Abstract
Constipation is one of the most common function bowel disorders encountered by primary care providers and gastroenterologists. Disorders of chronic constipation, including irritable bowel syndrome with constipation, chronic idiopathic constipation, and opioid-induced chronic constipation, are associated with significant medical costs and a negative impact on quality of life. Although there is evidence supporting the effectiveness of some over-the-counter laxatives in chronic constipation, currently there is no evidence supporting lifestyle modification, dietary change or over-the-counter laxatives as effective long-term therapy for patients with chronic constipation. Lubiprostone is a prostaglandin-derived bicyclic fatty acid available to use for long-term treatment of constipation. Lubiprostone works by increasing intraluminal chloride ion secretion, which results in a passive influx of water and sodium, leading to increased intestinal peristalsis and colonic laxation with decreased intestinal stool transit time. Randomized, double-blind, placebo-controlled trials of lubiprostone in patients with chronic constipation, irritable bowel syndrome and opioid-induced constipation have shown it to be effective and free of serious adverse effects. The most common side effects associated with lubiprostone are mild to moderate nausea and diarrhea. Currently lubiprostone is approved for treatment of chronic constipation and opioid-induced constipation for men and women at 24 µg twice daily and for treatment of irritable bowel syndrome with constipation in women at 8 µg twice daily. Additional research continues to shed light on the molecular mechanisms of lubiprostone and further work may expand its clinical applications.
Keywords: chronic constipation, irritable bowel syndrome, lubiprostone, chloride ion secretion
Introduction
Chronic constipation and irritable bowel syndrome (IBS), as defined by the Rome III criteria (Table 1), are both common functional bowel disorders. It is estimated that these conditions may affect between 10 and 27% of the Western population [Everhart et al. 1989; Drossman et al. 1993; Pare et al. 2001; Saito et al. 2002; Higgins and Johanson, 2004; Longstreth et al. 2006]. There is also a growing recognition in the literature of the prevalence of these conditions in non-Western countries worldwide [Tan et al. 2003; Husain et al. 2008; Khoshkrood-Mansoori et al. 2009]. Yet despite this prevalence, these conditions are undertreated with only 26% of patients who meet Rome III criteria for chronic constipation seeking medical attention [Stewart et al. 1999].
Table 1.
Rome III diagnostic criteria for functional constipation and IBS [Longstreth et al. 2006].
| Functional constipation: (criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis) |
|
| Irritable bowel syndrome: (criterion fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis) |
Recurrent abdominal pain or discomfort at least 3 days per month in the last 3 months associated with two or more of the following:
|
Constipation is also the most common adverse effect of opioid medications. It is estimated that 100 million adults in the US have chronic pain [Institute of Medicine, 2011] and opioid therapy is central to the management of chronic moderate-to-severe noncancer pain [Fine et al. 2009]. Opioid-induced constipation may affect approximately 41% of these patients and often imposes a further burden upon their quality of life beyond the chronic pain [Kalso et al. 2004]. Together these conditions are associated with significant costs related to medical expenses as well as decreased productivity and absenteeism [Levy et al. 2001; Sandler et al. 2002]. In the US, for instance, IBS accounts for between 25 and 50% of referrals to gastroenterologists and has an estimated economic burden of $20–25 billion annually [Chey et al. 2012a].
The goals of treatment in constipation are to allow complete and spontaneous bowel movements with associated improvements in quality of life. For those patients seeking medical attention, the first step is typically lifestyle modification including adequate fluid intake, high fiber diet and regular physical activity; however, there is little evidence to support these measures [Young et al. 1998; Bosshard et al. 2004; Tuteja et al. 2005]. Lifestyle modifications are often followed by the addition of over-the-counter (OTC) laxatives including bulk laxatives, stimulants, osmotic laxatives and emollients. Current data support the use of a soluble supplement such as ispaghula/psyllium. An estimated $800 million is spent annually on over-the-counter laxatives in the US, and although some patients may benefit from the addition of these agents, there are limited data to support their long-term use [Jones et al. 2002]. Furthermore, many patients become refractory to one or more OTC laxatives with chronic use, which may cause frustration for both the clinician and the patient, and ultimately leads many patients to abandon therapy and remain dissatisfied with their condition. A survey of over 500 patients who met Rome III criteria for chronic constipation revealed that 96% were using OTC laxatives, yet nearly a half of respondent were dissatisfied with current treatment options [Johanson and Kralstein, 2007]. Intestinal secretion has been the subject of active research for the development of treatments for chronic constipation and IBS with constipation (IBS-C) in the past decade. For patients whose symptoms persist despite these interventions there are other therapeutic options. These are as follows:
Linaclotide – acts peripherally on the guanylate cyclase C (GC-C) receptor located on the luminal surface of intestinal epithelial cells [Chey et al. 2012; Rao et al. 2012b].
Prucalopride – a selective 5-HT4 receptor agonist with prokinetic activity that is known to accelerate colonic transit and improve constipation related complaints; it is not approved by the US Food and Drug Administration (FDA) [Camilleri et al. 2010].
Lubiprostone – a highly selective chloride channel activator.
Emerging novel therapies that are currently under clinical investigation (i.e. bile acid modulators, non linaclotide GC-C receptor agonists, sodium reuptake inhibitors and partial 5-HT3 receptor agonists) will be the focus of our future reviews. This review focuses on the pharmacology and clinical applications of lubiprostone, a chloride channel activator, for treatment of constipation-related disorders.
Chloride channels
Chloride channels (ClCs) are cell-membrane bound protein pores involved in chloride secretion that are found throughout the body [Lipecka et al. 2002]. ClCs are principally involved in transport of fluid and ions across epithelial cell membranes for the purposes of secretion and fluid transport, maintenance of cell volume and pH, and regulation of cell membrane potential [Chapman et al. 1985]. A total of nine ClC subtypes have been described [Lipecka et al. 2002].
