Abstract
Background: Cardiovascular disease (CVD) screening in Title X settings can identify low-income women at risk of future chronic disease. This study examines follow-up related to newly identified CVD risk factors in a Title X setting.
Methods: Female patients at a North Carolina Title X clinic were screened for CVD risk factors (n=462) and 167/462 (36.1%) were rescreened one year later. Clinical staff made protocol-driven referrals for women identified with newly diagnosed CVD risk factors. We used paired t-tests and chi square tests to compare screening and rescreening results (two-tailed, p<0.05).
Results: Among 11 women in need of referrals for newly diagnosed hypertension or diabetes, 9 out of 11 (81.8%) were referred, and 2 of 11 (18.2%) completed referrals. Among hypertensive women who were rescreened (n=21), systolic blood pressure decreased (139 to 132 mmHg, p=0.001) and diastolic blood pressure decreased (90 to 83 mmHg, p=0.006). Hemoglobin A1c did not improve among rescreened diabetic women (n=5, p=0.640). Among women who reported smoking at enrollment, 129 of 148 (87.2%) received cessation counseling and 8 of 148 (5.4%) accepted tobacco quitline referrals. Among smokers, 53 out of 148 (35.8%) were rescreened and 11 of 53 (20.8%) reported nonsmoking at that time. Among 188 women identified as obese at enrollment, 22 (11.7%) scheduled nutrition appointments, but only one attended. Mean weight increased from 221 to 225 pounds (p 0<.05) among 70 out of 188 (37.2%) obese women who were rescreened.
Conclusions: The majority of women in need of referrals for CVD risk factors received them. Few women completed referrals. Future research should examine barriers and facilitators of referral care among low-income women.
Introduction
Low-income women of reproductive age have greater rates of cardiovascular disease (CVD) risk factors compared with their higher income counterparts.1 A study published by the current authors demonstrated that many low-income women accessing reproductive health services at a North Carolina health department Title X family planning clinic had CVD precursors (pre-hypertension, borderline high cholesterol, or prediabetes) or risk factors (smoking or obesity).2 Optimizing low-income women's health during reproductive years may impact their long-term health and may also prevent adverse pregnancy outcomes such as low birth weight, preterm deliveries, and birth defects.3
Title X is a federal program that provides subsidized contraceptive services for more than five million low-income patients annually, and health departments are major providers of Title X services.4 Most women who receive family planning services through Title X report that their family planning provider is also their usual source of health care.2,5 Because Title X clinics routinely screen for CVD risk factors, such as hypertension, smoking and obesity, these clinics frequently identify CVD risk factors among low-income women.
Title X clinics are expected to refer women for conditions identified during family planning visits that require medical care, but for which the clinics may lack resources to treat, such as hypertension. While making referrals are a requirement of Title X funding, only a few studies have examined referral patterns in family planning clinic settings.6,7 One study found that providers in those settings were more likely to refer women testing positive for human immunodeficiency virus when providers were aware of local available referral resources.6 Another study reported family planning patients were more likely to seek follow-up care for abnormal Papanicolaou (Pap) tests if they were told by their provider where to obtain the follow-up care.7
To our knowledge, no published studies have documented referral practices related to management of CVD risk factors identified in Title X settings. This study examines the outcomes of referrals for CVD risk factors (hypertension, diabetes, smoking, and obesity) among nonpregnant women receiving family planning services at a Title X clinic in North Carolina, and examines whether CVD risk factors improved one year later among women who screened positive.
Materials and Methods
Overview
The research design and methods of the Integrated Screening and Health Assessment, Prevention and Evaluation (InShape) Study have been described elsewhere.2 Participants were enrolled and offered screening for CVD risk factors at an initial or annual family planning visit at a Title X family planning clinic in Pitt County, North Carolina. A research assistant obtained written informed consent from participants that included permission to request medical records related to referrals. Upon enrollment, participants were also informed that they would have the opportunity to be rescreened for CVD risk factors when they returned for their next annual family planning visit. At the screening visit, clinical staff made referrals and offered follow-up care for women with screening values requiring medical management according to clinic protocols. At the subsequent annual family planning visit, participants were rescreened for CVD risk factors and completed a self-administered questionnaire that included questions about health practices and health history.
