Abstract
Objectives. We (1) evaluated the impact of an evidence-based HIV prevention program with and without a parent component among mid-adolescents living in the Caribbean and (2) determined the effect of prior receipt of a related intervention during preadolescence on intervention response.
Methods. A randomized, controlled 4-cell trial of a 10-session, theory-based HIV prevention intervention involving 2564 Bahamian grade-10 youths (some of whom had received a comparable intervention in grade 6) was conducted (2008–2011). Randomization occurred at the level of the classroom with follow-up at 6, 12, and 18 months after intervention. The 3 experimental conditions all included the youths’ curriculum and either a youth–parent intervention emphasizing adolescent–parent communication, a parent-only goal-setting intervention, or no parent intervention.
Results. An intervention delivered to mid-adolescents in combination with a parent–adolescent sexual-risk communication intervention increased HIV/AIDS knowledge, condom-use skills, and self-efficacy and had a marginal effect on consistent condom use. Regardless of prior exposure to a similar intervention as preadolescents, youths benefited from receipt of the intervention.
Conclusions. Preadolescents and mid-adolescents in HIV-affected countries should receive HIV prevention interventions that include parental participation.
Evidence acquired over the course of the global HIV epidemic conclusively demonstrates that risk reduction can be achieved through interventions delivered in various venues at the individual, group, class, and community levels using a wide range of intervention approaches.1,2 Prevention researchers agree that even greater impact could be achieved by employing approaches that are multidimensional (defined here as delivered in different settings, using differing approaches or occurring at multiple times in an individual’s life, and integrated into a wide array of public health and educational efforts).3,4 Consequently, the next generation of prevention efforts will need to be correspondingly “highly active”5 and appropriately targeted.
Adolescents are of primary importance in curtailing the epidemic. The Joint United Nations Programme on HIV/AIDS (UNAIDS) has estimated that nearly one half of the world’s HIV infections have occurred among individuals aged 15 to 24 years.6 In the United States, individuals 15 to 29 years old, who represent one fifth of the total population, account for two fifths of new infections.7 Adolescence is a time of remarkable change in neural development, cognition, physical maturity, and social exposure. These changes have great impact on youths’ mood and impulse control, potential exposure to risk, and ability to comprehend the consequences of their actions.8–10 Adolescents are variably affected by family, peers, community (including neighborhood and school), and the wider sociocultural context in which they live,11–13 all of which can exert protective or risk influences.14 The relative impacts of these social forces change during adolescence, but parents remain prominent throughout.15–17 Accordingly, prevention efforts targeting adolescents require emphasis on parental involvement. Moreover, intervening with adolescents and parents together has been shown to reduce risk behaviors,18,19 leading intervention researchers to call for efforts to bring parents and adolescents together for at least 1 session.20
Although there is consensus regarding the importance of the multiple phases of adolescence in terms of HIV prevention,8 there is no consensus as to when adolescent interventions should be delivered: in preadolescence or early adolescence (ages 10 to 13 years, prior to the onset of most risk behavior, including consensual sexual activity), during mid-adolescence (ages 14 to 16 years, when some risk taking and experimenting has been initiated), or later in adolescence (ages 17 to 20 years, when many of the situations confronting youths are no longer theoretical).8,21–23 Some have argued that prevention interventions should not be conceptualized as something that can be completed as a stand-alone intervention; rather, they will need to be repeated over time.3 Repetition may be especially important for adolescents, given the rapid changes they are experiencing across multiple biological, social, and cognitive fronts.
HIV prevention efforts of the 21st century call for multidimensional interventions24,25; mounting such interventions in a fashion that permits assessment of effectiveness presents a formidable challenge. Settings with vibrant biomedical and community-based prevention and treatment efforts may offer the opportunity to examine the potential augmentative effects of school-based programs (with and without a parent component) offered across the adolescent period.
One such setting is the Commonwealth of The Bahamas, with the second-highest prevalence of HIV/AIDS in the Caribbean area, peaking at 5.5% in 1994. In partnership with the World Health Organization, the Pan American Health Organization, UNAIDS, and the President’s Emergency Plan for AIDS Relief, The Bahamas has reduced this rate to an estimated 3%, with a 39% decrease in new HIV and AIDS cases from 2001 to 2011,26 placing it among the 25 nations with the greatest decrease.25 This substantial decrease required a multidisciplinary, interagency approach. In 2009, the Bahamian Ministry of Health initiated a new National Health Systems Strategic Plan for 2010 through 2020, based on 7 strategic elements that include collaboration across public and private sectors working with communities to improve health and well-being, health care services focusing on prevention at all stages of life, and an emphasis on improved outcomes through an evidence-based approach to decision-making. The country hosts an aggressive educational, testing, and treatment program using multiple sources, including multimedia and a community-outreach service system.
In this setting, the Bahamian Ministries of Health and of Education have been collaborating with US investigators in the development and evaluation of school-based prevention efforts. As described in The Bahamas’ 2012 UN General Assembly Special Session report, the goal of the original collaborative effort
was to reach youth before the onset of sexual risk behavior. . . . The US–Bahamian research team evaluated the Bahamian adaptations of Focus on [Youth] which resulted in a 10-session adolescent HIV prevention program entitled “Focus on Youth in The Caribbean” (FOYC) and the 1-hour adapted parental monitoring intervention entitled “Caribbean Informed Parents and Children Together” (CImPACT). These adapted programs were evaluated through a randomized, controlled trial involving 1360 6 grade youth and 1175 of their parents. . . . The intervention effects across 3 years for knowledge, condom-use skills, perceptions and intentions regarding condoms and condom-use behavior are strong, with increases among FOYC youth showing significant improvements in most categories compared with youth receiving the control condition.26(pp24–25)
Accordingly, the Bahamian Ministry of Education incorporated FOYC plus CImPACT into the grade-6 curriculum in government schools throughout The Bahamas27 and decided to test an adapted version of FOYC (Bahamian Focus on Older Youth, or BFOOY) for use among grade-10 students. As a result of these actions, The Bahamas offers a unique opportunity to examine the impact of an HIV curriculum, delivered at either the grade-6 or grade-10 level or at both, in the context of a country with a robust HIV prevention and treatment program.
