Abstract
Aim:
To determine if the long terms effects of non-invasive home mechanical ventilation (NIHMV) in the elderly are as beneficial as in younger subjects for a dedicated non-invasive ventilation unit in a tertiary referral hospital within the UK.
Patients and Methods:
The study population included 256 patients who were successfully established on NIHMV between May 2009 and August 2013. Patients were divided into three groups according to age: group 1 (n=103) ≥75; group 2 (n=81) 65 -74; and group 3 (n=72) < 65 years of age. Initial assessments, both prior to starting NIHMV and at 12 month follow up were determined which included establishing the primary cause of respiratory insufficiency, measurement of arterial blood gas parameters, spirometry, overnight oximetry, and sniff nasal inspiratory pressure (SNIP) in those patients with neuromuscular disease. The number of hospital admissions in the year prior to starting NIHMV, and in the subsequent year, along with the number of days spent as an inpatient were ascertained as a measure of burden to local health care resources. Compliance with NIV at follow up, facilitated by recorded data within the ventilator software, was established along with an assessment of any reported side effects.
Results:
Group 3 had the most profound abnormalities in lung function and blood gas parameters at initial assessment with a trend towards a higher number of acute admissions. In absolute terms, there was a greater decline in the number of admissions for subjects in group 2 after being established on NIHMV. Although more subjects in group 3 had chest wall deformities, COPD or bronchiectasis, this group had the lowest number of subjects with neuromuscular disease. Improvements in gas exchange were most pronounced for group 3 subjects despite no significant differences in the selected ventilator settings across the 3 groups. For neuromuscular patients, when measured, SNIP pressures were lowest in group 3.
Conclusion:
NIHMV was effective and tolerated for all three age groups. There was an improvement in measured patient centred endpoints across all three age groups, all of whom benefited equally.
Keywords: Non-invasive ventilation, respiratory failure, elderly
INTRODUCTION
A more diverse patient group now benefit from non-invasive ventilation (NIV) for acute hypercapnic respiratory failure (AHRF) since its conception over two decades ago,1 and its role in this context is simply beyond reproof. Initially this form of supportive therapy was reserved almost exclusively for subjects with acute exacerbations of chronic obstructive pulmonary disease (COPD), and avoidance of tracheal intubation was achieved for many of these subjects.1 The recent BTS NIV audit highlighted just how much progress has been achieved. Impressively, across 130 hospitals and including 2490 patients, intubations were as low at 2.7%, and NIV was deemed to be effective in an overwhelming 69% of patients.2 Recent studies confirm and extend these observations, demonstrating benefits in other respiratory conditions such as restrictive lung disease3,4 and a variety of neuromuscular conditions.3–5 However, it is not clear if this progress in the acute setting has also translated to those subjects requiring domiciliary NIV, particularly for elderly subjects, and there has been a paucity of data available in more recent times to address this question.
With the development of more sophisticated interfaces, themselves serving to provide a more acceptable, safer and comfortable ventilator support, in conjunction with a broader repertoire of positive-pressure support systems, the patient population which now benefit from NIV has vastly expanded.6 Furthermore, dedicated non-invasive ventilation units which provide this care have developed over the last decade, now accepting patients with more significant blood gas abnormalities, and yet still maintaining outstanding patient outcomes. As a result, in our institution, admissions to intensive care for respiratory failure have not only diminished, but NIV units have facilitated a more timely discharge from the critical care environment.7 Many of these subjects are subsequently commenced on non-invasive home mechanical ventilation (NIHMV) in an effort to reduce subsequent hospital admissions, maintain quality of life, relieve chronic hypoventilation related symptoms, all of which ultimately serve to mitigate health care utilisation.
