Abstract
Objectives:
Treating complex regional pain syndrome (CRPS) is difficult because it still does not have a recommended therapy. A 29-year-old man was diagnosed with CRPS after surgery on his 4th and 5th left toes 7 years ago. Though he had undergone diverse pain treatment, the symptoms persisted, so he visited Dunsan Korean Medicine Hospital of Daejeon University. This case report presents results on the effect of bee venom pharmacopuncture in treating patient with CRPS.
Methods:
Bee venom pharmacopuncture (BVP), 0.15 to 0.4 mL dosage, was administered at GB43. The treatment was applied each week for a total 14 times. The symptoms were evaluated using a numeric rating scale (NRS) and the dosage of pain medicine.
Results:
On the first visit, he was taking an anticonvulsant, a trycyclic antidepressant, and an analgesic. On the NRS the worst pain in the toes received a score of 8. He also complained of severe pain and hypersensitivity when the 4th and the 5th toes were touched just slightly. Other complaint included dyspepsia, rash, and depression. After treatment, on the NRS, the score for toe pain was 0, and he no longer needed to take pain medication. During the 4-months follow-up period, he has remained without pain; neither have additional symptoms appeared nor adverse events occurred.
Conclusion:
BVP may have potential benefits for treating patients with CRPS.
Keywords: bee venom, complex regional pain syndrome, pharmacopuncture, reflex sympathetic dystrophy
1. Introduction
Complex regional pain syndrome (CRPS) is a neuropathic pain disease, which is the name now given to group of conditions previously described as ‘reflex sympathetic dystrophy (RSD)’, ‘Causalgia’, ‘Algodystrophy’, ‘Sudeck’s atrophy’. This chronic pain syndrome appears after big and small tissue damage, such as a sprain, a fracture, neurologic damage, spinal cord injury, cerebral infarction and myocardial infarction. These conditions share a number of clinical features, including spontaneous pain that is mostly on the limbs, associated allodynia, hyperalgesia, autonomic changes, trophic changes, and functional loss [1].
The diagnosis of CRPS had been based on the criteria of the International Association for the Study of Pain published in 1994. However, due to the lack of specificity and accuracy of diagnosis, the criteria, as revised in 2004, are used instead [2].
The primary medications for treating CRPS are anti-inflammatory drugs, anticonvulsants, antidepressants, and steroids [3]. For additional pain control, nerve blocks, such as regional nerve blocks and sympathecotomies, and interventional treatment, such as spinal cord stimulation, are used together [4]. Though various remedies exist, the therapeutic responses to traditional treatments are relatively poor, and because of the complicated symptoms, a diverse approach is necessary [5].
Besides the traditional therapy, patients with CRPS recently treated in China were reported to have been improved by 80%, and that improvement continued for more than 20 months [6]. Also, chronic CRPS patients treated with acupuncture have been reported to show reduced pain and depression and enhanced quality of life [7]. In additional to international studies on acupuncture, cases using anti-inflammatory pharmacopuncture [8], Harpagophytum radix. pharmacopuncture [9], and placental extracts [10] have been reported in Korea. In this research study, we describe the case of a patient with CRPS who responded to bee venom pharmacopuncture (BVP) with impressive and sustained results.
2. Case report
This patients was a 29-year-old male with a history of congenital polysyndactylia of the 4th and the 5th toes. He had undergone a polydactyly resection, separation of syndactyly, and split thickness skin-graft on March 14, 2006 and surgery on the necrosis site on April 20, 2006. His mother had a history of hypertension.
After joining the army in 2006 and complaining of difficulty with military life because of the congenital polysyndactylia, he underwent resection, separation of syndactyly, on his 4th and 5th toes. After the surgery he reported pain and paresthesia on those toes and was diagnosed with CRPS; however, according to the operation notes, no neurologic damage had occurred. Afterward the diagnosis, he was treated with anti-inflammatory drugs, anticonvulsants and antidepressants and had undergone nerve blocks 10 times before being examined at our clinic. When the pain worsened, he was prescribed a narcotic analgesic, in spite of which he complained of pain of more than 5 on the numeric rating scale (NRS), depression, and anxiety. Although he had received treatments such as medications and nerve blocks, the pain had not decreased under a NRS score of 5, even reaching a NRS score of 8 on occasion. Also, long-term therapy and medication had led to depression and anxiety. On the first visit, he was taking an anticonvulsant (Gabapentin) 2700 mg/day, a trycyclic antidepressant (amitriptyline hydrochloride) 10 mg/day, and an analgesic (tramadol hydrochloride) 50 mg as required. At the first examination in our clinic, he complained of severe pain and hypersensitivity when his 4th and 5th toes were touched just slightly and of dyspepsia, rash, and depression.