ClC type 2 (ClC-2) channels are expressed in the stomach, intestine, colon, heart, brain and muscles. In the intestine, ClC-2 is expressed on both the basal and apical cell surfaces. Another major epithelial cell membrane ClC is the cystic fibrosis transmembrane conductance regulator (CFTR). The CFTR protein is also involved in chloride and water secretion, and is expressed in multiple tissue types across the body. Absent or dysfunctional CFTR protein leads to the disordered transepithelial ion and fluid transport that causes cystic fibrosis [Cuppoletti et al. 2004; Jentsch, 2008].
Lubiprostone
Lubiprostone (Amitiza®, Sucampo Pharmaceuticals, Bethesda & Takeda Pharmaceuticals of North America) is a bicyclic fatty acid derived from a metabolite of prostaglandin E1 (PGE1) (Figure 1) [Cuppoletti et al. 2004; Camilleri et al. 2006]. It is commercially available as a gelatin capsule in 2 dosages, 8 and 24 µg. Lubiprostone acts within the gastrointestinal (GI) lumen and has a rapid onset of action. When administered orally, lubiprostone has poor absorption by the gut. As a result there is limited systemic availability and serum concentrations of lubiprostone are too low to quantify (<10 pg/ml). Lubiprostone is 94% protein-bound in human plasma, rapidly metabolized by carbonyl reductase located in the epithelium of the stomach and jejunum to M3, the only systemically detectable metabolite [Mizumori et al. 2009]. Lubiprostone is not metabolized via the hepatic p450 system. Studies using radiolabeled lubiprostone demonstrate that it is nearly completely eliminated after 48 hours [Soubra and Schey, 2012].
Figure 1.
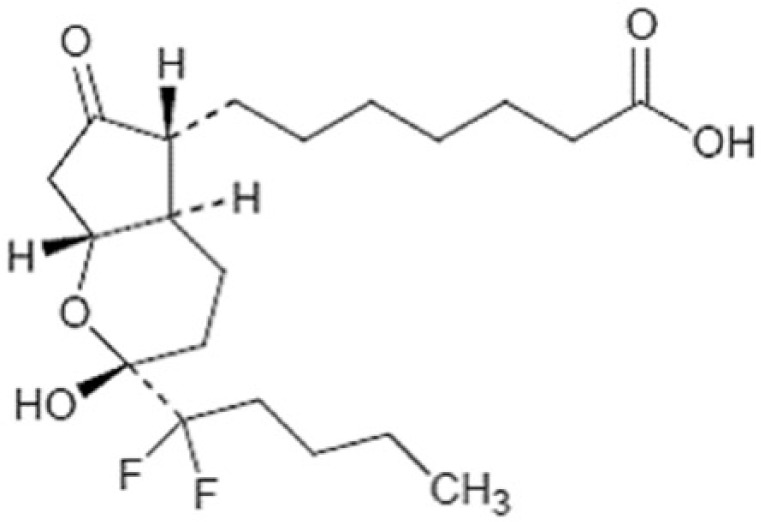
Chemical structure of lubiprostone.
Lubiprostone is classified as a prostone and acts within the GI tract to increase ion and fluid secretion. The primary effect of lubiprostone within the GI tract is controversial. It was initially believed that lubiprostone led to activation of ClC-2 channels on the apical surface of intestinal epithelium, stimulating intraluminal chloride and bicarbonate secretion with resultant passive increase of intraluminal sodium and water [Cuppoletti et al. 2004, 2014]. Studies on murine nasal epithelium demonstrate increased chloride efflux with lubiprostone through both ClC-2 and CFTR ClCs [Schiffhauer et al. 2013]. However, additional data have questioned the cellular function and localization of ClC-2 [Akiba and Kaunitz, 2012]. More recent evidence indicates that ClC-2 channels are localized on the basolateral membranes of the jejunal and colonic epithelium, and are involved primarily in absorption rather than secretion of chloride [Catalan et al. 2012]. Lubiprostone exposure leads to internalization of basolateral ClC-2 into the cytoplasm with concomitant trafficking of CFTR and chloride/hydrogen carbonate exchanger PAT-1 to the apical membrane [Jakab et al. 2012].
There is evidence that lubiprostone stimulates CFTR-dependent chloride secretion both in vivo and in vitro via EP4 receptors and thus increases chloride and water secretion into the lumen [Cuppoletti et al. 2004; Bijvelds et al. 2009; Cuthbert, 2011]. This is supported by research demonstrating no lubiprostone-induced chloride secretion from rectal epithelial cells of mice that are homozygous for the delF508 mutation of CFTR [Bijvelds et al. 2009]. Taken together, these data suggest lubiprostone acts via EP4 receptors to increase intraluminal secretion of chloride by CFTR channels and inhibit chloride and fluid absorption through simultaneous internalization of ClC-2 channels [Akiba and Kaunitz, 2012]. Although chloride ion secretion from lubiprostone appears CFTR-dependent, case series have demonstrated clinical improvement in constipation in cystic fibrosis patients [O’Brien et al. 2010, 2011]. This could be possibly mediated by CFTR-independent means, such as internalization of ClC-2 leading to decreased absorption of intraluminal chloride and water. The increased chloride and fluid secretion in the GI lumen due to lubiprostone leads to increased peristalsis and colonic laxation, with decreased intestinal transit time and quicker passage of stool [Kapoor, 2009].
In addition to its effects on ion and fluid transport in the intestine, lubiprostone also has effects on smooth muscle of the GI tract. Lubiprostone induces a dose-dependent increase in circular muscle contraction in mouse stomach. This response appears to be via EP1 receptors, and the effect is inhibited by pretreatment with an EP1 antagonist. Lubiprostone also causes a dose-dependent increase in basal pyloric sphincter tone [Chan and Mashimo, 2013]. This effect may be responsible for the observation that lubiprostone is associated with increased fasting gastric volume and delayed gastric emptying [Camilleri et al. 2006]. This delayed gastric emptying and increased pyloric tone may contribute to nausea, which is one of the common adverse effects of lubiprostone. However, lubiprostone has no significant effect on postprandial gastric volume or aggregate symptoms; it decreases fullness 30 minutes after a fully satiating meal, and accelerates small intestinal and colonic transit [Camilleri et al. 2006].