Sample
Women eligible for the screening study were nonpregnant, English speaking, ages 18–44 years, and attending the Pitt County family planning clinic for an initial or annual reproductive health exam between May 23, 2011, and February 28, 2012. Among eligible women, 54% (462/859) enrolled and participated in the screening. Eligibility criteria for InShape rescreening at the subsequent annual visit were participation in the initial screening and being nonpregnant when they returned for their subsequent annual visit, which occurred at least 12 months after the screening visit. If a participant did not return within 13 months for the annual visit, research staff called and mailed letters to remind her about the opportunity to be rescreened. The Institutional Review Board of the University of North Carolina, Chapel Hill approved and monitored this study.
Measurement
We describe outcomes of referrals among the women who were newly identified with hypertension or diabetes at enrollment and report results from the InShape rescreening, which involved the same screening measures that were previously reported.2 In accordance with the health department protocol for usual clinical care, blood pressure (BP) was assessed with a single nurse-administered measurement using automated equipment. Blood samples were obtained for hemoglobin A1c assessment and sent to a commercial laboratory (LabCorp). Tobacco use and demographic characteristics were obtained from the self-administered questionnaire. Obesity (body mass index [BMI] ≥30kg/m2) was determined by clinical measurement of weight (kilograms) and height (meters).
Criteria for referrals
According to the health department's existing protocol, which was adapted from the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure,8 the threshold for hypertension referral was systolic or diastolic BP ≥160/95 mmHg.
The newly developed clinic protocol for elevated blood glucose recommended that all women with A1c levels ≥6.5% be referred to the health department's diabetes self-management program for further evaluation. Women with screening A1c values 6.5%–7.5% had to have a repeat A1c three months later that was ≥6.5% before an external referral was indicated. All women with screening A1c values >7.5% met criteria for external referrals.
An existing clinic protocol required that the clinic nurse provide five A's counseling (Ask, Advise, Assess, Assist, Arrange) on smoking cessation9and information about the tobacco quitline to patients who smoke. Patients who smoke were also offered help from a trained smoking cessation counselor and if accepted, a referral form was faxed to the tobacco quitline.
An existing clinic protocol for obesity screening and referral was revised to add referral options available through the InShape program. All obese patients were invited to participate in either the InShape lifestyle intervention for nutritional education and promotion of physical activity or the weight loss program. Obese patients with BMI ≥40 kg/m2 or a BMI ≥35 kg/m2 plus comorbidities (i.e., hypertension, diabetes, elevated lipids) also had the option of a referral to medical nutrition therapy services provided by the Pitt County Health Department.
Referral process
Family planning clinic staff received training on the newly developed protocol for A1c screening. When family planning clinic staff identified participants who met referral criteria, designated health department staff arranged formal referrals by phone and informed participants of their referral appointments. The health department provided information on formal referrals to research staff, including indication for referral, date referral was made, and the medical practice receiving the referral (i.e., referral resource). Clinicians also made informal referrals, which we define as verbal referrals that were documented in the medical record (i.e., “patient told to follow-up with…”), but not arranged by the health department staff. Research staff (TK, CR, SF) reviewed the medical charts of all participants with indicated referrals to verify formal and informal referrals. For both formal and informal referrals, research staff requested medical records from referral resources for the 12-month time period after the date of the screening visit.
Analytic plan
To compare participants who received rescreening with those who did not, we examined differences in distributions of demographic characteristics and CVD risk factors from the enrollment visit using Fisher's exact tests. We calculated percent of women who received referrals and the percent of women who completed referrals. To examine changes in CVD risk factors over time, we compared the mean values of BP and A1c from enrollment and the subsequent annual visit among women with abnormal levels, respectively. We report the mean differences and 95% confidence intervals (CIs) for those values. Similarly, we compared mean values of weight from enrollment and the subsequent annual visit among obese women and we assessed change in smoking status among smokers who were rescreened using chi square tests. For sensitivity analyses, we repeated comparison analyses of those same measures using the full sample of women who returned for the subsequent annual visit. All reported significance tests and 95% CIs are two-tailed (p<0.05). Analyses were conducted with Stata v.13 (StataCorp LP, 2013).
