Abstract
To combat disparities in oral health and access to dental care among infants and toddlers, most state Medicaid programs now reimburse physician-based preventive oral health services, such as fluoride varnish applications. We used geospatial data to examine the distribution of dental and medical Medicaid providers of pediatric oral health services throughout North Carolina to determine if these services have improved access to care for Medicaid enrollees younger than three years old. We then used claims data to examine the association between distance from these practices and use of dental services for a cohort of approximately 1,000 young children. Among 100 counties, four counties had no physician-based preventive oral health services and nine counties had no dental practice. While children who lived further from the nearest dental practice were less likely to make dental visits, distance from physician-based preventive oral health services did not predict use. For young Medicaid enrollees, oral health services provided in medical offices can improve access and increase use.
Dental care is the greatest unmet health need for children,[1] with young children living in poverty experiencing more untreated decay than children living above the federal poverty level.[2] Shortages and uneven distribution of the dental workforce adversely affect access to care [3,4] and young Medicaid-enrollees encounter additional barriers to care because of dentists’ reluctance to accept Medicaid, often due to administrative hassle or low reimbursement, and see young children, which may be due to lack of training and being uncomfortable treating young children.[3,4,5,6] Despite recommendations that children visit a dentist by their first birthday, most states reported that fewer than 10 percent of children younger than age three years had a dental visit in 2007.[7,8]
Training medical primary care providers to deliver physician-based preventive oral health services in medical settings is one strategy to combat disparities in oral health and access to care among infants and toddlers living in poverty. The rationale for physician-based preventive oral health services is that children are more likely to visit physicians than dentists during the first three years of life because well-child medical visits are recommended to occur at nine, twelve, fifteen, eighteen, twenty-four, and thirty-six months of age.[9–13] The geographic barriers to preventive oral health services caused by dental workforce shortages and uneven distribution of dentists may be lessened by providing care in a setting young children visit frequently and in conjunction with well-child visits.
Physician-based preventive oral health services may include screening and risk assessment, parental oral health counseling, referral to dentists when needed, and fluoride varnish application.[11] Fluoride varnish is a powerful tool for preventing dental caries, commonly called tooth decay. Fluoride application is reimbursed by nearly all state Medicaid programs, and the US Preventive Services Task Force recommends that physicians apply fluoride varnish to all children ages five and younger.[12,14] Physician-based preventive oral health services increase the use of preventive oral health services among young Medicaid enrollees,[15,16] and receipt of physician-based preventive oral health services over multiple visits reduces restorative dental treatment and dentally related hospital visits.[17,18] Nationally, the number of providers delivering physician-based preventive oral health services is low, [19] however since 2000 the North Carolina Medicaid program has supported nearly one million visits with physician-based preventive oral health services.[15]
Research examining the association between distance to health care providers and use of health care services supports Hagerstrand’s distance decay theory,[20] in which use decreases as distance increases.[21–25] For children, there is less evidence to support the distance decay theory. Among children living in rural North Carolina, no association was observed between distance from providers and number of medical visits.[26] For adolescents enrolled in Iowa Medicaid, distance was not a barrier to orthodontic care.[27] However, only 3 percent of the sample received orthodontic care, and it is not known how distance may affect use of more common nonspecialty oral health services. Geospatial studies of dentists treating children and Medicaid enrollees report that urban and highly populated areas have more dentists.[28–30]
We tested the hypothesis that preventive oral health services conveniently located in medical offices and public health clinics would improve access to oral health services for infants and toddlers. First, we examined the geographic distribution of the dental and medical practices providing pediatric oral health services for Medicaid enrollees to determine if physician-based preventive oral health services have expanded the geographic availability of providers, and where. We then combined this geographic information with Medicaid claims for a cohort of approximately 1,000 infants and toddlers to test the hypothesis that distance from the nearest practice was inversely associated with dental visits and not associated with physician-based preventive oral health services.
Study Data And Methods
The study was approved by an Institutional Review Board. For a full description of the methods and results see the online Appendix.[31]
Framework
The framework guiding this study posits that the probability of making a dental visit is influenced by a multitude of factors relating to: structure (for example, distance to care and demographic characteristics); history (for example, preventive behaviors and past dental use); cognition (for example, dental knowledge and opinions); and expectations (for example, rewards and costs).[32] Many of these factors are less likely to affect a child’s probability of receiving physician-based preventive oral health services. For instance, a caregiver’s dental fear or uncertainty about the timing of a first dental visit is unlikely to affect his or her decision to take a child to well-child medical visits where physician-based preventive oral health services are provided. The success of physician-based preventive oral health services at improving access to preventive oral health services for Medicaid-enrolled infants and toddlers requires sufficient provider participation so that structural factors, such as distance to care, promote rather than deter use. This study examines how physician-based preventive oral health services have expanded the geographic availability of care and uses a unique combination of survey and claims data to model the relationship between distance from the nearest practice and use of physician-based preventive oral health services and dental visits, adjusting for additional factors described in the conceptual framework.
Geographic Distribution Of Practices
We obtained street addresses for 630 dental practices that had at least one paid Medicaid claim for a child younger than three years of age and street addresses for 409 medical practices having at least one paid claim for physician-based preventive oral health services (oral evaluation and fluoride varnish application) from the North Carolina Division of Medical Assistance for the calendar year 2009. Physicians are reimbursed about $50 per visit for physician-based preventive oral health services by the North Carolina Medicaid program, up to six times per child before 3.5 years of age. ArcMap 10.1 was used to geocode and plot practice locations at the street level.
