Abstract
Anxiety is a common condition which can manifest with symptoms of chest discomfort. Chest discomfort is one of the most common reasons to seek emergency medical care. We hypothesize that anxiety is highly prevalent, poorly diagnosed, and poorly treated in an acute care environment. We analyzed data from a prospective registry of chest pain patients with low to intermediate likelihood of acute coronary syndrome and coronary artery disease. Scores from the General Anxiety Disorder-7 questionnaire determined the prevalence of anxiety. Differences in presentation, evaluation, and 30 day outcomes were compared for subjects with and without severe anxiety. Of the 151 included subjects, severe anxiety was observed in 15%, moderate 14%, mild 30%, and 41% had no anxiety symptoms. Subjects with severe anxiety had similar baseline characteristics, cardiac risk factors, and symptoms to those without severe anxiety, except for the current use of tobacco 50.0% versus 18.6%, p=0.001). Anxiety was self-reported by 54.5% of subjects with severe anxiety and 27.3% were on antianxiety medications. Hospital admission (p=0.888) and repeat ED visits within 30 days (p=0.554) were not different between the two groups. Anxiety is common among patients seeking emergency evaluation of chest pain. Half of patients with severe anxiety were diagnosed and roughly one quarter were medically treated. Cardiac risk factors and symptoms are not different for patients with severe anxiety; these patients warrant a similar evaluation for heart disease as those patients without anxiety.
Keywords: anxiety, chest pain, outcomes, coronary artery disease, risk assessment
Introduction
Anxiety disorders are prevalent in the general population, affecting up to one in five patients in community samples1 and higher in samples of patients referred for cardiac complaints.2 These disorders are associated with poorer quality of life and higher utilization of health care resources.3,4,5 Up to half of patients with generalized anxiety disorder report a history of chest pain symptoms and, for many patients, this distressing symptom prompts them to seek immediate medical attention at the nearest emergency department.6
Chest pain complaints are also prevalent and are the principal reason for millions of emergency department (ED) visits in the United States annually.7 Lacking a definitive test for anxiety related chest pain, ED doctors are obliged to evaluate each instance for life-threatening conditions such as myocardial infarction and ischemia. These evaluations are time consuming and costly. Further, patients are frequently unsatisfied with the results as they are left wondering, “if not my heart, what is causing my symptoms?” Underrecognition and undertreatment of anxiety disorder could play a role in these patients seeking acute medical attention.
To investigate interactions between chest pain and anxiety, we evaluated data from patients evaluated at our institution's Chest Pain Evaluation Center (CPEC). The CPEC is a standalone section in our ED for extended observation and testing of chest pain patients with low to intermediate risk of acute coronary syndrome (ACS) and pretest likelihood of coronary artery disease (CAD). Patients in the CPEC are asked to participate in a prospective registry which includes several patient directed questionnaires, including a standardized assessment of anxiety symptoms. We hypothesize that anxiety is prevalent in this population and that anxiety is underdiagnosed and undertreated.
Materials and Methods
At our academic institution, patients presenting to the ED with an acute complaint of chest discomfort are evaluated for possible ACS. If initial laboratory testing and electrocardiogram (ECG) do not indicate ACS, patients are eligible for further care in the CPEC based on their age, symptoms, and CAD risk factors. The CPEC is a 8 bed unit physically located within our ED; further details on our CPEC and chest pain protocol have been previously described.8 Further care for the patients includes serial laboratory testing and ECGs as well as testing for CAD, typically with either exercise treadmill testing or computed tomographic coronary angiography (CTCA). Patients in the CPEC are asked to participate in a prospective registry documenting their symptoms, medical history, standardized questionnaires, and outcomes. An analysis of anxiety symptoms was prespecified in the design of the registry.