Lubiprostone also has prostaglandin-like action within the GI tract, including enhancing intestinal barrier function and preventing acid related injury to the duodenum [Mizumori et al. 2009]. Lubiprostone may be protective against nonsteroidal anti-inflammatory drug (NSAID) induced enteropathy via the EP4-dependent pathway. In rats, administration of lubiprostone significantly reduced indomethacin-induced damage to the small intestine, an effect that was eliminated in the presence of a selective EP4 antagonist [Hayashi et al. 2014]. In a mouse model of cystic fibrosis, administration of lubiprostone increased proximal- and mid-intestinal mucin secretion [De Lisle, 2012]. In ischemia-damaged pig intestine, lubiprostone, but not linaclotide, was effective at protecting and repairing the epithelial cell barrier and cell function after ischemic stress [Cuppoletti et al. 2012]. Compromised barrier function leading to increased permeability and presence of inflammatory cells and cytokines is one of the proposed mechanisms in the pathogenesis of IBS. Lubiprostone has also been an associated with a shift in murine colonic bacterial composition with an increase in Alistipes and Lactobacillus species [Musch et al. 2013]. These findings may allow for further applications of lubiprostone beyond treatment of constipation-related disorders.
Lubiprostone was approved by the FDA for treatment of chronic idiopathic constipation in men and women in 2006 at a dose of 24 µg twice daily. In 2008 it was approved for use in IBS-C in women at a dose of 8 µg twice daily. Recently, the FDA approved lubiprostone for use in opioid-induced constipation in patients with non-cancer pain at a dose of 24 µg twice daily (Table 2). Internationally, lubiprostone has been approved in Japan for treatment of chronic constipation, excluding constipation caused by organic disease, at a dose of 24 µg twice daily. In the UK, the Medicines and Healthcare Products Regulatory Agency approved the use lubiprostone 24 µg twice daily for treatment of chronic idiopathic constipation (CIC) and associated symptoms in adults when response to diet and other non-pharmacological measures is inappropriate. However, lubiprostone approval was denied in the UK for treatment of opioid-induced constipation. Lubiprostone 24 µg twice daily is also approved for treatment of CIC in Switzerland.
Table 2.
Summary of major clinical trials of lubiprostone in irritable bowel syndrome with constipation (IBS-C), chronic constipation, and opioid-induced constipation.
| Study type |
Patients |
Interventions | Key results | ||||
|---|---|---|---|---|---|---|---|
| Design | Duration | n | Age | Female (%) | |||
| Johanson, et al.[2008b] | Two randomized, double-blind, placebo-controlled phase III trials in patients with chronic idiopathic constipation | 4 weeks | 479 | 47.2 | 89.1 | Lubiprostone 24 µg twice daily versus placebo | Significantly higher percentage of patients treated with lubiprostone had a spontaneous bowel movement within 24 hours versus placebo. (56.7% versus 36.9%, 62.9% versus 31.9%). Also significant improvements in straining effort, stool consistency, and global satisfaction with bowel function |
| Barish, et al. [2010] | 242 | ||||||
| 237 | |||||||
| Johanson et al . [2006] | Three open-label, long-term trials | 24–48 weeks | 880 | N/A | N/A | Lubiprostone 24 µg twice daily | Significant and persistent improvement in constipation severity [29% at 24 weeks (n = 512); 28% at 48 weeks (n = 281)], bloating [20% at 48 weeks], abdominal discomfort [17% at 48 weeks] |
| 308 | |||||||
| 248 | |||||||
| 324 | |||||||
| Drossman, et al. [2009] | 2 randomized, double-blind, placebo-controlled trials in pts with IBS-C | 12 weeks | 1,171 | 46.6 | 92% | Lubiprostone 8 µg twice daily versus placebo | Significantly greater percentage of overall responders versus placebo (17.9% versus 10.1%, p = 0.001). Similar incidence of adverse events |
| Cryer, et al. [2014] | Randomized, double-blind, placebo-controlled, multicenter trial for opioid-induced constipation in patients on chronic opioids for non-cancer pain | 12 weeks | 418 | 50.4 | 64.4 | Lubiprostone 24 µg twice daily versus placebo | Significantly higher rates of spontaneous bowel movements (p = 0.004), significant improvement in abdominal discomfort, straining, and constipation severity |
N/A, not applicable. Underlined numbers represent the total numbers of subjects in a trial.
Currently the average wholesale price of a month’s supply of lubiprostone costs is $296.30. This is comparable with the average wholesale price of a month’s supply of linaclotide at $255, though both are significantly more expensive at this time than the bulk, stimulant or osmotic laxatives. To date, no studies have been completed to investigate the cost-effectiveness of treatment with lubiprostone. The cost, and cost-effectiveness, of treatment with lubiprostone will be an important factor in determining therapy as the prevalence of chronic constipating disorders continues to gain recognition worldwide.
Clinical efficacy
CIC
Within the past few years, several studies have established the role of lubiprostone in CIC. A double-blind, placebo-controlled, dose-finding study of lubiprostone in CIC randomized 129 patients who met Rome II criteria for chronic constipation to lubiprostone at doses of 12, 24 or 36 µg twice daily or placebo for 3 weeks and recorded the frequency of spontaneous bowel movements, use of rescue medications, symptoms and adverse events. The primary endpoint was the average daily number of bowel movements. Lubiprostone improved spontaneous bowel movement frequency in a dose-dependent manner and the overall number of bowel movements for all 3 doses of lubiprostone was greater than placebo at week 2. There was no statistically significant difference between the groups in serious and minor adverse events [Johanson and Ueno, 2007]. Based on the results of this study, it was determined that the lubiprostone dose of 24 µg twice daily had the best risk–benefit profile and it was chosen for subsequent phase III studies.
