Abstract
Background
There is a need to improve classification of alcohol use disorders (AUDs) in general population surveys. We developed and tested follow-up questions for 2 commonly-reported symptom domains (withdrawal and larger/longer) to assess effects on DSM-5 AUD classification.
Methods
Telephone interviews recontacted a selective follow-up sample of respondents under age 46 from the 2010 National Alcohol Survey with at least 1 lifetime AUD symptom (N=244). Items included detailed questions about past-year AUD symptoms. Three items (vomiting, sweating, irritability) were recoded as acute intoxication rather than withdrawal if they most recently occurred within 8 hours of stopping drinking. The larger/longer criterion was recoded as socially motivated if respondents endorsed “got caught up in drinking with a group of friends” and not “feel compelled to drink and just can’t stop” as a reason for drinking more than intended.
Results
Of 225 current drinkers, 11% reported past-year withdrawal, with 28% of those reporting acute intoxication instead of physical withdrawal. Adjusting past-year withdrawal classification reduced AUD prevalence by 6%. A minority (12%) reported the past-year larger/longer criterion. Of those, 50% indicated social reasons for drinking more than intended, rather than compulsion to drink. Adjusting the past-year larger/longer criterion reduced AUD prevalence by 8%. Accounting for both adjustments reduced AUD prevalence by 13%. Cases that met AUD criteria after both adjustments were substantially heavier drinkers than those that were reclassified.
Conclusions
Follow-up items could be implemented in epidemiologic studies with minimal response burden and may help reduce mis-classification of AUD.
Keywords: alcohol use disorder, population surveys, measurement
Introduction
Alcohol use disorders (AUD) are associated with profound health, social and economic costs for drinkers and their families, friends and employers. The development and consequences of AUD have been informed by studies of individuals seeking treatment, as well as by general population studies that include non-dependent drinkers. However, compared to clinical studies where assessment of alcohol problems takes place in lengthy, one-on-one interviews, in general population survey research utilizing a relatively brief set of items, there is a risk of over-identification of AUD, particularly among young heavy drinkers (Caetano and Babor, 2006; Midanik et al., 2007). This could be due to misinterpretation of survey questions (Slade et al., 2013) or to misperception of after-effects of acute intoxication as “true” symptoms of AUD (Caetano and Babor, 2006), among other possibilities. Misspecification of AUD with instruments used in large-scale epidemiologic studies is understudied, and, importantly, it may be avoidable. Guided by standard theories and definitions of AUD, this pilot study thus had two principal aims: (1) better understand the age and heavy-drinking profile of survey-identified AUD cases, and (2) identify follow-up items that may help reduce misclassification of non-dependent, heavy drinkers in general population surveys.
Theories and definitions of alcohol use disorder
Contemporary definitions of AUD are based on research by Edwards and Gross (1976) who described an Alcohol Dependence Syndrome characterized by a psychobiology of dependence leading to loss of control over persistent, heavy drinking. This loss of control is accompanied by an increased value placed on alcohol use, physiological tolerance to alcohol and withdrawal upon cessation (Caetano and Babor, 2006).
As defined by the 5th edition of the American Psychiatric Association’s Diagnostic and Statistical Manual (DSM-5; American Psychiatric Association, 2013), alcohol use disorder is characterized by cognitive, behavioral and physiological symptoms indicating continued use despite significant problems. Symptoms in 11 different domains are considered (failure to fulfill role obligations; drinking despite social or interpersonal problems; drinking when physically hazardous; craving; tolerance; withdrawal; using more than intended or for longer than intended [larger/longer]; persistent desire to cut down or control use; giving up important activities; spending a lot of time getting alcohol, using or recovering from use; and drinking despite physical or psychological problems caused by drinking) and must be experienced in the same 12-month period. Three levels of severity are possible: mild (symptoms in 2–3 domains), moderate (4–5 domains) and severe AUD (6 or more domains; American Psychiatric Association, 2013).
Development and symptomology of AUDs in general population samples
Studies suggest the majority of cases of AUD are mild or moderate in severity (Hesselbrock and Hesselbrock, 2006), with some showing that as few as 25% of people with a lifetime diagnosis of AUD ever enter formal treatment for their problem (Hasin et al., 2007). In many general population samples, research suggests a relatively early age of first classification as dependent (in the early 20’s; Hasin et al., 2007), the highest rates of AUD among drinkers under 30 (Hasin et al., 2007), and a typical age at first treatment in the early 30’s (Hasin et al., 2007). General population studies using the National Alcohol Survey (NAS; Caetano and Tam, 1995), National Epidemiologic Survey of Alcoholism and Related Conditions (NESARC; Saha et al., 2006) and other datasets (Schuckit et al., 2008) suggest that using more than intended, withdrawal, tolerance and a desire to cut down are the most commonly reported AUD symptoms, with withdrawal and tolerance being particularly common among younger drinkers who have recently initiated use (Rose et al., 2012).