Our institutional review board reviewed and approved this prospective registry which was conducted in accord with the Declaration of Helsinki. Written, informed consent was sought from all CPEC patients consecutively. Refusal to consent was the only exclusion criterion for the registry. After consent was given, registry data were collected on paper forms at the point of care. Data from those forms were recorded electronically in a custom database using REDcap software.9
Data collected included demographics, symptoms, medical history, risk factors for CAD (age, gender, body mass index, hypertension, dyslipidemia, diabetes, tobacco use, history of stroke, and family history of coronary artery disease), comorbid conditions, and outcomes of the CPEC evaluation. Subjects were asked to describe three specific characteristics of their angina: the location, onset with exertion, and relief with rest. These responses were used to categorize angina using Diamond and Forrester's model: noncardiac (0 or 1 characteristics), atypical (2 characteristics), or typical (3 characteristics).10 Each of these data fields as well as determinations about angina were made by the CPEC providers. These individuals are either nurse practitioners or physician assistants with specific training in both research methods and the evaluation/ management of chest pain. Monthly inservice meetings were held that served to review recent clinical encounters as well as discuss research progress with the principal investigator (DEW). Regular updates were discussed including review of enrollment and any difficulties with the study. Antianxiety medications broadly defined and based on patient self report, including benzodiazepines as well as neurotransmitter modulating drugs such as selective serotonin reuptake inhibitors. All subjects were contacted 30 days after their CPEC visit to ascertain any repeat ED visits, additional cardiovascular testing, or other cardiovascular events. Subjects were initially contact by phone; if they could not be reached, certified mail was sent to their last known address. Follow-up data was input directly into the REDcap database at the time of collection.
Subjects in the CPEC Registry are asked to complete several self-administered standardized questionnaires, including the GAD-7.11 The GAD-7 is an instrument used to screen for generalized anxiety disorder and consists of seven questions, each rated on a zero to three scale, inquiring about anxiety related symptoms within the last 2 weeks. A score of 0-4 denotes no anxiety, 5-9 mild anxiety, 10-14 moderate anxiety, and over 15 severe anxiety. The GAD-7 has been used and validated in multiple populations; when comparing the GAD-7 to a structured psychiatric interview, area under the receiver-operator curve for generalized anxiety disorder is 0.91 and for any anxiety disorder is 0.86.12,13,14
Outcomes and Analysis
The outcomes for this investigation are to 1) establish the prevalence of anxiety in the CPEC registry and 2) make comparisons of presentation, evaluation, and outcomes for subjects with and without severe anxiety symptoms. Prevalence of anxiety was determined using GAD-7 scores for the entire CPEC Registry population. Patients with severe anxiety would be most likely to benefit from further evaluation and treatment of their psychiatric illness and were therefore selected as the focus of analysis. Comparisons were made between the subset of subjects with severe anxiety (GAD-7 score > 15) and the remainder of the subjects. Continuous variables were compared by the student's t-test. Categorical variables were compared using the chi square test. All statistical analyses were performed using SPSS version 21 (IBM, Armonk, NY). We followed the STROBE statement in the development and reporting of this investigation.15
Results
Of the subjects in the CPEC Registry, 151 were recruited from December 2011 through January 2013 and had complete data on their GAD-7 and 30 day followup. Distribution of anxiety scores based on the results of the GAD-7 questionnaire were 41% with no anxiety (score of 0-4), 30% with mild anxiety (score of 5-9), 14% with moderate anxiety (score of 10-14), and 15% with severe anxiety (score ≥ 15). (Figure 1) Subjects were categorized as either severe anxiety (SA, n=22) or non-severe anxiety (NSA, n=129). Baseline characteristics are presented in Table 1.
Figure 1. Distribution of anxiety categories.
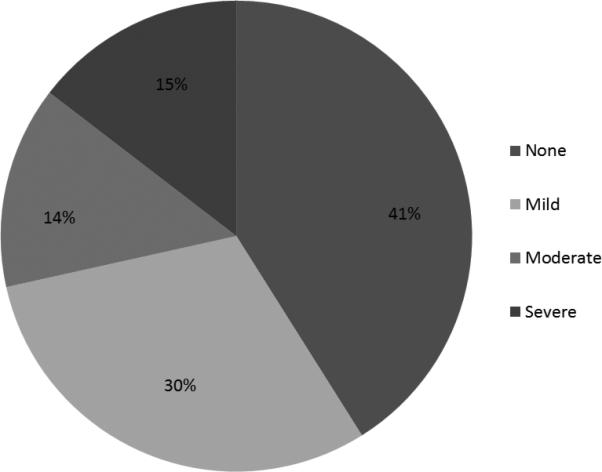
Subjects in this investigation completed a standardized questionnaire on anxiety symptoms to categorize them as having severe, moderate, mild, or no anxiety. This chart demonstrates the distribution of anxiety categories.
