Abstract
Introduction:
Radiotherapy (RT)-based curative regimens for head and neck squamous cell carcinomas (HNSCC) deliver a dose of 66–70 Gray (Gy) over a period of 6–7 weeks, and incomplete treatments are unlikely to result in cure. Non-compliance to RT is major contributory factor to treatment failure.
Aims:
To assess the proportion of patients who do not complete planned treatment after initiation of curative RT. This study also aims to explore a possible relationship of non-compliance due to socio-economic, disease-related and treatment-related factors.
Materials and Methods:
The records of HNSCC patients treated from January 2012–December 2013 were audited. Data from the treatment records were to collect patient-related, disease-related, and social demographic parameters. Of the patients who had not completed treatment, the reasons behind the same were investigated.
Results:
Of the 324 patients of HNSCC who were initiated on radical RT, a total of 76 patients were found to have discontinued treatment without authorization of the treating clinician. There was no significant predilection for treatment non-compliance with regards to patient age, educational status, religion, site of the disease, use of neoadjuvant chemotherapy, or use of concurrent chemotherapy. There tended to be a higher association of treatment non-compliance among patients residing >100 km away from the treatment center, patients hailing from hilly regions, patients without the below poverty line (BPL) card, unemployed patients, and patients with stage IV-A/B disease. Of the 76 patients who did not complete treatment, telephonic questionnaire could be obtained from 54 patients. Causes for non-compliance included preference for traditional healers (22.2%), fear of toxicity (7.4%), logistic reasons (18.5%), financial reasons (24.1%), and lack of interest/faith in RT (5.6%).
Conclusion:
There is a high incidence of treatment default among patients of HNSCC during RT in this region. The revelation of the higher propensity for treatment default among patients from distant, hilly regions, unemployed, patients without BPL cards, and stages-IVA/IVB highlights the need for specific interventions for these special populations.
Keywords: Head and neck cancer, Non-compliance, Radiotherapy, Socio-economic factors, Treatment default
INTRODUCTION
Curative treatment for head and neck squamous cell cancer (HNSCC) often involves the use of radiotherapy (RT) with or without concurrent chemotherapy. Compliance to the full course of treatment is an important determinant of success. However, a radical course of treatment spans for a protracted period of 6–7 consecutive weeks. Adverse effects can be severe, and may include mucositis, dermatitis, infections, and marrow toxicity. Nutritional status tends to be compromised due to exquisite mucosal toxicity.[1,2,3,4]
Given the fact that toxicities are anticipated as a rule rather than the exception, radiation oncologists do prepare the patient in advance to tide over the toxicity crisis. Measures such as nasogastric-tube insertions, symptomatic medications, and nutritional supplements are frequently used. Most radiation oncologists do undertake psychological counselling of the patients, so as to enable them to endure the difficult toxicities. Despite these preventive measures, one of the main causes for treatment failure in HNSCC is non-compliance to the planned course of treatment. This is however not provided due to emphasis as an avoidable cause for treatment failure.
The Kumaon region is one of the two major administrative divisions in the state of Uttarakhand in Northern India. The region of Kumaon comprises six districts (namely the districts of Pithoragarh, Bageshwar, Almora, Champawat, Nainital, and Udham Singh Nagar), and though the terrain is mainly montane, there are considerable plain terrain areas in the districts of Udham Singh Nagar and Nainital. The region is served by only one functional cancer institute, namely the Swami Rama Cancer Hospital and Research Institute, which is affiliated to the Government Medical College, Haldwani.[5,6]
The cross-section of patients visiting the center represents a mixture of patients from the hills, as well as the plains. The main cancer diagnosis which gets treated in this center happens to be HNSCC, attributable to a high prevalence of tobacco/alcohol abuse, along with a lack of cancer awareness.
However, a major cause of concern and dissatisfaction is the fact that a large number of patients earmarked for treatment with curative intent do not actually comply with the treatment plan. Thus, this study is the first of its kind, which attempts to elucidate the reasons causing patients not to adhere to the planned course of treatment.