Dependence theory would not predict such high rates of physiological dependence after such a short duration drinking (Caetano and Babor, 2006). This suggests that there may be measurement error in general population surveys that affects epidemiological findings regarding precursors and prognosis of AUD (Caetano and Babor, 2006; Midanik et al., 2007). For example, there may be over-reporting of physiological symptoms of withdrawal and tolerance. Survey respondents may mistake relatively minor, short-term effects of heavy drinking (such as a severe hang-over) for withdrawal symptoms, or confuse an alcoholic’s ability to consume very high volumes of alcohol (such as a liter of spirits in a day) with an initial development of tolerance that occurs in young heavy drinkers shortly after initiating use (Caetano and Babor, 2006). A recent German study suggests that even after controlling for drinking, young adults are significantly more likely than older drinkers to report tolerance to alcohol and drinking more than intended (larger/longer), although withdrawal was very infrequently reported by the German respondents of all ages (Pabst et al., 2012).
Young drinkers also may report drinking more or longer than intended due to easy access to low-cost alcohol, peer pressure to continue drinking or a lack of clear intentions about personal and situational drinking limits, rather than a compulsion to drink alcohol (Hasin et al., 2003). A recent study conducted in Australia found that young adult drinkers report a variety of attributions for drinking more than intended, with the vast majority of those being social and other non-compulsion reasons (Slade et al., 2013).
The current study
To better understand age-related patterns of AUD symptomology and improve classification of AUD in a general population sample, this study focused on two commonly-reported symptom domains in younger adults (ages 18–45): withdrawal and drinking larger amounts or over longer periods than intended (larger/longer). Research conducted almost 20 years ago showed these domains were highly prevalent at low levels of AUD severity in general population samples, including among respondents who failed to meet diagnostic thresholds defined by either DSM or International Classification of Disease (ICD) criteria (Caetano and Tam, 1995). As Table 1 suggests, these domains still predominate among respondents with no AUD or mild AUD in the 2010 NAS, as well as in the 2001–2002 NESARC (Wave 1) sample, which was collected almost 10 years earlier. Reports of tolerance also are highly prevalent among young and non-dependent drinkers (Harford et al., 2009), however due to variation in tolerance by biological factors such as sex, metabolism, body mass index and muscle mass (Kalant, 2000; Nolen-Hoeksema, 2004; Thomasson, 1995; Thomasson, 2000), which are difficult to assess in population surveys, we emphasize withdrawal and drinking more than intended in the current study.
Table 1.
Proportions of current drinkers under age 45 reporting DSM-5 AUD criteria, by total number of domains endorsed
| Current Study (N = 225) | 2010 NAS (N = 4,048) | 2001–02 NESARC (N = 17,820) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| Overall domain count1 | Overall domain count | Overall domain count | |||||||||||||
| Symptom domains | 1 | 2–3 | 4–5 | 6+ | Total | 1 | 2–3 | 4–5 | 6+ | Total | 1 | 2–3 | 4–5 | 6+ | Total |
| Withdrawal | 13.5 | 22.9 | 88.9 | 75.0 | 11.0 | 5.9 | 22.6 | 62.1 | 83.0 | 8.3 | 9.9 | 35.5 | 61.0 | 86.3 | 10.1 |
| More/longer than intended | 8.1 | 34.3 | 66.7 | 87.5 | 12.4 | 14.4 | 29.8 | 75.6 | 90.4 | 11.0 | 25.7 | 59.2 | 84.6 | 95.9 | 16.0 |
| Tolerance | 10.8 | 22.9 | 55.6 | 75.0 | 10.3 | 17.6 | 45.9 | 65.1 | 81.1 | 12.6 | 13.8 | 33.7 | 64.5 | 82.7 | 10.4 |
| Desire/efforts to cut down/control | 5.4 | 11.4 | 44.4 | 87.5 | 7.6 | 8.8 | 16.7 | 60.5 | 76.8 | 7.8 | 22.8 | 39.8 | 65.1 | 79.7 | 12.2 |
| Use despite physical/psychological problems | 0 | 8.6 | 11.1 | 100 | 5.3 | 2.7 | 3.8 | 22.1 | 74.7 | 4.2 | 1.8 | 13.1 | 39.8 | 86.3 | 5.7 |
| Giving up important activities | 0 | 8.6 | 22.2 | 75.0 | 4.9 | 1.9 | 9.9 | 16.3 | 68.1 | 4.3 | 0.1 | 1.0 | 3.7 | 36.1 | 1.3 |
| Time spent to obtain/use/recover | 0 | 0 | 11.1 | 37.5 | 1.8 | 0 | 1.7 | 9.2 | 48.4 | 2.2 | 0.4 | 5.8 | 28.9 | 72.0 | 3.9 |
| Craving | 32.4 | 68.6 | 77.8 | 87.5 | 22.2 | 1.8 | 2.3 | 6.8 | 26.2 | 1.5 | --- | --- | --- | --- | --- |
| Use despite social/interpersonal problems | 29.7 | 60.0 | 88.9 | 75.0 | 20.4 | 27.7 | 58.9 | 78.2 | 90.5 | 16.3 | 1.6 | 6.6 | 22.4 | 64.4 | 3.7 |
| Failure to fulfill role obligations | 0 | 0 | 0 | 12.5 | 0.4 | 0.3 | 4.5 | 13.8 | 30.9 | 2.1 | 0 | 1.1 | 6.8 | 44.2 | 1.7 |
| Drinking in hazardous situations | 0 | 0 | 0 | 12.5 | 0.4 | 20.2 | 37.0 | 33.7 | 46.3 | 9.7 | 24.0 | 39.3 | 63.4 | 84.2 | 12.4 |
In DSM-5, three levels of AUD severity are possible: mild (symptoms in 2–3 domains), moderate (4–5 domains) and severe (6 or more domains).