Additional randomized controlled trials with similar study designs have been conducted [Johanson et al. 2008b; Barish et al. 2010]. A total of 479 patients were randomized to receive lubiprostone 24 µg or placebo for 4 weeks after an initial 2 week washout period. The primary endpoint in these studies was frequency of spontaneous bowel movements. In both studies a significantly higher percentage of patients treated with lubiprostone had a spontaneous bowel movement within 24 hours compared with placebo (56.7% versus 36.9%, 62.9% versus 31.9%). There were also significant improvements in straining effort, stool consistency and global satisfaction with bowel function compared with placebo. An abstract recently submitted to the British Society of Gastroenterology reported that lubiprostone improves constipation and related symptoms in patients refractory to other constipation therapies [Panas et al. 2013].
IBS-C
Lubiprostone is currently FDA approved for IBS-C at a dose of 8 µg twice daily based on established clinical trials. A large phase II multicenter study randomized 195 patients who met the Rome III criteria for IBS-C to receive 8, 16 or 24 µg of lubiprostone twice daily or placebo for 3 months. The primary endpoint for the study was a change from baseline in mean abdominal pain/discomfort score in the first month, with secondary endpoints including frequency of spontaneous bowel movements, stool consistency, frequency of straining, and bloating. Although all doses of lubiprostone had absolute improvement in the primary endpoint of pain scores at 3 months, there was no statistically significant difference over placebo. Similarly, all doses of lubiprostone were associated with nonsignificant differences over placebo in secondary endpoints including reduced straining and bloating, increased stool frequency, improved stool consistency, and decreased severity of constipation. Among the dosages, the 24 µg dose had the greatest improvement in symptoms but also conferred the greatest incidence of side effects, primarily nausea and vomiting [Johanson et al. 2008a]. The authors determined that 8 µg twice daily offered the best risk-benefit profile for patients with IBS-C.
Another phase II, multicenter, double-blind, placebo-controlled dose-finding study randomized 170 patients in Japan who met the Rome III criteria for chronic idiopathic constipation, with or without IBS-C, to lubiprostone at doses of 8, 16 or 24 µg twice daily or placebo for 2 weeks. The primary endpoint was a changeover baseline in weekly average spontaneous bowel movements at one week, with a secondary endpoint of change over baseline at week 2. All doses of lubiprostone showed a dose-dependent increase in the frequency of spontaneous bowel movements compared with placebo in both weeks. The subgroup of patients with IBS-C showed the greatest increase in spontaneous bowel movement frequency with the 24 µg twice daily dose, but this dose was also associated with the greatest number of side effects [Fukudo et al. 2011]. Although neither phase II study of lubiprostone in IBS-C was gender-specific, 91% of the enrolled subjects in these trials were female. As a result, the clinical efficacy of lubiprostone in males with IBS-C was unable to be conclusively demonstrated based on the available data.
An analysis of two phase III, randomized trials comparing lubiprostone 8 µg twice daily versus placebo for 12 weeks included 1,171 patients who met Rome II criteria for IBS-C. Study subjects recorded their symptoms in an electronic diary. The primary endpoint for this study was the percentage of subjects whose symptoms were at least moderately relieved for all 4 weeks in a month, or significantly relieved for 2 weeks in a month. A patient was considered an ‘overall responder’ if they were monthly responders for at least 2 of the 3 months. The lubiprostone arm had a significantly greater percentage of overall responders compared with placebo (17.9% versus 10.1%, p = 0.001). The incidence of adverse events was similar between the two groups [Drossman et al. 2009]. Furthermore, a subsequent analysis of these two studies demonstrated a significant improvement in quality of life (QOL) amongst the lubiprostone-treated group based on an IBS-QOL questionnaire. Specifically subjects noted improvement within the domains of social reaction, food avoidance, health worry, body image and dysphoria.
Opioid-induced constipation
In a prospective, randomized, double-blind, placebo-controlled multicenter clinical trial patients with opioid-related constipation who take opioids for chronic noncancer pain were randomized to receive lubiprostone 24 µg twice daily versus placebo. Subjects who received lubiprostone had significantly higher rates of spontaneous bowel movements and significant improvement in abdominal discomfort, straining and constipation severity compared with placebo [Cryer et al. 2014]. Based on this study lubiprostone is considered well tolerated and effective in treatment in chronic opioid-induced constipation for patients taking opioids for noncancer pain. It was approved for this indication by the FDA in April 2013 at a dose of 24 µg twice daily, as the first medication approved for opioid-induced constipation in adults taking opioids for non-cancer pain. Studies on guinea pig, mouse and human small intestine tissue have shown that morphine inhibits chloride currents, but this inhibition was reversed with the addition of lubiprostone [Fei et al. 2010; Sun et al. 2011]. The efficacy of lubiprostone has not been established for patients taking diphenylheptane opioids (e.g. methadone). In a subgroup analysis of a clinical trial, methadone appeared to prevent the beneficial effects of lubiprostone [Wong and Camerilli, 2011]. In vitro studies using human colonic epithelial cell lines found that methadone, but not morphine, inhibited lubiprostone-stimulated chloride currents through ClC-2 channels [Cuppoletti et al. 2013]. Of note, the FDA has also recently granted approval to methylnaltrexone, a µ-opioid antagonist, and naloxegol, a peripherally acting opioid antagonist, for the treatment of opioid-induced constipation.
In addition to its current FDA-approved indications, use of lubiprostone has been reported in clozapine-induced constipation. Clozapine, a potent atypical antipsychotic, is typically reserved for patients with severe schizophrenia in whom there is often no effective alternative. Clozapine is associated with constipation in up to 60% of patients, rarely causing ileus, perforation and death. In some instances constipation may necessitate discontinuation of clozapine therapy. Institutional experience has shown lubiprostone to be a safe and effective adjunct in patients who have clozapine-associated constipation who may have few other antipsychotic medication options [Meyer and Cummings, 2014].