We examined the effect of a grade-10 HIV prevention program among participating youths overall and by gender, and according to prior exposure to a similar intervention in grade 6, in a country with substantial prevention efforts. We addressed 3 questions of significant public health relevance, both in The Bahamas and globally: (1) Does a school-based intervention targeting mid-adolescents improve knowledge, skills, perceptions, and practices about sexual-risk reduction overall? (2) What is the impact on sexual-risk knowledge, skills, perceptions, and practices of a parent component added to the youth intervention? (3) Does prior receipt of a similar intervention during early adolescence affect intervention effects among mid-adolescents, and if so, how?
METHODS
The data used for these analyses are from the 2564 Bahamian youths who participated in a randomized controlled trial, which we conducted evaluating the effectiveness of the adolescent HIV risk reduction intervention BFOOY. Per study protocol, the youths’ parents were also invited to participate and were randomized to receive a parental monitoring intervention (CImPACT), a goal-setting intervention (Goal for It [GFI]), or no intervention.
Interventions
FOYC (for grade-6 students) and BFOOY (for grade-10 students) are age-appropriate variations of a 10-session program based on a social cognitive model, protection motivation theory.28 FOYC and BFOOY include games, interactive discussions, role plays, and homework exercises to reinforce main messages and to increase knowledge and skills regarding risk avoidance. An ongoing story throughout the sessions focuses on a fictional family to contextualize decision-making and the importance of carefully considering the long-term consequences of actions.29 A decision-making model (Stop, Options, Decision, Action [SODA]) is accentuated throughout FOYC and BFOOY to provide guidance and practice in consequential thinking and action. Multiple exercises illustrating different communication styles emphasize the effective delivery of a message and the need to listen.
We derived the 2 parent interventions, CImPACT and GFI, from US interventions. CImPACT, adapted by the US and Bahamian research team from Informed Parents and Children Together (ImPACT), includes a 22-minute video followed by a discussion between the parent and youth.30 The video illustrates parent–child conversations about sex and provides correct information about HIV transmission and prevention, including a demonstration of condom use. Following the video, the parent and child engage in discussion and playacting to improve communication about difficult subjects and situations. The session concludes with the youth and parent practicing the correct use of condoms. GFI, which is also a 22-minute video delivered to parents, is about setting goals for career development. GFI describes and illustrates with examples the steps involved in career planning: establishing long-term goals, determining steps necessary to achieve one’s goals, establishing a plan to enact these steps, executing the plan, and reassessing progress. A parent–child discussion about these steps follows the video.
Evaluation of grade-10 intervention.
We conducted the randomized, controlled evaluation of BFOOY among youths in grade 10 in all government high schools (n = 7 in 2008; n = 8 in 2009) in New Providence, the most populous island of The Bahamas, with approximately 60% of the population. The control condition was the existing Bahamian Health and Family Life Education (HFLE) curriculum, which focuses on a range of health topics, including a factual presentation of HIV and pregnancy prevention and discussions of marriage and parenting. We randomized the 2564 participating students at the class level to 1 of 4 study conditions: BFOOY plus CImPACT, BFOOY plus GFI, BFOOY only, or HFLE only. (For a flowchart of student and school participation in the grade-6 and grade-10 interventions, see Figure A, available as a supplement to the online version of this article at http://www.ajph.org.)
The Bahamian research team delivered CImPACT and GFI to the parent and youth together in the evenings or weekends at the youth’s school.
Grade-6 intervention exposure (baseline enrollment in 2004 and 2005).
Because we examined the effect of prior participation in FOYC on the 2564 students who were in the grade-10 study of BFOOY, we briefly describe the grade-6 effectiveness trial of FOYC, which involved 15 of the 26 government elementary schools, on the island of New Providence. Ten of the 15 schools were randomized over 2 years to receive FOYC. The control comparison for FOYC was a 10-session ecology curriculum regarding the shoreline and wetlands.28 Relevant to the current study, all youths in the 10 intervention schools received FOYC and none of the youths in the remaining 16 schools received FOYC.
Measures
Condom-use self-efficacy.
We assessed a youth’s self-perceived ability to perform tasks to achieve protection through condom use through 5 items (e.g., “I could put on a condom correctly”). We measured each response on a 5-point Likert scale (1 = strongly disagree; 5 = strongly agree; α = 0.77–0.81). A composite score was calculated as a mean score across the 5 items (range = 1–5).
Condom-Use Skills Checklist.
The Condom-Use Skills Checklist31 assessed understanding of correct condom use. From among 16 items, students identified the 8 correct steps. We assigned 1 point for each item that was correctly marked (0 = incorrect; α = 0.50–0.66), resulting in a summary score of 1 to 16 for each participant.
HIV knowledge.
We used 16 true–false questions to assess knowledge of disease transmission, prevention, treatment, symptoms, and effects of HIV/AIDS. Correct responses were scored 1 (incorrect = 0; α = 0.55–0.62), resulting in a summary score of 1 to 16 for each participant.
Self-reported condom use.
To assess condom use, the questionnaire posed 2 questions to the youths: the last time they engaged in sex, did they use a condom (yes or no), and when they had sex, in general, how often did they use a condom (always, sometimes, or never).
Familiarity with the FOYC–BFOOY curriculum.
Youths were asked to identify the correct meaning of the acronym SODA (correct response = “Stop, Options, Decision, Action,” which is the decision-making model invoked throughout the FOYC–BFOOY curricula) from among 4 choices (correct = 1, incorrect = 0).
Data Analysis
We examined baseline differences between the 3 intervention groups and 1 control group using the χ2 test (for categorical variables) or analysis of variance (ANOVA) (for continuous variables). The means (including error bars) of scores for HIV/AIDS knowledge, condom-use skills, and condom-use self-efficacy, and the proportions of participants reporting consistent condom use, are displayed graphically in Figure 1 to indicate the longitudinal trends across the 4 intervention groups. To examine the effect of the intervention on these outcomes in this intention-to-treat analysis, we compared the change over time within each group and differences in mean scores and mean change scores (from baseline to 18 months) between the 4 groups, using repeated-measures ANOVA and regular ANOVA. To assess the effect of the intervention on students’ sexual behavior and condom use, we employed a χ2 test. Using mixed-effects models and generalized linear mixed model, we further assessed the effect of the intervention on knowledge, perceptions, and condom use, controlling for the dependence of repeated measures and the clustering effects of school. The mixed models included age, gender, intervention group, time (baseline and 6-, 12-, and 18-month follow-up), and interaction between intervention group and time.