During the treatment period at our clinic, which ran from January 2, 2014, to April 10, 2014, the patient underwent 14 treatments.
The patient first visited Dunsan Korean Medicine Hospital on December 14, 2013, and started receiving injection of sweet BVP from January 2, 2014. The skin test showed a negative reaction. The acupuncture point was GB43, near the tender point, and the dosage of bee venom was gradually increased from 0.15 to 0.4 mL. The initial plan was once a week for 10 weeks, but as the treatment progressed, we added the treatment period was extended to 14 weeks.
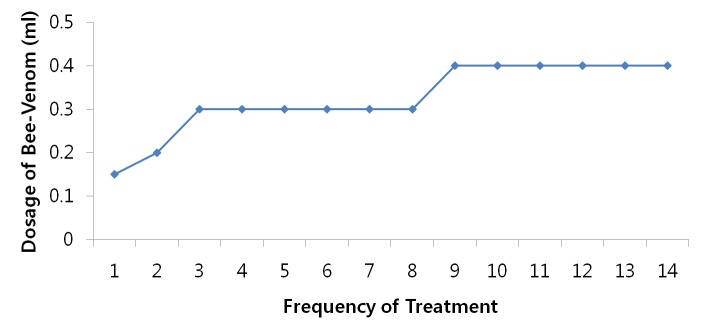
At the first treatment, the dosage of the BVP was 0.15 mL, at the second treatment, it was 0.2 mL, and at the third treatment, it was 0.3 mL. As the dosage of 0.3 mL induced no side effect, the dosage was kept at 0.3 mL until the 8th treatment. For the remaining treatment after the 8th , it was increased to 0.4 mL (Fig 1).
Fig. 1. Dosage of bee venom.
No side effects appeared after the first injection. The irritation decreased, but no change in the NRS score was noted. On the 2nd day of treatment, the patient reduced Gabapentin from 2700 to 900 mg/day, though the NRS score still persisted. On the 4th day of treatment, the average NRS score declined from 5 to 3, and the sharpest pain appeared just once or twice a week, with rare sudden pain. On the 5th day of treatment, the sharpest pain fell from NRS 7 to 3. After that treatment, the patient experienced pain to a regular degree without sudden severe pain. After the 7th day of treatment, he reduced the dosage of Gabapentin from 900 to 600 mg/day for 2 weeks, but upon feeling discomfort, increased it to 900 mg/day again. On the 10th day of treatment, he reduced the dosage to 300 mg/day and experienced no increase in pain after that. On the 11th day of treatment, he discontinued taking amitriptyline hydrochloride. While insomnia and anxiety arose without the trycyclic antidepressant, he took additional herbal medicine, Ondam-tanggami (Wendan-tangjiawei). On the 13th day of treatment, he stopped taking all western medicines. After the 14th treatment, the last injection, the average NRS score was 1 to 2. On the NRS, the patient rated his pain as 0 after the 2-months and the 4-months follow-ups (May 30 and of July 31, 2014). No additional symptoms have occurred (Table 1), (Fig 2).
Table. 1. Date of treatment and dosage of medicine, and adverse events.
| Treatment | Date | Gabapentin (mg/day) |
Amitriptyline (mg/day) |
Other Medicine | Adverse Events |
|---|---|---|---|---|---|
| 1st | 1/2 | 2700 | 10 | None | None |
| 2nd | 1/9 | 2700 | 10 | None | None |
| 3rd | 1/16 | 900 | 10 | None | None |
| 4th | 1/23 | 900 | 10 | None | None |
| 5th | 1/29 | 900 | 10 | None | None |
| 6th | 2/8 | 900 | 10 | None | None |
| 7th | 2/15 | 600 | 10 | None | None |
| 8th | 2/22 | 600 | 10 | None | None |
| 9th | 2/28 | 900 | 10 | None | None |
| 10th | 3/7 | 600 | 10 | None | None |
| Observation | 3/14 | 300 | 10 | None | None |
| 11th | 3/21 | 300 | 10 | None | None |
| Observation | 3/25 | 300 | 10 | Ondam-tanggami | Insomnia and Anxiety (After Stopping Amitriptyline) |
| 12th | 3/27 | 300 | 0 | Ondam-tanggami | Insomnia and Anxiety |
| 13th | 4/3 | 300 | 0 | None | None |
| 14th | 4/10 | 0 | 0 | None | None |
| Observation | 4/24 | 0 | 0 | None | None |
| Observation | 5/30 | 0 | 0 | None | None |
| Observation | 7/31 | 0 | 0 | None | None |
Fig. 2. Variations in pain during the treatment period.
