Abstract
Objective
To test the hypothesis that childhood maltreatment history would be associated with inadequate prenatal care utilization.
Design
A post-hoc analysis of a prospective cohort study of the effects of post traumatic stress disorder (PTSD) on pregnancy outcomes.
Setting
Recruitment took place via prenatal clinics from three academic health systems in southeast Michigan.
Participants
This analysis included 467 diverse, nulliparous, English-speaking adult women expecting their first infants.
Methods
Data were gathered from structured telephone interviews at two time points in pregnancy and from prenatal medical records.
Results
Contrary to our hypothesis, history of childhood maltreatment was associated with better likelihood of using adequate prenatal care. Risk for inadequate prenatal care occurred in association with the posttraumatic stress and interpersonal sensitivity that can result from maltreatment, with low alliance with the maternity care provider, and with public insurance coverage. Prior mental health treatment was associated with using adequate prenatal care.
Conclusion
When childhood maltreatment survivors were resilient or have used mental health treatment, they were more likely to utilize adequate prenatal care. The maternity care relationship or service delivery model (e.g., no continuity of care) as well as structural factors may adversely affect utilization among PTSD-affected survivors. Since inadequate care was associated with adverse outcomes, further studies of these modifiable factors are warranted.
Keywords: posttraumatic stress disorder, women's mental health, prenatal care, childhood maltreatment
Introduction
One in eight women in the United States will be affected by posttraumatic stress disorder in her lifetime, with almost 5% meeting PTSD diagnostic criteria at any given time (Breslau, Kessler, Chilcoat, Schultz, Davis & Andreski,1997; Kessler, Berglund, Delmer, Jin, Merikangas, & Walters, 2005; Resnick, Kilpatrick, Dansky, Saunders & Best, 1993). Women who are victims of violence have a higher conditional risk of PTSD, from 27% among women sexually abused in childhood to 80% of battered women and survivors of rape (Resnick, Kilpatrick, Dansky, Saunders & Best, 1993). The Diagnostic and Statistical Manual for Mental Disorders 4th edition lists the diagnostic criteria for PTSD as trauma exposure with at least 6 symptoms from three clusters: intrusive re-experiencing such as flashbacks or nightmares, numbing and avoidance symptoms such as amnesia or avoiding reminders, and hyperarousal symptoms such as exaggerated startle reflex, irritability or hyper-vigilance (American Psychiatric Association, 2000). PTSD rarely occurs in isolation. Depression and substance use are common comorbidities. Associated features include high levels of somatic symptoms, alterations in consciousness (including dissociation and amnesia), and difficutlies in maintaining healthy relationships. People with PTSD engage in more high-risk behaviors such as substance abuse (Morland, Goebert, Onoye, Frattarelli, Derauf, Herbest, Friedman, et al, 2007; Smith, Poschman, Cavaleri, Howell, & Yonkers, 2006).
In pregnancy, rates are higher and estimated at 8% in prenatal clinic samples (reviewed in Seng et al., 2009). Childhood maltreatment and prior medical trauma have been found to convey the largest risk for meeting PTSD diagnostic criteria in pregnancy. Childhood maltreatment history increased risk for PTSD in pregnancy 12-fold (adjusted OR = 11.9, 95% CI 3.6, 40.0). Prior medical trauma, including spontaneous or elective abortion that the woman reported to be a trauma exposure, increased risk for PTSD in pregnancy six fold (adjusted OR 6.1, 95% CI 1.5, 24.4) (Seng, Low, Sperlich, Ronis & Liberzon, 2009). Effects of PTSD on pregnancy health and perinatal outcomes have been less well-studied, but recent research is showing PTSD to be a cause of increased risks, physical discomforts, and adverse outcomes in pregnancy as well. PTSD has been linked with a number of concerns during pregnancy, including high risk behaviors, such as tobacco and alcohol use (Smith, Poschman, Cavaleri, Howell, & Yonkers, 2006), complications such as miscarriage, ectopic pregnancy, hyperemesis gravidarum, preterm contractions that do not lead to preterm delivery (Seng, Oakley, Sampselle, Killion, Graham-Bermann, Liberzon, 2001), and the adverse outcomes of lower birth weight, and shorter gestation (Rosen, Seng, Mallinger, et al., 2007; Seng, Low, Sperlich, Ronis & Liberzon, 2011). PTSD in pregnancy has also been identified as a predisposing factor for worse subjective appraisals of the labor experience (Garthus-Niegel, von Soest, Vollrath, & Eberhard-Gran, 2012), postpartum depression (Slade, Morrell, Rigby, Ricci, Spittlehouse & Brugha, 2010), and impaired maternal bonding with the infant (Seng et al, 2013). Decrements in neonatal and subsequent neuro-development child outcomes also have been found in prospective studies when mothers had been affected by PTSD (Muzik et al., 2013).
In our own recent prospective three-cohort study of PTSD effects on childbearing outcomes, Stress, Trauma and the Childbearing Year (STACY) Project, we found a strongly adverse effect on birth weight and a smaller effect on length of gestation. Infants of trauma-exposed women affected by posttraumatic stress disorder (PTSD cases) had significantly lower birth weight than infants of control women who were trauma-exposed but resilient (mean decrement of 283 grams, SD = 682 grams), and lower birth weight than control women with no trauma exposure (mean decrement of 221 grams, SD =628) (Seng, Low, Sperlich, Ronis & Liberzon, 2011). Because pregnancy PTSD was so strongly predicted by childhood maltreatment history (i.e., physical abuse, sexual contact abuse, sexual penetration, emotional abuse, physical neglect), we used stratified analyses to examine outcomes of women abused in childhood. The regression models indicated that, for women with a maltreatment history, prenatal care was not protective against either lower birth weight or shorter gestation. This was a somewhat unexpected finding. Adequate prenatal care was protective (i.e., was associated with longer gestation) for the sample overall (beta = .254, p < .001) and for the sub-sample of women with other-cause PTSD (beta = .292, p < .001). But prenatal care was NOT protective for the sub-sample of women with child abuse related PTSD (beta = .073, p = .332).
Prenatal care has long been associated with better outcomes for both mother and child, and this consistent research finding has informed visit schedules of prenatal care delivery and undergirds mandates to provide public sector clinics and insurance coverage for complete prenatal care (National Institutes of Health, 1989; American Academy of Pediatrics and the American College of Obstetricians and Gynecologists, 2007). Recent studies reaffirm the importance of prenatal care for preventing adverse outcomes, showing increased adverse outcomes among women with non-attended or low-attended prenatal care profiles (Raatikainen, Heiskanen, & Heinonen, 2007), including preterm delivery, low birth weight, and perinatal mortality (Abu-Ghanem, Sheiner, Sherf, Wiznitzer, Sergienko & Shoham-Vardi, 2012). Thus the question of why prenatal care is not protective for pregnant women with childhood maltreatment-related PTSD (CM-PTSD) is an important one.