Results
Among the 462 women who were screened at enrollment, a total of 167 (36.2%) were rescreened at their subsequent annual visit between 12 and 22 months (median=13) after study enrollment. Loss rates include 48 (10.4%) women who became pregnant and were ineligible for screening at the subsequent annual visit, 13 (2.8%) who declined participation, 32 (6.9%) who visited the family planning clinic 12–22 months after screening, but were missed by research staff and were not offered rescreening, and 202 (43.7%) who did not return for an annual visit within the study period. No statistically significant differences on baseline demographics or CVD risk factors were found between 167 women who were rescreened and 295 who were not (Table 1).
Table 1.
Characteristics of Female InShape Screening Study Participants Stratified by Rescreen Status, North Carolina
| Screened 2011–2012 (N=462) | Rescreened 2012–2013 (N=167) | Not rescreened 2012–2013 (N=295) | |||||
|---|---|---|---|---|---|---|---|
| Variables | n | % | n | % | n | % | p valuea |
| Baseline visit demographics | |||||||
| Age (years), mean (SE) | 26.4 (0.3) | 26.9 (0.5) | 26.1 (0.4) | 0.704 | |||
| 18–24 | 249 | 53.9 | 87 | 52.1 | 162 | 54.9 | |
| 25–29 | 97 | 21.0 | 33 | 19.8 | 64 | 21.7 | |
| 30–34 | 61 | 13.2 | 24 | 14.4 | 37 | 12.5 | |
| 35–44 | 55 | 11.9 | 23 | 13.8 | 32 | 10.9 | |
| Race/ethnicity | 0.175 | ||||||
| White, non-Hispanic | 126 | 27.3 | 54 | 32.3 | 72 | 24.4 | |
| Black, non-Hispanic | 291 | 63.0 | 97 | 58.1 | 194 | 65.8 | |
| Hispanic | 38 | 8.2 | 15 | 9.0 | 23 | 7.8 | |
| Other | 7 | 1.5 | 1 | 0.6 | 6 | 2.0 | |
| Education (highest level) | 0.640 | ||||||
| Less than 12th grade | 73 | 15.9 | 28 | 16.8 | 45 | 15.5 | |
| 12th grade, GED, or high school graduate | 213 | 46.5 | 81 | 48.5 | 132 | 45.4 | |
| Some college | 172 | 37.6 | 58 | 34.7 | 114 | 39.2 | |
| Marital Status | 0.253 | ||||||
| Single | 307 | 66.7 | 116 | 69.5 | 191 | 65.2 | |
| Cohabitating | 74 | 16.1 | 30 | 18.0 | 44 | 15.0 | |
| Married | 36 | 7.8 | 10 | 6.0 | 26 | 8.9 | |
| Separated/divorced | 43 | 9.4 | 11 | 6.6 | 32 | 10.9 | |
| Student status | 0.112 | ||||||
| No | 285 | 61.7 | 95 | 56.9 | 190 | 64.4 | |
| Yes | 177 | 38.3 | 72 | 43.1 | 105 | 35.6 | |
| Employment Status | 0.236 | ||||||
| Unemployed | 90 | 19.5 | 34 | 20.4 | 56 | 19.0 | |
| Employed or self-employed | 194 | 42.0 | 77 | 46.1 | 117 | 39.7 | |
| Otherb | 178 | 38.5 | 56 | 33.5 | 122 | 41.4 | |
| Federal Poverty Level | 0.777 | ||||||
| ≤100% | 383 | 83.4 | 141 | 85.5 | 242 | 82.3 | |
| 101%–199% | 39 | 8.5 | 11 | 6.7 | 28 | 9.5 | |
| 200%–250% | 28 | 6.1 | 10 | 6.1 | 18 | 6.1 | |
| >250% | 9 | 2.0 | 3 | 1.8 | 6 | 2.0 | |
| Health insurance | 0.885 | ||||||
| Uninsured | 371 | 80.3 | 133 | 79.6 | 238 | 80.7 | |
| Publicc | 79 | 17.1 | 29 | 17.4 | 50 | 17.0 | |
| Private | 12 | 2.6 | 5 | 3.0 | 7 | 2.4 | |
| Baseline cardiovascular disease risk factors | |||||||