According to consensus guidelines, age, in and of itself, does not feature as a variable which should be considered as to whether commencing domiciliary NIV is appropriate.5,8 It has recently been reported that NIV is effective and safe in an elderly patient population, many of whom had multiple comorbidities, including significant cognitive impairment and acute delirium, at least in the context of acute presentations with respiratory insufficiency.9 However, when long term domiciliary ventilation in individuals over 75 years is considered, early reports did not report particularly favourable outcomes. This was primarily on the basis of a higher risk of neuropsychological impairment and difficulties adapting to the overall burden on NIHMV when compared to younger individuals.10 A subsequent study, although only including six patients over the age of 75, when evaluating similar endpoints, demonstrated more positive findings.11
Despite extensive published literature, and with the exception of only two Spanish studies which demonstrated efficacy of NIHMV in the elderly, the appropriateness of NIHMV in patients over 75 years has not been particularly thoroughly assessed in comparison to published research on the merit of acute NIV.12–13 Furthermore, with recent progress in the use of NIV in more general terms, it would be of interest if this is also reflected in the older age group, and in the long term domiciliary setting. We therefore aimed to ascertain how successful NIHMV is in the elderly, and across a breadth of underlying pathology, by evaluating endpoints which are of relevance to individual patients along with measures of health care utilisation. We hypothesised that, in line with overall progress in the use of NIV, elderly patients also benefit to the same degree as younger subjects, and that our efforts should not be curtailed on the basis of age alone when considering this form of supportive therapy in the long term.
METHODS
Patients and assessments
Two hundred and fifty six patients who were successfully initiated on domiciliary ventilation between May 2009 and August 2013 were included. Data was retrieved in a retrospective fashion using electronic records of clinic letters and case note retrieval. The underlying cause of respiratory insufficiency, arterial blood gas (ABG) measurements, overnight oximetry to ascertain if there was evidence of nocturnal hypoventilation, spirometry according to the criteria of the European Respiratory Society, and sniff nasal inspiratory pressure (SNIP) for those individuals with neuromuscular disease were all recorded. For overnight oximetry, if oxygen saturations were below 90% for more than 30% of the reading, this was considered to be significant hypoventilation according to local practice. A prediction of the patient's height was established in those subjects with kyphoscoliosis by substituting height for arm span.
Follow up after 12 months included repeat ABG parameters, repeat spirometry, adverse effects of NIV and on occasion repeat SNIP pressures for those subjects with neuromuscular disease. Compliance and tolerance to NIV was determined, primarily by “interrogating” of the NIV machine in order to establish the average numbers of hours used per night. Ventilator parameters, including inspiratory (IPAP) and expiratory (EPAP) pressures, mode of ventilation and difficulties with mask leak, if present at all, were documented. The number of hospital admissions, including the total number of days spent in hospital, in both the year before and in the subsequent year after starting NIV was available using internal electronic system databases.
Statistical analysis
Statistical analysis was performed using SPSS version 17.0 (SPSS inc., Chicago, IL, USA). Data are presented as mean values ± SD. Comparisons between groups were performed byANOVA with Bonferoni's multiple comparison test after confirming normality of the data by the D'Agostino-Pearson test. A p value of less than 0.05 was considered significant.
RESULTS
The relevant baseline patient characteristics are outlined in table 1 and underlying cause of respiratory insufficiency in table 2. In many cases, there were several potential causes of respiratory impairment, and judgement was made on a case by case basis as to the main culprit. In those patients whereby it was impossible to know with sufficient certainty which disease process was most relevant, the aetiology of the respiratory insufficiency was deemed to be multifactorial. Changes in the various endpoints after 12 months NIHMV is outlined in table 3.
Table 1.
Patient characteristics at initial presentation.
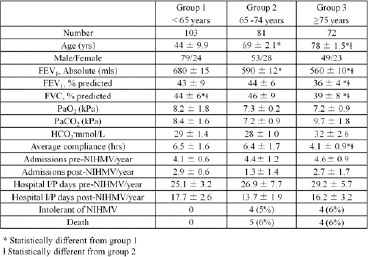
Table 2.
Underlying cause of respiratory insufficiency.
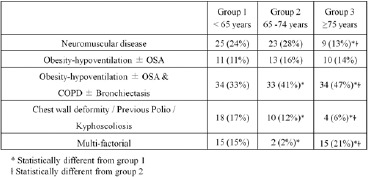
Table 3.
Improvement in gas exchange after 12 months.