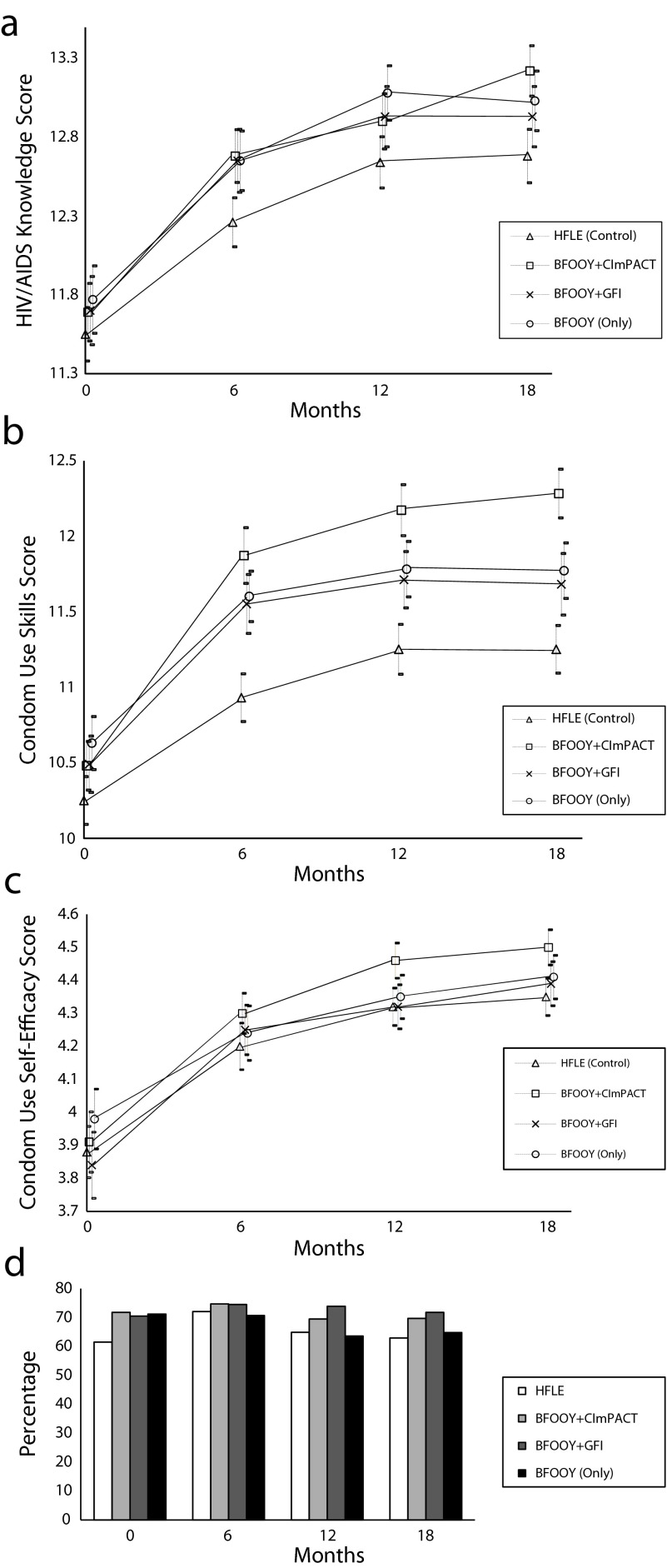
FIGURE 1—
Change through the 18-month intervention period, by intervention group, in mid-adolescents’ (a) HIV/AIDS knowledge, (b) condom-use skills, (c) condom-use self-efficacy, and (d) consistent condom use: The Bahamas, 2008–2011.
Note. HFLE = Health and Family Life Education; BFOOY = Bahamian Focus on Older Youth; CImPACT = Caribbean Informed Parents and Children Together; GFI = Goal for It.
To address the effect of prior exposure to FOYC, we conducted stratified analyses to explore differential intervention effects among youths who had and had not received FOYC in grade 6 and whose parents had or had not participated in the intervention, using ANOVA and the χ2 test. We controlled for baseline differences using logistic regression and multiple linear regression. We conducted a second set of mixed models that included “previous exposure to FOYC” to look at the impact of a similar intervention during early adolescence and intervention effects among mid-adolescents. We performed statistical analyses using the SAS 9.3 statistical software package (SAS Institute Inc, Cary, NC). We adopted a significance level of .05 in bivariate comparisons and multivariate analyses.
RESULTS
As shown in Table 1, among the 2564 grade-10 youths (1447 females [56.4%]) at baseline, 772 were in the control group (HFLE) and 1792 were randomized to 1 of the 3 BFOOY groups. The youths did not differ by age or gender, but a significantly higher percentage of the BFOOY-only group had received FOYC in grade 6 compared with all other groups and exhibited higher baseline condom-use skills than the control (HFLE) group. The 4 groups did not differ at baseline regarding HIV/AIDS knowledge, self-efficacy, sexual activity, or condom use. In the BFOOY plus CImPACT group, 76% of the youths (n = 664) and their parents attended the evening intervention session. In the BFOOY plus GFI group, 69% of the youths (n = 559) and their parents attended the evening intervention session. In the BFOOY only group (569 youths) and the 772 in HFLE group (772 youths), 68.4% and 71.5% of parents participated in the evaluation (but no parent intervention), respectively.