Note. Current study included two indicators of craving, and the 2010 NAS included one indicator. The NESARC Wave 1 survey did not assess craving; only 10 of the 11 DSM-5 AUD domains were represented in overall domain count for this survey.
Our guiding hypotheses are that (1) younger to middle-aged general population survey respondents over-report withdrawal due to misperception of relatively minor, short-term effects of heavy episodic drinking (HED) as physiological symptoms of withdrawal, and (2) most respondents consume alcohol in larger amounts or for longer periods of time than intended due to social reasons, rather than because of a compulsion to drink or an actual loss of control over use. We further speculated that these effects would be more pronounced among the younger respondents in our sample, as they would be more likely to have recently initiated HED and are likely to consume greater alcohol volumes per occasion than older non-dependent drinkers (Kerr et al., 2009).
Materials and Methods
This pilot study was conducted as a follow-up to the 2010 National Alcohol Survey (NAS). The 2010 NAS was a survey of the US adult population ages 18 and older (N = 7,969) utilizing random digit dialing of landlines and cell phones and computer-assisted telephone interviews (CATI) in English and Spanish. In the 2010 NAS, the prevalence of past-year AUD was 21% for respondents ages 18–23, 14% for ages 24–30, and 9% for ages 31–45, with about 8% of respondents under age 46 classified as mild, 2% as moderate, and 3% as severe AUD. New follow-up items for several AUD symptoms were developed by the study team and reviewed by an expert in measurement of AUD. As a key aim of the current study was to develop and pilot test these new follow-up items with a group of high-risk drinkers, sampling from the 2010 NAS provided a unique opportunity to identify respondents with a higher likelihood of meeting the criteria for AUD, which is relatively rare in the general population.
Survey methods
In the current NAS follow-up study, we conducted CATIs with a sub-sample of adults ages 18–45 who reported at least 1 lifetime AUD symptom, as well as a smaller group who reported past-year HED (5+ drinks in one day) but no lifetime AUD symptoms (by design). We drew a quota sample of respondents from the 2010 NAS using strata defined by age (targeting 33% from each: ages 18–25, 26–35, and 36–45 in 2010) and AUD symptom prevalence (targeting 60% with 1+ past-year AUD symptom, 30% with 1+ lifetime symptom but without past-year symptoms, and 10% with past-year heavy drinking and no history of AUD symptoms). At the end of data collection, we supplemented the samples of the two youngest age strata with a few interviews (n= 17) from past-year drinkers who did not meet AUD or heavy-drinking criteria in order to increase the representation of these younger adults in the sample. Due to budget limitations, the sample was limited to English-speaking respondents (23 otherwise eligible respondents were excluded).
About half (56%) of the 2010 NAS respondents drawn for the current sample had an address on file, to which we sent advance notification letters describing the study. Over a 5-month period in early 2012, the NAS fieldwork agency conducted 244 interviews for the study. Interviewers made up to 15 call-back attempts on different days and times to reduce non-response bias. We were able to resolve the eligibility status for 82% of the current study sample, with 51% of the cases determined to be eligible in 2012, and 34% of eligible cases agreeing to participate (overall response rate 29%). To avoid household mismatches, respondents’ identities were verified using 2010 NAS data on respondent’s name (if available), date of birth, gender, and, if necessary, city of residence in 2010, age they started drinking and race/ethnicity. Interviews lasted approximately 30 minutes, and respondents received a $25 gift code to a major online retailer in compensation for their time. All study protocols (for both 2010 NAS and current study) were approved by the Institutional Review Board of the Public Health Institute, Oakland, CA.
Those who completed the follow-up interview in 2012 had an average age of 36 years, and 51% were male. Compared to all eligible respondents from the 2010 NAS, respondents with complete follow-up interviews were significantly more likely to be White (77% vs. 59%) and significantly more were college graduates (55% respondents vs. 43% eligibles). There were no significant differences in rates of heavy drinking among past-year drinkers (11% respondents, 13% eligibles), rates of past-year AUD (13% respondents vs. 15% eligibles) or reports of lifetime alcohol treatment (4% respondents, 5% eligibles). The analysis sample for the current study includes 225 respondents who were past-year drinkers at follow-up.