Safety and tolerability
The safety and efficacy of lubiprostone has been evaluated in multiple studies. A safety and tolerability study administered lubiprostone to 26 healthy volunteers for 7 days. Study subjects received 72, 90 or 108 µg of lubiprostone divided into 3 daily doses. There were no serious adverse events, and the most common reported adverse events were vomiting, nausea, and abdominal cramping [Ueno 2005].
In a study by Chey and colleagues, 522 patients with IBS-C who had participated in 1 of 2 randomized phase III trials were enrolled in an open-label extension study of lubiprostone 8 µg twice daily for 36 weeks to evaluate long-term safety and tolerability. There were no significant changes in vital signs of laboratory values during the study and no serious adverse events. The most common adverse events were diarrhea (11%), nausea (11%), urinary tract infection (9%), sinusitis (9%) and abdominal distension (5.8%). A total of 21 patients out of the 522 subjects (4%) discontinued the drug due to adverse events, while 41 subjects (7.9%) decreased their dose due to adverse events. Diarrhea and nausea were the most common adverse events that led to stopping the medication. In subjects who developed diarrhea as a result of lubiprostone, the diarrhea was mild to moderate in severity with no changes in serum electrolytes or electrocardiography. Based on these results, the extended use of lubiprostone at 8 µg twice daily for IBS-C was found to be safe and well tolerated [Chey et al. 2012a]. These results are similar to adverse event profiles in prior studies, including phase II and phase III clinical trials of lubiprostone for IBS-C, in which the most commonly reported adverse events were nausea (8%), diarrhea (7%) and abdominal pain (5%) [Johanson et al. 2008a].
Studies of lubiprostone 24 µg twice daily for 4 weeks compared with placebo in CIC have shown similar safety profiles. There were no serious adverse events, including no significant changes in vital signs, laboratory values or physical examination findings. The most common adverse events were nausea (21%), abdominal pain (6.7%) and dyspnea (3.4%). Treatment was discontinued in the study by 15 patients receiving lubiprostone (12.6%) and 1 receiving placebo (0.8%), with the most common adverse events amongst those who discontinued therapy being nausea and abdominal pain [Barish et al. 2010]. A multicenter, open-labeled trial evaluated the long-term safety of patients taking lubiprostone at 24 µg twice daily for chronic constipation and found the most common adverse effects were nausea (19.8%), diarrhea (9.7%), abdominal distension (6.9%), headache (6.9%) and abdominal pain (5.2%). Overall long-term therapy with lubiprostone was considered well tolerated [Lembo et al. 2011].
Nausea is the most commonly reported adverse event related to lubiprostone. Nausea is generally mild to moderate in severity and is dose dependent, with up to 17% of patients taking 24 µg twice daily reporting nausea. The mechanism causing nausea in lubiprostone is unclear, though it may be related to decreased circular smooth muscle contraction, increased pyloric sphincter tone, or distension of the small bowel as a result of increased fluid secretion in the gut. It is recommended to take lubiprostone with food to mitigate the symptoms of nausea.
Dyspnea is an uncommon side effect of lubiprostone, with reported rates of 2.5% in patients treated for CIC and 0.4% in patients treated for IBS-C. Patients experiencing dyspnea subjectively describe chest tightness and difficulty breathing. In affected patients, dyspnea typically occurs within an hour of the first dose, lasts a few hours, and generally recurs with repeated dosing. The reported incidences have been self- limited and not considered a serious adverse event [FDA, 2008]. The exact mechanism for lubiprostone-induced dyspnea is not known, although in vitro experiments using respiratory epithelium with topically applied lubiprostone increased chloride secretion [Bao et al. 2008]. It is recommended that patients experiencing dyspnea should discontinue lubiprostone. Recently, a case report described a patient who developed ischemic colitis related to taking the 24 µg dose of lubiprostone [Sherid et al. 2013].
There is no dose adjustment of lubiprostone required with renal impairment. For patients with hepatic impairment, the FDA recommends no dose adjustment for patients with Childs–Pugh class A. Those with Childs–Pugh class B or moderate hepatic impairment should receive a maximum dose of 16 µg twice daily, and those with Childs–Pugh class C or severe hepatic impairment should receive a maximum of 8 µg twice daily [Sucampo, Takeda]. There are no drug–drug interactions described to date.
Pregnancy and lactation
Lubiprostone is classified as pregnancy category C, meaning studies of animal reproduction have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans. It is recommended that any woman of child-bearing age have a negative pregnancy test prior to initiating therapy and be capable of complying to an effective contraceptive regimen. Use of lubiprostone during pregnancy can be justified only if the benefits outweigh the potential risks to the fetus [Barish et al. 2010]. Table 3 lists the approved indications and dosages. It is unknown whether lubiprostone is excreted in breast milk.
Table 3.
Approved indications and dosages of lubiprostone.
| Indication | Dose (by mouth) | Gender | Pregnancy category |
|---|---|---|---|
| Chronic idiopathic constipation | 24 µg twice daily | Male and female | C |
| Irritable bowel syndrome with constipation | 8 µg twice daily | Female | C |
| Opioid-induced constipation | 24 µg twice daily | Male and Female | C |
Conclusion
Constipation affects a large percentage of the Western population, with CIC and IBS-C being the main cause and associated with decreased quality of life and significant morbidity. CIC and IBS-C commonly overlap and the first-line therapy in treatment of these patients often includes lifestyle modification and OTC laxatives. However, these measures may not always be effective in relieving symptoms for long-term treatment of constipation, often leading to frustration for both patients and healthcare providers.