TABLE 1—
Mid-Adolescent Participants’ Baseline Demographic Characteristics, Previous Exposure to Focus on Youth in the Caribbean, Risk Behaviors, and HIV-Related Knowledge, Skills, and Perceptions, by Intervention Group: The Bahamas, 2008–2011
| Intervention Group |
|||||||
| Variables | Overall | HFLE | BFOOY Plus CImPACT | BFOOY Plus GFI | BFOOY Only | F or χ2 | P |
| Sample size, no. | 2564 | 772 | 664 | 559 | 569 | ||
| Age, y (SD) | 14.50 (0.71) | 14.55 (0.78) | 14.45 (0.67) | 14.51 (0.68) | 14.48 (0.66) | 2.38 | .068 |
| Gender, % | |||||||
| Male | 43.6 | 43.9 | 41.7 | 44.2 | 44.6 | 1.32 | .726 |
| Female | 56.4 | 56.1 | 58.3 | 55.8 | 55.4 | ||
| Exposure to FOYC in grade 6, % | 47.3 | 47.7 | 43.4 | 45.1 | 53.4 | 13.82 | .003 |
| Correctly answered SODA question, % | 41.1 | 38.3 | 41.5 | 40.9 | 44.5 | 5.31 | .151 |
| HIV-related knowledge, skills, and perceptions | |||||||
| HIV/AIDS knowledgea (SD) | 11.67 (2.47) | 11.55 (2.38) | 11.69 (2.37) | 11.70 (2.62) | 11.77 (2.55) | 0.94 | .42 |
| Condom-use skillsa (SD) | 10.45 (2.15) | 10.25 (2.19) | 10.48 (2.14) | 10.49 (2.19) | 10.63 (2.05) | 3.49 | .015 |
| Condom-use self-efficacyb (SD) | 3.38 (1.28) | 3.38 (1.28) | 3.34 (1.27) | 3.37 (1.30) | 3.43 (1.27) | 0.49 | .692 |
| Sexual activity and condom use | |||||||
| No. of sexually active youths at baseline | 509 | 145 | 130 | 104 | 130 | ||
| Ever had sex, % | 27.5 | 28.6 | 25.6 | 25.0 | 30.6 | 6.09 | .107 |
| Had sex in the last 6 mo, % | 22.3 | 21.9 | 21.5 | 20.9 | 25.0 | 3.22 | .359 |
| No. of sex partners, last 6 mo, % | |||||||
| 1 | 52.1 | 56.5 | 51.5 | 55.8 | 44.6 | 1.45 | .229 |
| 2 | 26.9 | 22.1 | 26.9 | 28.8 | 30.8 | ||
| ≥ 3 | 21.0 | 21.4 | 21.5 | 15.4 | 24.6 | ||
| Used a condom during last sexual episode, % | 76.5 | 70.3 | 78.3 | 77.0 | 81.9 | 7.46 | .059 |
| Consistent condom use, % | 68.2 | 61.5 | 71.8 | 70.5 | 71.2 | 6.24 | .101 |
Note. FOYC = Focus on Youth in the Caribbean; HFLE = Health and Family Life Education; BFOOY = Bahamian Focus on Older Youth; CImPACT = Caribbean Informed Parents and Children Together; GFI = Goal for It; SODA = Stop, Options, Decision, Action.
Score range 0–16.
Score range 1–5.
Effect of a School-Based Intervention For Mid-Adolescents
Effect on knowledge, perceptions, and condom-use skills.
Figure 1 depicts the change in HIV knowledge over 18 months after the intervention according to intervention group. Comparable at baseline, knowledge increased significantly among all groups throughout the follow-up. Six months after the intervention, HIV/AIDS knowledge was significantly higher in the 3 BFOOY intervention groups than in the HFLE group (F = 4.67; P = .003); at 18 months, it remained significantly higher in the BFOOY plus CImPACT group than in the HFLE group (F = 4.89; P = .002). Condom-use skills (Figure 1) increased significantly from baseline through 18 months. After being higher among BFOOY-only youths at baseline, 6 months later, condom-use skills were significantly higher in all 3 BFOOY groups than in the HFLE group (F = 18.77; P < .001). At 12 and 18 months, condom-use skills were highest in the BFOOY plus CImPACT group, followed by the BFOOY plus GFI and BFOOY-only groups, with the HFLE group demonstrating the lowest skills (at 12 months, F = 15.85; P < .001; at 18 months, F = 18.87; P < .001). The figure shows that condom-use self-efficacy, comparable at baseline, increased significantly among all groups over time; at 12 months, it was significantly higher in the BFOOY plus CImPACT group than in the HFLE group (F = 3.47; P = .016). More details are shown in Table A, available as a supplement to the online version of this article at http://www.ajph.org.
Effect on sexual-risk behavior.
Sexual initiation rose steadily (28% of youths reporting no prior sexual activity at baseline initiated sex during the 18 months of follow-up) and did not differ by intervention group. The proportion of youths reporting that they engaged in sex in the last 6 months rose steadily throughout the follow-up period (22% at baseline to 37% at 18 months) and did not differ significantly by intervention assignment (Table B, available as a supplement to the online version of this article at http://www.ajph.org).
Self-reported rates of condom use at the last episode of sex ranged from 77% to 83% and rates of consistent condom use ranged from 67% to 73% throughout the 18-month study period. These rates were not significantly different among the 4 groups at baseline or 6-, 12-, or 18-month follow-up (Figure 1; also, Table C, available as a supplement to the online version of this article at http://www.ajph.org).
Intervention effect by gender.
We also conducted analyses separately for females and males (Table D, available as a supplement to the online version of this article at http://www.ajph.org). At baseline, compared with males, females had higher levels of knowledge (11.8 vs 11.5 out of possible 16; t = 3.36; P < .001), lower condom-use skills (10.3 vs 10.6 out of possible 16; t = 3.70; P < .001) and self-efficacy (3.7 vs 4.2 out of possible 5; t = 11.92; P < .001), and higher rates of condom use (condom use in the sexual episode: 82.4% vs 73.9%; χ2 = 5.81; P = .016; consistent condom use: 74.9% vs 65.3%; χ2 = 5.88; P < .015).
Among males, there were no differences at baseline regarding knowledge, condom-use skills, self-efficacy, or condom use during the last sexual episode. Rates of consistent condom use were higher among BFOOY plus CImPACT and BFOOY-only youths than among HFLE youths. After the intervention, knowledge significantly increased among BFOOY plus CImPACT youths at 6 months and among BFOOY-only youths at 6 and 12 months. Compared with HFLE youths, BFOOY plus CImPACT youths had higher condom-use skills at all 3 follow-ups, with the BFOOY plus GFI and BFOOY-only groups also demonstrating some increase relative to the HFLE group. At 12 months, self-efficacy was higher among BFOOY plus CImPACT youths than among BFOOY-only youths. At 12 months, consistent condom use was higher among BFOOY plus GFI youths than among HFLE or BFOOY-only youths, whereas at 18 months it was higher among BFOOY plus CImPACT youths than among HFLE youths. Logistic regression analyses, which controlled for age and baseline difference in consistent condom use, indicated that consistent condom use was higher at 18 months among BFOOY plus CImPACT youths than among HFLE youths (adjusted odds ratio [AOR] = 3.85; 95% confidence interval [CI] = 1.72, 8.63; P = .001); consistent condom use was higher at 12 months among BFOOY plus GFI youths than among HFLE youths (AOR = 2.74; 95% CI = 1.13, 6.65; P = .026) and BFOOY-only youths (AOR = 2.70; 95% CI = 1.06, 6.88; P = .038).