Measures
We assessed lifetime and past-year occurrence of alcohol use disorder symptoms using standard items that have been used in the NAS series since 1990 (Caetano and Tam, 1995). With a few exceptions (such as item phrasing on withdrawal items, which refer to “when the effects of alcohol are wearing off” in the NESARC), these items are similar to those used in the NESARC (which are based on the Alcohol Use Disorder and Associated Disabilities Interview Schedule, AUDADIS; Grant et al., 1995) and, importantly, result in similar population estimates of AUD across the two surveys despite their differences. Endorsement of individual symptom domains varies somewhat across the two instruments (see Table 1), with the largest difference evident for social problems (more prevalent in the NAS), drinking more than intended (more prevalent in the NESARC) and desire to cut down (more prevalent in the NESARC) among respondents with symptoms in just 1–2 domains. The follow-up interview targeted the domains of physiologic withdrawal and drinking alcohol in larger amounts and/or for longer time than intended. Respondents indicating that they had ever experienced symptoms in either domain were asked targeted follow-up questions, as described below.
Withdrawal
Withdrawal was ascertained using 6 items, 3 of which are possible to interpret in relation to an episode of heavy drinking (“I was sick or vomited after drinking or the morning after drinking”, “Sometimes I have awakened during the night or early morning sweating all over because of drinking” and “I was depressed, irritable or nervous after drinking or the morning after drinking”). For each of these questions, a follow-up item prompted respondents to think about the most recent occasion that the symptom occurred and asked how much time had elapsed since they had finished drinking before they experienced the reported symptom. (“The most recent time this happened, about how long after you had finished drinking did you… get sick? wake up sweating? feel depressed, irritable or nervous after drinking?”) Anchoring the follow-up questions to the last symptom occurrence served two functions: (1) Given that withdrawal is theorized to develop over time (Edwards and Gross, 1976), this would ostensibly index a recent serious occasion for currently dependent heavy drinkers, and (2) It would provide a distinct reference point to facilitate recall (Midanik and Hines, 1991). Response options were “was still drinking”, “less than 3 hours after stopping drinking”, “4–8 hours after stopping drinking” and “more than 8 hours after stopping drinking”, with all responses of less than 8 hours coded as likely due to acute intoxication, not withdrawal. The 8-hour cut-point was chosen based on a generalized alcohol elimination rate of approximately one drink per hour (Brick, 2006). Past-year withdrawal was re-coded using the 3 adjusted values (with items appearing to represent acute intoxication coded as negative for withdrawal) and the unadjusted values for the other withdrawal symptom (“My hands shook a lot in the morning after drinking”), as well as unadjusted values for two items assessing drinking to relieve symptoms of withdrawal (“I found that I needed a drink to keep from getting the shakes or becoming sick” and “I have taken a strong drink in the morning to get over the effects of last night’s drinking”). Respondents were coded as positive for withdrawal if they reported two or more of the four withdrawal symptoms or if they endorsed at least one item indicating drinking to relieve withdrawal.
Drinking larger amounts/over longer periods than intended
The larger/longer criterion was ascertained using 2 items (“Once I started drinking it was difficult for me to stop before I became completely intoxicated” and “I sometimes kept on drinking after I had promised myself not to”). Respondents positively endorsing either question (or both) were asked 2 follow-up items: “Sometimes when people drink more than they had planned, it is because they get caught up in drinking with a group of friends. Has this ever been true for you?” and “Sometimes when people drink more than they had planned, it is because they feel compelled to drink and just can’t stop. Has this ever been true for you?” To reduce the possibility of over-adjustment of this symptom domain, these items were phrased in terms of lifetime occurrence to allow reporting of compulsion to drink that may have occurred prior to the past year. Past-year drinking more than intended was re-coded using the adjusted values, with all respondents who reported only social reasons for drinking more than intended (answering “no” to the second item on compulsion to drink) coded as negative for the past-year larger/longer criterion. Regardless of whether they endorsed social reasons for drinking more than intended, any respondent affirming the second item on compulsion to drink was left as positive for the past-year larger/longer criterion.
AUD status
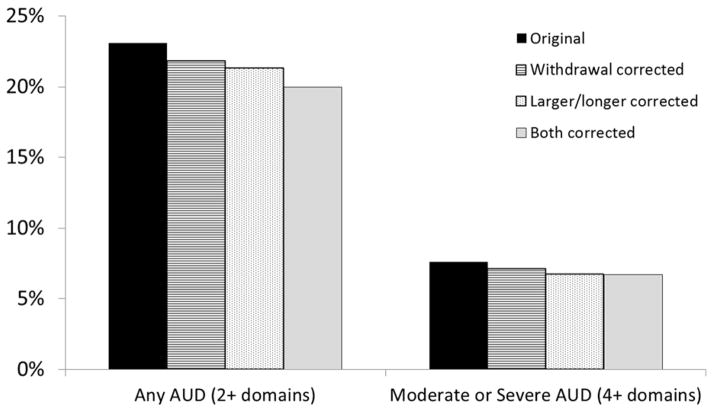
The original and adjusted AUD classifications were based on DSM-5 AUD criteria (endorsing symptoms in 2 or more of the 11 domains; American Psychiatric Association, 2013). Using the unadjusted symptom domain counts, 23% (n =52) met DSM-5 criteria for AUD. In addition to the original, unadjusted AUD classification, there were three adjusted AUD classifications: one using the new withdrawal status (all other domains remained as originally reported), another using the new larger/longer indicator (all other domains as originally reported), and the last integrating revisions for both withdrawal and larger/longer (all other domains as originally reported). An additional variable designated those respondents who changed AUD status once both adjustments were taken into account; 20% were still classified as having an AUD, 3% were reclassified as not having an AUD, and 77% were never classified as having an AUD.