Reports in the qualitative literature suggest possible reasons for why women with CM-PTSD may not be benefitting from prenatal care. A qualitative study conducted with women who did not adhere to the prenatal care visits (not selected for maltreatment history or PTSD), revealed fear and discomfort about the bodily experience of pregnancy and the process of becoming a mother as primary factors in the lack of adherence. These authors note that attention to psychosocial issues and good communication are important (Duarte, de Andrade, Mamede, 2009). These fears could be particularly profound among women with a childhood maltreatment history (Sperlich & Seng, 2008), and they could trigger symptoms in women with CM-PTSD. As we will see below, these women's capacity to form the relationship necessary to address such fears may be impaired (Sperlich & Seng, 2008).
Qualitative studies have been conducted with child sexual abuse survivors regarding their pregnancies and prenatal care experiences. Results indicated that prenatal care may be triggering for women with child abuse history, particularly childhood sexual abuse, due to intrusive medical procedures that can be reminders of past trauma and cause PTSD reactions (Roller, 2011; Seng, Sparbel, Kane Low, & Killion, 2002). Thus aspects of pregnancy itself (e.g., inescapable bodily experience, impending maternal role), or aspects of prenatal care (e.g., vaginal examinations, blood draws), could be particularly stressful for women who adhere to visits, and in others could prompt avoidance behaviors. Avoidance of reminders of the trauma (triggers) are a hallmark of—and diagnostic criterion for—PTSD (American Psychiatric Association, 2000). Information from these qualitative interviews also indicated that the relationship with the maternity care providers could be stressful, for more than one reason. Some of the interview participants reported that on-going risk exposures made engaging in prenatal care difficult due to stigma. Specifically they related current intimate partner violence to their childhod abuse history. They also related self-medicating with tobacco and illicit drugs to PTSD symptoms that were noxious and hard to bear. But they feared professionals involved in their care would not understand these problems as trauma-related (Seng, Sparbel, Kane Low, & Killion, 2002). They also reported difficulty trusting a caregiver and feared being dependent and relatively powerless, especially in labor. Thus, aspects of the relationships with the maternity care professionals may also prompt avoidance.
There is very little specific information about the effects of past or current mental health treatment on abiity to utilize the maternity care relationship and prenatal care to good effect. But positive past experiences with on-going, intimate caregiver relationships, even in the absence of cure of PTSD or depression, may favorably influence uptake and adherence to prenatal care (Roller, 2011). Past treatment also may make it easier for women affected by CM-PTSD to articulate their needs, having potentially discussed their trauma history, triggers, and symptoms in the mental health context.
Quantitative research on childhood maltreatment survivors and prenatal care utilization patterns is less available. Nevertheless, there is some evidence from the larger samples used in quantitative studies to support the possible explanations advanced from the above qualitative reports. Women with CM-PTSD in particular are known to have difficulty engaging in clinical relationships for PTSD treatment, to an extent that there are treatment engagement interventions designed for them (e.g., Cloitre, 2002 STAIR-PE psychoeducation program); this difficulty may well carry over into other health care settings. A recent study found that over one-third of pregnant women who had been exposed to childhood maltreatment were unhappy with their prenatal care experience (Leeners, et al, 2012), over half of the women reported effects from the maltreatment as affecting their pregnancy and prenatal care, including fear related to appointments, and lack of confidence in their maternity care provider. This pattern is concerning because rates of dissatisfaction with prenatal care usually are much lower (e.g., 1% in Scotland, 2.1% in team care and 7.7% in standard care in Australia, and 7% in a US study) (van Teijlingen, Hundley, Rennie, Graham, & Fitzmaurice, 2003; Biro, Waldenstrom, Brown & Pannifex, 2003; Sullivan & Beeman, 1982).
Taken together, these qualtitative data especially indicate that there may be several reasons why child maltreatment survivors with PTSD do not receive risk-protective benefits from prenatal care, but more quantitative research is needed to confirm and provide evidence for changes in clinical care. Thus, returning to the central question for this paper, we want to further examine the STACY Project data to begin to understand why prenatal care was not protective for the women with CM-PTSD by testing the hypothesis that affected women are using less prenatal care.
Methods
Design and Parent Study Description
This effort was a post-hoc analysis of a prospective three cohort study of the effects of PTSD on pregnancy outcomes known as the STACY Project (NIH NR008767, PI Seng) which followed up a main finding of the study that PTSD-affected women had lower birth weight and shorter gestation, and that prenatal care was not protective against these adverse outcomes for the childhood maltreatment survivors with PTSD. Data used in this analysis were from the initial survey interview which was conducted prior to 28 weeks gestation, from the late-pregnancy survey conducted at approximately 35 weeks gestation, and from medical record review conducted after delivery of the infant. Recruitment, procedures, and instruments have been fully described elsewhere (Seng et al., 2009; Seng et al., 2011) and are briefly summarized here.
Recruitment and Procedures
The study took place at maternity care clinics within three health systems in the midwestern United States. Obstetric clinic nurses determined eligibility (age 18 or older, expecting a first infant, able to speak English without an interpreter, and gestational age less than 28 weeks) from the clinical interview. Eligible women were invited to take part in a telephone survey about “stressful things that happen to women, emotions, and pregnancy.” Interested women received a written information document and gave contact information. Institutional Review Board (IRB) approvals were obtained from the three health systems where recruitment took place. In the original data collection, 9,556 women were evaluated for inclusion in the study, of which 6,408 were not eligible. A total of 3,148 were invited to particiapte, and 459 of those declined to do so. Out of this group, 2,689 accepted the invitation to participate and provided contact information.
A survey research organization (DataStat, Ann Arbor, Michigan) used the contact information provided to conduct interviews from August 2005 through October 2008. The initial interview took place prior to 28 weeks gestational age. It began by validating eligibility and continued with a verbal informed consent process, that included explanation of the confidentiality certificate protections. Professional research interviewers used a computer-assisted telephone interview (CATI) program to conduct a standardized psychiatric diagnostic interview designed for use with lay interviewers. Interviews lasted an average of 33 minutes. Participants who completed the interview were sent a $20 check by mail. Of the 2,689 who gave contact information, 758 could not be reached. Among the 1,931 who could be reached, 278 were not actually eligible or their pregnancy had ended. Finally, 1,653 women were reached and eligible, with 1,581 affirming willingness to participate and completing the interview.