Data from the 2010 American Community Survey provided information on the county-level population and the child poverty rate.[33] The number of practices seeing young Medicaid-enrollees in a county is likely affected by the number of young Medicaid-enrollees per county. Lacking a measure of the number of Medicaid-enrollees younger than three years per county, we used data from the American Community Survey to estimate demand for care by calculating the number of practices per 1,000 children younger than five years old in each county. Counties were grouped into four categories: 0 practices; less than 1 practice per 1,000 children; 1 to 1.9 practices per 1,000 children; and 2 or more practices per 1,000 children. We constructed categories that could be easily compared to the Health Resources and Services Administration’s definition of a dental health professional shortage area (1 provider:5,000 population) and 2009 estimates published by the National Center for Health Statistics (nationwide = 1:1,667 and North Carolina = 1:2,222).[34,35] We included categories with higher practice-to-population ratios (such as lower demand) because our denominator included only some of a practice’s potential patient population.
Distance To Care And Use
We used baseline data for 1,405 low-income child-caregiver dyads, primarily a mother and her child, from the Carolina Oral Health Literacy cohort study who were enrolled from July 2008–09 in seven North Carolina counties. Caregivers were eighteen years of age or older, English-speaking, and the primary caregiver to a healthy, Medicaid-eligible child age five years or younger.[36] Structured interviews covered a wide range of domains including demography, socioeconomic status, health literacy, and self-reported oral health status and behaviors. Data from structured interviews with caregivers were linked to Medicaid claims for 1,245 children during calendar years 2008, 2009, and 2010. We successfully geocoded home addresses for 1,000 dyads (80 percent match rate) to identify the closest medical and dental practices. We excluded pregnant women (n = 2), children with less than five months Medicaid enrollment (n = 46), and children ages thirty-seven months or older (n = 35).
Medicaid claims were used to construct two variables indicating whether or not a child had a dental visit or received physician-based preventive oral health services. Using ArcGIS Network Analyst, we calculated the driving time in minutes from each child’s home address to the nearest dental practice or medical practice providing physician-based preventive oral health services.
We compared variables relating to the aforementioned framework domains of structure, history, and cognition (no variables were available to measure expectations) for children who received and did not receive dental visits and physician-based preventive oral health services. Adjusted logistic regression models determined whether distance from the nearest practice affected receipt of a dental visit or physician-based preventive oral health services. Analyses were conducted with Stata 13 statistical software.
Limitations
We examined practices having one or more Medicaid claims for infants and toddlers, and the results of a study focused on practices that treat a higher volume of Medicaid patients may yield different results about geographic accessibility of care. On average, there were more dental practices per capita than medical practices, but solo practices are more common in dentistry.
Our regression analyses assume that children visit the nearest practice and that families use their own vehicle to travel there, but this assumption may not hold true for all families in our sample. We were unable to compare actual travel distance to assumed distance among users because our administrative claims lacked provider addresses. Children in our sample lived relatively close to practices, which may differ for those in more rural communities for whom the distance barrier may be more pronounced. Finally, our findings may have limited generalizability because we examined a nonprobability, convenience sample. Compared to the full state population, our sample was more likely to live in metropolitan counties with larger populations and a higher rate of child poverty.
Study Results
Geographic Distribution Of Practices
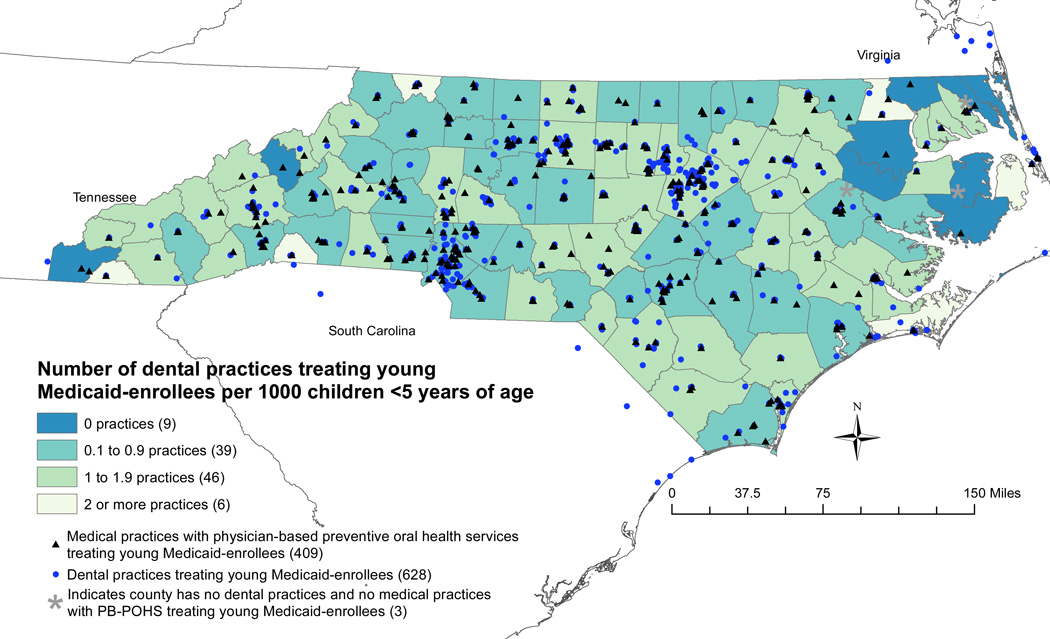
We successfully geocoded 409 medical practices with physician-based preventive oral health services (100 percent match rate) and 628 dental practices (99 percent match rate) serving North Carolina Medicaid-enrolled children ages three years and younger. The median number of physician-based preventive oral health services practices and dental practices per county was three. As Exhibit 1 illustrates, nine counties had no dental practices that treat young Medicaid enrollees. Among these counties, five had medical practices providing physician-based preventive oral health services (1.34 practices with physician-based preventive oral health services per 1,000 children, standard deviation (SD) = 1.39). Furthermore, the number of medical practices with physician-based preventive oral health services per 1,000 children younger than age five was greatest in the nine counties with no dental practices (mean = 1.33, SD = 1.39) and the six counties with two or more dental practices per 1,000 children (mean = 2.69, SD = 2.84). Counties with a dental practice-to-population ratio from 0.1 to 0.9 (n = 39) had a similar physician-based preventive oral health services-to-population ratio (mean = 0.95, SD = 0.58), while counties with 1.0 to 1.9 dental practices per 1,000 children younger than age five (n = 46) had on average a lower physician-based preventive oral health services practice-to-population ratio (mean = 0.93, SD = 0.67).