Drinking pattern and other validating variables
Past-year drinking pattern was assessed using a graduated quantity-frequency approach asking about the frequency of drinking 1–2, 3–4, 5–7, 8–11 and 12+ drinks in the prior 12 months. This graduated quantity-frequency approach is very effective for measuring consumption among individuals who occasionally drink heavily (Greenfield, 2000). From this measure, we calculated the total volume (number of drinks/year), volume from light drinking days (days having just 1–4 drinks) and volume from heavy drinking days (days having 5 or more drinks), as well as the frequency of drinking (number of days/year), frequency of light drinking, frequency of heavy drinking, and frequency of very heavy drinking (days having 8 or more drinks). We also assessed the frequency of drunkenness in the past year. In addition to respondent age at the time of the survey, we ascertained the age they started drinking and the age at which their period of heaviest drinking began. We also asked whether either biological parent was a problem drinker or alcoholic, as well as the number of significant others who had suggested in the past year they should drink less or act differently when drinking.
Analysis Strategy
Given the exploratory nature of the study and the relatively small sub-samples of respondents meeting AUD criteria, analyses consisted of bivariate associations. Comparisons of original and adjusted AUD classifications were assessed using chi-squares, and associations between the severity measures and the indicators of changed AUD status were assessed using chi-squares and ANOVAs.
Results
Withdrawal
Of 225 current drinkers, 11% reported past-year withdrawal symptoms. Follow-up items indicated 28% of those cases may have been reporting effects of acute intoxication instead of physical withdrawal symptoms, because every reported “withdrawal” symptom had occurred within 8 hours of stopping drinking (most reported that symptoms occurred within 3 hours of stopping drinking). After adjustment, the prevalence of past-year withdrawal symptoms was reduced from 11% to 8% of current drinkers. Respondents who remained classified as positive for withdrawal symptoms in the past year had significantly higher frequencies of very heavy drinking (8+ per occasion; M=56 days in past year, SD=93) than their counterparts who were reclassified as negative for withdrawal symptoms (M=2 days, SD=4; t(17.2)=-2.41, p<.05) and they were significantly more likely to report getting drunk at least monthly in the past year (72% vs. 29%, chi-square(N=25, df=1)=4.0, p<.05). Adjusting past-year AUD classifications using the adjusted withdrawal indicator reduced AUD prevalence by 6% (from 23% to 22% of past-year drinkers).
Drinking more than intended
A small proportion (12%) of current drinkers reported the past-year larger/longer criterion (drinking more than intended or drinking over a longer time period than intended). Of those, 50% indicated only social reasons for drinking more than intended, rather than drinking more than intended due to a compulsion to drink; after adjustment, 6% of current drinkers were classified as meeting the past-year larger/longer criterion. Respondents who remained classified as meeting the larger/longer criterion in the past year had significantly higher frequencies of heavy drinking (M=127 days drinking 5+ drinks in past year, SD=128) than their counterparts who were reclassified as negative (M=32 days, SD=42; t(11.7)=-2.36, p<.05), with significantly more of these respondents drinking 5+ drinks at least weekly over the past year (64% vs. 21%, chi-square(N=25, df=1)=4.57, p<.05). Adjusting past-year AUD classifications using the adjusted larger/longer indicator reduced DSM-5 AUD prevalence by 8% (from 23% to 21% of past-year drinkers).
Adjusting both symptom domains
The larger/longer adjustment changed the DSM-5 AUD classification for 94% (n = 45) of the same respondents as the withdrawal adjustment. In addition, the larger/longer adjustment changed classification for an additional 4 respondents and left unadjusted another 3 respondents with revised withdrawal classifications. Simultaneously accounting for both adjustments reduced AUD prevalence by 13% (from 23% to 20% of past-year drinkers). Figure 1 shows the percentage of past-year drinkers meeting the DSM-5 AUD criteria according to the original, unadjusted domains, as well as according to criteria incorporating the adjusted withdrawal status, criteria using the adjusted larger/longer indicator, and criteria integrating adjustments for both withdrawal and larger/longer. Proportions are presented for any AUD, as well as for moderate or severe AUD (4 or more of the 11 criteria).
Figure 1.
Percentage of past-year drinkers meeting criteria for DSM-5 alcohol use disorder using original and adjusted criteria.
We anticipated the adjustments would have a greater impact on AUD classification for younger drinkers. Figure 2 displays percentages of respondents meeting AUD criteria for both age strata according to frequency of HED (5+ drinks) in the past year. Rates of AUD rose as frequency of HED increased for both age groups. Counter to expectations, none of the age differences were significant (all exact p > .05), despite increased representation of younger drinkers in the groups meeting AUD criteria.
Figure 2.