Novel therapies for the treatment of chronic constipation have emerged as effective alternatives for patients with CIC and IBS-C. Currently the only drugs in this category approved by the FDA are lubiprostone and linaclotide. Lubiprostone is an orally acting agent which selectively activates ClC-2 and causes increased fluid secretion. In multiple controlled trials lubiprostone has proven safe and effective for the treatment of men and women with CIC, as well as women with IBS-C, and opioid-induced constipation. Linaclotide is a GC-C receptor agonist also approved for use in IBS-C and CIC. These drugs operate via different mechanisms, but both have been shown to be effective, have a favorable safety profile and similar cost. In addition to its effect on constipation, linaclotide also affects visceral afferent neurons, reducing nociception. Prucalopride, a novel 5-HT4 receptor agonist developed for treatment of chronic constipation, is approved for use in Europe and Canada, but has not been approved by the FDA due to relatively low efficacy, and caution surrounding safety and tolerability given the cardiac toxicities observed with other 5-HT4 agonists such as tegaserod, which was withdrawn by the FDA in 2007 due to concerns for increased adverse cardiovascular events. Although these novel agents have all been shown to be superior to placebo, to date there have been no head to head studies comparing the relative efficacy of these newer agents.
Trials extending up to 13 months have demonstrated that lubiprostone is well tolerated with long-term use, with no serious adverse events reported. At this time there are insufficient data on its efficacy in men with IBS. Lubiprostone is also approved for opioid-induced constipation in patients on chronic opioid medications for chronic noncancer pain. Recent animal studies have shown that lubiprostone has certain prostaglandin-like effects within the bowel, and may improve intestinal barrier function and help resist epithelial injury, which may further expand its range of clinical applications in the future. The most common side effects in patients taking lubiprostone were mild to moderate nausea and diarrhea. It is recommended that women of childbearing age should have a negative pregnancy test prior to initiating lubiprostone and should comply with effective contraceptive measures while taking lubiprostone.
Overall lubiprostone is an effective and well tolerated option for patients who require long-term treatment of constipation.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare no conflict of interest in preparing this article.
Contributor Information
Nicholas Wilson, Section of Gastroenterology, Department of Medicine, Temple University School of Medicine, Philadelphia, PA, USA.
Ron Schey, Neurogastroenterology & Esophageal Disorders Program, Temple University Physicians/Section of Gastroenterology, 3401 N Broad Street, Philadelphia, PA 19140, USA.
References
- Akiba Y., Kaunitz J. (2012) May the truth be with you: lubiprostone as Ep receptor agonist/Clc-2 internalizing ‘inhibitor’. Dig Dis Sci 57: 2740–2742. [DOI] [PubMed] [Google Scholar]
- Bao H., Liu L., Self J., Duke B., Ueno R., Eaton D. (2008) A synthetic prostone activates apical chloride channels in A6 epithelial cells. Am J Physiol Gastrointest Liver Physiol 295: G234–G251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barish C., Drossman D., Johanson J., Ueno R. (2010) Efficacy and safety of lubiprostone in patients with chronic constipation. Dig Dis Sci 55: 1090–1097. [DOI] [PubMed] [Google Scholar]
- Bijvelds M., Bot A., Escher J., De Jonge H. (2009) Activation of intestinal Cl- secretion by lubiprostone requires the cystic fibrosis transmembrane conductance regulator. Gastroenterology 137: 976–985. [DOI] [PubMed] [Google Scholar]
- Bosshard W., Dreher R., Schnegg J., Bula C. (2004) The treatment of chronic constipation in elderly people: an update. Drugs Aging 21: 911–930. [DOI] [PubMed] [Google Scholar]
- Camilleri M., Bharucha A., Ueno R., Burton D., Thomforde G., Baxter K., et al. (2006) Effect of a selective chloride channel activator, lubiprostone, on gastrointestinal transit, gastric sensory, and motor functions in healthy volunteers. Am J Physiol Gastrointest Liver Physiol 290: G942–G947. [DOI] [PubMed] [Google Scholar]
- Camilleri M., Van Outryve M., Beyens G., Kerstens R., Robinson P., Vandeplassche L. (2010) Clinical trial: the efficacy of open-label prucalopride treatment in patients with chronic constipation - follow-up of patients from the pivotal studies. Aliment Pharmacol Ther 32: 1113–1123. [DOI] [PubMed] [Google Scholar]
- Catalan M., Flores C., Gonzalez-Begne M., Zhang Y., Sepulveda F., Melvin J. (2012) Severe defects in absorptive ion transport in distal colons of mice that lack Clc-2 channels. Gastroenterology 142: 346–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan W., Mashimo H. (2013) Lubiprostone increases small intestinal smooth muscle contractions through a prostaglandin E Receptor 1 (Ep1)-mediated pathway. J Neurogastroenterol Motility 19: 312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman R., Sillery J., Fontana D., Matthys C., Saunders D. (1985) Effect of oral dioctyl sodium sulfosuccinate on intake-output studies of human small and large intestine. Gastroenterology 89: 489–493. [DOI] [PubMed] [Google Scholar]
- Chey W., Drossman D., Johanson J., Scott C., Panas R., Ueno R. (2012a) Safety and patient outcomes with lubiprostone for up to 52 weeks in patients with irritable bowel syndrome with constipation. Aliment Pharmacol Ther 35: 587–599. [DOI] [PubMed] [Google Scholar]
- Chey W., Lembo A., Lavins B., Shiff S., Kurtz C., Currie M., et al. (2012b) Linaclotide for irritable bowel syndrome with constipation: a 26-week, randomized, double-blind, placebo-controlled trial to evaluate efficacy and safety. Am J Gastroenterol 107: 1702–1712. [DOI] [PubMed] [Google Scholar]