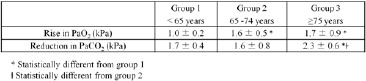
Four (6%) patients in group 3, 4 (6%) in group 2, and no subjects in group 1 were intolerant of NIHMV, all of whom returned their ventilator. Satisfactory compliance, arbitrarily defined as 4 hours NIV per night, was satisfactory across all three groups, although the average number of hours used was lowest in group 3. Over this period of time, there were no deaths in group 1, whereas there were 5 (6%) in group 2 and 4 (5%) in group 3. The number of hospital admissions, including number of inpatient days, was reduced in all three groups, with most benefit for subjects in group 2. Overnight oximetry was only assessed in those subjects deemed borderline for requiring NIV on the basis of blood gas parameters. All subjects included in table 1 met requirements for NIV on the basis of either evidence of nocturnal hypoventilation, or more commonly, measured hypercarbia at initial assessment when clinically stable. SNIP measurements, when measured for neuromuscular patients, were significantly lower for group 3 (26 ± 2 cmH2O) than for both group 1 (32 ± 3 cmH2O) and for group 2 (34 ± 6 cmH2O). There were no statistical differences in SNIP pressures between the latter two groups. On reviewing case notes, side effects were reported to similar degrees across the groups (data not shown).
DISCUSSION
NIHMV in the elderly is effective, tolerated, and with equally favourable outcomes when compared to younger subjects. NIHMV provided sustained improvement in gas exchange, reduced overall burden on health care resources, mitigated nocturnal hypoventilation, and with minimal adverse side effects reported. Overall tolerance and compliance to NIHMV was acceptable, and although 4 (6%) patients in the elderly group abandoned NIHMV, this was similar to those subjects in group 2. In those who were unable to tolerate NIV, the machine itself was returned.
Physiological parameters, social support, patient motivation, co-morbidities, and the projected natural history of the disease process itself all need to be taken into consideration when considering the appropriateness of embarking on long term NIHMV for individual patients. Obviously all of these elements are intimately related to each other, and it is not possible to dissect out any single variable in order to meaningfully conclude whether it, in isolation, should influence the decision whether to start NIHMV or not. With increasing age of patients who are now treated for respiratory failure, these decisions have now become increasingly more complex.
There were significant differences in the three groups with regard to the underlying cause of respiratory insufficiency, with a higher proportion of patients with neuromuscular disease, COPD or bronchiectasis in group 3. In contrast, there were few patients with chest wall deformities in group 3. It is difficult to interpret the clinical significance of these findings, but we feel it unlikely that such observations made any significant impact on our final conclusion. Despite this, it was of interest that those subjects in group 3, many of whom had COPD, had such a favourable response to NIHMV, particularly in the knowledge that it remains controversial if subjects with COPD alone benefit from NIHMV. This is currently being addressed in a large multicentre study, the HOT HMV study in COPD (UK Clinical Research Network Study ID:8059).
It is quite concerning that the absolute numbers of patients who fall into the obesity hypoventilation/OSA category across all groups is so much higher than previous reports.13 Our data substantiates the notion there is an alarming epidemic of obesity, and highlights its impact on healthcare utilisation, particularly for ventilation services. This observation, and the benefits of NIHMV for obese subjects, has been shown to improve quality of life.14
Overall improvement in gas exchange was greatest in group 3 in the context of minimal differences in the ventilator settings adopted (data not shown). Despite this observation, this finding did not translate into improved survival, or a disproportionate reduction in hospital admissions. However, this is perhaps not particularly surprising as subjects in group 3 had the lowest lung function parameters at baseline. Other outcomes in this group, such as hospital inpatient days and side effects, were similar to similar to those in group 1, itself a most positive finding. Keeping in mind the morphological and physiological respiratory changes that occur with advancing age, such as a decrease in alveolar air, loss of pulmonary capillaries and increased dead space, along with a greater likelihood of having unrelated respiratory co-morbidities, renders these outcomes overall to be very encouraging.
Age itself alone is clearly a poor marker of potential response of NIHMV. For the optimist we conclude that NIHMV improves gas exchange and reduces hospital admissions for elderly people. For the pessimist, we report that for the elderly group, who potentially should benefit disproportionately more from NIHMV when baseline variables are considered, the improvements, relatively speaking, seem to be somewhat blunted. However, when all aspects are considered, we should all agree that the decision making process as to the appropriateness of long term NIV, as complex as it may be, should not inadvertently lean towards excluding the elderly, as these individuals can potentially benefit to the same degree as their younger counterparts.
