Abstract
The pleural cavity is the potential space between the two pleurae (visceral and parietal) of the lungs. The pleurae are serous membranes which fold back onto themselves to form a two-layered membranous structure. The thin space between the two pleural layers is known as the pleural cavity and normally contains a small amount of pleural fluid. There are two layers; the outer pleura (parietal pleura) is attached to the chest wall and the inner pleura (visceral pleura) covers the lungs and adjoining structures, via blood vessels, bronchi and nerves. The parietal pleurae are highly sensitive to pain, while the visceral pleura are not, due to its lack of sensory innervation. In the current review we will present the anatomy of the pleural space.
Keywords: Pneumothorax, anatomy, pleural space
The pleural cavity is the potential space between the two pleurae (visceral-parietal) of the lungs. The pleura is a serous membrane which folds back onto itself to form a two-layered membrane structure. The thin space is known as the pleural cavity and contains a small amount of pleural fluid (few milliliters in a normal human). The outer pleura is attached to the chest wall (1-9).
The pleural cavity aids optimal functioning of the lugs during breathing. It transmits movements of the chest wall to the lungs, particularly during heavy breathing. The closely approved chest wall transmits pressures to the visceral pleural surface and hence to the lung (10-19).
In human, there is no anatomical connection between the pleural cavities. The visceral pleura receives its blood supply from the bronchial circulation and the parietal pleura receives its blood supply from the intercostal arteries. Only in cases of pneumonothorax (tension-simultaneous) may collapse the contralateral parenchyma and blood vessels. Normally visceral pleura glides on parietal without sound or pain, but when the pleura are in action sounds can be auscultated. If fluid then distends cavity, the sounds disappear and the lung gradually the heart and mediastinum being displaced towards the lung. Air the cavity, rupture of the lung as the elastic tissue of the lung recoils. The pleura crosses the rib at the region is above the reflexion.
The thoracic structures (inlet) consist of two groups. Those in the median plane and those on each side closely related to the cervical parts of pleurae and lungs.
Near the midline, the lowest parts of the sternohyoid muscles enter the thorax, thymic vestiges and inferior thyroid veins. Posteriorly, trachea and oesophagus, with the recurrent laryngeal nerves. Anterior to the vertebral column are the prevertebral longus colli muscles (20-29);
On each side, the upper part of the pleura and pulmonary apex occupy the inlet. Between the pleura and neck of the first rib are the sympathetic trunk, superior intercostal artery and ventral ramus of the first thoracic nerve. The internal thoracic artery enters the thorax between pleura and first costal cartilage;
On the right, the brachiocephalic artery leaves the thorax between the trachea and pleura. The vagus nerve is between the pleura and brachiocephalic artery at the inlet;
On the left, the left common carotid and subclavian arteries leave the thorax between the pleura and trachea. The left phrenic nerve crosses the internal thoracic artery at a higher level, because it is between the left brachiocephalic vein and common carotid arteries.
The thoracic outlet is wider transversely and slopes down, so the vertical extend of the cavity is longer. The diaphragm closes the opening and forms a convex floor for the cavity. Centrally, it is flatter. The diaphragm slopes down to the costal and vertebral attachments, so the thoracic wall narrows rapidly inferiorly (29-39).
The thoracic cavity is divided by the mediastinum. The heart is in the mediastinum, enclosed by the pericardium. The lungs occupy the left-right regions and the pleura lines the corresponding half of the thorax and forms the lateral mediastinal boundary.
The superior part extends from the thoracic inlet passing through the lower edge of manubrium sterni. The inferior part is subdivided into an anterior part of the pericardium. The pericardium contains the heart and juxtacardiac parts. It is posterior to corpus sterni and anterior to the 5-8 thoracic vertebrae. It consists of two opposed surfaces of serous membrane (fibrous pericardium-serous pericardium). The fibrous pericardium is compacted of collagenous fibrous tissue. The serous pericardium is a thin layer of flat mesothelial cells which blends with the fibrous pericardium and myocardial tissue.
The mediastinum is the partition between the lungs and includes the mediastinal pleura. It is commonly applied to the internal between the two pleural sacs, the sternum and the thoracic vertebral column extending to the diaphragm.