| Blood pressure (mmHg) | 0.780 | ||||||
| Normal (SBP <120 and DBP <80) | 245 | 53.0 | 85 | 50.9 | 160 | 54.2 | |
| Pre-HTN (SB 120–139 or DBP 80–89) | 162 | 35.1 | 61 | 36.5 | 101 | 34.2 | |
| HTN (SBP ≥140 or DBP ≥90)d | 55 | 11.9 | 21 | 12.6 | 34 | 11.5 | |
| A1c classification (%) | 0.669 | ||||||
| Normal (≤5.6) | 307 | 66.5 | 107 | 64.1 | 200 | 67.8 | |
| Prediabetes (5.7–6.4) | 143 | 31.0 | 55 | 32.9 | 88 | 29.8 | |
| Diabetes (≥6.5)e | 12 | 2.6 | 5 | 3.0 | 7 | 2.4 | |
| Tobacco usef | |||||||
| Nonsmoker | 305 | 67.3 | 112 | 67.9 | 193 | 67.0 | 0.917 |
| Smoker | 148 | 32.7 | 53 | 32.1 | 95 | 33.0 | |
| BMI (kg/m2) | 0.434 | ||||||
| Underweight/normal (<24.9) | 149 | 32.3 | 59 | 35.3 | 90 | 30.5 | |
| Overweight (25–29.9) | 125 | 27.1 | 38 | 22.8 | 87 | 29.5 | |
| Obese (30.0–39.9) | 132 | 28.6 | 50 | 29.9 | 82 | 27.8 | |
| Extremely obese (≥40.0) | 56 | 12.1 | 20 | 12.0 | 36 | 12.2 | |
| Physical activityg | 0.261 | ||||||
| Active | 262 | 57.7 | 87 | 52.7 | 175 | 60.6 | |
| Insufficiently active | 106 | 23.4 | 43 | 26.1 | 63 | 21.8 | |
| Inactive | 86 | 18.9 | 35 | 21.2 | 51 | 17.7 | |
Due to missing data and rounding, values may not add to 462 or 100%, respectively.
Fisher's exact test used (rescreened versus not rescreened).
Includes student, homemaker, other.
Includes Medicaid, U.S. Government plans, Champus, and Veterans Affairs.
Includes women who are currently taking medication for high blood pressure.
Includes women who are currently taking medication for diabetes.
Defined by self-reported cigarette smoking.
Active defined as any combination totaling ≥150 minutes/week (self-reported). Insufficiently active defined as some but <150 minutes of moderate—or <75 minutes of vigorous—effort activity per week, or an equivalent combination. Inactive defined as no weekly physical activity.
BMI, body mass index; DBP, diastolic blood pressure; HTN, hypertension; InShape, Integrated Screening and Health Assessment, Prevention, and Evaluation; SBP, systolic blood pressure; SE, standard error.
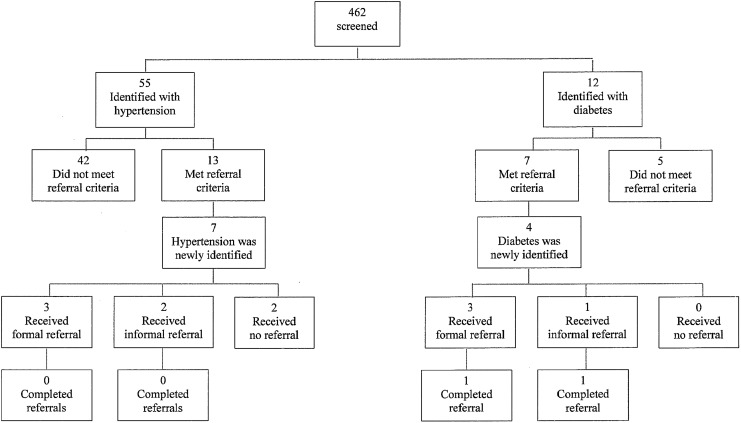
Of CVD risk factors identified at enrollment that met referral criteria [hypertension, n=13 (2.8%); diabetes, n=7 (1.5%)], 11 out of 20 (73.3%) were new diagnoses (Fig. 1). Of the 11 women with new diagnoses, formal referrals were made for 6 women (54.5%), informal referrals were made for 3 (27.3%), and 2 (18.2%) women were not referred. For the 11 newly diagnosed women, 6 referrals (54.5%) were made to the local federally qualified community health center (CHC), 2 (18.2%) were made to the local university medical center, and 1 (9.1%) was made to a clinic in a neighboring community. Among 11 women who met referral criteria, 2 (18.2%) completed referrals: one was the result of a formal referral to the university medical center and the other resulted from an informal referral to the neighboring community clinic.