A computerized algorithm applied Diagnostic and Statistical Manual of Mental Disorders, 4th Edition-TR (DSM-IV; American Psychiatric Association, 2000) PTSD symptom diagnostic criteria and assigned women to one of three cohorts for follow-up: PTSD-diagnosed (lifetime, n=319), trauma-exposed, but resilient controls (n=380), and nonexposed controls (n=350).Women who did not fit these cohort definitions (n=532), most of whom had partial PTSD, were dismissed from follow-up. The second interview took place in late pregnancy, near 35 weeks gestation. Most of the life event stress data were collected in this interview, as well as information about the relationship with the maternity care provider. Chart data was abstracted from the medical record after delivery using an abstraction instrument developed for this study that attained an interrater agreement greather than 90% initially and throughout a 5% audit that continued across the life of the study.
Sample for Analysis
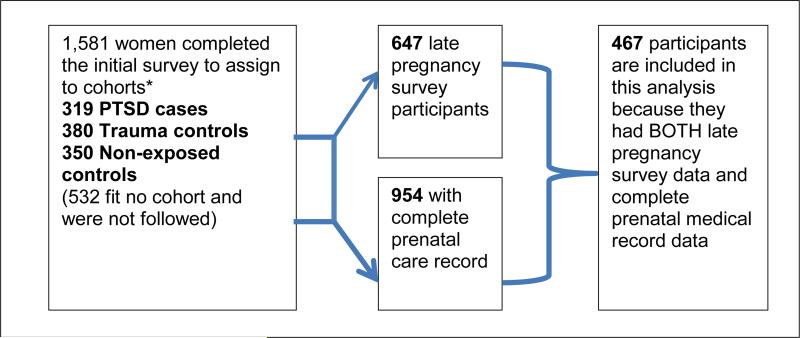
The final sample size included in this analysis was 467 women. This includes the subset of women who had complete data on prenatal care and who participated in the second wave of data collection in late pregnancy where alliance was assessed. See figure 1 for depiction of the procedure for obtaining the sample size for this analysis. The sample was large, racially, economically and geographically diverse, addressing a limitation to generalizability in previous prevalence studies that focused on primarily low income samples (Seng et al., 2009).
Figure 1.
Depiction of sample enrollment and follow-up
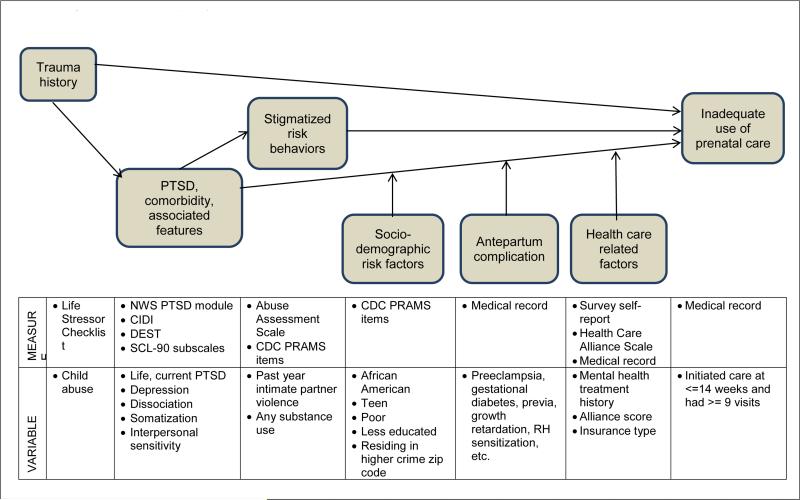
Organizing Framework
The organzing framework that guides modeling in the parent study suggested that trauma exposure affects outcomes of childbearing—in this instance the outcome of interest is adequacy of prenatal care utilization—via PTSD. This association might be mediated via biological pathways and behavioral risk exposures. The relationship between these main predictors (i.e., trauma exposure, PTSD) and outcomes might also be moderated by three sets of factors. These include (1) non-modifiable factors, such as obstetric complications, (2) potentially modifiable factors such as socioeconomic stress, and (3) modifiable health-care related factors such as insurance coverage, mental health care, and maternity care. Figure 2 depicts these relationships and lists the measures used to operationalize each component in this analysis.
Figure 2.
Organizing framework, measures, and variables.
Measures
The outcome of interest in this analysis was presence or absence of “adequate” prenatal care. The question of what constitutes an adequate amount of prenatal care has been a subject of debate. One standard in the United States is having one visit prior to 12 weeks, one visit per month until 28 weeks, bimonthly until 36 weeks, and then weekly until delivery (American Academy of Pediatrics and the American College of Obstetricians and Gynecologists, 2007). We defined the standard for this study using these guidelines, requiring for women expecting their first infant at least 9 visits, beginning at 14 weeks or earlier. We used the total number of prenatal visits on the prenatal flow sheet and the gestational age at the time of the first prenatal visit to create the variable showing presence or absence of adequate prenatal care.
The main predictor variables were created from well-establised instruments designed for epidemiology research. Childhood maltreatment history was assessed using the Life Stressor Checklist (LSC; Wolfe & Kimerling,1997), which was designed for use with women. This instrument was modified for use in a telephone format to assess 29 potentially traumatic events. This measure is considered the most sensitive measure of potentially traumatic events for use with women because it includes many potentially traumatic events that are gendered, such as caring for dying relatives and experiencing miscarriage or elective termination (Cusack, Falsetti, & de Arellano, 2002). From this measure we counted a woman as a childhood maltreatment survivor if she had disclosed physical, sexual, or emotional abuse or physical neglect prior to age 16. The Abuse Assessment Screen (McFarlane, Parker, Soeken & Bullock, 1992) was used to determine past year experience of intimate partner violence, another potentially relevant factor influencing prenatal care utilization. Both of these trauma history measures meet the important reliability standards of querying using behaviorally specific questions. Lifetime and current (pregnancy) PTSD symptoms and diagnosis were obtained using the National Women's Study PTSD module (Resnick et al., 1993). This was used in the largest epidemiological study of PTSD in women, with high sensitivity (sensitivity 0.99, specificity of 0.79) to PTSD when compared with the established Structured Clinical Interview for DSM Disorders (SCID; Kilpatrick et al., 1994). PTSD is often comorbid with depression and those whose PTSD is subsequent to childhood maltreatment trauma are also likely to experience the associated features of interpersonal sensitivity, dissociation, and somatization. Thus, we also determined past year major depressive disorder diagnosis using the Composite International Diagnostic Interview which has been validated in numerous multi-nation epidemiology studies (Wittchen, 1994).