Among females, knowledge significantly increased in the BFOOY plus CImPACT group compared with the HFLE group at 18 months only. Condom-use skills increased more in the BFOOY plus CImPACT group than in the HFLE group at all follow-up intervals, and in the BFOOY plus GFI group at 12-month and 18-month follow-up. Self-efficacy and condom use did not vary significantly between groups at any follow-up period.
Intervention impact of parent intervention exposure, controlling for baseline differences.
In Table 2, using 4 mixed models including a generalized linear mixed model, we compare the 3 intervention groups to the control group (HFLE) with regard to knowledge, condom-use skills, self-efficacy, and reported consistent condom use. Advanced age was associated with lack of improvement in HIV/AIDS knowledge and condom-use skills. Female gender was associated with increased HIV/AIDS knowledge, whereas male gender was associated with increased condom-use skills and self-efficacy.
TABLE 2—
Mixed Models Comparing 3 Intervention Groups With the Control Groups Regarding HIV/AIDS Knowledge, Condom-Use Skills, Self-Efficacy, and Consistent Condom Use: The Bahamas, 2008–2011
| HIV/AIDS Knowledge |
Condom-Use Skills |
Self-Efficacy |
Consistent Condom Use |
|||||
| Variables | β (95% CI) | t | β (95% CI) | t | β (95% CI) | t | β (95% CI) | t |
| Fixed effects | ||||||||
| Intercept | 18.129 (16.449, 19.808) | 23.15*** | 16.277 (14.729, 17.824) | 22.56*** | 4.497 (3.831, 5.163) | 14.48*** | 0.542 (0.074, 1.010) | 2.49* |
| Age | −0.366 (−0.471, −0.261) | −6.85*** | −0.357 (−0.453, −0.261) | −7.26*** | −0.020 (−0.061, 0.022) | −0.92 | 0.006 (−0.023, 0.035) | 0.39 |
| Male gendera | −0.362 (−0.508, −0.217) | −4.88*** | 0.435 (0.301, 0.568) | 6.37*** | 0.420 (0.362, 0.478) | 14.18*** | 0.002 (−0.040, 0.044) | 0.10 |
| Intervention groupb | ||||||||
| BFOOY plus CImPACT | 0.322 (0.042, 0.602) | 2.25* | 0.849 (0.581, 1.118) | 6.20*** | 0.081 (0.002, 0.161) | 1.99* | 0.070 (−0.011, 0.151) | 1.70 |
| BFOOY plus GFI | 0.184 (−0.108, 0.476) | 1.24 | 0.337 (0.058, 0.616) | 2.37* | −0.016 (−0.099, 0.068) | −0.37 | 0.076 (−0.011, 0.162) | 1.71 |
| BFOOY only | 0.201 (−0.092, 0.493) | 1.35 | 0.336 (0.056, 0.615) | 2.36* | 0.038 (−0.044, 0.121) | 0.91 | 0.032 (−0.052, 0.116) | 0.74 |
| Time | ||||||||
| Baseline | −1.044 (−1.233, −0.854) | −10.80*** | −0.958 (−1.146, −0.769) | −9.98*** | −0.517 (−0.557, −0.477) | −25.20*** | 0.016 (−0.057, 0.089) | 0.42 |
| 6-mo follow-up | −0.330 (−0.526, −0.133) | −3.29*** | −0.325 (−0.521, −0.129) | −3.25** | −0.166 (−0.207, −0.124) | −7.84*** | 0.099 (0.030, 0.169) | 2.79** |
| 12-mo follow-up | −0.015 (−0.214, 0.184) | −0.15 | −0.008 (−0.206, 0.190) | −0.08 | −0.049 (−0.090, −0.007) | −2.27* | 0.032 (−0.034, 0.097) | 0.95 |
| 18-mo follow-up: group × timec | −0.326 (−0.602, −0.050) | −2.31* | −0.743 (−1.015, −0.470) | −5.35*** | −0.047 (−0.155, 0.060) | −0.86 | −0.058 (−0.159, 0.044) | −1.12 |
| Random effects | ||||||||
| School | 0.041 (0.005, 0.087) | 1.74* | 0.057 (0.002, 0.112) | 2.03* | 0.001 (−0.002, 0.005) | 0.83 | 0.002 (−0.001, 0.004) | 1.28 |
| Student (nested within school) | 2.407 (2.218, 2.597) | 24.92*** | 1.898 (1.740, 2.056) | 23.57*** | 0.393 (0.363, 0.424) | 25.31*** | 0.081 (0.069, 0.093) | 13.76*** |
Note. CI = confidence interval; HFLE = Health and Family Life Education; BFOOY = Bahamian Focus on Older Youth; CImPACT = Caribbean Informed Parents and Children Together; GFI = Goal for It.
Female gender is the reference.
HFLE (the control group) is the reference.
Interaction between BFOOY plus CImPACT and time. 18-mo follow-up is the reference.
*P < .05; **P < .01; ***P < .001.
We found significant effects regarding knowledge, condom-use skills, and self-efficacy and marginally significant effects for consistent condom use among BFOOY plus CImPACT youths. Significant effects regarding condom-use skills and marginally significant effects for consistent condom use were found for BFOOY plus GFI youths. For BFOOY-only youths, we found significant effects for condom-use skills.
The BFOOY plus CImPACT × time interactions were significant for knowledge and condom-use skills. Mean scores for HIV/AIDS knowledge, condom-use skills, and self-efficacy at baseline and 6 months were significantly lower than mean scores at 18 months, indicating improvements in scores over time for each group. School random effects were significant in the models of HIV/AIDS knowledge and condom-use skills, indicating significant similarity in knowledge and skills among students in the same school and differences between schools.
Effect of Prior Exposure to Focus on Youth in The Caribbean
To explore the question of the impact of prior exposure to FOYC during preadolescence, we separately analyzed data from (1) the 1352 youths who attended 1 of the 10 schools in which FOYC was delivered to all grade 6-students and (2) the 1212 youths who attended 1 of the 16 schools that did not receive FOYC. Knowledge and condom-use self-efficacy test scores increased among both those who had and those who had not received FOYC (knowledge: 1.1 vs 1.2; t = 0.96; P > .05; condom-use self-efficacy: 0.5 vs 0.6; t = 1.70; P > .05). The increase in test scores for condom-use skills was significantly greater among those who had not received FOYC than those who had received FOYC (1.4 vs 1.1; t = 2.24; P < .05).