EXHIBIT 1.
Location Of Medical Practices Providing Physician-Based Preventive Oral Health Services And The Number Of County-Level Dental Practices Per 1,000 Children Ages Five Years Or Younger In North Carolina, 2009–10
Sources: Five-year estimates from the 2006–10 American Community Survey and practice addresses from the North Carolina Division of Medical Assistance during 2009.
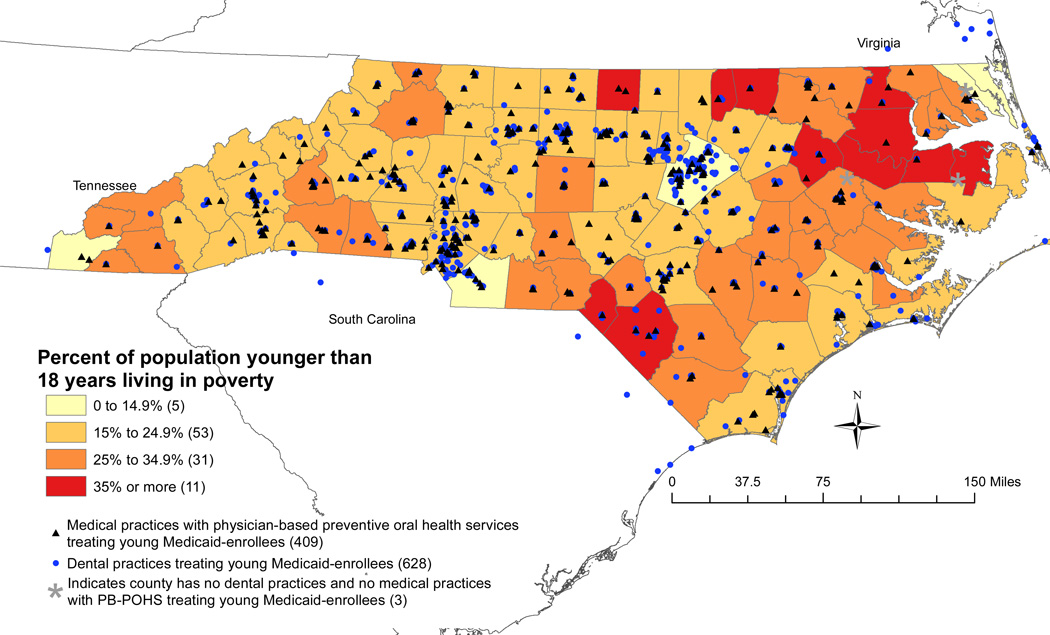
Exhibit 2 provides information on the child poverty rate and the location of medical and dental practices providing pediatric oral health services to young Medicaid-enrollees in each county. Counties with a child poverty rate of 35 percent or greater (n = 11) had 0.85 (SD = 0.67) dental practices and 0.82 (SD = 0.75) practices with physician-based preventive oral health services per 1,000 children on average. The three counties that had neither physician-based preventive oral health services nor dental practices had rates of child poverty of 10 percent, 38 percent, and 42 percent.
EXHIBIT 2.
Location Of Dental Practices And Medical Practices Providing Physician-Based Preventive Oral Health Services And The County-Level Percent of Population Younger Than 18 Years Of Age Living in Poverty In North Carolina, 2009–10
Source: Five-year estimates from the 2006–10 American Community Survey and practice addresses from the North Carolina Division of Medical Assistance during 2009.
Distance To Care And Use
We examined 917 child-caregiver dyads living in seventeen counties. Exhibit 3 illustrates that 483 dyads, or 53 percent of children, received physician-based preventive oral health services and 438 dyads, or 48 percent, had a dental visit during 2008–10. On average, children lived seven minutes (SD = 6) from the nearest dental practice and nine minutes from the nearest medical practice with physician-based preventive oral health services (SD = 7). Receipt of dental visits and physician-based preventive oral health services differed by child’s age, caregiver’s race, family size, and residence in a metropolitan county.