The superior mediastinum is lying between the manubrium sterni and the upper four thoracic vertebrae. It contains the ends of the sternohyoid, colli muscles, left common carotid, the brachiocephalic artery and the aortic arch (32,39-48).
The anterior mediastinum lying between the sternal body and pericardium. It contains loose areolar tissue, the sternopericardial ligaments, sometimes part of thymous gland and the mediastinal branches of the internal thoracic artery.
The middle mediastinum contains pericardium, ascending aorta, the terminal azygos vein, both pulmonary veins, the phrenic nerves and tracheal bifurcation.
The posterior mediastinum is bounded in front by the tracheal bifurcation, pericardium and the upper surface of diaphragm, behind by the vertebral column. It contains the thoracic aorta, the vagus, the azygos-hemiazygos vein and the thoracic duct.
Each lung is invested by a delicate serous membrane and the pleura, which is arranged in the investigated sac. A portion of the serous membrane dips into the fissures between its lobes—the pulmonary pleura. The rest of the membrane lines cover the diaphragm—the parietal pleura. The two layers are continuous with one another around and below the root of the lung—the pleural cavity. The right and left pleural sacs are entirely separate and they touch each other for a short distance in front, opposite the 2nd-3rd pieces of the sternum the interval between the two sacs—the mediastinum.
In the front of the chest, where the parietal pleura is reflected backward to the pericardium, the two pleural sacs are in contact. At the upper part of the chest they are separated by an angular interval. From this point the two pleurae descend in close contact to the level of the fourth costal cartilages. The inferior limit of the pleura is on a considerably lower level than the corresponding limit of the lung but does not extend to the attachment of the diaphragm. So, the thin inferior margin of the lung doesn’t extend as low as the line of the pleural reflection—the phrenicocostal sinus.
Between the two layers of pleura forms—the costomediastinal sinus.
The line along which the right pleura is reflected from the chess-wall to the diaphragm starts in front and runs behind the seventh costal cartilage. The reflection of the left pleura follows the ascending part of the sixth cartilage and it’s lower than the right side. The right sac is shorter, wider and reaches higher in the neck (Figures 1,2,3,4,5,6,7,8,9,10,11,12).
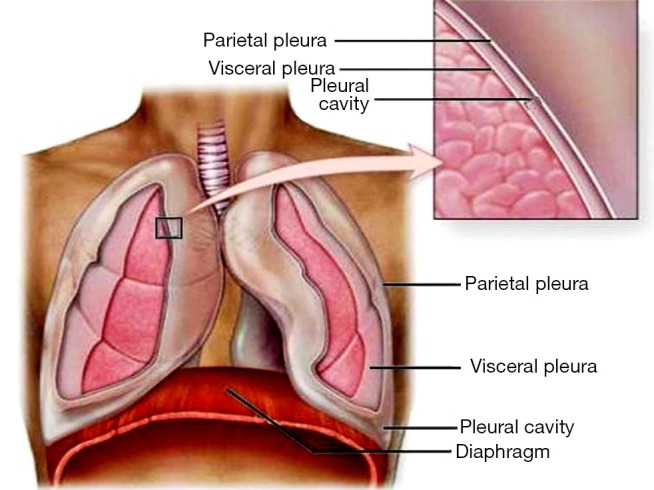
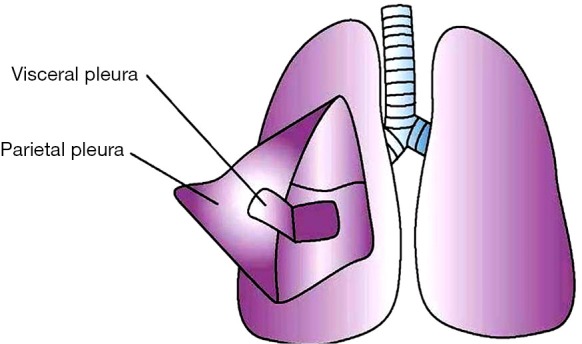
Figure 1.