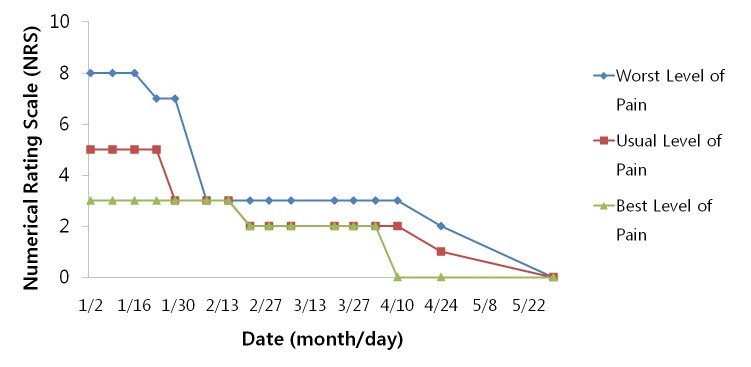
During the 14 treatments, no side effects due to bee venom were observed; however, insomnia and anxiety developed while reducing western medicines. Especially, at the 11th treatment, the patient noted insomnia and anxiety after discontinuing amitriptyline hydrochloride. He took herbal medicine for 2 weeks, after which those symptoms were relieved, with no further occurrence. After the 14th treatments, the pain had disappeared at the surgical site, and the sensation in the 4th and the 5th left toes was 80% that in the 4th and the 5th right toes (Table 1).
3. Discussion
We administered 0.15 mL of sweet BVP initially, but because the duration of the disease had been long and the pain control had been difficult, the dosage was increased gradually to 0.4 mL (Fig 1) We checked for any side effects while increasing the dosage. Although the patient felt stiffness at the injection point on the foot, a dosage under 0.3 mL was considered to be appropriate.
The initial plan was for one injection to be given each week for 10 weeks, which was based on the experience of the therapist. After 10 treatments and 2 weeks of observation, although his pain level on the NRS was 2 and he felt no inconvenience in daily living, we decided to perform four additional injections until the symptoms disappeared.
On the 10th day of treatment, the pain had decreased to an average NRS score of 2, and on the 13th day of treatment, the patient noted pain relief without any medication. Especially, on the 14th day of treatment, of the last treatment, pain had disappeared, and just a little paresthesia was noted. Neither recurrence nor additional symptoms were observed during the 4-month follow-up.
We could relieve the symptoms with 10 treatments, but they had completely disappeared after the four additional treatments. Thus, we recommend that the treatment plan be based on 10 treatments, with the possibility of about 5 additional treatments, depending on the state of the patient.
The patient additionally complained of insomnia and anxiety during the course of treatment, the 11thday. He had undergone depression because of persistent pain and failure to control the pain associated with CRPS. As the insomnia and anxiety were thought to be symptoms caused by discontinuing the nervous system drugs which he had taken for the last 7 years, we administered herbal medicine. He reported that it irritated him, but not strongly, and the insomnia and anxiety disappeared after 2 weeks. A period for discontinuing medication that has been taken for a long time, rather herbal medicine, seems to be needed.
No new systemic symptoms appeared following the treatment, and no additional medication was prescribed, except for the herbal medicine Ondam-tanggami (Wendan-tangjiawei) used for insomnia and anxiety and the intermittent herbal medicine Sojukgunbihuan (xiaojijianpiwan) used for dyspepsia.
Due to the fact that there are few distinct treatments for CRPS, many studies on anti-inflammatory drugs, nerve blocks, vitamin therapy, and acupuncture for treating patients with CRPS [11, 12]. Among those, a study on bee venom therapy is now ongoing, and it has been proven with rodents that bee venom alleviates thermal hyperalgesia [13]. Also, a chemotherapy-induced peripheral neuropathic pain model [14] and clinical research [15, 16] have already established the effect of bee venom therapy. Although these studies are not related to CRPS, they do show the effectiveness of using bee venom to treat neuropathic disease. Thus, using bee venom therapy to treat patients with CRPS should hold promise.
In the present case, bee venom therapy administered to a patient who had been suffering from CRPS with failure to control its pain for almost 7 years proved to be effective. However, the exact mechanism and therapy methods are beyond the limits of this case report. We particularly suggest further studies on the required length of the treatment and the dosage for bee venom therapy, clinical observations of bee venom therapy, and studies on the mechanisms of bee venom therapy applied to neuropathy.
Footnotes
Conflicts of interest The authors declare that there are no conflict of interest.