- Cryer B., Katz S., Vallejo R., Popescu A., Ueno R. (2014) A randomized study of lubiprostone for opioid-induced constipation in patients with chronic noncancer pain. Pain Med 15: 1825–1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuppoletti J., Blikslager A., Chakrabarti J., Nighot P., Malinowska D. (2012) Contrasting effects of linaclotide and lubiprostone on restitution of epithelial cell barrier properties and cellular homeostasis after exposure to cell stressors. BMC Pharmacol 12: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuppoletti J., Chakrabarti J., Tewari K., Malinowska D. (2013) Methadone but not morphine inhibits lubiprostone-stimulated Cl- currents in T84 intestinal cells and recombinant human Clc-2, but Not Cftr Cl- currents. Cell Biochem Biophys 66: 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuppoletti J., Chakrabarti J., Tewari K., Malinowska D. (2014) Differentiation between human Clc-2 and Cftr Cl- channels with pharmacological agents. Am J Physiol Cell Physiol 307: C479–C492. [DOI] [PubMed] [Google Scholar]
- Cuppoletti J., Malinowska D., Tewari K., Li Q.J., Sherry A., Patchen M., et al. (2004) Spi-0211 activates T84 cell chloride transport and recombinant human Clc-2 chloride currents. Am J Physiol Cell Physiol 287: C1173–C1183. [DOI] [PubMed] [Google Scholar]
- Cuthbert A. (2011) Lubiprostone targets prostanoid Ep(4) receptors in ovine airways. Br J Pharmacol 162: 508–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Lisle R. (2012) Lubiprostone stimulates small intestinal mucin release. BMC Gastroenterol 12: 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drossman D., Chey W., Johanson J., Fass R., Scott C., Panas R., et al. (2009) Clinical trial: lubiprostone in patients with constipation-associated irritable bowel syndrome–results of two randomized, placebo-controlled studies. Aliment Pharmacol Ther 29: 329–341. [DOI] [PubMed] [Google Scholar]
- Drossman D., Li Z., Andruzzi E., Temple R., Talley N., Thompson W., et al. (1993) U.S. householder survey of functional gastrointestinal disorders. prevalence, sociodemography, and health impact. Dig Dis Sci 38: 1569–1580. [DOI] [PubMed] [Google Scholar]
- Everhart J., Go V., Johannes R., Fitzsimmons S., Roth H., White L. (1989) A longitudinal survey of self-reported bowel habits in the United States. Dig Dis Sci 34: 1153–1162. [DOI] [PubMed] [Google Scholar]
- FDA Center for Drug Evaluation and Research (CDER) (2008) April. [Google Scholar]
- Fei G., Raehal K., Liu S., Qu M., Sun X., Wang G., et al. (2010) Lubiprostone reverses the inhibitory action of morphine on intestinal secretion in guinea pig and mouse. J Pharmacol Exp Ther 334: 333–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine P., Mahajan G., Mcpherson M. (2009) Long-acting opioids and short-acting opioids: appropriate use in chronic pain management. Pain Med 10(Suppl. 2): S79–S88. [DOI] [PubMed] [Google Scholar]
- Fukudo S., Hongo M., Kaneko H., Ueno R. (2011) Efficacy and safety of oral lubiprostone in constipated patients with or without irritable bowel syndrome: a randomized, placebo-controlled and dose-finding study. Neurogastroenterol Motility 23: 544–e205. [DOI] [PubMed] [Google Scholar]
- Hayashi S., Kurata N., Yamaguchi A., Amagase K., Takeuchi K. (2014) Lubiprostone prevents nonsteroidal anti-inflammatory drug-induced small intestinal damage by suppressing the expression of inflammatory mediators Via Ep4 receptors. J Pharmacol Exp Ther 349: 470–479. [DOI] [PubMed] [Google Scholar]
- Higgins P., Johanson J. (2004) Epidemiology of Constipation in North America: A systematic review. Am J Gastroenterol 99: 750–759. [DOI] [PubMed] [Google Scholar]
- Husain N., Chaudhry I., Jafri F., Niaz S., Tomenson B., Creed F. (2008) A population-based study of irritable bowel syndrome in a non-western population. Neurogastroenterol Motility 20: 1022–1029. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (2011) Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: National Academies Press. [PubMed] [Google Scholar]
- Jakab R., Collaco A., Ameen N. (2012) Lubiprostone targets prostanoid signaling and promotes ion transporter trafficking, mucus exocytosis, and contractility. Dig Dis Sci 57: 2826–2845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jentsch T. (2008) Clc chloride channels and transporters: from genes to protein structure, pathology and physiology. Crit Rev Biochem Mol Biol 43: 3–36. [DOI] [PubMed] [Google Scholar]
- Johanson J., Drossman D., Panas R., Wahle A., Ueno R. (2008a) Clinical trial: phase 2 study of lubiprostone for irritable bowel syndrome with constipation. Aliment Pharmacol Ther 27: 685–696. [DOI] [PubMed] [Google Scholar]
- Johanson J., Kralstein J. (2007) Chronic constipation: a survey of the patient perspective. Aliment Pharmacol Ther 25: 599–608. [DOI] [PubMed] [Google Scholar]
- Johanson J., Morton D., Geenen J., Ueno R. (2008b) Multicenter, 4-week, double-blind, randomized, placebo-controlled trial of lubiprostone, a locally-acting type-2 chloride channel activator, in patients with chronic constipation. Am J Gastroenterol 103: 170–177. [DOI] [PubMed] [Google Scholar]
- Johanson J., Ueno R. (2007) Lubiprostone, a locally acting chloride channel activator, in adult patients with chronic constipation: a double-blind, placebo-controlled, dose-ranging study to evaluate efficacy and safety. Aliment Pharmacol Ther 25: 1351–1361. [DOI] [PubMed] [Google Scholar]
- Johanson J., Panas R., Holland P., Ueno R. (2006) Long-term efficacy of lubiprostone for the treatment of chronic constipation. Gastroenterology 130: A317. [Google Scholar]
- Jones M., Talley N., Nuyts G., Dubois D. (2002) Lack of objective evidence of efficacy of laxatives in chronic constipation. Dig Dis Sci 47: 2222–2230. [DOI] [PubMed] [Google Scholar]