Interpersonal sensitivity and somatization symptoms were measured with 10-item and 13-item subscales of the Symptom Checklist 90 (SCL-90), which had internal consistency alpha coefficients in this study of .84 and .74 respectively (Derogatis & Savitz, 2000). Dissociation symptoms were measured with the 8-item taxonomic version of the Dissociative Experiences Scale (DES-T), which assesses symptoms of pathological dissociation associated with dissociative disorder diagnoses (Waller, Putnam, & Carlson, 1996). The alpha coefficient for this scale in this sample was .68.
The potential mediator and moderator (or confounding) variables were formed from several sources. A dichotomous antepartum complication variable was derived from the chart abstraction if any of the following complications were noted: gestational diabetes, intrauterine fetal demise, previa, abruption, severe pregnancy induced hypertension/preeclampsia, pyelonephritis, and/or Rh sensitization. Sociodemographic status was used as a proxy for chronic stress. Demographic information was obtained using the standardized self-report items from the Centers for Disease Control and Prevention Prenatal Risk Assessment and Monitoring System (PRAMS) survey (Beck et al., 2002). Across analyses from the STACY project we use an index of five sociodemographic risk factors particularly relevant to PTSD. This index is the sum of being a teen (18-20 years of age), African American, with high school education or less, living in poverty, and residing in a neighborhood with a crime rate higher than the US average. The crime rate was derived from the Federal Bureau of Investigation Uniform Crime Report in 2000 and the woman's zip code (simplymaps.com, retrieved May 20, 2009). We consider a woman to be in a high stress sociodemographic category if her index score is 2 or higher. We created a dichotomous substance use variable from PRAMS items as well, assessing for any pregnancy use of tobacco, alcohol, or illicit drugs. We took health care related factors into account with three variables. Insurance coverage was defined dichotomously as public (i.e., Medicaid) versus private, commercial insurance, based on the medical record.
The strength of the alliance with the maternity care provider as assessed with a newly developed scale, the Health Care Alliance Questionnaire (HCAQ, Roosevelt, Holland, Hiser, & Seng, under review). This is a 16-item measure derived from alliance scales used in psychotherapy research and enhanced with items specific to health care relationships (e.g., comfort with being physically examimed, collaboration in medical decision-making). The reliability of this scale in this sample is .93. Finally, we created a dichotomous variable to indicate any past or current use of mental health treatment in the form of individual psychotherapy or psychiatric medication.
Statistical Analyses
We described the sample overall and compare them on all elements of the organizing framework based on whether they did or did not utilize adequate prenatal care. We tested the hypothesis that childhood maltreatment is associated with inadequate prenatal care utilization via chi square and augment this analysis with a four-cell test comparing women with neither childhood maltreatment history nor PTSD, with childhood maltreatment history but not PTSD, with PTSD from other, nonmaltreatment trauma exposures, and with both maltreatment history and PTSD. Based on what characteristics differed significantly between those who did and did not use adequate prenatal care, we conducted multiple logistic regression to model all of these factors together. A post hoc power calculation conducted using PASS software (Hintze, 2005) verified that the sample size was sufficient for the modeling performed.
Results
The sample was demographically diverse (Table 1, column showing total sample rates), with a mean age of 26.6 years (SD = 5.4) and an average of 1.3 (SD = 1.7) sociodemographic risk factors, including 251 women who had no risk factors. African Americans made up 32.5% of the sample (n=152) and European Americans were 55.7% (n=260), with 5.6% Latinas (n=26), 3% Middle Eastern women (n=14), 8.4% Asian Americans (n=39), 0.9% Native American or Alaska Native women (n=4), 0.4% Native Hawaiian or Pacific Islanders (n=2), and 3.9% (n=18) who declined to describe their racial or ethnic identity. In this sample 18.4% (n=86) disclosed a history of childhood maltreatment. 24.4% (114) were classified into the lifetime PTSD group. The rate of PTSD among those with childhood maltreatment history (CM-PTSD) was 55.8% (n=48). The rate of PTSD among those with no maltreatment history was 17.3%, (n=66). There were 331 (70.9%) women who had received adequate prenatal care and 136 (29.1%) who had not.
Table 1.
Descriptions of the sample overall and by cohort, depicting all factors included in the multivariate models
| Total (n=467) | Adequate Prenatal Care n=331 (70.9) | NOT Adequate Prenatal Care n=136 (29.1) | Statistic | P | |
|---|---|---|---|---|---|
| Sociodemographic risk factors | |||||
| African American | 152 (32.5) | 72(20.1) | 80(63.5) | χ2 =75.3 | <.001 |
| Poverty (income <$15,000) | 78 (16.7) | 36(10.6) | 42(33.3) | χ2 =34.3 | <.001 |
| Teen | 88 (18.8) | 37(10.9) | 51(40.5) | χ2 =52.8 | <.001 |
| Low Education | 168 (36.0) | 84(24.6) | 84(66.7) | χ2 =70.6 | <.001 |
| High Crime | 142 (30.4) | 65(19.1) | 77(61.1) | χ2 =77.9 | <.001 |
| Socioeconomic Risk Index, mean (SD) | 1.3 (1.7) | 0.9 (1.4) | 2.6 (1.8) | t(184.5)=10.1 | <.001 |
| High or Low Risk Score | 167(35.8) | 79(23.2) | 88(69.8) | χ2 =87.3 | <.001 |
| Trauma and Complex PTSD | |||||
| Childhood maltreatment trauma | 86(18.4) | 69(20.2) | 17(13.5) | χ2 =2.7 | .095 |
| Lifetime PTSD | 114(24.4) | 83(24.3) | 31(24.6) | χ2 =0.0 | .953 |
| Current PTSD | 36(7.7) | 21(6.2) | 15(11.9) | χ2 =4.3 | .039 |
| Depression | 48(10.3) | 34(10.0) | 14(11.1) | χ2 =0.1 | .719 |
| Any Substance Use in Pregnancy | 112(24.0) | 71(20.8) | 41(32.5) | χ2 =6.9 | .008 |
| Dissociation score, mean (SD) | 1.0(2.3) | 1.0(2.4) | 1.0(2.2) | t(241)=-0.0 | .978 |
| Interpersonal sensitivity score, mean (SD) | 4.1(5.5) | 3.6(4.4) | 5.6(7.5) | t(159)=2.8 | .005 |
| Somatization score, mean (SD) | 5.2(5.1) | 5.3(5.1) | 4.9(5.1) | t(465)=0.2 | .503 |
| Healthcare Related Factors | |||||
| Pre-existing chronic condition | 211(45.2) | 174(51.0) | 37(29.4) | χ2 =17.4 | <.001 |
| Antepartum complication | 96(20.6) | 25(19.8) | 71(20.8) | χ2 =0.1 | .816 |
| Alliance with Provider, mean (SD) | 67.3(9.2) | 68.2(8.9) | 64.9 (9.4) | t(214.1)=−3.5 | .001 |
| Insurance coverage type | χ2 =51.0 | <.001 | |||
| Private | 305(74.6) | 244(83.8) | 61(51.7) | ||
| Medicaid | 99(24.2) | 47(16.2) | 52(44.1) | ||
| None | 3(0.7) | 0 | 3(2.5) | ||
| Self-pay | 2(0.5) | 0 | 2(1.7) |
Note: Values are n(%) unless stated otherwise. PTSD = post traumatic stress disorder; SD = standard deviation
Risk Factors for Inadequate prenatal care
We assessed, one by one, the full range of factors theorized (figure 2) to affect use of prenatal care that were available in the STACY data set: trauma history, mental health status, sociodemographic stress level, antepartum complications, and health care related factors (Table 1). We hypothesized that women with childhood maltreatment history would be less likely to use adequate prenatal care. Chi squared results do not support this hypothesis. The majority of women in the sample (70.9%) received more than 9 prenatal visits beginning by 14 weeks, thus meeting our criteria for adequate prenatal care. Women with adequate prenatal care included 20.2% who had any childhood maltreatment history. Women who did not have adequate prenatal care included 13.5% with a history of childhood maltreatment, a difference that did not reach statistical significance ( χ2 =2.8 OR =1.6, p =.095).