FIG. 1.
Flow diagram of referral outcomes for women identified with hypertension or diabetes at screening visit among Integrated Screening and Health Assessment, Prevention and Evaluation screening study participants, North Carolina, 2011–2012.
Twenty-one women identified with hypertension at screening were rescreened. The maximum systolic BP detected was 160 mmHg and the maximum diastolic BP detected was 114 mmHg. The overall mean systolic BP decreased 7 mmHg (139 mmHg to 132 mmHg, p=0.001) and diastolic BP decreased 7 mmHg (90 mmHg to 83 mmHg, p=0.006) at rescreening among these women (Table 2). In sensitivity analyses that included all women who returned for a subsequent annual visit and had data on BP (n=165), mean systolic BP did not differ statistically between enrollment and the subsequent annual visit (119 mmHg at both visits, p=0.983), but the overall mean diastolic BP decreased 2 mmHg at the subsequent annual visit (76 to 74 mmHg, p=0.007).
Table 2.
Mean Test Results at Screening and Rescreening One Year Later, and Difference in Measures Among InShape Study Participants Identified with Hypertensiona and Diabetesb (North Carolina, 2011–2012)
| Test | Screening visit mean (SE) | Rescreening visit mean (SE) | Difference (SE) | 95% Confidence interval | p value |
|---|---|---|---|---|---|
| Systolic blood pressure (mmHg, n=21) | 139 (2.5) | 132 (2.4) | −7 (2.0) | −12, −4 | 0.001 |
| Diastolic blood pressure (mmHg, n=21) | 90 (2.1) | 83 (1.9) | −7 (2.3) | −12, −2 | 0.006 |
| Hemoglobin A1c (%, n=5) | 7.5 (0.7) | 7.9 (1.4) | 0.4 (0.8) | −1.7, 2.5 | 0.640 |
Hypertension defined as blood pressure ≥140/90 mmHg; includes women with new and previously diagnosed hypertension
Diabetes defined as hemoglobin A1c ≥6.5%; includes women with new and previously diagnosed diabetes.
SE, standard error.
Five women identified with diabetes at screening were rescreened. The overall mean hemoglobin A1c was slightly higher at rescreening but not statistically different compared with the screening visit (7.9% versus 7.5%, respectively, p=0.640, Table 2). In sensitivity analyses that included all women who were rescreened and had data on A1c (n=160), the overall mean A1c did not differ statistically between the screening and rescreening visits (6% at both visits, p=0.820).
Among 148 women who reported smoking at enrollment, 129 (87.2%) received cessation counseling and 8 (5.4%) accepted tobacco quitline referrals. Of those referred, one accepted services and received multiple counseling sessions plus the nicotine patch, another woman declined services as she was already receiving quitline services, and six were unreachable. Of 148 smokers, 53 (35.8%) returned for their subsequent annual visit and 11 (20.9%) reported nonsmoking at that time (p<0.001, Table 3). In a sensitivity analysis that included all women who were rescreened and had data on smoking (n=165), prevalence of smoking was lower at rescreening (46/165, 27.9%) but not statistically different from smoking prevalence at screening (53/165, 32.1%, p=0.071).
Table 3.