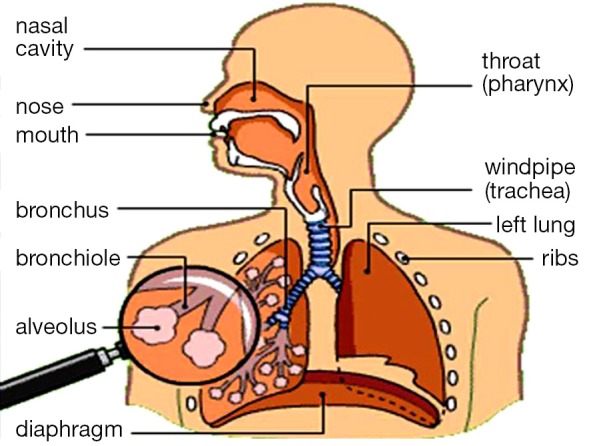
Anatomy of the respiratory system.
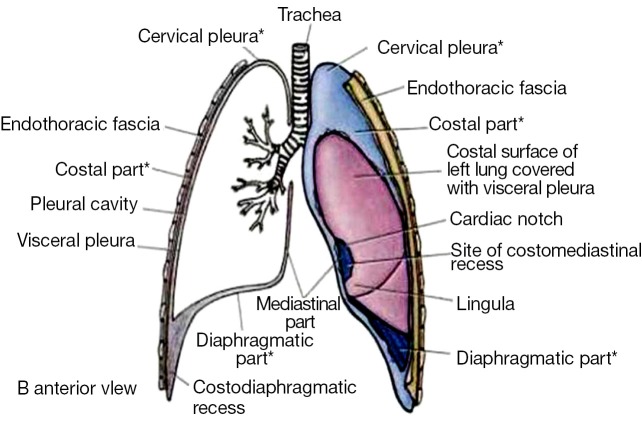
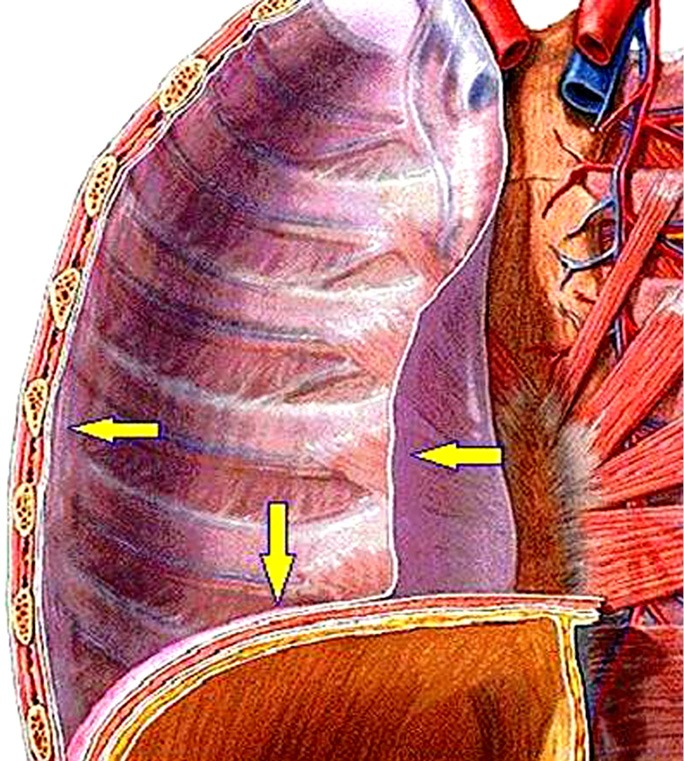
Figure 2.
Anatomy of the respiratory system within the thorax region.