Exhibit 3.
Characteristics Of The Cohort Of Child-Caregiver Dyads, 2008–10
| Mean (standard deviation) or % | ||||
|---|---|---|---|---|
| No dental visit (n = 479) |
Dental visit (n = 438) |
No PB-POHS (n = 434) |
PB-POHS (n = 483) |
|
| Child received PB-POHS | 58.25% | 46.68%**** | 0.00% | 100.00%**** |
| Child had a dental visit | 0.00 | 100.00**** | 53.92 | 42.24**** |
| Minutes driving to nearest dental practice that sees Medicaid enrollees younger than three years old, mean (SD) | 7 (6) | 6 (5)** | 7 (5) | 7 (6) |
| Minutes driving to nearest practice with PB-POHS, mean (SD) | 9 (7) | 8 (7) | 9 (7) | 9 (7) |
| Child’s age | ||||
| younger than one year | 60.96% | 24.66%**** | 35.48% | 50.93%**** |
| one year | 21.09 | 24.43**** | 18.66 | 26.29**** |
| two years | 12.73 | 21.92**** | 20.28 | 14.29**** |
| three years and older | 5.22 | 29.00**** | 25.58 | 8.49**** |
| Caregiver’s race | ||||
| white | 38.62% | 42.92%** | 48.16% | 33.95%**** |
| African American | 39.25 | 42.69** | 38.71 | 42.86**** |
| American Indian | 20.25 | 13.93** | 11.52 | 22.36**** |
| Asian | 1.88 | 0.46** | 1.61 | 0.83**** |
| Caregiver is Hispanic | 7.93% | 8.90% | 9.45% | 7.45% |
| Number of children in family | ||||
| one | 46.76% | 31.74%**** | 32.03% | 46.38%**** |
| two | 29.02 | 37.90**** | 35.25 | 31.47**** |
| three | 12.73 | 19.63**** | 20.74 | 11.80**** |
| four or more | 11.48 | 10.73**** | 11.98 | 10.35**** |
| Months enrolled in Medicaid after enrolling in study, mean (SD) | 21.87 (5.56) | 23.98 (4.61)**** | 22.55 (5.90) | 23.17 (4.53) |
| Caregiver reports brushing child’s teeth daily | 62.00% | 84.02%**** | 75.81% | 69.57%** |
| Caregiver had dental visit in last year | 54.28% | 61.19%** | 56.68% | 58.39% |
| Caregiver had low health literacy | 19.21% | 14.61% | 15.21% | 18.63% |
| Caregiver had low oral health literacy | 25.05% | 23.97% | 22.12% | 26.71% |
| % population in census tract younger than eighteen years old living in poverty, mean (SD) | 31.64% (20.00) | 30.40% (21.40) | 27.26% (19.97) | 34.42% (20.77)**** |
| Live in a metropolitan county | 68.89% | 80.37%**** | 83.987% | 65.84%**** |
| Number of practices with PB-POHS per 1,000 children younger than five years old, mean (SD) | 0.54 (0.24) | 0.57 (0.22) | 0.58 (0.21) | 0.51 (0.25)**** |
| Number of dental practices that see Medicaid enrollees younger than three years old per 1,000 children younger than five years old, mean (SD) | 1.33 (0.26) | 1.27 (0.27)**** | 1.34 (0.26) | 1.27 (0.27)**** |