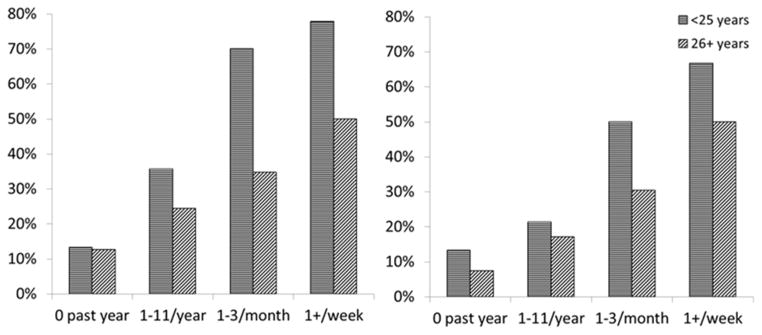
Percentage of past-year drinkers meeting DSM-5 criteria for an alcohol use disorder (symptoms in 2 or more domains) using original criteria (left panel) and adjusted criteria (right panel), by age and frequency of 5+ drinking
The final analysis step compared demographic characteristics, alcohol consumption and problem severity for cases that remained categorized as having an AUD under the adjusted classification scheme with those that were reclassified as non-AUD, as well as comparing reclassified cases with those that were never classified as having an AUD. As shown in Table 2, there were significant differences across these three groups in terms of whether a biological parent had an alcohol problem, whether someone had suggested the respondent drink less or act differently when drinking in the past year, frequent heavy drinking and drunkenness in the past year, and volume and frequency of alcohol consumption in the past year. Generally, cases that were still classified as having an AUD after both withdrawal and larger/longer criteria were adjusted were heavier drinkers than those who were reclassified as not having an AUD. These cases, in turn, were more frequent heavy drinkers than those who were never classified as having an AUD. There were no significant differences on most demographic variables (including age of onset of drinking and age when period of heaviest drinking began) across these three groups. Distribution of AUD symptoms across these three groups are presented in Table 3. Cases that were reclassified were less severe than their counterparts still classified as having an AUD.
Table 2.
Differences between past-year drinkers who retained their original AUD classification, those who were reclassified as non-AUD using the adjusted withdrawal and larger/longer criteria, and those who were never classified as having an AUD
| Still have AUD (n=45) | Reclassified as no AUD (n=7) | Never had AUD (n=173) | |
|---|---|---|---|
| College graduate (%) | 57.8 | 57.1 | 63.0 |
| Age at time of follow-up survey (mean) | 33.8 | 34.1 | 36.4 |
| Age started drinking (mean) | 17.3 | 18.6 | 18.2 |
| Age period of heaviest drinking started (mean) | 22.8 | 20.7 | 21.4 |
| Biological parent had alcohol problem (%) | 33.3 | 71.4 | 19.7** |
| At least 1 significant other suggested should drink less/act differently when drinking, past year (%) | 44.4 | 14.3 | 1.2** |
| Had 5+ drinks per day at least once a week, past year (%) | 33.3 | 0 | 6.9** |
| Got drunk at least once a month, past year (%) | 37.8 | 28.6 | 4.6** |
| Volume of alcohol consumed, past year (number of drinks) | |||
| Total volume (mean) | 832 | 257 | 264** |
| Volume from light drinking days 1 (mean) | 181 | 164 | 194** |
| Volume from heavy drinking days 2 (mean) | 518 | 76 | 100** |
| Frequency of drinking, past year (number of days) | |||
| Total drinking days (mean) | 197 | 100 | 100** |
| Light drinking days 1 (mean) | 134 | 90 | 85* |
| Heavy drinking days 2 (mean) | 62 | 9 | 15** |
| Very heavy drinking days 3 (mean) | 28 | 4 | 4** |
Overall significance test (F-test or chi-square):
p < .05.
p < .01.
Light drinking days: days consumed 1–4 drinks
Heavy drinking days: days consumed 5 or more drinks
Very heavy drinking days: days consumed 8 or more drinks
Table 3.