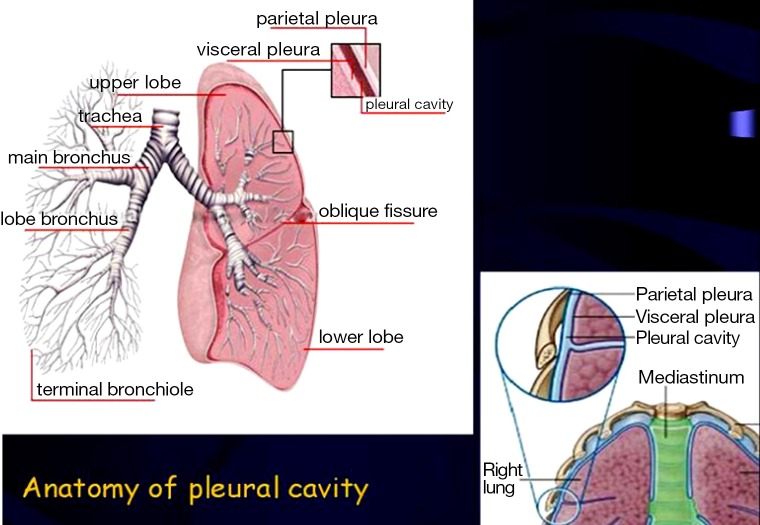
Figure 3.
Anatomy of the pleura cavity.
Figure 4.
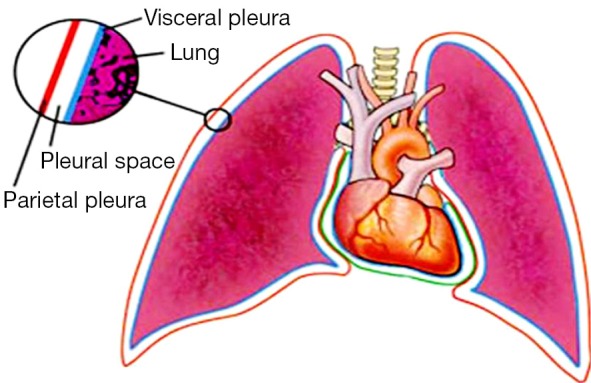
Two pleural layers continue with each other at root of the lung forming a closed potential cavity: pleural cavity.
Figure 5.
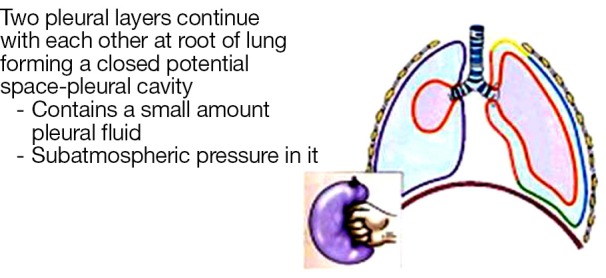
Anatomy of the pleura cavity (mechanism detail).
Figure 6.
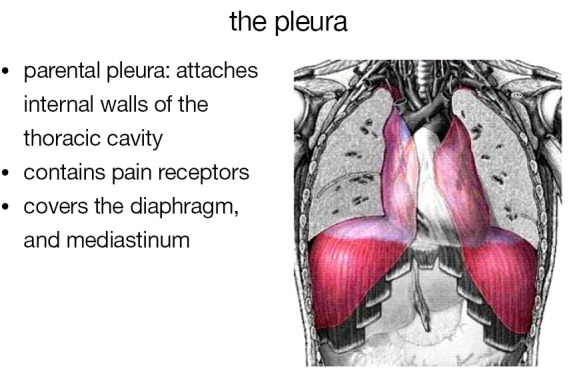
Anatomy of the pleura cavity (muscles).
Figure 7.
Anatomy of the pleura cavity (pleural layers).
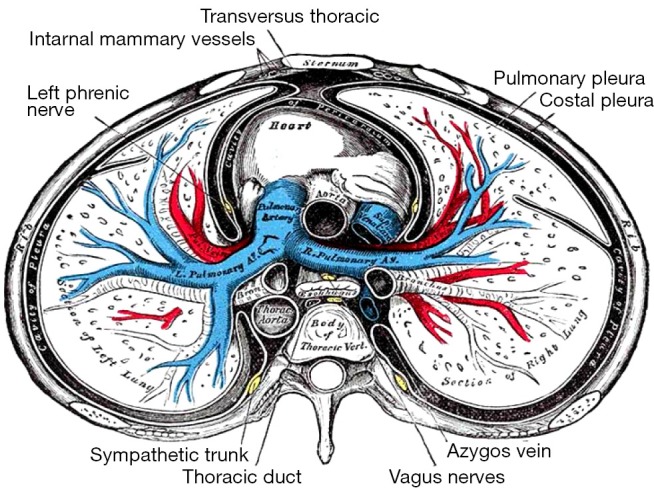
Figure 8.