Among youths who had not been exposed to FOYC in grade 6, self-reported rates of condom use at the last episode of sex were significantly higher at 12-month follow-up in the BFOOY plus CImPACT and BFOOY plus GFI groups than in the HFLE and the BFOOY-only groups (χ2 = 9.5; P < .05; see Table E, available as a supplement to the online version of this article at http://www.ajph.org). The rates did not differ significantly at baseline or at 6- or 18-month follow-up. Logistic regression analysis controlling for age, gender, and baseline differences revealed a marginal intervention effect (OR = 2.2; 95% CI = 0.9, 5.3; P = .09). At 12- and 18-month follow-up, self-reported rates of consistent condom use were significantly higher among youths who received BFOOY plus CImPACT or BFOOY plus GFI than among those who received HFLE or BFOOY only (12 months: χ2 = 10.4; P < .05; 18 months: χ2 = 8.3; P < .05).
Among the subset of youths who had been exposed to the FOYC intervention in grade 6, rates of self-reported condom use did not differ on the basis of intervention assignment at any time interval from baseline through 18 months.
The mixed model analysis assessing the overall intervention effect and controlling for prior exposure (yes or no) to FOYC (Table 3) revealed that the BFOOY intervention remained a significant factor in all of the outcomes showing improvement; the effect of prior exposure to FOYC was significant only for condom-use skills. Even with this significant impact, the results were very similar to those produced without controlling for prior exposure of FOYC, suggesting that prior receipt of FOYC several years earlier (in grade 6) did not substantially alter the effectiveness of BFOOY (delivered in grade 10), especially BFOOY plus CImPACT.
TABLE 3—
Mixed Models Comparing 3 Intervention Groups With the Control Group Regarding HIV/AIDS Knowledge, Condom-Use Skills, Self-Efficacy, and Consistent Condom Use, Controlling for Previous Exposure to Focus on Youth in the Caribbean: The Bahamas, 2008–2011
| HIV/AIDS Knowledge |
Condom-Use Skills |
Self-Efficacy |
Consistent Condom Use |
|||||
| Variables | β (95% CI) | t | β (95% CI) | t | β (95% CI) | t | β (95% CI) | t |
| Fixed effects | ||||||||
| Intercept | 18.084 (16.399, 19.769) | 23.02*** | 16.113 (14.563, 17.663) | 22.29*** | 4.485 (3.816, 5.153) | 14.40*** | 0.524 (0.054, 0.994) | 2.39* |
| Age | −0.365 (−0.470, −0.260) | −6.82*** | −0.353 (−0.449, −0.256) | −7.17*** | −0.019 (−0.061, 0.023) | −0.90 | 0.007 (−0.023, 0.036) | 0.44 |
| Male gendera | −0.363 (−0.508, −0.217) | −4.89*** | 0.432 (0.299, 0.566) | 6.35*** | 0.420 (0.362, 0.478) | 14.17*** | 0.002 (−0.040, 0.044) | 0.09 |
| Previous exposure to FOYCb | 0.054 (−0.093, 0.201) | 0.72 | 0.196 (0.061, 0.332) | 2.85** | 0.015 (−0.043, 0.074) | 0.52 | 0.017 (−0.024, 0.059) | 0.81 |
| Intervention groupc | ||||||||
| BFOOY plus CImPACT | 0.319 (0.039, 0.600) | 2.23* | 0.843 (0.574, 1.111) | 6.15*** | 0.081 (0.001, 0.161) | 1.98* | 0.070 (−0.011, 0.151) | 1.69 |
| BFOOY plus GFI | 0.182 (−0.110, 0.474) | 1.22 | 0.330 (0.051, 0.609) | 2.32* | −0.016 (−0.099, 0.067) | −0.38 | 0.074 (−0.012, 0.161) | 1.68 |
| BFOOY (Only) | 0.202 (−0.090, 0.494) | 1.35 | 0.342 (0.062, 0.621) | 2.40* | 0.039 (−0.044, 0.122) | 0.93 | 0.032 (−0.052, 0.115) | 0.74 |
| Time | ||||||||
| Baseline | −1.044 (−1.234, −0.855) | −10.80*** | −0.959 (−1.147, −0.771) | −10.00*** | −0.517 (−0.557, −0.477) | −25.21*** | 0.015 (−0.058, 0.088) | 0.40 |
| 6-mo follow-up | −0.330 (−0.526, −0.134) | −3.29*** | −0.327 (−0.523, −0.131) | −3.27** | −0.166 (−0.207, −0.124) | −7.84*** | 0.099 (0.029, 0.169) | 2.78** |
| 12-mo follow-up | −0.015 (−0.214, 0.184) | −0.15 | −0.008 (−0.206, 0.189) | −0.08 | −0.049 (−0.090, −0.007) | −2.27* | 0.032 (−0.034, 0.097) | 0.95 |
| 18-mo follow-up: group × timed | −0.326 (−0.602, −0.050) | −2.31* | −0.743 (−1.015, −0.470) | −5.35*** | −0.047 (−0.155, 0.060) | −0.86 | −0.057 (−0.159, 0.045) | −1.10 |
| Random effects | ||||||||
| School | 0.041 (0.005, 0.087) | 1.74* | 0.056 (0.001, 0.110) | 2.01* | 0.001 (−0.002, 0.004) | 0.82 | 0.002 (−0.001, 0.004) | 1.23 |
| Student (nested within school) | 2.408 (2.218, 2.597) | 24.92*** | 1.891 (1.733, 2.048) | 23.53*** | 0.393 (0.363, 0.424) | 25.31*** | 0.081 (0.066, 0.097) | 13.76*** |
Note. CI = confidence interval; FOYC = Focus on Youth in the Caribbean; HFLE = Health and Family Life Education; BFOOY = Bahamian Focus on Older Youth; CImPACT = Caribbean Informed Parents and Children Together; GFI = Goal for It.
Female gender is the reference.
No prior exposure to FOYC is the reference.
HFLE (the control group) is the reference.
Interaction between BFOOY plus CImPACT and time. 18-mo follow-up is the reference.
*P < .05; **P < .01; ***P < .001.
DISCUSSION
The results of this longitudinal study are important for The Bahamas and for countries around the globe responding to the HIV epidemic.32 In the context of substantial national HIV prevention efforts, including a national school-based program (FOYC) delivered 4 years earlier (grade 6), a school-based intervention delivered in the high school years (BFOOY) in combination with a parent–adolescent sexual communication intervention (CImPACT) increase knowledge, condom-use skills, and perceptions, with marginally significant increases in self-reported condom use among Bahamian youths overall. Both genders derive significant benefits.
