Introduction
Dr. Paul Zarogoulidis, MD, Ms.C, PhD, finished his medical studies in the Aristotle University of Thessaloniki, Greece. He continued his education as a pulmonary fellow in the Pulmonary Department of Democritus University of Thrace, Greece and finished his training as a pulmonary specialist in the Interventional Pulmonary Department, “Ruhrland” Clinic, University of Duisburg-Essen, Germany. His post graduate training includes fellowship with the Medical Oncology Department, Cristie Hospital, Manchester, UK and with the Interventional Pulmonary Department, “Ruhrland” Clinic, University of Duisburg-Essen, Germany. Currently he is a consultant in the Pulmonary Department, “G. Papanikolaou” General Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece. His interests apart from the daily activities of the department include research in the gene therapy field and novel drug, design, development and therapy. He is a member of EABIP, CABIP, WABIP, ASCO, IASLC, ERS, ISAM and ATS.
Dr. Paul Zarogoulidis is the Associate Editor of Journal of Thoracic Disease (JTD), editorial board member of Translational Lung Cancer Research (TLCR) and Annals of Translational Medicine (ATM).
On the 2014 Pan Hellenic Congress on Respiratory and Occupational Chest Diseases held in Thessaloniki, Greece, JTD Science Editor was honored to have an interview with Dr. Paul Zarogoulidis, who has organized a special issue on “Pneumothorax: from definition to diagnosis and treatment” published in JTD before the congress, including the fine contributions from the congress president and participants. In the interview (Figure 1) as follows, Dr. Paul Zarogoulidis excitedly shared the novel technique of using the endobronchial ultrasound (EBUS) for pericardial effusion, which was proposed by Consultant Wolfgang Hohenforst-Schmidt, regional hospital of “Coburg”, Coburg, Germany.
Figure 1.

Dr. Paul Zarogoulidis is speaking at the interview by AME.
Interview
JTD: First of all, thank you very much for your great devotion to lead the special issue of pneumothorax for JTD. As a pulmonary physician, do you think how should the pulmonary physicians and thoracic surgeons work together to provide the best treatment for pneumothorax patients?
Dr. Paul Zarogoulidis: We have collaborations with several thoracic surgeons, and we need more multimodality approaches for pneumothorax. Usually, pulmonary physicians have minimally invasive treatments while the thoracic surgeons adopt more aggressive approaches. We need to have more multimodality approaches depending on different kinds of pneumothorax and different volumes of pneumothorax. Thoracic surgeons and pulmonary physicians have to present all their methods and to collaborate whenever necessary. Therefore, in many cases when the treatment of the pulmonary physicians is not going to plan, we need to collaborate with thoracic surgeons for substantial outcomes. Pulmonary physicians and thoracic surgeons always work together as a team.
What we do in Greece every year, including all of the experts of European society of thoracic surgeons, we organize meetings which last 2 or 3 days. We have forum speakers around the world, such as from China, from the United States, from Europe. Usually, we show novel techniques or repeat the ones that are already being done for the education of fellows.
JTD: Are there any controversies in the treatment of pneumothorax?
Dr. Paul Zarogoulidis: Thoracic surgeons use two ports, while pulmonary physicians one port. Pulmonary physicians use local sedation with xylocaine injection, while thoracic surgeons use general anesthesia. Upgrading the local anesthesia to general is not possible in most cases and therefore a careful planning is necessary for the treatment of patient in a case by case scenario.
JTD: In your speech on the congress, you talked about the EBUS as a diagnostic tool for lung disease. What do you think of the future of EBUS?
Dr. Paul Zarogoulidis: We can use this equipment for lung cancer diagnosis and in specific when have small lesions next to blood vessels like the pulmonary arteries. Of course there is no other equipment that can actually visualize the lymph nodes and make a targeted biopsy. Yesterday, I learned something that I didn’t know, although speaking of the EBUS. My very dear friend and former colleague Dr. Wolfgang Hohenforst-Schmidt told me that he uses the EBUS for pericardial effusion aspiration, so he can actually get through the pericardium and get the effusion fluid out with the EBUS needle. That is something very novel (Figure 2). Dr. Wolfgang Hohenforst-Schmidt can do that because he is both a pulmonary physician and cardiologist. He is an expert in EBUS and he can actually take out the fluid from the pericardium with EBUS needle, because the EBUS needle is empty from the inside, so you can actually put the EBUS needle within the pericardium and aspirate the fluid, so it is something amazing. And the next step I guess would be to use the EBUS to measure the pulmonary hypertension. This is something novel again. Regarding the future of EBUS, so it is not going to be used just for lung cancer or cancer metastasis diagnosis, but also for pulmonary hypertension.
Figure 2.
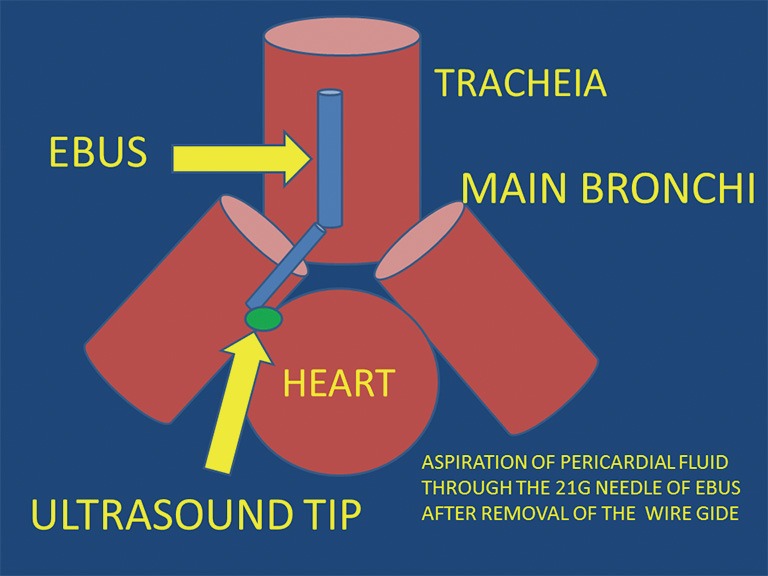
Aspiration of pericardial fluid through the 21 g needle of endobronchial ultrasound (EBUS) after removal of the wire gide.
JTD: As you are going to organize another special issue on pneumothorax, what will it be different from the first issue published in JTD?
Dr. Paul Zarogoulidis: As you already know, because we collaborate closely on the first special issue on pneumothorax, on the second special issue of pneumothorax we are going to speak about the minimal invasive techniques for the treatment of pneumothorax. The first issue was some unusual cases of pneumothorax, the second issue it will be more focused to the treatment of pneumothorax, we will present more equipment and more techniques with more figures. We are also going to present the anatomy of the pleura, and we will give more details regarding the mechanism or the other mechanisms of pneumothorax that we did not present in the first issue.
JTD: That would be great! We are all looking forward to this very special issue. Thank you very much for your wonderful sharing time!
Dr. Paul Zarogoulidis: Thank you for your collaboration throughout the special issue and throughout this year’s collaboration. It is always a pleasure and honor to work with Chinese colleagues.
JTD: Thank you very much!
Acknowledgements
Disclosure: The author declares no conflict of interest.


