Abstract
Background and Aims: Pregnancy tumours (PTs) are a non-neoplastic, reactive, inflammatory conditional gingival enlargement which occurs in the oral cavity during pregnancy. The lesion most frequently occurs on the gingiva but may also develop on the lip, tongue, oral mucosa and palate. When a large PT develops, it can interfere with mastication, speech, maintenance of oral hygiene and can be aesthetically disfiguring. The treatment of PTs depends upon the size of the lesion; smaller lesions can regress after parturition however large lesions need to be surgically removed. Conventional surgical techniques have the disadvantage of more bleeding from the surgical site and delay in healing of the scar tissue. The diode laser is a relatively new alternative to conventional surgical technique in intra-oral areas with the added advantage of bloodless procedures and rapid healing.
Case report: The purpose of the present study is to highlight the management of a PT in a 25-year-old female using a diode laser delivering a painless, bloodless procedure with rapid postoperative healing.
Conclusions: Diode laser excision of a persistent pregnancy tumour in a postpartum patient was safe and effective with minimal bleeding, good coagulation, and good wound healing. Among other lasers, the diode laser can therefore be considered for excisional treatment of persistent PTs.
Keywords: Pregnancy tumour, Granuloma gravidum, angiogranuloma, diode laser
Introduction
Pregnancy tumours (PTs) are a non-neoplastic, reactive, inflammatory conditional gingival enlargement which occurs during pregnancy in the oral cavity. Pts usually appear after the 3rd month of pregnancy but may also occur earlier 1). The reported incidence of PTs is 1.8 to 5% 2). They are associated with erythema, oedema with gingival overgrowth and an increased tendency for bleeding. The growth may be extensive and can interfere with performance of functions like mastication, speech and maintenance of oral hygiene, and may also be of aesthetical concern to the patient. This lesion usually appears on the gingiva especially on the anterior maxillary gingiva but may appear on the tongue, lip, palate and oral mucosa. The lesion classically occurs in the region of gingival inflammation where plaque and calculus are present. In most of the cases PTs regress completely and spontaneously after delivery. But if PTs persist, they may be quite painful and hence hamper normal functioning of the oral cavity. In such cases, they should be completely excised along with removal of any aetiological factors. Various treatment modalities have been documented for the treatment of this lesion which include surgical intervention with the scalpel, pulsed laser surgery, cryosurgery, radiosurgery and intralesional injection of sodium tetradecyl sulphate, ethanol or corticosteroids 3). However, excision with the laser has been reported relatively infrequently. This report presents a case of a pregnancy tumour in a patient reported postpartum, which was excised with a soft tissue diode laser.
Case report
A 25-year old female patient reported one month post-partum with the complaint of a gingival overgrowth on the lingual aspect of the lower left anterior region. She had noted the growth 6 months previously (i.e., 4 months post-conception), which had gradually increased in size. This overgrowth was associated with bleeding due to which the performance of the patient's normal functions were affected. She presented with no other signs of systemic or extraoral abnormality. Intraoral examination revealed a gingival overgrowth measuring approximately 4x4x5 cm presenting lingually, and extending from the lower left incisor to the canine region [Figure 1]. It was a discrete, pyramid shaped, pedunculated mass protruding from the interdental lingual gingival tissue in relation to the left mandibular canine. The lesion was magenta coloured, semi-firm in consistency and non-tender on palpation. Dental calculus and soft deposits were present on the teeth beneath the lesion. The growth was painless but creating problem during speech and mastication due to bleeding on slight irritation. Radiographic examination (intraoral periapical radiograph and orthopantomogram) did not reveal any bony involvement. Based on the patient's history, clinical sign and symptoms, a provisional diagnosis of pregnancy tumor was reached. As the overgrowth had not regressed postpartum and posed significant clinical problems, it was decided to completely excise the lesion [Figures 2 and 3]. After taking informed consent from the patient, the treatment plan was made to excise the lesion using the diode laser. Povidone iodine was applied at the incision site as an antiseptic agent and topical lidocaine (2%) gel was used for surface anaesthesia. A 940 nm diode laser was used for the procedure, with an output power of 2 W in the pulsed mode with a single use 300 µm, 4 mm long fibre tip. Postoperative instructions were given to the patient which included rinsing with 10 mL of chlorhexidine gluconate 0.2% mouthwash twice daily for 1 week. No anti-inflammatory agents or antibiotics were prescribed since neither pain nor infection was expected. The excised tissue was sent for histopathological examination.