Across the two cohorts of adequate prenatal care versus not adequate prenatal care versus not adequate prenatal care, the rate of having lifetime PTSD did not differ. However women with current PTSD were less likely to have adequate prenatal care (6% vs 12%, χ2 = 4.3, OR =.49, p=.039). There was virtually no difference between the two cohorts among women with depression comorbidity. Those with higher scores on the PTSD associated feature of interpersonal sensitivity also did not differ significantly. Women using any substances during pregnancy were less likely to use adequate prenatal care (20.8% vs 32.5%, χ2 =6.9, OR =.54, p=.008). Women with recent (past year) exposure to intimate partner violence did not differ in the likelihood of using adequate prenatal care.
Across all demographic categories, more disadvantaged women used less prenatal care. This is the case for individual risk factors as well as for the classification of the women as having low-risk or high-risk sociodemographic status (t(184.5) = 10.1, p<.001). Women had antepartum complications at a 20.8% rate overall, but this factor did not affect the odds of using adequate prenatal care. Those with higher alliance scores are more likely to receive adequate prenatal care (t (465) =−3.6, p<.001. Use of mental health treatment increased the odds of using adequate prenatal care (χ2 =3.4, OR=2.1, p=.065), as did coverage with private insurance t(139)=5.7, OR=, p<.001.
Regression Analysis
Although maltreatment history was not independently associated with using inadequate prenatal care, it may be a contributing factor in interaction with other factors, especially the posttraumatic sequelae and relational variables. The full model containing all predictors was statistically significant, (χ2 (3, 467)=32.9, p<.001, which indicates that the model distinguished between women using adequate versus inadequate prenatal care (see table 2). The model as a whole explained 16% of the variance likelihood of using adequate prenatal care, and correctly classified 75.6% of cases. The steps of the model examined in their theorized order are helpful to understanding the relationships among these variables.
Table 2.
Stepwise logistic regression model predicting adequate prenatal care
| Model | Odds ratio | p | 95% CI | |
|---|---|---|---|---|
| Step 1: | R2=.009, p=.087 | |||
| Starts with maltreatment history | Childhood maltreatment trauma | 1.627 | .097 | .915, 2.891 |
| Step 2: | R2=.031, R2Δ=.022, p=.006 | |||
| Adds pregnancy PTSD | Childhood maltreatment trauma | 2.136 | .019 | 1.134, 4.022 |
| Pregnancy PTSD diagnosis | .347 | .007 | .162, .745 | |
| Step 3: | R2=.052, R2Δ=.062, p=.001 | |||
| Adds interpersonal factors | Childhood maltreatment trauma | 2.277 | .011 | 1.205, 4.304 |
| Pregnancy PTSD diagnosis | .508 | .104 | .224, 1.151 | |
| Highest quartile interpersonal sensitivity score | .510 | .008 | .310, .841 | |
| Step 4: | R2=.064, R2Δ=.012, p<.001 | |||
| Adds risk behavior | Childhood maltreatment trauma | 2.368 | .009 | 1.245, 4.504 |
| Pregnancy PTSD diagnosis | .537 | .139 | .235, 1.225 | |
| Highest quartile interpersonal sensitivity score | .554 | .023 | .333, .922 | |
| Any Pregnancy substance use | .604 | .038 | .375, .973 | |
| Step 5: | R2=.159, R2Δ=.095, p<.001 | |||
| Adds health care related factors | Childhood maltreatment trauma | 2.888 | .004 | 1.414, 5.899 |
| Pregnancy PTSD diagnosis | .501 | .112 | .213, 1.175 | |
| Highest quartile interpersonal sensitivity score | .458 | .005 | .265, .790 | |
| Any pregnancy substance use | .594 | .039 | .362, .975 | |
| Lowest quartile Health Care Alliance Score | .553 | .021 | .335, 914 | |
| Any treatment | 2.531 | .001 | 1.491, 4.295 | |
| Insurance | .464 | .001 | .295, .729 |
Note: PTSD=posttraumatic stress disorder; CI=confidence interval
In the first step, when child abuse history was entered by itself, it was not significantly associated with use of prenatal care, but the coefficient is in the direction of increasing the likelihood of using adequate care. In the second step, when PTSD during pregnancy was added, the model became statistically significant. Childhood maltreatment history became independently significant and doubled the likelihood of using adequate care once those women who were affected by PTSD were taken into account. We thus see a separation in the model of those abuse survivors who are resilient being more likely to use adequate care and those who developed PTSD being less likely to do so. In the third step, we see that it was not PTSD diagnosis per se, but rather the interpersonal sensitivity associated feature that seems to account for decreased likelihood of using adequate care because when the characteristic of having an interpersonal sensitivity score in the highest quartile is considered, the role of PTSD itself was no longer significant.
The PTSD-associated risk behavior of any substance use in pregnancy explained additional variance in the outcome. The final step, health care related factors, more than doubled the variance explained. Women with Health Care Alliance Questionnaire scores in the lowest quartile and with public insurance had reduced likelihood of adequate care. Those who have ever used mental health treatment had increased likelihood of adequate care. Thus, we concluded that child abuse history itself is not a predictor of using adequate prenatal care. Rather it was PTSD-affected women, especially those with interpersonal sensitivity and substance use, those who have low alliance with the maternity care provider, those who have never had mental health treatment, and those who are economically disadvantaged as evidenced by having insurance through the public sector who were less likely to use adequate prenatal care.