Table 1.
Baseline Characteristics
| Characteristic | NSA Group, n=129 | SA group, n=22 | P value | ||
|---|---|---|---|---|---|
| mean | SD | mean | SD | ||
| Body mass index | 30.7 | 7.6 | 29.4 | 6.3 | 0.414 |
| Age (years) | 46.2 | 10.2 | 42.4 | 9.3 | 0.102 |
| N | % | N | % | ||
| Female | 88 | 68.2% | 14 | 63.6% | 0.671 |
| Diabetes | 9 | 7.0% | 3 | 13.6% | 0.286 |
| Hypertension | 48 | 37.2% | 6 | 27.3% | 0.369 |
| Hyperlipidemia | 22 | 17.1% | 1 | 4.5% | 0.131 |
| Current Tobacco | 24 | 18.6% | 11 | 50.0% | 0.001 |
| Stroke | 4 | 3.1% | 0 | 0.0% | 0.403 |
| Family History | 69 | 53.5% | 7 | 31.8% | 0.679 |
NSA = non severe anxiety, SA = severe anxiety, SD = standard deviation
Baseline characteristics
Both groups were predominantly female, no difference in gender was observed between the two groups. (SA=63.6%, NSA=68.2%, p=0.67). The only cardiovascular risk factor difference between the groups was current tobacco use, more common in the SA group (50.0%) as compared to the NSA group (18.6%) (p=0.001). No differences were observed in prevalence of diabetes, hypertension, dyslipidemia, or family history of coronary artery disease.
Angina
Subjects were asked several questions about specific characteristics of their angina including the frequency of angina episodes in the week prior to ED evaluation and angina severity rating on a 10 point scale (1 being no pain at all, and 10 being the worst pain imaginable). (Table 2) Angina severity was significantly higher for the SA group (7.7 vs. 6.3 on 10 point scale, p=0.002) while angina episodes in the preceding week were non-significantly higher for the SA group (7.9 vs 3.7 episodes per week, p=0.267). The distribution of angina classifications was not different between the groups (p=0.269) and neither was the typical duration of angina symptoms (p=0.261). Numerically fewer patients in the SA group, however, had typical angina symptoms.
Table 2.
Symptom characteristics
| Characteristic | NSA Group, n=129 | SA group, n=22 | P value | ||
|---|---|---|---|---|---|
| Mean/N | SD/% | Mean/N | SD/% | ||
| Angina | |||||
| When you have angina how severe is it (scale of 1-10)? | 6.3 | 2.5 | 7.7 | 1.6 | 0.002 |
| How many episodes of angina have you had in the last week? | 3.7 | 4.5 | 7.9 | 16.4 | 0.267 |
| How many minutes does an episode of angina usually last? | 0.261 | ||||
| 0-15 minutes | 47 | 37.0% | 6 | 27.3% | |
| 15-60 minutes | 16 | 12.6% | 1 | 4.5% | |
| over 60 minutes | 64 | 50.4% | 15 | 68.2% | |
| Angina Classification | 0.269 | ||||
| noncardiac | 66 | 51.2% | 12 | 54.5% | |
| atypical | 33 | 25.6% | 8 | 36.4% | |
| typical | 30 | 23.3% | 2 | 9.1% | |
| Anxiety | |||||
| Diagnosed with anxiety | 24 | 18.6% | 12 | 54.5% | <0.001 |
| Taking antianxiety medications | 9 | 7.0% | 6 | 27.3% | 0.003 |
| Very/extremely worried about chest pain | 42 | 32.8% | 16 | 72.7% | <0.0001 |
NSA = non severe anxiety, SA = severe anxiety, SD = standard deviation
Anxiety
GAD-7 scores were used to classify subjects as having SA or NSA. Subjects were also asked if they had been clinically diagnosed with anxiety in the past. The prevalence of anxiety was higher in the SA group, however, only half of the subjects in the SA group were aware of their diagnosis (54.5% versus 18.6% in the NSA group, p<0.001); (Table 2) The use of medications to treat anxiety was higher in the SA group but only one quarter were receiving medications. (27.3% versus 7.0%, p=0.003), Subjects were asked to rate how worried they were about their chest pain. Of the SA group, 72.7% indicated they were very worried or extremely worried, compared to 34.7% of the NSA group (p<0.0001).