SOURCE Combination of national survey data, survey data from the Carolina Oral Health Literacy cohort study, and North Carolina Medicaid claims data, 2008–10.
NOTES Differences in variables between children with dental visits versus no dental visits and physician-based preventive oral health services versus no physician-based preventive oral health services were examined using chi-squared tests to compare proportions and t-tests to compare means. PB-POHS stands for physician-based oral health services. N = 917.
p <0.05
p <0.01
p <0.001
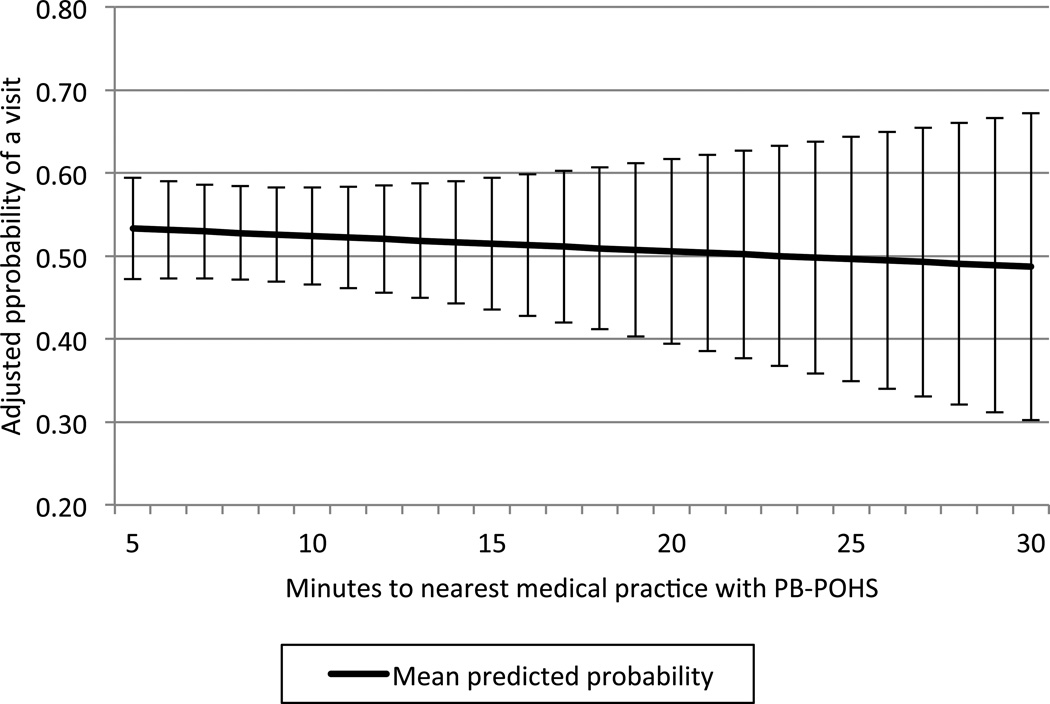
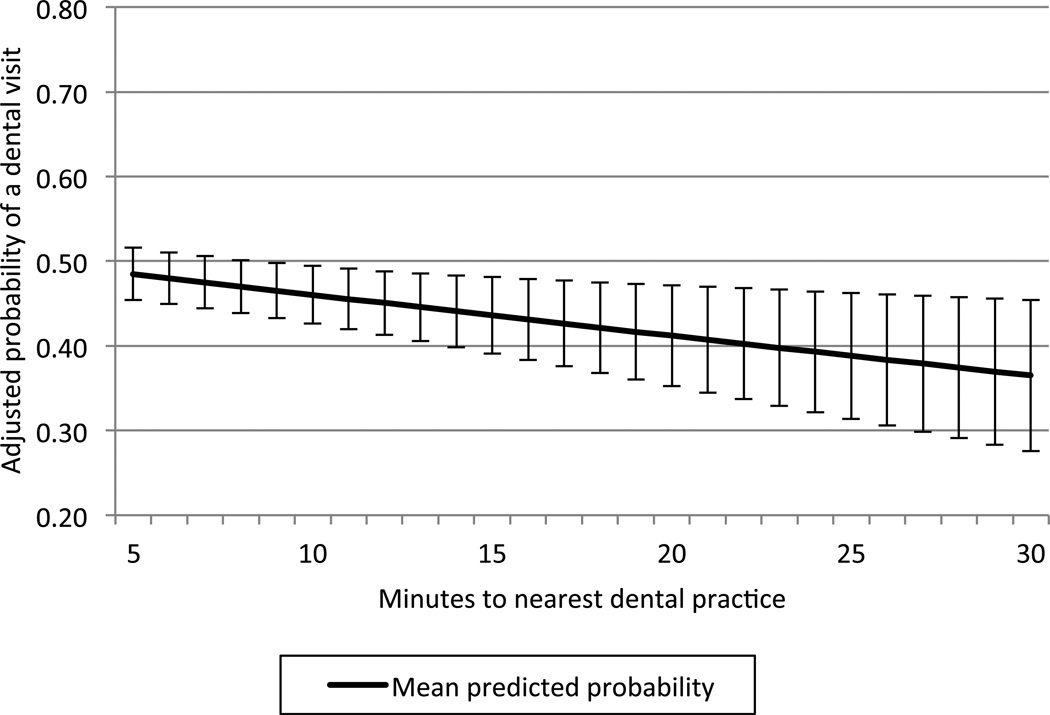
Exhibits 4 and 5 show the adjusted regression results examining the relationship between distance from Medicaid providers of pediatric oral health services and the probability of a visit. Exhibit 4 shows that distance from physician-based preventive oral health services was not associated with having a medical visit (coefficient = −0.01, p = 0.65). Exhibit 5 illustrates that living further from a dental practice was associated with a decreased likelihood of having a dental visit (coefficient = −0.03, p = 0.01). On average, the probability of a dental visit decreased from 46 percent (95 percent confidence interval (CI) = 43 percent, 59 percent) when ten minutes from the nearest dental practice to 37 percent (95 percent CI = 28 percent, 45 percent) when thirty minutes away, a 24 percent decline in the probability of a dental visit (p = 0.007). Results concerning the relationship between use and additional factors described in the conceptual framework are included in the online Appendix.[31]
EXHIBIT 4.
Effects Of Distance To Care On Probability Of Physician-Based Preventive Oral Health Services Among Infants And Toddlers Enrolled In North Carolina Medicaid, 2008–10
Source: Combination of national survey data, survey data from the Carolina Oral Health Literacy cohort study, and North Carolina Medicaid claims data, 2008–10. NOTES. Whisker marks represent 95% confidence intervals.
EXHIBIT 5.
Effects Of Distance To Care On Probability Of Dental Visit Among Infants And Toddlers Enrolled In North Carolina Medicaid, 2008–10
Source: Combination of national survey data, survey data from the Carolina Oral Health Literacy cohort study, and North Carolina Medicaid claims data, 2008–10. NOTES. Whisker marks represent 95% confidence intervals.