This finding that BFOOY plus CImPACT confers additional benefits beyond the effects of BFOOY only is consistent with our experience in the United States,2,30 with the FOYC grade-6 trial in The Bahamas,29,33,34 and with the literature on the role of parents in adolescent decision-making and risk reduction.18–20,35 The protective impact gained from including parents in adolescent risk reduction interventions potentially imposes a logistical and resource burden on implementing agencies. Participation in the CImPACT component required the parent and the adolescent, along with the CImPACT trainer, to return to the school setting during evenings or weekends. Indeed, in a subanalysis comparing the outcomes of FOYC plus CImPACT youths and parents who did participate in the CImPACT portion (70%) with the outcomes of those who did not (30%), participating youths showed greater improvement over the 18-month follow-up in condom-use skills (1.9 vs 1.4; t = 2.09; F = 4.38; P = .0369) and reported increased condom use at the last sexual episode at 6 months follow-up (88% vs 77%; OR = 4.32; 95% CI = 1.14, 16.35; P = .0315; supplemental Table F). These results underscore the importance of (1) including a session with parents and youths and (2) exploring options to deliver the intervention to parents and youths together in a manner that is respectful of their time and the community’s resources.
Compared with youths who had been exposed to FOYC in grade 6, those who had not been exposed showed greater improvement from the grade-10 intervention, although both groups improved. This finding is consistent with our earlier research36 that followed Bahamian youths who were enrolled in the grade-6 FOYC trial and whose data were available through grade 11; moreover, viewed from grade 6 through grade 11, the youths who received both FOYC and BFOOY showed the highest overall scores in condom-use skills.
In summary, the data suggest that substantial benefit can be gained by reintroducing these topics to youths when they have reached a different biological, cognitive, social, and experiential stage in their development.8–10
Potential Limitations
The results in this study are from the approximately two thirds of all grade-10 students attending 8 government high schools who agreed to participate in the study prior to the closing of enrollment when the desired sample size was reached; we cannot say whether they are representative of the one third who did not participate. However, we do know that youths who participated in the grade-6 FOYC trial, but not in the grade-10 BFOOY trial, did not differ substantially from youths who participated in both trials.37
The question of intervention “contamination” is a possibility in any study in which youths within the same school are receiving different interventions. To assess the presence of contamination, we assigned all classes in a comparison school to the control (HFLE) condition. Analysis of the 181 HFLE students in this school revealed that there were no differences in response to the SODA model question (a proxy for exposure to the BFOOY curriculum) among the students in the HFLE-only school whereas there were increases in the BFOOY–HFLE mixed schools. These data suggest that in the mixed schools, contamination of HFLE classes was occurring. However, such contamination would only serve to decrease the apparent BFOOY intervention impact.
Failure to find an intervention effect on condom use at last episode of sexual activity may result from a “ceiling effect” given the overall high rates of self-reported condom use (approximately 80%) throughout the study period. Finally, behavioral outcomes were self-reported and thus subject to recall or social-desirability bias.
Current Public Health Implications
The Bahamian Ministries of Education and of Health have carefully reviewed the data regarding the relative impacts of the various in-school interventions with and without the addition of a parent intervention. BFOOY and FOYC will continue to be a part of the grade-6 and possibly the grade-10 curricula. There remains considerable enthusiasm for implementation of FOYC and BFOOY with CImPACT. Currently, discussions are focused on mechanisms for ensuring appropriate training for grade-6 and grade-10 teachers that are both affordable and effective. These discussions are being informed by the joint ongoing research.27,35
Acknowledgments
We appreciate the support provided by the National Institute of Mental Health (grant R01MH069229).
We thank the many students and parents who participated in the study, the wonderful teachers and school administrators who provided the training, and the many colleagues who helped us conduct the research.
Human Participant Protection
The research described in this study was approved by the Wayne State University institutional review board and the Princess Margaret Hospital Authority (Nassau, The Bahamas) institutional review board. Youths and parents provided their consent to participate in each trial.
References
- 1.Johnson BT, Scott-Sheldon LA, Huedo-Medina TB, Carey MP. Interventions to reduce sexual risk for human immunodeficiency virus in adolescents: a meta-analysis of trials, 1985–2008. Arch Pediatr Adolesc Med. 2011;165:77–84. doi: 10.1001/archpediatrics.2010.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Compendium of evidence-based HIV behavioral interventions. 2014. Available at: http://www.cdc.gov/hiv/prevention/research/compendium/index.html. Accessed October 28, 2014.
- 3.Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet. 2008;372(9639):669–684. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bertozzi SM, Laga M, Bautista-Arredondo S, Coutinho A. Making HIV prevention programmes work. Lancet. 2008;372(9641):831–844. doi: 10.1016/S0140-6736(08)60889-2. [DOI] [PubMed] [Google Scholar]
- 5.Holmes KK. King Kennard Holmes—chair of the Department of Global Health of the University of Washington. Interviewed by Marc Vandenbruaene. Lancet Infect Dis. 2007;7(6):516–520. doi: 10.1016/S1473-3099(07)70184-6. [DOI] [PubMed] [Google Scholar]
- 6. Joint United Nations Programme on HIV/AIDS. Report on the global AIDS epidemic 2008. August 2008. Available at: http://whqlibdoc.who.int/unaids/2008/9789291737116_eng.pdf. Accessed October 28, 2014.
- 7.Centers for Disease Control and Prevention. HIV among youth: 2011. Available at: http://www.cdc.gov/hiv/youth/pdf/youth.pdf. Accessed January 11, 2014.