Evaluation and outcomes
Subjects with and without severe anxiety underwent a similar diagnostic testing while in the ED. (Table 3) In the NSA group, 57.4% underwent exercise treadmill stress testing versus 63.6% of the SA group (p=0.581), while 28.7% of the NSA group versus 22.7% of the SA group (p=0.565) underwent computed tomography coronary angiography. 5.8% of the NSA group versus 5% of the SA group (p=0.888) were admitted to the hospital for further evaluation. There was no statistical difference regarding 30 day follow up with a PCP or other doctor about chest pain (p=0.439), or 30 day recidivism to the ED with chest pain (p=0.554).
Table 3.
Evaluation and outcomes
| Outcome | NSA Group, n=129 | SA group, n=22 | P value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Evaluation | |||||
| Exercise treadmill | 74 | 57.4% | 14 | 63.6% | 0.581 |
| Computed tomography coronary angiography | 37 | 28.7% | 5 | 22.7% | 0.565 |
| Admit to hospital | 7 | 5.8% | 1 | 5.0% | 0.888 |
| 30 day follow-up | |||||
| Follow up with primary care doctor | 32 | 33.0% | 4 | 23.5% | 0.439 |
| Return ED visit for chest pain | 2 | 2.0% | 0 | 0.0% | 0.554 |
| Treated for anxiety since ED visit | 5 | 3.9% | 4 | 18.2% | 0.009 |
ED = emergency department, NSA = non severe anxiety, SA = severe anxiety
Discussion
While chest pain is a common primary reason for patients to seek acute care in an ED, the culprit diagnosis is heart disease in a minority of cases. This prospective evaluation of patients with chest pain and low risk of heart disease has established that anxiety is common, underdiagnosed, and undertreated.
We demonstrated our initial hypothesis that anxiety would be highly prevalent in our prospective registry. The possible causes for this observation, however, are multiple. We postulate that there is a true overrepresentation of anxiety disorder in the acute chest pain population. The observed prevalence of anxiety in our cohort is several fold higher than a general population (5% moderate, 1% severe),13 but closer to that observed in another ED population (12.7% using another questionnaire).16 This higher prevalence has also been reported in other populations of patients with chest pain and referred for chest pain evaluations.2,17 Within our cohort, however, subjects responded to a question about worry and their chest pain. SA group subjects were more likely to indicate a high degree of worry about their chest pain, but we cannot prove the causality of this relationship. Anxiety may provoke sensations of chest discomfort, however chest discomfort may also induce anxiety symptoms, particularly in those who already carry a diagnosis of anxiety. Anxiety is more common in patients with established heart disease18 and has been linked to poorer outcomes for patients with demonstrated heart disease or ischemia.19,20
Given these confounders, the prospective clinical utility of our observation may be limited, especially during the initial evaluation of chest pain patients. While we observed a high prevalence of anxiety symptoms, the subjects with the most severe anxiety had essentially the same symptom and risk factor profile as the subjects without severe anxiety. Absence of any differences may be due to low power of our investigation for this sort of analysis. Anxiety may not be as useful as other signs and symptoms for distinguishing those with and without ACS,21 making anxiety challenging to use to prospectively identify patients who could undergo a less extensive evaluation for heart disease. Once possible heart disease has been adequately evaluated, the clinical utility of diagnosing anxiety is more relevant. Screening for anxiety as part of a secondary assessment of chest pain would seem to be appropriate and has been demonstrated to be effective as part of a protocol to screen for psychiatric diseases, musculoskeletal disorders, and gastroesophageal reflux.22
Screening for anxiety has been attempted with other instruments23 and led to the development of additional questionnaires beyond the GAD-7. The Cardiac Anxiety Questionnaire, for example, sought to isolate cardiac anxiety from other forms of anxiety in hospitalized patients.24 The Panic Screening Score is another instrument which has demonstrated modest accuracy in the ED setting.25 These questionnaires have not been cross-validated with the GAD-7 or a reference standard, such as clinical psychiatric assessment, so it remains to be seen which might be the most relevant to the ED physician.