Discussion
In 2000 the North Carolina Medicaid program began reimbursing physician-based preventive oral health services to improve access to care for infants and toddlers. Our data underscore how physician-based preventive oral health services have expanded the geographic availability of preventive oral health services. Of the nine counties that lacked a dentist who treated infants and toddlers enrolled in Medicaid, five had physician-based preventive oral health services. Among the forty-two counties with equal to or greater than 25 percent of children living in poverty, 60 percent have as many or more practices providing physician-based preventive oral health services than dental practices that cared for the youngest Medicaid enrollees. Geographic disparities in access to care persist. The three counties without physician-based preventive oral health services or dental practices were located in the northeast. Counties with few dental practices tended to have few practices with physician-based preventive oral health services. The 39 counties with less than 1 dental practice per 1,000 children younger than 5 years of age also had an average of less than 1 physician-based preventive oral health services practice.
Our regression results indicated that greater distance to care was associated with decreased probability of dental visits. This was not true for physician-based preventive oral health services, likely because physician-based preventive oral health services can be provided during well- or sick-child medical visits, and thus the services require no additional effort from busy caregivers.[11,15] Although the effect of distance on use of dental care was modest, children in our sample lived on average less than ten minutes from the nearest dental practice, and the magnitude of this effect may increase in samples with a greater average distance to dental care. Unlike dental visits, physician-based preventive oral health services may be less affected by access barriers that may reinforce disparities, such as workforce shortages, providers’ reluctance to accept Medicaid, and parents’ value and knowledge of oral health. In North Carolina, the rate of physician-based preventive oral health services with fluoride application is nearly four times the rate of dental visits with fluoride application,[15] suggesting physician-based preventive oral health services can help to increase children’s use of oral health services, a leading health indicator in Healthy People 2020 and a 2014 core child health care quality measure for Medicaid.[37,38]
The United States Preventive Services Task Force recommends that physicians apply fluoride varnish as soon as a child’s first tooth comes in,[12] and national reports have promoted the integration of dentistry and medicine to promote child health.[9,10] Yet delivery of physician-based preventive oral health services is low nationally.[19] Although most state Medicaid programs reimburse varnish applications received in medical offices, few programs have adopted North Carolina’s model that includes an in-person American Medical Association–approved continuing medical education session on early childhood oral health and reimbursement for oral evaluation, risk assessment, caregiver counseling, and fluoride varnish application.[11,39] Moreover, North Carolina reimburses $50 for physician-based preventive oral health services compared to a reimbursement rate of $15 or less in some states.[39] Collectively, these factors may help to explain the high rates of provider participation in physician-based preventive oral health services in North Carolina.[15]
Although the Affordable Care Act lists pediatric dental care as one of ten essential health benefits, the law’s effect on oral health is uncertain because families are not required to purchase dental insurance in most states; there are no subsidies for dental insurance; and there are no provisions aimed at increasing dentist participation in Medicaid.[40,41] Dentists are essential for preventing, diagnosing, and treating oral diseases. This is an important public health service, especially for children, in whom untreated disease is associated with pain, decreased quality of life, and missed school days.[3] Strategies to increase the number of dentists treating infants and toddlers include enhanced training during dental school (for example, hands-on experience with infants) and afterwards through continuing education.[42] States might also use a geospatial algorithm to efficiently allocate dentists to unserved areas.[43]
As steps are taken to increase the number of dentists accepting Medicaid and treating infants and toddlers, physician-based preventive oral health services can help to fill gaps in care by using providers already living in or near these communities and serving these children. Physician-based preventive oral health services offer a convenient option for triage in areas with limited dental workforces. For instance, children at low risk of developing caries could receive physician-based preventive oral health services, while higher-risk children could be referred to dentists, an approach recommended by the American Academy of Pediatrics.[44]
Conclusion
This study underscores how physician-based preventive oral health services can help increase the geographic availability of oral health services for young Medicaid enrollees, enabling the delivery of oral health services in areas not served by a dental provider. Disparities associated with workforce availability and accessibility may be addressed in part by scaling-up state programs that train and reimburse physician-based preventive oral health services. Strong advocacy and bold leadership at national and state levels are needed to increase physician-based preventive oral health services programs and providers’ participation in these programs.
Supplementary Material
Acknowledgment
The Carolina Oral Health Literacy Project is supported by a grant from the National Institute of Dental and Craniofacial Research (Grant No. R01DE018045). Ashley M. Kranz was supported by a National Institutes of Health National Research Service Award Training for a New Interdisciplinary Research Workforce grant (Grant No. NIH/NIDCR 5T90DE021986-03).
Footnotes
An early version of this research was presented at the Oral Epidemiology Forum and the American Association for Dental Research Annual Meeting, both in Charlotte, North Carolina, in March 2014.