Status of Smoking and Obesity Among InShape Participants Who Smoked or Were Obese at Screening and Were Rescreened One Year Later (North Carolina, 2011–2013)
| Status of CVD risk factors | Screening visit n (%) | Rescreening visit n (%) | Chi square p value |
|---|---|---|---|
| Cigarette smokersa (n=53) | 0.0005 | ||
| Nonsmoker | 0 (0) | 11 (21) | |
| Smoker | 53 (100) | 42 (79) | |
| Weight (pounds), mean (SE) (n=70) | 221 (5.3) | 225 (5.3) | 0.0465 |
| BMI (kg/m2),b (n=70) | <0.0001 | ||
| Underweight/normal (<24.9) | 0 (0) | (0) | |
| Overweight (25–29.9) | 0 (0) | 6 (9) | |
| Obese (30.0–39.9) | 50 (71) | 42 (60) | |
| Extremely obese (≥40.0) | 20 (29) | 22 (31) |
Due to rounding, percentages may not add to 100%.
Defined by self-reported smoking.
Calculated from clinically measured height and weight.
CVD, cardiovascular disease.
Among 188 women identified as obese at enrollment, 22 (11.7%) scheduled nutrition appointments, but only one attended. Six obese participants who returned for a subsequent annual visit lost weight and were no longer obese (Table 3). However, the mean weight significantly increased between enrollment (221 lbs.) and the subsequent annual visit (225 lbs.) among obese women who were rescreened (n=70, p=0.047). In a sensitivity analysis that included all women who returned for a subsequent annual visit and had data on weight (n=165), the overall mean weight also increased from 175 to 181 lbs. between visits (p<0.001).
Discussion
Of women who were screened, approximately one-third were rescreened at their next annual family planning visit; more than half did not return to the clinic, declined participation, or were missed; and an additional 10% became pregnant. Most women who were newly diagnosed with hypertension or diabetes were offered referrals. However, only 2 of 11 women with newly diagnosed hypertension or diabetes completed referrals, even though the majority of referrals were formally facilitated by the health department.
Reported referral completion rates among similar populations of women who receive formal referrals for abnormal Pap tests are substantially higher. A study of Medicaid-enrolled family planning providers in Arkansas and Alabama found 62.4% of their patients reported receiving follow up care for an abnormal Pap test.7 Some women were treated on-site by their family planning providers, while others received external referrals. Among women who were not treated on-site but were referred for follow up, 40.5% completed the referrals.7
The difference in referral completion rates between our study and those reported by the aforementioned study of low-income family planning women7 is notable. An important difference between the two studies is the condition of interest. The earlier study examined follow up for cervical cancer screening. There is a culture that supports cancer screening and taking action for abnormal results from cancer screening tests, in part due to the perceived suffering generated by cancer.10 The same culture may not exist for other diseases and conditions, such as CVD risk factors, which may not be perceived by patients as debilitating or life threatening. In the absence of such a culture, it may be difficult to engage women in taking action for asymptomatic problems—such as hypertension. Moreover, follow up rates in the Pap test study7 were higher among women who were treated by the same family planning provider that did the screening, compared with those who were referred to other providers. It is possible that follow up for hypertension and diabetes would have been more successful if treated on-site rather than by referral.
Since Title X clinics are expected to treat on-site or make referrals to meet their low-income clientele's additional health care needs,11 the very low referral completion rates reported in this study are concerning. Screening for hypertension and smoking are quality standards of care for safe and effective use of some forms of contraception, particularly hormonal contraceptive methods. Screening for obesity and diabetes, as clinically indicated, is considered part of preconception care,3 which is a component of family planning services.11 Therefore, understanding the outcomes of referrals made in these settings has important programmatic implications for Title X and other health care systems concerned with ensuring access to quality, comprehensive care.
Finding primary care providers who will accept referrals for uninsured and indigent patients can be challenging.12 This barrier is particularly difficult for Title X family planning clinics, which often are located in resource-limited areas. Unlike many rural communities, Pitt County does not have this barrier, as there are multiple medical resources that could provide referral care for indigent patients with CVD risk factors, including a state-supported academic medical center and a federally qualified CHC. In our study, most women were referred to the CHC, which uses a standard sliding fee scale for low-income patients.