Our 30 day follow up did not demonstrate a significant difference between the SA and NSA groups with regard to return ED visits. We would presume that additional attention to establishing a firm diagnosis for a chest pain complaint would result in fewer return visits, however we cannot make such an assertion based on our data. Return visits were not a primary outcome for this investigation and will require further study.
Limitations
Our analysis is limited in having gathered data on anxiety and chest pain evaluation during the same encounter. Sample size leaves the investigation underpowered to determine if SA group patients have significantly risk of repeat ED visits. Selection bias is a possibility in our registry, however patients concerned about documentation of psychiatric disease would be less likely to participate and would then serve to underestimate anxiety. Proving a causal relationship between the two conditions is not possible with this investigation. As noted previously, interactions between anxiety, chest pain, and heart disease may confound the degree to which anxiety is a stand-alone diagnosis for subjects in this investigation.
Conclusions
In summary, anxiety is common in ED patients with chest pain with prevalence several fold higher than the general population. In the ED population, anxiety is markedly underdiagnosed and undertreated. CAD risk factors and symptoms were similar between patients with and without severe anxiety suggesting that a diagnosis of anxiety does not identify patients suitable for an abbreviated or accelerated heart disease evaluation.
Acknowledgments
Grant support: Data collection was supported in part by the Clinical and Translational Science Institute (NIH grant 1UL1RR029890)
Abbreviations
- ACS
acute coronary syndrome
- CAD
coronary artery disease
- CPEC
Chest Pain Evaluation Center
- CTCA
computed tomography coronary angiography
- ECG
electrocardiogram
- ED
emergency department
- NSA
non-severe anxiety group
- SA
severe anxiety group
Footnotes
Disclosures: Dr. Winchester is a member of the Society of Cardiovascular Patient Care Board of Directors, all other authors have no conflicts to disclose
Institutional Review Board: Approved by our institution, all participants provided written, informed consent
Meetings: These data were presented at the Congress of the Society of Cardiovascular Patient Care in Orlando, FL (April 2013)
References
- 1.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007 Mar 6;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 2.Jonsbu E, Dammen T, Morken G, Lied A, Vik-Mo H, Martinsen EW. Cardiac and psychiatric diagnoses among patients referred for chest pain and palpitations. Scand Cardiovasc J. 2009 Aug;43(4):256–259. doi: 10.1080/14017430902946749. [DOI] [PubMed] [Google Scholar]
- 3.Bereza BG, Machado M, Einarson TR. Systematic review and quality assessment of economic evaluations and quality-of-life studies related to generalized anxiety disorder. Clin Ther. 2009 Jun;31(6):1279–1308. doi: 10.1016/j.clinthera.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Konnopka A, Leichsenring F, Leibing E, Konig HH. Cost-of-illness studies and cost-effectiveness analyses in anxiety disorders: a systematic review. J Affect Disord. 2009 Apr;114(1-3):14–31. doi: 10.1016/j.jad.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Deacon B, Lickel J, Abramowitz JS. Medical utilization across the anxiety disorders. J Anxiety Disord. 2008;22(2):344–350. doi: 10.1016/j.janxdis.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Carter CS, Maddock RJ. Chest pain in generalized anxiety disorder. Int J Psychiatry Med. 1992;22(3):291–298. doi: 10.2190/RGC5-PJK2-7TG5-KL1B. [DOI] [PubMed] [Google Scholar]
- 7.Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Advance Data. 2007;(386):1–32. 386. [PubMed] [Google Scholar]