- 8.Pedlow CT, Carey M. Developmentally appropriate sexual risk reduction interventions for adolescents: rationale, review of interventions, and recommendations for research and practice. Ann Behav Med. 2004;27(3):172–184. doi: 10.1207/s15324796abm2703_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinberg L. Risk taking in adolescence: new perspectives from brain and behavioral science. Curr Dir Psychol Sci. 2007;16(2):55–59. [Google Scholar]
- 10.Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability. Am J Psychiatry. 2003;160(6):1041–1052. doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jackson CA, Henderson M, Frank JW, Haw SJ. An overview of prevention of multiple risk behaviour in adolescence and young adulthood. J Public Health (Oxf) 2012;34(suppl 1):i31–i40. doi: 10.1093/pubmed/fdr113. [DOI] [PubMed] [Google Scholar]
- 12.Barrow FH, Armstrong MI, Vargo A, Boothroyd RA. Understanding the findings of resilience-related research for fostering the development of African American adolescents. Child Adolesc Psychiatr Clin N Am. 2007;16(2):393–413. doi: 10.1016/j.chc.2006.12.004. ix–x. [DOI] [PubMed] [Google Scholar]
- 13.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 14.National Research Council. The Science of Adolescent Risk-Taking: Workshop Report. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 15.Mayberry M. Adolescent Risk Behaviors: Considering the Influences and Interactions of Multiple Contexts. Ann Arbor: UMI Dissertation Publishing; 2011. [Google Scholar]
- 16.Willoughby T, Hamza CA. A longitudinal examination of the bidirectional associations among perceived parenting behaviors, adolescent disclosure and problem behavior across the high school years. J Youth Adolesc. 2011;40(4):463–478. doi: 10.1007/s10964-010-9567-9. [DOI] [PubMed] [Google Scholar]
- 17.Romer D, Stanton B. Feelings about risk and the epidemic diffusion of adolescent sexual behavior. Prev Sci. 2003;4(1):39–53. doi: 10.1023/a:1021734827116. [DOI] [PubMed] [Google Scholar]
- 18.Burrus B, Leeks KD, Sipe TA et al. Person-to-person interventions targeted to parents and other caregivers to improve adolescent health: a community guide systematic review. Am J Prev Med. 2012;42(3):316–326. doi: 10.1016/j.amepre.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Murry VM, Berkel C, Chen YF, Brody GH, Gibbons FX, Gerrard M. Intervention induced changes on parenting practices, youth self-pride and sexual norms to reduce HIV-related behaviors among rural African American youths. J Youth Adolesc. 2011;40(9):1147–1163. doi: 10.1007/s10964-011-9642-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lightfoot M. HIV prevention for adolescents: where do we go from here? Am Psychol. 2012;67(8):661–671. doi: 10.1037/a0029831. [DOI] [PubMed] [Google Scholar]
- 21.Clark-Lempers DS, Lempers JD, Ho C. Early, middle, and late adolescents’ perceptions of their relationships with significant others. J Adolesc Res. 1991;6:296–315. [Google Scholar]
- 22.Dixon SD, Stein MT. Encounters With Children: Pediatric Behavior and Development. 3rd ed. St Louis, MO: Mosby Inc; 2000. [Google Scholar]
- 23.Cromer B. Adolescent development. In: Kleigman R, Stanton B, St. Geme J, Schor N, Behrman R, editors. Nelson Textbook of Pediatrics. 19th ed. Philadelphia, PA: Elsevier; 2011. pp. 649–653. [Google Scholar]
- 24.US Dept of State. PEPFAR blueprint: creating an aids-free generation. 2012. Available at: http://www.pepfar.gov/documents/organization/201386.pdf. Accessed January 11, 2014.
- 25. Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic: 2012. Available at: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_with_annexes_en.pdf. Accessed January 11, 2014.
- 26. Commonwealth of The Bahamas. Global AIDS Response Progress Reporting. Monitoring the 2011 Political Declaration on HIV/AIDS Country Report 2012 (UNGASS 2012). Available at: http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_BS_Narrative_Report%5B1%5D.pdf. Accessed October 28, 2014.
- 27.Knowles V, Kaljee L, Deveaux L, Lunn S, Rolle G, Stanton B. National implementation of an evidence-based HIV prevention and reproductive health program for Bahamian youth. Int Electron J Health Educ. 2012;15(1):173–190. [PMC free article] [PubMed] [Google Scholar]
- 28.Rodgers R. Cognitive and physiological processes in fear appeals and attitude change: a revised theory of protection motivation. In: Caaioppi T, Petty R, editors. Social Psychology. New York, NY: Guilford Press; 1983. pp. 153–176. [Google Scholar]
- 29.Deveaux L, Stanton B, Lunn S et al. Reduction in human immunodeficiency virus risk among youth in developing countries. Arch Pediatr Adolesc Med. 2007;161(12):1130–1139. doi: 10.1001/archpedi.161.12.1130. [DOI] [PubMed] [Google Scholar]
- 30.Wu Y, Stanton B, Galbraith J et al. Sustaining and broadening intervention impact: a randomized controlled trial of three adolescent risk reduction intervention approaches. Pediatrics. 2003;111(1):e32–e38. doi: 10.1542/peds.111.1.e32. [DOI] [PubMed] [Google Scholar]
- 31.Stanton B, Deveaux L, Lunn S et al. Condom-Use Skills Checklist: a proxy for assessing condom-use knowledge and skills when direct observation is not possible. J Health Popul Nutr. 2009;27(3):406–413. doi: 10.3329/jhpn.v27i3.3383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Michielsen K, Chersich MF, Luchters S, De Koker P, Van Rossem R, Temmerman M. Effectiveness of HIV prevention for youth in sub-Saharan Africa: systematic review and meta-analysis of randomized and nonrandomized trials. AIDS. 2010;24(8):1193–1202. doi: 10.1097/QAD.0b013e3283384791. [DOI] [PubMed] [Google Scholar]
- 33.Chen XG, Lunn SJ, Deveaux L et al. A cluster randomized controlled trial of an adolescent HIV prevention program among Bahamian youth: effect at 12 months post-intervention. AIDS Behav. 2009;13(3):499–508. doi: 10.1007/s10461-008-9511-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gong J, Stanton B, Lunn S et al. Effects through 24 months of an HIV/AIDS prevention intervention program based on protection motivation theory among preadolescents in the Bahamas. Pediatrics. 2009;123(5):e917–e928. doi: 10.1542/peds.2008-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Forehand R, Armistead L, Long N et al. Efficacy of a parent-based sexual-risk prevention program for African American preadolescents: a randomized controlled trial. Arch Pediatr Adolesc Med. 2007;161(12):1123–1129. doi: 10.1001/archpedi.161.12.1123. [DOI] [PubMed] [Google Scholar]
- 36.Dinaj-Koci V, Chen X, Deveaux L et al. Developmental implications of HIV prevention during adolescence: examination of the long-term impact of HIV prevention interventions delivered in randomized controlled trials in grade six and in grade 10. Youth Soc. 2012 doi: 10.1177/0044118X12456028. Available at: http://yas.sagepub.com/content/early/2012/08/20/0044118X12456028.abstract. Accessed October 28, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stanton B, Chen X, Koci V et al. Effect of a grade 6 HIV risk reduction intervention four years later among students who were and were not enrolled in the study trial. J Adolesc Health. 2012;50(3):243–249. doi: 10.1016/j.jadohealth.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]