Referrals to telephone quitlines for smoking cessation pose no financial barriers to women, as quitlines are free and offer assistance that may not be available to uninsured smokers elsewhere.13 Unfortunately, in this study, most women who accepted telephone quitline referrals were later unreachable. On-the-spot interventions (e.g., prescriptions for pharmacotherapy) and same-day referrals may be more successful. Brief clinical interventions—such as five A's cessation counseling— are effective9 and clinicians might consider incorporating these during family planning clinic visits, as was done at the health department. Smoking cessation might also increase if one-on-one counseling sessions with tobacco-cessation specialists were available, as was demonstrated by a Well-Integrated Screening and Evaluation for Women across the Nation (WISEWOMAN) program in Alaska among women aged 40–64 years.14 However, participation in counseling sessions and impact of cessation rates may differ between reproductive age and older women. Moreover, the additional cost and time required to incorporate these services into routine medical visits needs to be examined.
While health care access does not always translate into utilization,15 it is unknown why the majority of women with CVD risk factors in this study did not receive needed follow-up care. Implementation of electronic medical records may alert clinicians to noncompletion of referrals and trigger follow up on failed referrals when patients return to the clinic. Tangible solutions to patient-level reasons for noncompletion of referrals are less clear. For example, some research among similar populations suggests fatalism and having previous negative experiences with health care providers as reasons for nonuse of breast cancer screening when such care is available and accessible.16 Additionally, a recent systematic review reported that prioritizing clinic visits over the needs of family members and work was commonly reported by patients as a barrier to hypertension treatment and follow up.17 Finally, low referral completions in our study may be explained by financial and transportation barriers and delays in referral appointment dates.
Since the health department is the usual source of care for the majority of women in this sample,2 it is also unclear why nearly half did not return for their subsequent annual visits. Low-income women of reproductive age, particularly those with young children, can have limited free time and competing priorities. Therefore, timely preventive health care visits may not rise to the top of the daily demands. However, interruption of contraceptive services is likely to result in unplanned pregnancies. Additionally, the discontinuity of care represented by the low rescreening rates presents challenges for providing preconception care and preventing unintended pregnancies—both of which are essential components of quality family planning services and Title X.11 It is possible that rescreening rates would have been higher among this population if all women participating had the opportunity to be rescreened up to 18 months after the initial screening. Our re-screening period captured all women who were screened and rescreened 12–13 months later. However, women who were screened earlier during the interval of May 2011–February 2012 had longer to get rescreened than those who were screened later.
The limitations of the screening study were previously elucidated and included possible overestimation of hypertension prevalence, potential selection and recall bias, and the generalizability of results.2 Although the rescreened sample constitutes only 36% of the initial sample of women who were screened at enrollment, women who were rescreened did not differ on baseline characteristics from those who were not rescreened. However, it is likely that we did not measure all characteristics that affect health care–seeking behavior. Finally, evaluating improvements among women who screened positive for CVD risk factors was limited by the small sample. Nevertheless, few published studies have examined outcomes of screening for CVD risk factors in women of reproductive age; therefore, this study contributes to that small literature.
Conclusions
Women attending Title X clinics are routinely screened for several CVD risk factors, but previous studies have not examined the outcomes of that screening. This study found that the majority of women with newly identified CVD risk factors received indicated referrals, but few women completed those referrals. Treating CVD risk factors can impact the long-term health of women and improve their pregnancy outcomes. Thus, research is needed to (1) improve understanding about the barriers and facilitators to receiving referral care for management of CVD risk factors among low-income women of reproductive age, (2) explore the feasibility of managing CVD risk factors on-site in Title X settings, and (3) identify best practices in managing these risk factors for women who screen positive in these settings.
Acknowledgments
The authors gratefully acknowledge the Pitt County Health Department nurses and leadership for assisting in this study, particularly Deborah B. Herring, MHA, BSN, MHA; Kimberly B Hardy, MSN, FNP-BC; Stephanie Hart, RN, MA; and Susan S. Shelton, BSN. We also thank Ashley Ronay, MPH, for her help with the study and all of the women who participated in this project. The authors also express appreciation to Anne Cole, BA, for her role in assuring data quality, and Rachel Urrutia, MD, (University of North Carolina at Chapel Hill) for her review of the manuscript.