Discussion
Contrary to our hypothesis, childhood maltreatment history in and of itself was not associated with inadequate use of prenatal care. Rather, it was non-resilient, PTSD-affected, maltreatment survivors, especially those with impairment in interpersonal relationships generally and within the maternity care relationship in particular, especially within the public sector health care system who have not previously engaged in mental health care for their abuse sequelae. This analysis suggests there may be modifiable factors that can be addressed for women with CMPTSD. This finding is consistent with PTSD research which often finds that it is not the trauma exposure itself, but rather the psychological sequelae which are associated with adverse outcomes. These results suggest we can expect some maltreatment survivors to be resilient and others to need additional support. Screening for PTSD would help distinguish who is likely to need “posttraumatic stress” to be added to the problem list and attended to in the care plan.
While psychosocial education and counseling is a standard of care recommended by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists(2007), integration of trauma-specific care practices for PTSD survivors is not the norm. Health promotion activities incorporated into the prenatal care experience have been related to healthy behaviors in pregnancy (Vonderheld, Norr & Hander, 2007), as have enhanced models of prenatal care that incorporated lifestyle and psychosocial risk factor care to women in high-risk groups, which have shown to be effective in decreasing associated risk factors, including low birth weight risk (Ricketts, Murray & Schwalberg, 2005). A meaningful relationship with the maternity care provider, in which the childbearing woman is encouraged to ask questions, and feels comfortable in the environment enhances the quality of the care experience, as well as influences the woman's adherence to following care guidelines (Sword, Heaman, Brooks, Tough, Janssen, Young, et al, 2012). Thus, the quality of the experience seems relevant for addressing risk factors that can lead to adverse maternal outcomes.
This study extends our knowledge about women with childhood maltreatment PTSD in maternity care. The key finding that some abuse survivors are resilient and use an adequate amount of prenatal care was not our initial hypothesis. Furthermore, we assumed that women with PTSD would avoid healthcare providers due to wanting to avoid potential triggers that may lead to intrusive re-experiencing or other symptoms. However, the independent significance of PTSD itself—the condition for which intrusive re-experiencing is the hallmark—was lost when interpersonal factors were considered. It appears that the relationship with the provider is a stronger issue. Since triggers for PTSD as well as stigma from substance use could be barriers to adhering to scheduled prenatal care visits, this finding makes sense. Triggers could be mitigated within a high-alliance relationship, but potentially exacerbated in a situation where alliance could not be solidified. This exacerbation could be due to interpersonal factors in the client-provider dyad, or due to lack of continuity of care, which is common in many settings, especially in the public sector.
There are limitations and strengths to consider when interpreting the results. As this study was a secondary data analysis, information about the experience of prenatal care was limited. We only looked at the quantity of care, not the quality of care or any other factors related to prenatal care. Further, we set a high threshold for what constitutes adequate prenatal care based on national policy recommendations at the time of the study. However, recent studies have shown that less prenatal care may be still be efficacious within low risk groups (Partridge & Holman, 2005). We did not consider another less-than-optimal scenario, which is over-use of prenatal care in the form of excess triage visits or telephone contacts. The Health Care Alliance Questionnaire is a new measure, but its psychometric properties indicate it performs well (Roosevelt, Holland, and Seng, under review). Data available for this analysis did not allow us to consider directly the issue of stress that women using less prenatal care may experience. These stressors may occur when women do attend a visit or from foregoing desired care that they avoid to reduce PTSD or interpersonal reactivity or to reduce reliance of substances for self-soothing after a stressful medical encounter. This points to the need for a closer examination of the subjective experience of prenatal care within the group of maltreatment survivors who are not adhering to the visit schedule.
It is a strength of this study that the sample size is relatively large and that the women were characterized on the trauma history, PTSD, depression comorbidity, interpersonal sensitivity associated feature, mental health treatment history, and pregnancy substance use prospectively and that the number of prenatal visits is derived from the count of visits on the prenatal medical record using an abstraction tool with excellent interrater reliability demonstrated through auditing across the life of the study (Seng, Mugisha & Miller, 2008). It also is a strength to have included a measure of alliance to begin to capture the relational aspects of maternity care, even if the reporting is one-sided and we know nothing about the provider's capacity for alliance nor about the number of providers the woman had to work with. The sample is derived from three health systems comprising varying proportions of women with private-versus-public payor insurance, with urban, suburban, and small city contexts, and with racial and ethnic diversity and is thus generalizable to a broad population of women expecting their first infant in the US.
To summarize the implications for research, both qualitative and quantitative studies that further explore the maternity care needs of women with childhood maltreatment associated PTDS are needed to build upon our findings. An important next step would be to test the hypothesis that continuity of care with a supportive maternity care provider and/or with a perinatal nurse may result in a more satisfying experience, decreased stress, improved adherence to prenatal care and self-care behaviors, and improved outcomes.
There also are implications for practice. Our findings suggest that childhood maltreatment survivors who are resilient are fully engaged in maternity care and may be well able to navigate existing services, although we do not know the extent to which they have trauma-related needs or the extent to which they manage to get these needs addressed. The maltreatment survivors who are not resilient, however, are not as well-engaged in care. Therefore history-taking or use of screening measures would help identify survivors of maltreatment who may be non-adherent because they experience reactivity or interpersonal sensitivity in their relationships with health care providers. Following up positive screens with questions to elicit concerns and suggestions may be useful (e.g., “How stressful is it for you to talk to health care providers about your needs? What helps with that?”). In the long-term, it may be most satisfying, efficient, and effective in terms of outcomes to provide continuity of care with at least one person on the maternity care team. A nurse with an interest in psychosocial care may be well-positioned to provide this care. This enhanced management plan would seem to be commensurate with identification of PTSD via screening or disclosure. Quality improvement evaluation and nursing intervention research with this population would likely point to many options for tailoring care.
Conclusion
Women with CM-PTSD who were resilient or have previously utilized mental health services were more likely to utilize adequate prenatal care. The type of maternity care relationship or service delivery model as well as structural factors may adversely affect utilization among PTSD-affected survivors. The psychosocial support that should be included in an ideal maternity care system ideally would be suited to facilitating a stress-reducing relationship that can address CM-PTSD, improve health behaviors, and result in good outcomes. Since inadequate care is associated with adverse outcomes, further studies of modifiable factors including insurance coverage, outreach and engagement in both maternity care and potentially mental health care are warranted. A priority would be to create and test trauma-informed maternity care content or practice models that facilitate a stronger relationship between the woman and her caregivers.
Call outs.