Notes
- 1.Newacheck PW, Hughes DC, Hung Y, Wong S, Stoddard JJ. The unmet health needs of America’s children. Pediatrics. 2000;105(4 Pt 2):989–997. [PubMed] [Google Scholar]
- 2.Dye BA, Li X, Thornton-Evans G. Hyattsville (MD): National Center for Health Statistics; 2012. [cited 2014 Oct 16]. Oral health disparities as determined by selected Healthy People 2020 oral health objectives for the United States, 2009–2010. [Internet]. Available from: http://www.cdc.gov/nchs/data/databriefs/db104.pdf. [PubMed] [Google Scholar]
- 3.Department of Health and Human Services. Washington (DC): HHS; 2000. [cited 2014 Oct 16]. Oral health in America: a report of the Surgeon General. [Internet]. Available from: http://www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/Documents/hck1ocv.@www.surgeon.fullrpt.pdf. [Google Scholar]
- 4.Government Accountability Office. Washington (DC): GAO; 2010. Nov, [cited 2014 Oct 16]. Oral health: efforts under way to improve children’s access to dental services, but sustained attention needed to address ongoing concerns. [Internet]. Available from: http://www.gao.gov/assets/320/312818.pdf. [Google Scholar]
- 5.Seale NS, Casamassimo PS. Access to dental care for children in the United States: a survey of general practitioners. J Am Dent Assoc. 2003;134(12):1630–1640. doi: 10.14219/jada.archive.2003.0110. [DOI] [PubMed] [Google Scholar]
- 6.Garg S, Rubin T, Jasek J, Weinstein J, Helburn L, Kaye K. How willing are dentists to treat young children?: a survey of dentists affiliated with Medicaid managed care in New York City, 2010. J Am Dent Assoc. 2013;144(4):416–425. doi: 10.14219/jada.archive.2013.0135. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Pediatric Dentistry. Guideline on periodicity of examination, preventive dental services, anticipatory guidance/counseling, and oral treatment for infants, children, and adolescents. Chicago (IL): AAPD; 2013. [cited 2014 Oct 16]. [Internet]. Available from: http://www.aapd.org/media/Policies_Guidelines/G_Periodicity.pdf. [Google Scholar]
- 8.Hakim RB, Babish JD, Davis AC. State of dental care among Medicaid-enrolled children in the United States. Pediatrics. 2012;130(1):5–14. doi: 10.1542/peds.2011-2800. [DOI] [PubMed] [Google Scholar]
- 9.Health Resources and Services Administration. Rockville (MD): HRSA; 2014. Feb, [cited 2014 Oct 16]. Integration of oral health and primary care practice. [Internet]. Available from: http://www.hrsa.gov/publichealth/clinical/oralhealth/primarycare/integrationoforalhealth.pdf. [Google Scholar]
- 10.Institute of Medicine. Improving access to oral health care for vulnerable and underserved populations. Washington (DC): IOM; 2011. Jul, [cited 2014 Oct 16]. [Internet]. Available from: http://www.iom.edu/Reports/2011/Improving-Access-to-Oral-Health-Care-for-Vulnerable-and-Underserved-Populations.aspx. [Google Scholar]
- 11.Rozier RG, Sutton BK, Bawden JW, Haupt K, Slade GD, King RS. Prevention of early childhood caries in North Carolina medical practices: implications for research and practice. J Dent Educ. 2003;67(8):876–885. [PubMed] [Google Scholar]
- 12.Moyer VA. Prevention of dental caries in children from birth through age 5 years: US Preventive Services Task Force recommendation statement. Pediatrics. 2014;133(6):1102–1111. doi: 10.1542/peds.2014-0483. [DOI] [PubMed] [Google Scholar]
- 13.Yu SM, Bellamy HA, Kogan MD, Dunbar JL, Schwalberg RH, Schuster MA. Factors that influence receipt of recommended preventive pediatric health and dental care. Pediatrics. 2002;110(6):e73. doi: 10.1542/peds.110.6.e73. [DOI] [PubMed] [Google Scholar]
- 14.Sams LD, Rozier RG, Wilder RS, Quiñonez RB. Adoption and implementation of policies to support preventive dentistry initiatives for physicians: a national survey of Medicaid programs. Am J Public Health. 2013;103(8):e83–e90. doi: 10.2105/AJPH.2012.301138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rozier RG, Stearns SC, Pahel BT, Quiñonez RB, Park J. How a North Carolina program boosted preventive oral health services for low-income children. Health Aff (Millwood) 2010;29(12):2278–2285. doi: 10.1377/hlthaff.2009.0768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herndon JB, Tomar SL, Catalanotto FA, Vogel WB, Shenkman EA. The effect of Medicaid primary care provider reimbursement on access to early childhood caries preventive services. Health Serv Res. 2014 Jul. doi: 10.1111/1475-6773.12200. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pahel BT, Rozier RG, Stearns SC, Quiñonez RB. Effectiveness of preventive dental treatments by physicians for young Medicaid enrollees. Pediatrics. 2011;127(3):e682–e689. doi: 10.1542/peds.2010-1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stearns SC, Rozier RG, Kranz AM, Pahel BT, Quiñonez RB. Cost-effectiveness of preventive oral health care in medical offices for young Medicaid enrollees. Arch Pediatr Adolesc Med. 2012;166(10):945–951. doi: 10.1001/archpediatrics.2012.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis CW, Boulter S, Keels MA, Krol DM, Mouradian WE, O’Connor KG, et al. Oral health and pediatricians: results of a national survey. Acad Pediatr. 2009;9(6):457–461. doi: 10.1016/j.acap.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 20.Gesler WM. The cultural geography of health care. Pittsburgh (PA): University of Pittsburgh Press; 1992. pp. 92–94. [Google Scholar]
- 21.Higgs G. The role of GIS for health utilization studies: literature review. Health Serv Outcomes Res Method. 2009;9(2):84–99. [Google Scholar]