- 8.Winchester DE, Stomp D, Shifrin RY, Jois P. Design and implementation of a stand-alone chest pain evaluation center within an academic emergency department. Crit Pathw Cardiol. 2012 Sep;11(3):123–127. doi: 10.1097/HPC.0b013e31825d28b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979 Jun 14;300(24):1350–1358. doi: 10.1056/NEJM197906143002402. [DOI] [PubMed] [Google Scholar]
- 11.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006 May 22;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 12.Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010 Jul-Aug;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Lowe B, Decker O, Muller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008 Mar;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 14.Herr NR, Williams JW, Benjamin S, McDuffie J. Does this patient have generalized anxiety or panic disorder?: The Rational Clinical Examination systematic review. JAMA. 2014 Jul;312(1):78–84. doi: 10.1001/jama.2014.5950. [DOI] [PubMed] [Google Scholar]
- 15.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007 Oct 16;4(10):e296. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Srinivasan K, Joseph W. A study of lifetime prevalence of anxiety and depressive disorders in patients presenting with chest pain to emergency medicine. Gen Hosp Psychiatry. 2004 Nov-Dec;26(6):470–474. doi: 10.1016/j.genhosppsych.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Rohani A, Akbari V, Zarei F. Anxiety and depression symptoms in chest pain patients referred for the exercise stress test. Heart Views. 2011 Oct;12(4):161–164. doi: 10.4103/1995-705X.90903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Todaro JF, Shen BJ, Raffa SD, Tilkemeier PL, Niaura R. Prevalence of anxiety disorders in men and women with established coronary heart disease. J Cardiopulm Rehabil Prev. 2007 Mar-Apr;27(2):86–91. doi: 10.1097/01.HCR.0000265036.24157.e7. [DOI] [PubMed] [Google Scholar]
- 19.Moser DK, McKinley S, Riegel B, et al. Relationship of persistent symptoms of anxiety to morbidity and mortality outcomes in patients with coronary heart disease. Psychosom Med. 2011 Nov-Dec;73(9):803–809. doi: 10.1097/PSY.0b013e3182364992. [DOI] [PubMed] [Google Scholar]
- 20.Rutledge T, Kenkre TS, Bittner V, et al. Anxiety associations with cardiac symptoms, angiographic disease severity, and healthcare utilization: The NHLBI-sponsored Women's Ischemia Syndrome Evaluation. Int J Cardiol. 2013 Oct 3;168(3):2335–2340. doi: 10.1016/j.ijcard.2013.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Panju AA, Hemmelgarn BR, Guyatt GH, Simel DL. The rational clinical examination. Is this patient having a myocardial infarction? JAMA. 1998 Oct 14;280(14):1256–1263. doi: 10.1001/jama.280.14.1256. [DOI] [PubMed] [Google Scholar]
- 22.Husser D, Bollmann A, Kuhne C, Molling J, Klein HU. Evaluation of noncardiac chest pain: diagnostic approach, coping strategies and quality of life. Eur J Pain. 2006 Jan;10(1):51–55. doi: 10.1016/j.ejpain.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 23.Fleet RP, Dupuis G, Marchand A, Burelle D, Beitman BD. Detecting panic disorder in emergency department chest pain patients: a validated model to improve recognition. Ann Behav Med. 1997;19(2):124–131. doi: 10.1007/BF02883329. Spring. [DOI] [PubMed] [Google Scholar]
- 24.van Beek MH, Voshaar RC, van Deelen FM, van Balkom AJ, Pop G, Speckens AE. The cardiac anxiety questionnaire: cross-validation among cardiac inpatients. Int J Psychiatry Med. 2012;43(4):349–364. doi: 10.2190/PM.43.4.e. [DOI] [PubMed] [Google Scholar]
- 25.Foldes-Busque G, Fleet R, Poitras J, et al. Preliminary investigation of the Panic Screening Score for emergency department patients with unexplained chest pain. Acad Emerg Med. 2011 Mar;18(3):322–325. doi: 10.1111/j.1553-2712.2011.01009.x. [DOI] [PubMed] [Google Scholar]