Women with childhood maltreatment history who are resilient or who have previously utilized mental health services are more likely to utilize adequate prenatal care.
Non-resilient maltreatment survivors, especially those with impairment in interpersonal relationships and low alliance with the maternity care provider are those least likely to use adequate prenatal care.
Continuity with the provider or maternity nurse might increase alliance, trust, and improve adherence to care guidelines. Research on survivors’ preferred care models is warranted.
Contributor Information
Sue Anne Bell, University of Michigan School of Nursing. Her research focuses on the intersection of reproductive health and mental health..
Julia Seng, University of Michigan School of Nursing where she studies the effects of posttraumatic stress disorder on women's health and childbearing outcomes. 204 South State Street G120 Lane Hall Ann Arbor, MI 48109 jseng@umich.edu 734-647-4291.
References
- Abu-Ghanem S, Sheiner E, Sherf M, Wiznitzer A, Sergienko R, Shoham-Vardi I. Lack of prenatal care in a traditional community: Trends and perinatal outcomes. Archives of Gynecology and Obstetrics. 2012;285(5):1237–42. doi: 10.1007/s00404-011-2153-x. [DOI] [PubMed] [Google Scholar]
- Adewuya A, Ologun YA, Ibigbami OS. Post-traumatic stress disorder after childbirth in Nigerian women: Prevalence and risk factors. British Journal of Obstetrics and Gynecology. 2006;113(3):284–8. doi: 10.1111/j.1471-0528.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians & Gynecologists . ACOG Education Bulletin. The College; Washington, DC: 2000. Adult manifestation of childhood sexual abuse. p. 259. [Google Scholar]
- American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (AAP/ACOG) Guidelines for Perinatal Care. (Sixth Edition.) 2007 [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. 4th ed. American Psychiatric Association; Washington, DC.: 2000. [Google Scholar]
- Biro MA, Waldenstrom U, Brown S, Pannifex J. Satisfaction with team midwifery care for low- and high-risk women: A randomized controlled trial. Birth. 2003;30:1–10. doi: 10.1046/j.1523-536x.2003.00211.x. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz L. Psychiatric sequelae of posttraumatic stress disorder in women. Archives of Genral Psychiatry. 1997;54:81–7. doi: 10.1001/archpsyc.1997.01830130087016. [DOI] [PubMed] [Google Scholar]
- Carroli G, Villar J, Piaggio G, Khan-Neelofur D, Gulmezoglu M, Mugford M, Lumbiganon P, Farnot U, Bersgjø P. WHO Antenatal Care Trial Research Group: WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 2001;357(9268):1565–70. doi: 10.1016/S0140-6736(00)04723-1. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough K, Nooner K, Zorbas P, Cherry S, Jackson C, Gan W, Petkova E. Treatment for PTSD Related to Childhood Abuse: A Randomized Controlled Trial. American Journal of Psychology. 2002;AiA:1–10. doi: 10.1176/appi.ajp.2010.09081247. [DOI] [PubMed] [Google Scholar]
- Cusack K, Falsetti SA, de Arellano MA. Gender Considerations in the Psychometric Assessment of PTSD. In: Kimmerling R, Ouimette P, Wolf J, editors. Gender and PTSD. Guilford Press; New York: 2002. [Google Scholar]
- Derogatis L, Savitz K. The SCL-90-R and the Brief Symptom Inventory (BSI) in Primary Care. In: Maruish ME, editor. Handbook of psychological assessment in primary care settings. Vol. 236. Lawrence Erlbaum Associates; Mahwah, NJ: 2000. [Google Scholar]
- Duarte S, de Andrade S, Mamede M. Maternal decision on obtaining prenatal care: a study in Brazil. Midwifery. 2009;27(2):160–164. doi: 10.1016/j.midw.2009.04.008. [DOI] [PubMed] [Google Scholar]
- Falsetti S, Resnick H, Resick P, Kilpatrick D. The modified PTSD symptom scale: a brief self-report measure of posttraumatic stress disorder. Behavior Therapy. 1993;16:161–2. [Google Scholar]
- Garthus-Niegel S, vonSoest T, Vollrath M, Eberhard-Gran M. The impact of subjective birth experiences on post-traumatic stress symptoms: a longitudinal study. Archives of Women's Mental Health. 2013;16(1):1–10. doi: 10.1007/s00737-012-0301-3. doi: 10.1007/s00737-012-0301-3. [DOI] [PubMed] [Google Scholar]
- Hintze JL. PASS 2005 User's Guide. Number Cruncher Statistical Software; Kaysville, Utah: 2005. [Google Scholar]
- Kessler R, Berglund P, Delmer O, Jin R, Merikangas K, Walters E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. American Journal of Public Health. 1994;84(9):1414–1420. doi: 10.2105/ajph.84.9.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeners B, Stiller R, Block E, Görres G, Rath W. Pregnancy complications in women with childhood sexual abuse experiences. Journal of Psychosomatic Research. 2010;69(5):03–10. doi: 10.1016/j.jpsychores.2010.04.017. [DOI] [PubMed] [Google Scholar]
- Leeners B, Stiller R, Block E, Görres G, Rath W, Tschudin S. Prenatal care in adult women exposed to childhood sexual abuse. Journal of Perinatal Medicine. 2012;25:1–10. doi: 10.1515/jpm-2011-0086. doi: 10.1515/jpm-2011-0086. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy: Severity and frequency of injuries and associated entry into prenatal care. JAMA. 1992;267:3176–8. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- Modarres M, Afrasiabi S, Rahnama P, Montazeri A. Prevalence and risk factors of childbirth-related post- traumatic stress symptoms. BMC Pregnancy Childbirth. 2012;12(88) doi: 10.1186/1471-2393-12-88. doi: 10.1186/1471-2393-12-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland L, Goebert D, Onoye J, Frattarelli L, Derauf C, Herbest M, Matsu M, Friedman M. Posttraumatic stress disorder and pregnancy: Preliminary update and implications. Psychosomatics. 2007;48(4):304–308. doi: 10.1176/appi.psy.48.4.304. [DOI] [PubMed] [Google Scholar]
- Muzik M, Bocknek E, Broderick A, Richardson P, Rosenblu K, Thelen K, Seng J. Mother–infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Archives of Womens Mental Health. 2012;16(1):29–38. doi: 10.1007/s00737-012-0312-0. doi: 10.1007/s00737-012-0312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health . A Report of the Public Health Service Expert Panel on the Content of Prenatal Care. National Institutes of Health; Bethesda, MD.: 1989. Caring for Our Future: The Content of Prenatal Care. [Google Scholar]