References
- 1.Harden RN, Oaklander AL, Burton AW, Perez RS, Richardson K, Swan M et al. Complex regional pain syndrome: practical diagnostic and treatment guidelines, 4th edition. Pain Med. 2013;14(2):180–229. doi: 10.1111/pme.12033. [DOI] [PubMed] [Google Scholar]
- 2.Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007;8(4):326–331. doi: 10.1111/j.1526-4637.2006.00169.x. [DOI] [PubMed] [Google Scholar]
- 3.Rowbotham MC. Pharmacologic management of complex regional pain syndrome. Clin J Pain. 2006;22(5):425–429. doi: 10.1097/01.ajp.0000194281.74379.01. [DOI] [PubMed] [Google Scholar]
- 4.Van Buyten, JP, Smet I, Liem L, Russo M, Huygen F. Stimulation of dorsal root ganglia for the management of complex regional pain syndrome: a prospective case series. Pain Pract. 2014:12170. doi: 10.1111/papr.12170. [DOI] [PubMed] [Google Scholar]
- 5.Borchers AT, Gershwin ME. Complex regional pain syndrome: a comprehensive and critical review. Autoimmun Rev. 2014;13(3):242–265. doi: 10.1016/j.autrev.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Hommer DH. Chinese scalp acupuncture relieves pain and restores function in complex regional pain syndrome. Mil Med. 2012;177(10):1231–1234. doi: 10.7205/MILMED-D-12-00193. [DOI] [PubMed] [Google Scholar]
- 7.Sprague M, Chang JC. Integrative approach focusing on acupuncture in the treatment of chronic complex regional pain syndrome. J Altern Complement Med. 2011;17(1):67–70. doi: 10.1089/acm.2010.0088. [DOI] [PubMed] [Google Scholar]
- 8.Lee EJ, Yoon IJ. [The clinical observation of 1 case of the complex regional pain syndrome] J of the Institute of Orient Med of Daejeon Univ. 2009;18(1):109–116. Korean. [Google Scholar]
- 9.Chung JH, Yun YU, Cheong SH, Kim SW, Choi HS, Shin DJ et al. [The clinical observation of 1 case of type 1 complex regional pain syndrome treated with korean medicine treatment and harpagophytum radix pharmacopuncture] The Journal of Korea CHUNA Manual Medicine for spine & nerves. 2013;8(1):63–73. Korean. [Google Scholar]
- 10.Cho TH, Park KM. [Effect of placental extract on immobilization of shoulder joint in a complex regional pain syndrome patient] The Acupuncture. 2012;29(4):93–97. Korean. [Google Scholar]
- 11.Tran de, QH, Duong S, Bertini P, Finlayson RJ. Treatment of complex regional pain syndrome: a review of the evidence. Can J Anaesth. 2010;57(2):149–166. doi: 10.1007/s12630-009-9237-0. [DOI] [PubMed] [Google Scholar]
- 12.Shibuya N, Humphers JM, Agarwal MR, Jupiter DC. Efficacy and safety of high-dose vitamin C on complex regional pain syndrome in extremity trauma and surgery: systematic review and meta-analysis. J Foot Ankle Surg. 2013;52(1):62–66. doi: 10.1053/j.jfas.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Roh DH, Kwon YB, Kim HW, Ham TW, Yoon SY, Kang SY et al. Acupoint stimulation with diluted bee venom (apipuncture) alleviates thermal hyperalgesia in a rodent neuropathic pain model: involvement of spinal alpha 2-adrenoceptors. J Pain. 2004;5(6):297–303. doi: 10.1016/j.jpain.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Lim BS, Moon HJ, Li DX, Gil M, Min JK, Lee G et al. Effect of bee venom acupuncture on oxaliplatin-induced cold allodynia in rats. Evid Based Complement Alternat Med. 2013:369324. doi: 10.1155/2013/369324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park JW, Jeon JH, Yoon JW, Jung TY, Kwon KR, Cho CK et al. Effects of sweet bee venom pharmacopuncture treatment for chemotherapy-induced peripheral neuropathy: a case series. Integr Cancer Ther. 2012;11(2):166–171. doi: 10.1177/1534735411413265. [DOI] [PubMed] [Google Scholar]
- 16.Yoon JW, Jeon JH, Lee YW, Cho CK, Kwon KR, Shin JE et al. Sweet bee venom pharmacopuncture for chemotherapy- induced peripheral neuropathy. J Acupunct Meridian Stud. 2012;5(4):156–165. doi: 10.1016/j.jams.2012.05.003. [DOI] [PubMed] [Google Scholar]