References
- 1.Meduri GU, Conoscenti CC, Menashe P, Nair S. Noninvasive face mask ventilation in patients with acute respiratory failure. Chest. 1989;95(4):865–870. doi: 10.1378/chest.95.4.865. [DOI] [PubMed] [Google Scholar]
- 2.British Thoracic Society. NIV Audit 2012. Available online from: https://www.brit-thoracic.org.uk/document-library/audit-and-quality-improvement/audit-reports/bts-adult-niv-audit-report-2012/2012. [Last accessed December 2014.] [Google Scholar]
- 3.Yokoyama T, Kondoh Y, Taniguchi H, Kataoka K, Kato K, Nishiyama O, et al. Noninvasive ventilation in acute exacerbation of idiopathic pulmonary fibrosis. Intern Med. 2010;49(15):1509–1514. doi: 10.2169/internalmedicine.49.3222. [DOI] [PubMed] [Google Scholar]
- 4.Tomii K, Tachikawa R, Chin K, Murase K, Handa T, Mishima M, et al. Role of non-invasive ventilation in managing life-threatening acute exacerbation of interstitial pneumonia. Intern Med. 2010;49(14):1341–7. doi: 10.2169/internalmedicine.49.3491. [DOI] [PubMed] [Google Scholar]
- 5.British Thoracic Society Standards of Care Committee. Non-invasive ventilation in acute respiratory failure. Thorax. 2002;57(3):192–211. doi: 10.1136/thorax.57.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sferrazza Papa GF, Di Marco F, Akoumianaki E, Brochard L. Recent advances in interfaces for non-invasive ventilation: from bench studies to practical issues. Minerva Anestesiol. 2012;78(10):1146–53. [PubMed] [Google Scholar]
- 7.Dave C, Turner A, Thomas A, Beauchamp B, Chakraborty B, Ali A, et al. Utility of respiratory ward-based NIV in acidotic hypercapnic respiratory failure. Respirology. 2014;19(8):1241–7. doi: 10.1111/resp.12366. [DOI] [PubMed] [Google Scholar]
- 8.Clinical indications for noninvasive positive pressure ventilation in chronic respiratory failure due to restrictive lung disease, COPD, and nocturnal hypoventilation--a consensus conference report. Chest. 1999;116(2):521–34. doi: 10.1378/chest.116.2.521. [DOI] [PubMed] [Google Scholar]
- 9.Laudisio A, Scarlata S, Pedone C, Cortese L, Zito A, Antonelli Incalzi R. Noninvasive ventilation in older adults admitted to a pneumogeriatric unit. J Am Geriatr Soc. 2014;62(6):1195–7. doi: 10.1111/jgs.12865. [DOI] [PubMed] [Google Scholar]
- 10.Chevrolet JC, Fitting JW, Knoblauch A, Domenighetti G. Schweiz Med Wochenschr. 1991;121(11):368–77. [Home mechanical ventilation in Switzerland in 1990. Future developments] [PubMed] [Google Scholar]
- 11.Janssens JP, Cicotti E, Fitting JW, Rochat T. Non-invasive home ventilation in patients over 75 years of age: tolerance, compliance, and impact on quality of life. Respir Med. 1998;92(12):1311–20. doi: 10.1016/s0954-6111(98)90135-4. [DOI] [PubMed] [Google Scholar]
- 12.Crespo A, Munoz X, Torres F, Marti S, Ferrer J, Morell F. Noninvasive home mechanical ventilation in elderly patients. Gerontology. 2010;56(2):150–6. doi: 10.1159/000237874. [DOI] [PubMed] [Google Scholar]
- 13.Farrero E, Prats E, Manresa F, Escarrabill J. Outcome of non-invasive domiciliary ventilation in elderly patients. Respir Med. 2007;101(6):1068–73. doi: 10.1016/j.rmed.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Crummy F, Piper AJ, Naughton MT. Obesity and the lung: 2. Obesity and sleep-disordered breathing. Thorax. 2008;63(8):738–46. doi: 10.1136/thx.2007.086843. [DOI] [PubMed] [Google Scholar]