Figure 1:
Pre-treatment photograph showing the lesion
Figure 2:
Excised tissue
Figure 3:
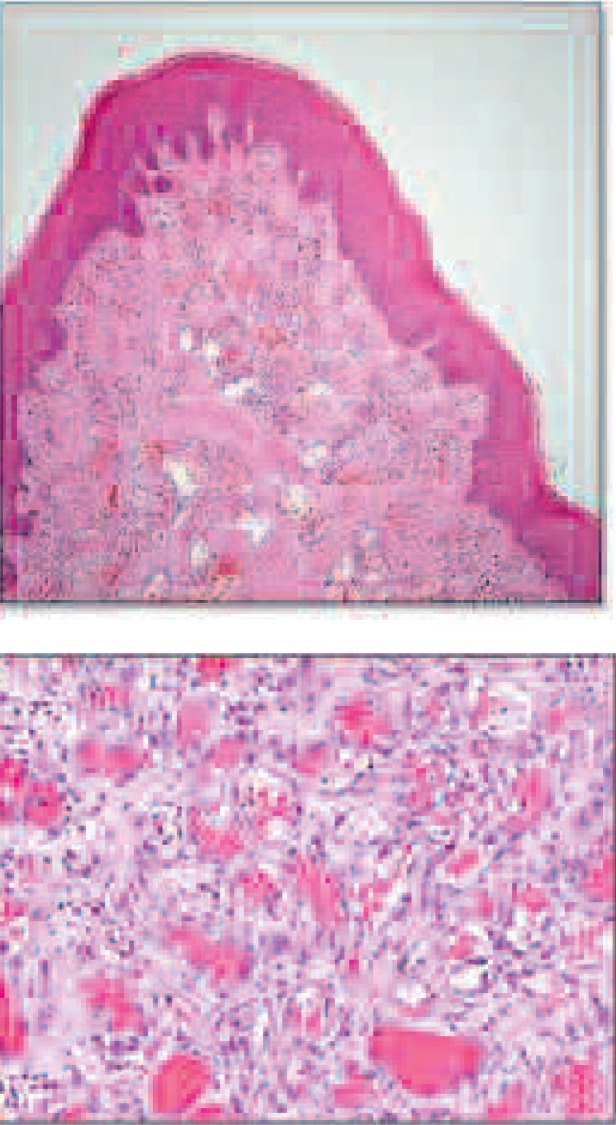
Histopathological findings
Results
Diode laser excision of the PT was successful, with minimal pain and minimal bleeding.
Histopathological examination
The hematoxylin & Eosin [Figure 3] stained sections showed stratified squamous surface epithelium. The connective tissue stroma was composed of loosely arranged collagen fibre bundles, interspersed with proliferating plump & spindle- to oval-shaped fibroblasts, and moderate chronic inflammatory cell infiltrate in the form of lymphocytes and plasma cells with many small and large proliferating endothelium-lined blood vessels containing red blood cells (RBCs) Based on a clinico-pathological correlation, a final diagnosis of PT was reached.
At a 3-day recall visit, healing was found to be satisfactory with no fresh complaints from the patient, who was motivated to maintain oral hygiene. The patient was recalled once more after 7 days for complete oral prophylaxis [Figure 5]. The healing was found to be complete with improved gingival contours and clinically visible epithelium over the surgical site.
Figure 5:
Seven days post-operative (Note the tissue healing and improved gingival contours)
Discussion
Pregnancy Tumours (also known as Granuloma gravidum, angiogranuloma, pregnancy epulis and florid granulation tissue) are a type of pyogenic granuloma considered to be a non-neoplastic, reactive gingival overgrowth occurring due to the influence of female sex hormones. Pinard and Pinard in 1877 recorded the first case of pregnancy tumour but the lesion was first described in 1897 by two French surgeons Poncet and Dor who then considered it to be a fungal infection 4, 5). The lesion is classified under the broad terminology of conditional inflammatory gingival enlargement because it is modified by the patient's systemic condition i.e., pregnancy-induced hormonal changes which influence the gingival response to dental plaque. PTs usually develop after the end of the first trimester of pregnancy but may occur earlier with a tendency to bleed associated with difficulty in chewing food 6). The reported prevalence is in the range of 5% in pregnant females 7). Various aetiological mechanisms have been postulated in the causation of PTs. In spite of numerous postulated mechanisms, it is generally agreed that hormonal imbalance during pregnancy heightens the organism's response to irritation 8). One of the mechanisms suggested is the change in the structure and function of the blood and lymph microvasculature of the skin and mucosa which in turn occurs due to hormonal changes associated with pregnancy 9). Increased chronic tissue reaction due to the immunosuppressant effect of progesterone on the gingival tissue resulting in exaggerated appearance of the inflamed tissues 10) has been postulated as another aetiological mechanism in the formation of PTs. The role of hormones in the causation of PTs has been contradicted by Nichols et al (1992) 11) who stated that the periodontium lacks steroid hormone receptors and hence formation of PTs is independent of estrogen or progesterone.