Symptoms reported by past-year drinkers who retained their AUD classification, those who were reclassified as non-AUD, and those who were never classified as having an AUD
| Symptom domains | Still have AUD (n=45) | Reclassified as no AUD (n=7) | Never had AUD (n=173) |
|---|---|---|---|
| Withdrawal (uncorrected %) | 84.8 | 71.4 | 20.2 |
| Withdrawal (corrected %) | 48.9 | 0 | 4.0 |
|
| |||
| More/longer than intended (uncorrected %) | 46.7 | 57.1 | 1.7 |
| More/longer than intended (corrected %) | 28.9 | 0 | 0.6 |
|
| |||
| Craving (%) | 77.8 | 42.9 | 6.9 |
| Use despite social/interpersonal problems (%) | 71.1 | 42.9 | 6.4 |
| Tolerance (%) | 40.0 | 14.3 | 2.3 |
| Desire/efforts to cut down/control (%) | 33.3 | 0 | 1.2 |
| Use despite physical/psychological problems (%) | 26.7 | 0 | 0 |
| Giving up important activities (%) | 24.4 | 0 | 0 |
| Time spent to obtain/use/recover (%) | 8.9 | 0 | 0 |
| Failure to fulfill role obligations (%) | 2.2 | 0 | 0 |
| Drinking in hazardous situations (%) | 2.2 | 0 | 0 |
|
| |||
| Mean # domains endorsed (uncorrected %) | 3.7 | 2.0 | 0.2 |
| Mean # domains endorsed (corrected %) | 3.5 | 1.0 | 0.2 |
Discussion
Using a follow-up interview conducted with heavy-drinking respondents in the 2010 National Alcohol Survey, results from this pilot study suggest there could be measurement error in respondents’ reports of withdrawal and drinking larger amounts or drinking for longer than intended (larger/longer) in general population surveys of young and middle-age adults. A relatively simple set of follow-up items identified respondents who may have misinterpreted physiologic withdrawal symptoms or confused them with acute intoxication effects. Two other items differentiated respondents who drank more than intended for purely social reasons from those who reported doing so due to a compulsion to drink. A recent study conducted in Australia with drinkers ages 18–24 found that most respondents who reported drinking more than intended did so for social reasons, rather than a compulsion to drink (Slade et al., 2013). However, it is possible that some individuals who attribute drinking more than intended solely to social context may be denying or ignoring a compulsion to drink, which may result in false negatives for this symptom domain. As noted above, in this small sample, respondents who reported only social motives for drinking more than intended were significantly lighter drinkers than those who reported a compulsion to drink. They also were less likely to report other indicators of impaired control over drinking, such as unsuccessful attempts to cut down. Nevertheless, additional queries to better assess respondents’ compulsion to consume alcohol may be informative.
Adjustment for possible reporting errors in both the withdrawal and larger/longer domains substantially affected the proportion of respondents classified as meeting DSM-5 AUD criteria in this sample. Differences in rates of AUD were most pronounced when both domains were simultaneously adjusted. This suggests that errors in reporting were not limited to one group of respondents; rather, those who over-reported withdrawal differed somewhat from those who endorsed only social motives for drinking more than intended. It is notable that after adjusting both the withdrawal and larger/longer domains, the most prevalent symptom domains reported were craving (22% of past-year drinkers) and drinking despite social/interpersonal problems (20%). Asking follow-up questions about craving may be indicated, as this domain also is meant to tap physiological dependence, rather than alcohol abuse (as is the case for social problems).
Counter to expectations, separate examination of two age cohorts revealed that errors in reporting these two AUD criteria are not limited to young heavy drinkers in this sample. A recent study using data from the Wave 2 NESARC also suggests that factors other than age may be related to the reporting of particular AUD symptoms (Casey et al., 2012). Results from both of these U.S. studies are counter to those from a German study, which found persistent age differences in reports of drinking more than intended (Pabst et al., 2012), however.
Results should be interpreted in light of the following limitations. First, the sample size was quite small, particularly for analyses stratifying by age. This limited the power for multivariate modeling and more advanced analysis of the data. Item response theory (IRT) analyses comparing severity and discrimination ability of both adjusted and unadjusted symptom reports would be very informative. Second, the sample was not representative of the larger national survey sample from which it was drawn. In addition to a low follow-up rate, White college graduates were over-represented in this small sample; thus, future research should assess the impact of these adjustment factors on a more representative sample of adult drinkers to determine whether these findings persist with more demographically diverse respondents. Further psychometric assessment (such as test-retest reliability) of the follow-up items is warranted. Debriefing with respondents could reveal whether framing the withdrawal symptoms in terms of the most recent occasion adequately represented past-year symptoms (that is, whether respondents experienced a prior episode of anxiety, depression or irritability more than 8 hours after stopping drinking not captured by the question as worded). A qualitative assessment of respondents’ responses to the specific items also might elucidate differences across groups of respondents that affect how they answer items about negative consequences of their own alcohol consumption. For example, it is possible that respondents with a family history of alcohol use disorders could be more sensitive to after-effects of their own drinking, and thus endorse AUD symptoms that, upon clarification, may not be actual indicators of AUD. Further measurement development work also may identify other brief clarification questions or phrasing (such as clarifying that withdrawal is not the same as a hangover, or that withdrawal most likely would be preceded by a period of relatively heavy, chronic drinking that was followed by a period of abstinence), which may help respondents more accurately assess their own alcohol problems. Finally, we note the DSM specifies 8 criteria to assess withdrawal; our survey addressed the 6 most common, less severe criteria. It is possible that some respondents could have been missed by omission of items assessing withdrawal-related hallucinations and seizures; however, in a general population sample, it seems probable that other withdrawal indicators would have been endorsed by these respondents.
Despite these limitations, results from this pilot study suggest follow-up items could be implemented in epidemiologic studies with minimal response burden and may substantially reduce misclassification of AUD. As such, preliminary recommendations for future population-based surveys are to ask about the amount of time elapsed between stopping drinking and withdrawal symptom occurrence, and to ask about motives for drinking larger amounts of alcohol over longer periods than intended in order to assess the possibility of misclassification in larger, more representative samples.
Acknowledgments
This work was supported by the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health (pilot study directed by K. Karriker-Jaffe; funded by P50AA005595, T. Greenfield, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health. The authors would like to thank Dr. Deborah Hasin for her suggestions during the formative stages of this study and the anonymous reviewers for their ideas about how to strengthen the manuscript.
