [DOI] [PubMed] [Google Scholar]
- 17.Humaidan P, Kol S, Papanikolaou EG Copenhagen GnRH Agonist Triggering Workshop Group. GnRH agonist for triggering of final oocyte maturation: time for a change of practice? Hum Reprod Update. 2011;17:510–524. doi: 10.1093/humupd/dmr008. [DOI] [PubMed] [Google Scholar]
- 18.Cakmak H, Rosen MP. Ovarian stimulation in cancer patients. Fertil Steril. 2013;99:1476–1484. doi: 10.1016/j.fertnstert.2013.03.029. [DOI] [PubMed] [Google Scholar]
- 19.Cavagna M, Dzik A. Depot GnRH-agonist trigger for breast-cancer patient undergoing ovarian stimulation resulted in mature oocytes for cryopreservation: a case report. Reprod Biomed Online. 2011;22:317–319. doi: 10.1016/j.rbmo.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 20.Kuang Y, Hong Q, Chen Q, Lyu Q, Ai A, Fu Y, Shoham Z. Luteal-phase ovarian stimulation is feasible for producing competent oocytes in women undergoing in vitro fertilization/intracytoplasmic sperm injection treatment, with optimal pregnancy outcomes in frozen-thawed embryo transfer cycles. Fertil Steril. 2014;101:105–111. doi: 10.1016/j.fertnstert.2013.09.007. [DOI] [PubMed] [Google Scholar]