- 22.Billi JE, Pai C, Spahlinger DA. The effect of distance to primary care physician on health care utilization and disease burden. Health Care Manage Rev. 2007;32(1):22–29. doi: 10.1097/00004010-200701000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Seidel JE, Beck CA, Pocobelli G, Lemaire JB, Bugar JM, Quan H, et al. Location of residence associated with the likelihood of patient visit to the preoperative assessment clinic. BMC Health Serv Res. 2006;6(13):1–9. doi: 10.1186/1472-6963-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gregory PM, Malka ES, Kostis JB, Wilson AC, Arora JK, Rhoads GG. Impact of geographic proximity to cardiac revascularization services on service utilization. Med Care. 2000;38(1):45–57. doi: 10.1097/00005650-200001000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res. 2005;40(1):135–155. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Woods CR, Arcury TA, Powers JM, Preisser JS, Gesler WM. Determinants of health care use by children in rural western North Carolina: results from the Mountain Accessibility Project. Pediatrics. 2003;112(2):e143–e152. doi: 10.1542/peds.112.2.e143. [DOI] [PubMed] [Google Scholar]
- 27.McKernan SC, Kuthy RA, Momany ET, McQuistan MR, Hanley PF, Jones MP, et al. Geographic accessibility and utilization of orthodontic services among Medicaid children and adolescents. J Public Health Dent. 2013;73(1):56–64. doi: 10.1111/jphd.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chinn CH, Rossy S, Best E. Analysis of InsureKidsNow.gov dental providers in New York state. Pediatr Dent. 2013;35(5):451–455. [PubMed] [Google Scholar]
- 29.Arevalo O, Saman DM, Tabares M, Sotomayor L, Hernandez A. Availability and distribution of pediatric dentists in Puerto Rico. J Theory Pract Dent Public Health. 2013;1(2):5–15. [Google Scholar]
- 30.Byck GR, Walton SM, Cooksey JA. Access to dental care services for Medicaid children: variations by urban/rural categories in Illinois. J Rural Health. 2002;18(4):512–520. doi: 10.1111/j.1748-0361.2002.tb00918.x. [DOI] [PubMed] [Google Scholar]
- 31.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 32.Grembowski D, Andersen RM, Chen M. A public health model of the dental care process. Med Care Rev. 1989;46(4):439–496. doi: 10.1177/107755878904600405. [DOI] [PubMed] [Google Scholar]
- 33.US Census Bureau. American Community Survey 2006–2010 (5-year estimates) New York (NY): Social Explorer; [cited 2014 May 12]. [Internet]. Available from: http://www.socialexplorer.com/tables/ACS2010_5yr/R10817223?ReportId=R10817223. [Google Scholar]
- 34.Health Resources and Services Administration. Rockville (MD): HRSA; 2014. Jun, [cited 2014 Oct 16]. Shortage designation: health professional shortage areas and medically underserved areas/populations. [Internet]. Available from: http://www.hrsa.gov/shortage/ [Google Scholar]
- 35.National Center for Health Statistics. Hyattsville (MD): National Center for Health Statistics; 2013. [cited 2014 Oct 16]. Health, United States, 2012. [Internet]. Available from: http://www.cdc.gov/nchs/data/hus/hus12.pdf. [Google Scholar]
- 36.Lee JY, Divaris K, Baker AD, Rozier RG, Lee SY, Vann WF., Jr Oral health literacy levels among a low-income WIC population. J Public Health Dent. 2011;71(2):152–160. doi: 10.1111/j.1752-7325.2011.00244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Medicare and Medicaid Services. 2014 core set of children’s health care quality measures for Medicaid and CHIP. Baltimore (MD): CMS; 2014. [cited 2014 Oct 16]. [Internet]. Available from: http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Quality-of-Care/Downloads/ChildCoreMeasures.pdf. [Google Scholar]
- 38.Healthy People 2020. Washington (DC): HHS; 2013. [cited 2014 Oct 16]. Oral health leading health indicator. [Internet]. Available from: http://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Oral-Health. [Google Scholar]
- 39.American Academy of Pediatrics. Caries prevention services reimbursement table. Elk Grove Village (IL): American Academy of Pediatrics; 2014. [cited 2014 Oct 16]. [Internet]. Available from: http://www2.aap.org/commpeds/dochs/oralhealth/docs/OralHealthReimbursementChart.xlsx. [Google Scholar]
- 40.American Academy of Pediatric Dentistry. The state of little teeth. Chicago (IL): American Academy of Pediatric Dentistry; 2014. Jan, [cited 2014 Oct 16]. [Internet]. Available from: http://www.aapd.org/assets/1/7/State_of_Little_Teeth_Final.pdf. [Google Scholar]
- 41.Department of Health and Human Services. Washington (DC): HHS; 2013. Feb 25, [cited 2014 Oct 16]. Patient Protection and Affordable Care Act; standards related to essential health benefits, actuarial value, and accreditation; final rule. 45 C.F.R. Sects. 147, 155, and 156. [Internet]. Available from: http://www.gpo.gov/fdsys/pkg/FR-2013-02-25/pdf/2013-04084.pdf. [PubMed] [Google Scholar]
- 42.Weber-Gasparoni K, Kanellis MJ, Qian F. Iowa’s public health-based infant oral health program: a decade of experience. J Dent Educ. 2010;74(4):363–371. [PubMed] [Google Scholar]
- 43.Horner MW, Mascarenhas AK. Analyzing location-based accessibility to dental services: an Ohio case study. J Public Health Dent. 2007;67(2):113–118. doi: 10.1111/j.1752-7325.2007.00027.x. [DOI] [PubMed] [Google Scholar]
- 44.Hale KJ. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111(5 Pt 1):1113–1116. doi: 10.1542/peds.111.5.1113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.