Anatomy of the pleura cavity (respiratory system).
Figure 9.
The parietal pleura lines the thoracic wall and superior surface of the diaphragm. It continues around the heart forming the lateral walls of the mediastinum. The pleura extends over the surface of the lungs as the visceral pleura. The surface tension of the fluid in the pleural cavity secures the pleura together. They can slide from side to side but it is hard to separate them.
Figure 10.
Anatomy of pleural cavity-pleural recesses.
Figure 11.
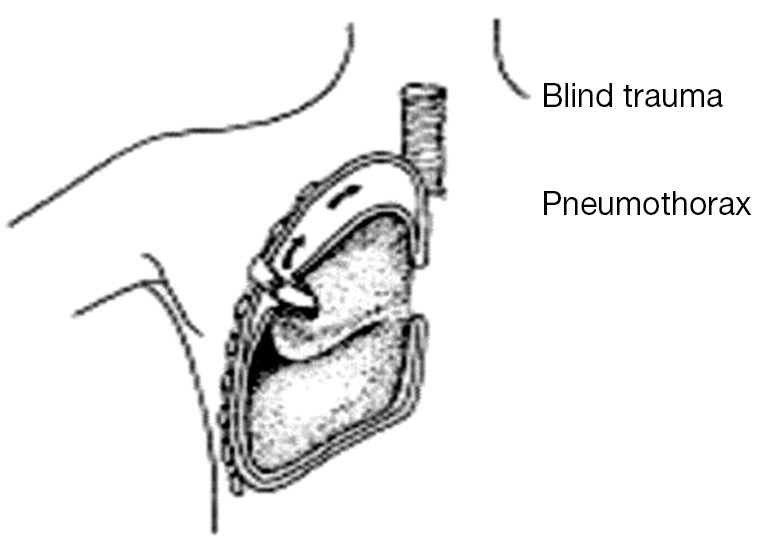
Types of pneumothorax.
Figure 12.
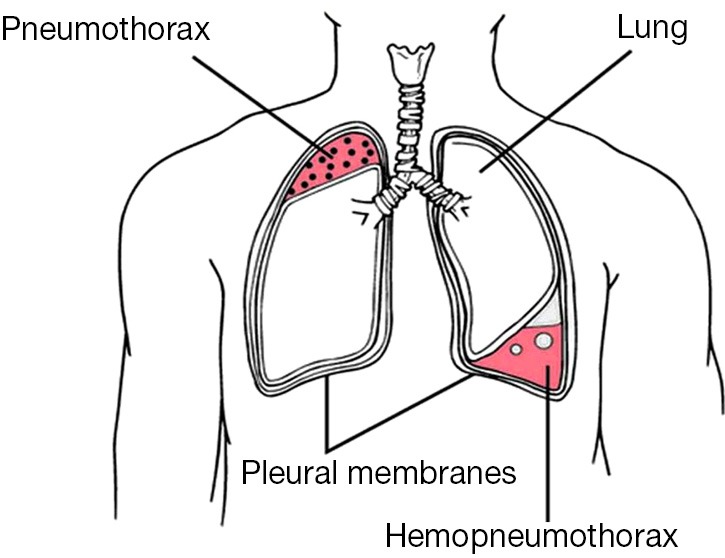
Pneumothorax.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Williams PL, Warwick R, Dyson M, et al. eds. Gray’s Anatomy. Edinburgh: Churchill Livingstone, 1995. [Google Scholar]
- 2.Murray IF, Nadel IA. eds. Textbook of Respiratory Medicine. Philadelphia: Saunders, 1988. [Google Scholar]
- 3.Wang NS. Anatomy and physiology of the pleural space. Clin Chest Med 1985;6:3-16. [PubMed] [Google Scholar]
- 4.Lee KF, Olak J. Anatomy and physiology of the pleural space. Chest Surg Clin N Am 1994;4:391-403. [PubMed] [Google Scholar]
- 5.Kioumis IP, Zarogoulidis K, Huang H, et al. Pneumothorax in cystic fibrosis. J Thorac Dis 2014;6:S480-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuhajda I, Zarogoulidis K, Kougioumtzi I, et al. Tube thoracostomy; chest tube implantation and follow up. J Thorac Dis 2014;6:S470-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manika K, Kioumis I, Zarogoulidis K, et al. Pneumothorax in sarcoidosis. J Thorac Dis 2014;6:S466-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuhajda I, Zarogoulidis K, Kougioumtzi I, et al. Penetrating trauma. J Thorac Dis 2014;6:S461-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Visouli AN, Zarogoulidis K, Kougioumtzi I, et al. Catamenial pneumothorax. J Thorac Dis 2014;6:S448-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang Y, Huang H, Li Q, et al. Transbronchial lung biopsy and pneumothorax. J Thorac Dis 2014;6:S443-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Terzi E, Zarogoulidis K, Kougioumtzi I, et al. Acute respiratory distress syndrome and pneumothorax. J Thorac Dis 2014;6:S435-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boskovic T, Stojanovic M, Stanic J, et al. Pneumothorax after transbronchial needle biopsy. J Thorac Dis 2014;6:S427-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li Z, Huang H, Li Q, et al. Pneumothorax: observation. J Thorac Dis 2014;6:S421-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang Y, Huang H, Li Q, et al. Approach of the treatment for pneumothorax. J Thorac Dis 2014;6:S416-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Browning RF, Parrish S, Sarkar S, et al. Bronchoscopic interventions for severe COPD. J Thorac Dis 2014;6:S407-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Machairiotis N, Kougioumtzi I, Dryllis G, et al. Laparoscopy induced pneumothorax. J Thorac Dis 2014;6:S404-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ouellette DR, Parrish S, Browning RF, et al. Unusual causes of pneumothorax. J Thorac Dis 2014;6:S392-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parrish