- Kalso E., Edwards J., Moore R., Mcquay H. (2004) Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain 112: 372–380. [DOI] [PubMed] [Google Scholar]
- Kapoor S. (2009) Lubiprostone: clinical applications beyond constipation. World J Gastroenterol 15: 1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoshkrood-Mansoori B., Pourhoseingholi M., Safaee A., Moghimi-Dehkordi B., Sedigh-Tonekaboni B., Pourhoseingholi A., et al. (2009) Irritable bowel syndrome: a population based study. J Gastrointest Liver Dis 18: 413–418. [PubMed] [Google Scholar]
- Lembo A., Johanson J., Parkman H., Rao S., Miner P., Jr., Ueno R. (2011) Long-term safety and effectiveness of lubiprostone, a chloride channel (Clc-2) activator, in patients with chronic idiopathic constipation. Dig Dis Sci 56: 2639–2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy R., Von Korff M., Whitehead W., Stang P., Saunders K., Jhingran P., et al. (2001) Costs of care for irritable bowel syndrome patients in a health maintenance organization. Am J Gastroenterol 96: 3122–3129. [DOI] [PubMed] [Google Scholar]
- Lipecka J., Bali M., Thomas A., Fanen P., Edelman A., Fritsch J. (2002) Distribution of Clc-2 chloride channel in rat and human epithelial tissues. Am J Physiol Cell Physiol 282: C805–C816. [DOI] [PubMed] [Google Scholar]
- Longstreth G., Thompson W., Chey W., Houghton L., Mearin F., Spiller R. (2006) Functional bowel disorders. Gastroenterology 130: 1480–1491. [DOI] [PubMed] [Google Scholar]
- Meyer J., Cummings M. (2014) Lubiprostone for treatment-resistant constipation associated with clozapine use. Acta Psychiatr Scand 130: 71–72. [DOI] [PubMed] [Google Scholar]
- Mizumori M., Akiba Y., Kaunitz J. (2009) Lubiprostone stimulates duodenal bicarbonate secretion in rats. Dig Dis Sci 54: 2063–2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musch M., Wang Y., Claud E., Chang E. (2013) Lubiprostone decreases mouse colonic inner mucus layer thickness and alters intestinal microbiota. Dig Dis Sci 58: 668–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien C., Anderson P., Stowe C. (2010) Use of the chloride channel activator lubiprostone for constipation in adults with cystic fibrosis: a case series. Ann Pharmacother 44: 577–581. [DOI] [PubMed] [Google Scholar]
- O’Brien C., Anderson P., Stowe C. (2011) Lubiprostone for constipation in adults with cystic fibrosis: a pilot study. Ann Pharmacother 45: 1061–1066. [DOI] [PubMed] [Google Scholar]
- Panas R., Joswick T., Lichtlen P., Panigrahi D., Ueno R. (2013) Lubiprostone Treatment Improves Constipation and Related Symptoms in Patients Refractory to other Constipation Therapies. Gut 62: A291. [Google Scholar]
- Pare P., Ferrazzi S., Thompson W., Irvine E., Rance L. (2001) An epidemiological survey of constipation in canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol 96: 3130–3137. [DOI] [PubMed] [Google Scholar]
- Rao S., Lembo A., Shiff S., Lavins B., Currie M., Jia X., et al. (2012) A 12-week, randomized, controlled trial with a 4-week randomized withdrawal period to evaluate the efficacy and safety of linaclotide in irritable bowel syndrome with constipation. Am J Gastroenterol 107: 1714–1724; quiz p 1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito Y., Schoenfeld P., Locke G., 3rd (2002) The epidemiology of irritable bowel syndrome in North America: a systematic review. Am Jf Gastroenterol 97: 1910–1915. [DOI] [PubMed] [Google Scholar]
- Sandler R., Everhart J., Donowitz M., Adams E., Cronin K., Goodman C., et al. (2002) The burden of selected digestive diseases in the United States. Gastroenterology 122: 1500–1511. [DOI] [PubMed] [Google Scholar]
- Schiffhauer E., Vij N., Kovbasnjuk O., Kang P., Walker D., Lee S., et al. (2013) Dual activation of cftr and clcn2 by lubiprostone in murine nasal epithelia. Am J Physio Lung Cell Mol Physiol 304: L324–L331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherid M., Sifuentes H., Samo S., Deepak P., Sridhar S. (2013) Lubiprostone induced ischemic colitis. World J Gastroenterol 19: 299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soubra M., Schey R. (2012) Lubiprostone for the treatment of adult women with irritable bowel syndrome with constipation. Clin Med Insights Gastroenterol 5: 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart W., Liberman J., Sandler R., Woods M., Stemhagen A., Chee E., et al. (1999) Epidemiology of constipation (Epoc) study in the United States: relation of clinical subtypes to sociodemographic features. Am J Gastroenterol 94: 3530–3540. [DOI] [PubMed] [Google Scholar]
- Sun X., Wang X., Wang G., Xia Y., Liu S., Qu M., et al. (2011) Lubiprostone reverses the inhibitory action of morphine on mucosal secretion in human small intestine. Dig Dis Sci 56: 330–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan Y., Goh K., Muhidayah R., Ooi C., Salem O. (2003) Prevalence of irritable bowel syndrome in young adult malaysians: a survey among medical students. Journal of Gastroenterology and Hepatology 18: 1412–1416. [DOI] [PubMed] [Google Scholar]
- Tuteja A., Talley N., Joos S., Woehl J., Hickam D. (2005) Is constipation associated with decreased physical activity in normally active subjects? Am J Gastroenterol 100: 124–129. [DOI] [PubMed] [Google Scholar]
- Ueno R. (2005) Multiple, escalating, oral-dose study to assess the safety, tolerance and pharmacodynamic profile of lubiprostone in normal health volunteers. Neurogastroenterol Motil 17: A78. [Google Scholar]
- Wong B., Camilleri M. (2011) Lubiprostone for the treatment of opioid-induced bowel dysfunction. Expert Opin Pharmacother 12: 983–990. [DOI] [PubMed] [Google Scholar]
- Young R., Beerman L., Vanderhoof J. (1998) Increasing oral fluids in chronic constipation in children. Gastroenterol Nursing 21: 156–161. [DOI] [PubMed] [Google Scholar]