- Raatikainen K, Heiskanen N, Heinonen S. Under-attending free antenatal care is associated with adverse pregnancy outcomes. BMC Public Health. 2007;7:268. doi: 10.1186/1471-2458-7-268. doi:10.1186/1471-2458-7-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partridge C, Holman J. Effects of a reduced-visit prenatal care clinical practice guideline. Journal of the American Board of Family Practice. 2005;18(6):555–60. doi: 10.3122/jabfm.18.6.555. [DOI] [PubMed] [Google Scholar]
- Resnick H, Kilpatrick D, Dansky B, Saunders B, Best C. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consultative Clinical Psychology. 1993;61:984–91. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Ricketts S, Murray E, Schwalberg R. Reducing low birth weight by resolving risks: results from Colorado's prenatal plus program. American Journal of Public Health. 2005;95(11):1952–1957. doi: 10.2105/AJPH.2004.047068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogal S, Poschman K, Belanger K, Howell H, Smith M, Medina J, Yonker K. Effects of posttraumatic stress disorder on pregnancy outcomes. Journal of Affective Disorders. 2007;102(1-3):137–43. doi: 10.1016/j.jad.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roller C. Moving beyond the pain: women's responses to the perinatal period after childhood sexual abuse. Journal of Midwifery and Womens Health. 2011;56(5):488–93. doi: 10.1111/j.1542-2011.2011.00051.x. doi: 10.1111/j.1542-2011.2011.00051.x. [DOI] [PubMed] [Google Scholar]
- Rosen D, Seng J, Tollman R, Mallinger G. Intimate partner violence, depression, and posttraumatic stress disorder as additional predictors of low birth weight infants among low-income mothers. Journal of Interpersonal Violence. 2007;22(10):1305. doi: 10.1177/0886260507304551. [DOI] [PubMed] [Google Scholar]
- Seng J, Oakley D, Sampselle C, Killion C, Graham-Bermann S, Liberzon I. Association of posttraumatic stress disorder with pregnancy complications. Obstetrics and Gynecololgy. 2001;97:17–22. doi: 10.1016/s0029-7844(00)01097-8. [DOI] [PubMed] [Google Scholar]
- Seng J, Sparbel K, Low L, Killion C. Abuse-related posttraumatic stress and desired maternity care practices: women's perspectives. Journal of Midwifery and Women's Health. 2002;47:360–370. doi: 10.1016/s1526-9523(02)00284-2. [DOI] [PubMed] [Google Scholar]
- Seng J, Kane Low L, Sparbel K, Killion C. Abuse-related post-traumatic stress during the childbearing year. Journal of Advanced Nursing. 2004;46(6):604–613. doi: 10.1111/j.1365-2648.2004.03051.x. [DOI] [PubMed] [Google Scholar]
- Seng J, Mugisha E, Miller J. Reliability of a perinatal outcomes measure: the Optimality Index-US. Journal of Midwifery and Women's Health. 2008;53(2):110–114. doi: 10.1016/j.jmwh.2007.09.006. doi: 10.1016/j.jmwh.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Seng J, Low L, Sperlich M, Ronis D, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstetrics and Gynecology. 2009;114(4):839–47. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng J, Kohn-Wood L, McPherson M, Sperlich M. Disparity in posttraumatic stress disorder diagnosis among African American pregnant women. Archives of Women's Mental Health. 2011;14(4):295–306. doi: 10.1007/s00737-011-0218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng J, Low LK, Sperlich M, Ronis D, Liberzon I. Post-traumatic stress disorder, child abuse history, birthweight and gestational age: a prospective cohort study. British Journal of Obstetrics and Gynecology. 2011;118(11):1329–39. doi: 10.1111/j.1471-0528.2011.03071.x. doi: 10.1111/j.1471-0528.2011.03071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng J, Sperlich M, Kane Low L, Ronis D. Childhood abuse history, posttraumatic stress disorder, postpartum mental health and bonding: A prospective cohort study. Journal of Midwifery and Women's Health. 2013;58(1):57–68. doi: 10.1111/j.1542-2011.2012.00237.x. doi: 10.1111/j.1542-2011.2012.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade P, Morrell C, Rigby A, Ricci K, Spittlehouse J, Brugha T. Postnatal women's experiences of management of depressive symptoms: a qualitative study. British Journal of General Practitioners. 2010;60(580):e440–448. doi: 10.3399/bjgp10X532611. doi: 10.3399/bjgp10X532611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MV, Poschman K, Cavaleri MA, Howell HB, Yonkers KA. Symptoms of posttraumatic stress disorder in a community sample of low-income pregnant women. American Journal of Psychiatry. 2006;163:881–884. doi: 10.1176/ajp.2006.163.5.881. [DOI] [PubMed] [Google Scholar]
- Sperlich M, Seng J. Survivor Moms: Women's Stories of Birthing, Mothering, and Healing after Sexual Abuse. Motherbaby Press; Eugene, OR: 2008. [Google Scholar]
- Sullivan DA, Beeman R. Satisfaction with maternity care: A matter of communication and choice. Medical Care. 1982;20:321–330. doi: 10.1097/00005650-198203000-00009. [DOI] [PubMed] [Google Scholar]
- Sword W, Heaman M, Brooks S, Tough S, Janssen P, Young D, Kingston D, Helewa M, Akhtar-Dinesh N, Hutton E. Women's and care providers' perspectives of quality prenatal care: a qualitative descriptive study. BMC Pregnancy Childbirth. 2012;12(29) doi: 10.1186/1471-2393-12-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Teijlingen E, Hundley V, Rennie AM, Graham W, Fitzmaurice A. Maternity satisfaction studies and their limitations: “What is, must still be best”. Birth. 2003;30:175–182. doi: 10.1046/j.1523-536x.2003.00224.x. [DOI] [PubMed] [Google Scholar]
- Vonderheid S, Norr K, Handler A. Prenatal health promotion content and health behaviors. Western Journal of Nursing Research. 2007;29(3):258–276. doi: 10.1177/0193945906296568. [DOI] [PubMed] [Google Scholar]
- Waller N, Putnam F, Carlson E. Types of dissociation and dissociative types: A taxometric analysis of dissociative experiences. Psychological Methods. 1996;1:300–321. [Google Scholar]
- Wittchen H. Reliability and validity of the WHO-Composite International Diagnostic Interview (CIDI): A critical review. Journal of Psychiatric Research. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Wolfe J, Kimerling R. Gender issues in the assessment of posttraumatic stress disorder. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. Guilford; New York, NY: 1997. pp. 192–238. [Google Scholar]
- World Health Organization . WHO Program to Map Best Reproductive Health Practices. World Health Organization; Geneva, Switzerland: 2002. [Google Scholar]