Figure 4:
Immediate post-operative photograph of the site (Note the soft tissue charring and underlying tooth with calculus attached)
Numerous treatment modalities for the management of this lesion have been suggested; however, choosing an appropriate technique may be difficult when the lesion occurs in an abnormal area or is large 3), 5). In many cases shrinkage of the small lesions may occur spontaneously after parturition and may not require surgery 12). In the present case, excision was planned because of the large size of the lesion and its failure to spontaneously regress one month post-partum. A diode laser operating in the near-infrared was used for excision because of lesser bleeding and better coagulation characteristics 13). Also, laser excision is considered to be well tolerated by the patients 14). Another factor to be highlighted is the prevention of PT formation during pregnancy. Regular brushing of the teeth using soft tooth brushes and dental floss coupled with routine dental check-ups during pregnancy are essential to prevent accumulation of plaque which in turn is an aetiological factor associated with the development of PTs
Conclusions
Near-infrared diode laser excision of a large and persistent pregnancy tumour in a postpartum patient was safe and effective with minimal bleeding, good coagulation, and good wound healing. Among other lasers which have been reported for this procedure, the diode laser can therefore be considered as a useful tool for excisional treatment of persistent PTs.
References
- 1: Newman MG, Takie HH, Klokkevold PR, Carranza's clinical periodontology 10th ed Saunders; 2007, 536. [Google Scholar]
- 2: Maier AW, Orban B: Gingivitis in pregnancy, Oral surg 1949;2:334. [DOI] [PubMed] [Google Scholar]
- 3: Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci 2006; 48:167. [DOI] [PubMed] [Google Scholar]
- 4: Pinard A, Pinard D: Treatment of the gingivitis of puerperal women. Dental Cosmos 1877;19:327. [Google Scholar]
- 5: Poncet A, Dor L. Botryomycose humaine. Rev Chir 1897;18:996. [Google Scholar]
- 6: Tumini V, Di Placido G, D'Archivio D, Del Giglio Matarazzo A. Hyperplastic gingival lesions in pregnancy (I). Epidemiology, pathology and clinical aspects. Minerva Stomatol 1998;47:159. [PubMed] [Google Scholar]
- 7: Sills ES, Zegarelli DJ, Hoschander MM, Strider WE. Clinical diagnosis and management of hormonally responsive oral pregnancy tumor (pyogenic granuloma). J Reprod Med 1996;41:467. [PubMed] [Google Scholar]
- 8: Eversole LR. Clinical outline of oral pathology: diagnosis and treatment 3rd ed, BC Decker, Hamilton: 2002;113. [Google Scholar]
- 9: Henry F, Quatresooz P, Valverde-Lopez JC, Pierard GE. Blood vessel changes during pregnancy: a review. AmJ Clin Dermatol 2006;7:65. [DOI] [PubMed] [Google Scholar]
- 10: Ojanotko-Harri AO, Hurttia HM, Sewon LA. Altered tissue metabolism of progesterone in pregnancy gingivitis and granuloma. J Clin Periodontol 1991;18:262. [DOI] [PubMed] [Google Scholar]
- 11: Nichols GE, Gaffey MJ, Mills SE, Weiss LM. Lobular capillary hemangioma. An immunohistochemical study including steroid hormone receptor status. AmJ Clin Pathol 1992;97:770. [DOI] [PubMed] [Google Scholar]
- 12: Bouquo JE, Nika H. Lesions of the oral cavity. In Diagnostic surgical pathology of the head and neck, Gnepp DR. ed, WB Saunders, Philadelphia: 2001:141. [Google Scholar]
- 13: Powell JL, Bailey CL, Coopland AT, Otis CN, Frank JL, Meyer I. Nd:YAG laser excision of a giant gingival pyogenic granuloma of pregnancy. Laser Surg Med 1994;14:178. [DOI] [PubMed] [Google Scholar]
- 14: White JM, Chaudhry SI, Kudler JJ, Sekandari N, Schoelch ML, Silverman S., Jr. Nd:YAG and CO2 laser therapy of oral mucosal lesions. J Clin Laser Med Surg 1998;16:299. [DOI] [PubMed] [Google Scholar]