S, Browning RF, Turner JF, Jr, et al. The role for medical thoracoscopy in pneumothorax. J Thorac Dis 2014;6:S383-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Terzi E, Zarogoulidis K, Kougioumtzi I, et al. Human immunodeficiency virus infection and pneumothorax. J Thorac Dis 2014;6:S377-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zarogoulidis P, Kioumis I, Pitsiou G, et al. Pneumothorax: from definition to diagnosis and treatment. J Thorac Dis 2014;6:S372-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsakiridis K, Mpakas A, Kesisis G, et al. Lung inflammatory response syndrome after cardiac-operations and treatment of lornoxicam. J Thorac Dis 2014;6Suppl 1:S78-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsakiridis K, Zarogoulidis P, Vretzkakis G, et al. Effect of lornoxicam in lung inflammatory response syndrome after operations for cardiac surgery with cardiopulmonary bypass. J Thorac Dis 2014;6Suppl 1:S7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Argiriou M, Kolokotron SM, Sakellaridis T, et al. Right heart failure post left ventricular assist device implantation. J Thorac Dis 2014;6Suppl 1:S52-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Madesis A, Tsakiridis K, Zarogoulidis P, et al. Review of mitral valve insufficiency: repair or replacement. J Thorac Dis 2014;6Suppl 1:S39-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siminelakis S, Kakourou A, Batistatou A, et al. Thirteen years follow-up of heart myxoma operated patients: what is the appropriate surgical technique? J Thorac Dis 2014;6Suppl 1:S32-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Foroulis CN, Kleontas A, Karatzopoulos A, et al. Early reoperation performed for the management of complications in patients undergoing general thoracic surgical procedures. J Thorac Dis 2014;6Suppl 1:S21-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nikolaos P, Vasilios L, Efstratios K, et al. Therapeutic modalities for Pancoast tumors. J Thorac Dis 2014;6Suppl 1:S180-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koutentakis M, Siminelakis S, Korantzopoulos P, et al. Surgical management of cardiac implantable electronic device infections. J Thorac Dis 2014;6Suppl 1:S173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spyratos D, Zarogoulidis P, Porpodis K, et al. Preoperative evaluation for lung cancer resection. J Thorac Dis 2014;6Suppl 1:S162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Porpodis K, Zarogoulidis P, Spyratos D, et al. Pneumothorax and asthma. J Thorac Dis 2014;6Suppl 1:S152-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Panagopoulos N, Leivaditis V, Koletsis E, et al. Pancoast tumors: characteristics and preoperative assessment. J Thorac Dis 2014;6Suppl 1:S108-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Visouli AN, Darwiche K, Mpakas A, et al. Catamenial pneumothorax: a rare entity? Report of 5 cases and review of the literature. J Thorac Dis 2012;4Suppl 1:17-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zarogoulidis P, Chatzaki E, Hohenforst-Schmidt W, et al. Management of malignant pleural effusion by suicide gene therapy in advanced stage lung cancer: a case series and literature review. Cancer Gene Ther 2012;19:593-600. [DOI] [PubMed] [Google Scholar]