The current study was approved by the Institutional Review Board of the Public Health Institute, Oakland, CA.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- Brick J. Standardization of alcohol calculations in research. Alcohol Clin Exp Res. 2006;30(8):1276–1287. doi: 10.1111/j.1530-0277.2006.00155.x. [DOI] [PubMed] [Google Scholar]
- Caetano R, Babor TF. Diagnosis of alcohol dependence in epidemiological surveys: an epidemic of youthful alcohol dependence or a case of measurement error? Addiction. 2006;101(Suppl 1):111–114. doi: 10.1111/j.1360-0443.2006.01599.x. [DOI] [PubMed] [Google Scholar]
- Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence: 1990 U.S. National Alcohol Survey. Alcohol Alcohol. 1995;30(2):177–186. [PubMed] [Google Scholar]
- Casey M, Adamson G, Shevlin M, McKinney A. The role of craving in AUDs: Dimensionality and differential functioning in the DSM-5. Drug and Alcohol Dependence. 2012;125:75–80. doi: 10.1016/j.drugalcdep.2012.03.019. [DOI] [PubMed] [Google Scholar]
- Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. British Medical Journal. 1976;1:1058–61. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39(1):37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Greenfield TK. Ways of measuring drinking patterns and the difference they make: experience with graduated frequencies. J Subst Abuse. 2000;12(1):33–49. doi: 10.1016/s0899-3289(00)00039-0. [DOI] [PubMed] [Google Scholar]
- Harford TC, Yi H-y, Faden VB, Chen CM. The dimensionality of DSM-IV alcohol use disorders among adolescent and adult drinkers and symptom patterns by age, gender, and race/ethnicity. Alcohol Clin Exp Res. 2009;33(5):868–878. doi: 10.1111/j.1530-0277.2009.00910.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Schuckit MA, Martin CS, Grant BF, Bucholz KK, Helzer JE. The validity of DSM-IV alcohol dependence: what do we know and what do we need to know? Alcohol Clin Exp Res. 2003;27(2):244–52. doi: 10.1097/01.ALC.0000060878.61384.ED. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hesselbrock VM, Hesselbrock MN. Are there empirically supported and clinically useful subtypes of alconol dependence? Addiction. 2006;101(Suppl 1):97–103. doi: 10.1111/j.1360-0443.2006.01596.x. [DOI] [PubMed] [Google Scholar]
- Kalant H. Effects of food and body composition on blood alcohol curves. Alcohol Clin Exp Res. 2000;24(4):413–414. [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age-period-cohort modeling of alcohol volume and heavy drinking days in the US National Alcohol Surveys: divergence in younger and older adult trends. Addiction. 2009;104(1):27–37. doi: 10.1111/j.1360-0443.2008.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik L, Hines AM. “Unstandard” ways of answering standard questions: protocol analysis in alcohol survey research. Drug Alcohol Depend. 1991;27(3):245–252. doi: 10.1016/0376-8716(91)90007-l. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Greenfield TK, Bond J. Addiction sciences and its psychometrics: the measurement of alcohol-related problems. Addiction. 2007;102(11):1701–1710. doi: 10.1111/j.1360-0443.2007.01886.x. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clinical Psychology Review. 2004;24(8):981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Pabst A, Kraus L, Piontek D, Baumeister SE. Age differences in diagnostic criteria of DSM-IV alcohol dependence among adults with similar drinking behaviour. Addiction. 2012;107(2):331–338. doi: 10.1111/j.1360-0443.2011.03611.x. [DOI] [PubMed] [Google Scholar]
- Rose JS, Lee C-T, Selya AS, Dierker LC. DSM-IV alcohol abuse and dependence criteria characteristics for recent onset adolescent drinkers. Drug and Alcohol Dependence. 2012;124:88–94. doi: 10.1016/j.drugalcdep.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006;36(7):931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Danko GP, Smith TL, Bierut LJ, Bucholz KK, Edenberg HJ, Hesselbrock V, Kramer J, Nurnberger JI, Jr, Trim R, Allan R, Kreikebaum S, Hinga B. The prognostic implications of DSM-IV abuse criteria in drinking adolescents. Drug Alcohol Depend. 2008;97(1–2):94–104. doi: 10.1016/j.drugalcdep.2008.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T, Teeson M, Mewton L, Memedovic S, Krueger RF. Do young adults interpret the DSM diagnostic criteria for alcohol use disorders as intended? A cognitive interviewing study. Alcoholism: Clinical and Experimental Research. 2013;37(6):1001–1007. doi: 10.1111/acer.12063. [DOI] [PubMed] [Google Scholar]
- Thomasson HR. Gender differences in alcohol metabolism: physiological responses to ethanol. In: Galanter M, editor. Recent Developments in Alcoholism: Alcoholism and women. Vol. 12. Plenum Press; New York: 1995. pp. 163–179. [DOI] [PubMed] [Google Scholar]
- Thomasson HR. Alcohol elimination: faster in women? Alcohol Clin Exp Res. 2000;24(4):419–420. [PubMed] [Google Scholar]