This work was supported by Cooperative Agreement Number 5U48DP001944 from the Centers for Disease Control and Prevention. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author Disclosure Statement
The authors report no conflicts of interest.
References
- 1.Bombard JM, Dietz PM, Galavotti C, England LJ, Tong VT, Hayes DK, et al. Chronic diseases and related risk factors among low-income mothers. Matern Child Health J 2012;16:60–71 [DOI] [PubMed] [Google Scholar]
- 2.Robbins CL, Keyserling TC, Pitts SB, Morrow J, Majette N, Sisneros JA, et al. Screening low-income women of reproductive age for cardiovascular disease risk factors. J Womens Health (Larchmt) 2013;22:314–321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Recommendations to improve preconception health and health care–United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep 2006;55(RR-6):1–23 [PubMed] [Google Scholar]
- 4.Fowler CI, Lloyd S, Gable J, Wang J, McClure E. (November 2012). Family planning annual report: 2012 National Summary. Research Triangle Park, NC: RTI International, 2013 [Google Scholar]
- 5.Gold RB, Sonfield A, Richards CL, Frost JJ. Next steps for America's family planning program: Leveraging the potential of Medicaid and Title X in an evolving health care system. New York: Guttmacher Institute, 2009 [Google Scholar]
- 6.Felix HC, Bronstein J, Bursac Z, Stewart MK, Foushee HR, Klapow J. Referral and referral facilitation behavior of family planning providers for women with HIV infection in the southern United States. J Womens Health (Larchmt) 2010;19:1385–1391 [DOI] [PubMed] [Google Scholar]
- 7.Felix HC, Bronstein J, Bursac Z, Stewart MK, Foushee HR, Klapow J. Family planning provider referral, facilitation behavior, and patient follow-up for abnormal Pap smears. Public Health Rep 2009;124:733–744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chobanian AV, Bakris GL, Black HR, et al. ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National High Blood Pressure Education Program Coordinating Committee. National Heart Lung Blood Institute. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–1252 [DOI] [PubMed] [Google Scholar]
- 9.Fiore MC, Jaén CR, Baker TB, et al. Treating tobacco use and dependence: 2008. update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service, May 2008 [Google Scholar]
- 10.Croswell JM, Ransohoff DF, Kramer BS. Principles of cancer screening: Lessons from history and study design issues. Semin Oncol 2010;37:202–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gavin L, Moskosky S, Carter M, Curtis K, Glass E, Godfrey E, et al. Providing quality family planning services: Recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep 2014;63(RR04):1–54 [PubMed] [Google Scholar]
- 12.Bodenheimer T, Chen E, Bennett HD. Confronting the growing burden of chronic disease: Can the U.S. health care workforce do the job? Health Aff (Millwood) 2009;28:64–74 [DOI] [PubMed] [Google Scholar]
- 13.Bombard JM, Farr SL, Dietz PM, Tong VT, Zhang L, Rabius V. Telephone smoking cessation quitline use among pregnant and non-pregnant women. Matern Child Health J 2013;17:989–995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vaid I, Ahmed K, May D, Manheim D. The WISEWOMAN Program: Smoking Prevalence and key approaches to smoking cessation among participants, July 2008–June 2013. J Womens Health (Larchmt) 2014;23:288–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Devoe JE, Baez A, Angier H, Krois L, Edlund C, Carney PA. Insurance+access not equal to health care: Typology of barriers to health care access for low-income families. Ann Fam Med 2007;5:511–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peek ME, Sayad JV, Markwardt R. Fear, fatalism and breast cancer screening in low-income African-American women: The role of clinicians and the health care system. J Gen Intern Med 2008;23:1847–1853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khatib R, Schwalm JD, Yusuf S, Haynes RB, McKee M, Khan M, et al. Patient and healthcare provider barriers to hypertension awareness treatment and follow up: A systematic review and meta-analysis of qualitative and quantitative studies. PLoS One 2014;9:e84238. [DOI] [PMC free article] [PubMed] [Google Scholar]