- 34.Papaioannou M, Pitsiou G, Manika K, et al. COPD assessment test: a simple tool to evaluate disease severity and response to treatment. COPD 2014;11:489-95. [DOI] [PubMed] [Google Scholar]
- 35.Boskovic T, Stanic J, Pena-Karan S, et al. Pneumothorax after transthoracic needle biopsy of lung lesions under CT guidance. J Thorac Dis 2014;6Suppl 1:S99-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Papaiwannou A, Zarogoulidis P, Porpodis K, et al. Asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS): current literature review. J Thorac Dis 2014;6Suppl 1:S146-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zarogoulidis P, Porpodis K, Kioumis I, et al. Experimentation with inhaled bronchodilators and corticosteroids. Int J Pharm 2014;461:411-8. [DOI] [PubMed] [Google Scholar]
- 38.Bai C, Huang H, Yao X, et al. Application of flexible bronchoscopy in inhalation lung injury. Diagn Pathol 2013;8:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zarogoulidis P, Kioumis I, Porpodis K, et al. Clinical experimentation with aerosol antibiotics: current and future methods of administration. Drug Des Devel Ther 2013;7:1115-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zarogoulidis P, Pataka A, Terzi E, et al. Intensive care unit and lung cancer: when should we intubate? J Thorac Dis 2013;5Suppl 4:S407-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hohenforst-Schmidt W, Petermann A, Visouli A, et al. Successful application of extracorporeal membrane oxygenation due to pulmonary hemorrhage secondary to granulomatosis with polyangiitis. Drug Des Devel Ther 2013;7:627-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zarogoulidis P, Kontakiotis T, Tsakiridis K, et al. Difficult airway and difficult intubation in postintubation tracheal stenosis: a case report and literature review. Ther Clin Risk Manag 2012;8:279-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zarogoulidis P, Tsakiridis K, Kioumis I, et al. Cardiothoracic diseases: basic treatment. J Thorac Dis 2014;6Suppl 1:S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kolettas A, Grosomanidis V, Kolettas V, et al. Influence of apnoeic oxygenation in respiratory and circulatory system under general anaesthesia. J Thorac Dis 2014;6Suppl 1:S116-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Turner JF, Quan W, Zarogoulidis P, et al. A case of pulmonary infiltrates in a patient with colon carcinoma. Case Rep Oncol 2014;7:39-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Machairiotis N, Stylianaki A, Dryllis G, et al. Extrapelvic endometriosis: a rare entity or an under diagnosed condition? Diagn Pathol 2013;8:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tsakiridis K, Zarogoulidis P.An interview between a pulmonologist and a thoracic surgeon-Pleuroscopy: the reappearance of an old definition. J Thorac Dis 2013;5Suppl 4:S449-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang H, Li C, Zarogoulidis P, et al. Endometriosis of the lung: report of a case and literature review. Eur J Med Res 2013;18:13. [DOI] [PMC free article] [PubMed] [Google Scholar]