MATERIALS AND METHODS
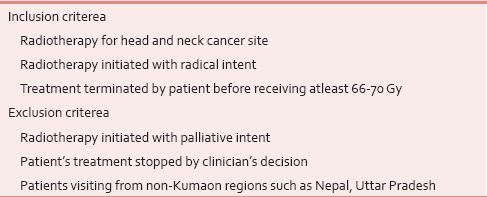
Patients with HNSCC treated with radical radiotherapy (either with RT alone, or concurrent chemoradiotherapy, with or without neoadjuvant chemotherapy) during the span of January 2012-December 2013 were included. Patients whose treatment was intentionally stopped by the clinicians’ decision were excluded from the study. Also, patients visiting from adjoining regions, such as the country of Nepal and the state of Uttar Pradesh were excluded to avoid socio-economic and cultural heterogeneity. The inclusion and exclusion criteria are mentioned in Table 1.
Table 1.
Inclusion and exclusion criterea
The social, economic, geographic, and cultural information were obtained from the patients’ treatment records. Non-compliance was defined as the premature termination of the planned treatment by the patient without consultation or recommendation from the treating clinician.
The proportion of patients non-compliant to treatment was assessed with regards to age, occupation, religion, educational status, distance of residence from hospital, geographical terrain at the patient's residence, stage of the disease, site of the disease, prior use of neoadjuvant chemotherapy, and the use of concurrent chemotherapy with RT.
Non-compliance was also assessed with regards to the below poverty line (BPL) status, which is a social assistance scheme provided by the Government of India for patients falling below the criteria set to define the poverty threshold. The criteria for BPL eligibility is revised frequently, and varies for urban and rural areas. (The interested reader is referred to the relevant documents made available by the Indian government).[7]
Data entry and analysis were performed by the use of LibreOffice 4 and Gnumeric 1.12. Proportions were compared with the Fisher exact test and P value below 0.05 was considered significant.
RESULTS
For the time span of January 2012-December 2013, a total of 324 patients of HNSCC were initiated on treatment with radical RT, of which 76 patients were noted to have discontinued RT without authorization by the treating clinician.
Social and economic factors such as age, occupation, religion, educational status, and BPL card status were considered for a possible association with treatment non-compliance [Table 2]. With regards to age, there was no significantly different rates of non-compliance among patients of age ranges: 18–40 years (20.6% non-compliance), 41–60 years (23.3% non-compliance), and >60 years (24.4% non-compliance).
Table 2.
Patient related and socioeconomic factors in relation with treatment non-compliance
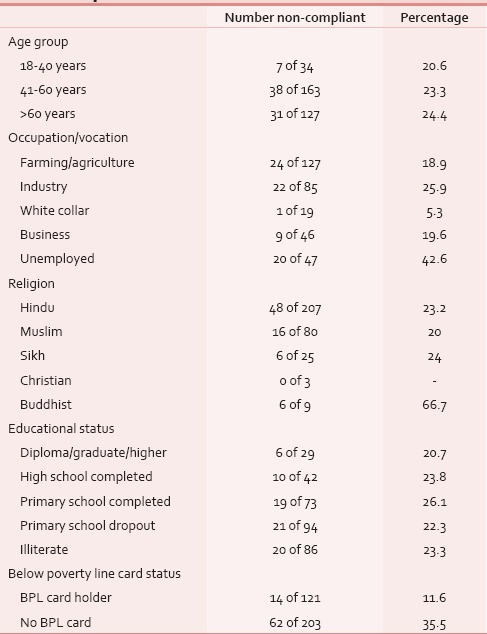
Patients’ occupational background had a major bearing on non-compliance. The percentage of non-compliance (in ascending order) was 5.3%, 18.9%, 19.6%, 25.9%, and 42.6%, respectively for white collar workers, farming workers, business persons, industrial workers, and unemployed persons. The rate of non-compliance was the highest among the unemployed (42.6%). This was a statistically significant difference when compared to patients involved in occupations (P = 0.0015). While occupational status did have an influence on the rate of non-compliance, there was surprisingly no influence of patients’ educational status upon compliance.
The percentage of patients defaulting among the commonest religions namely Hinduism, Islam, and Sikhism were 23.2%, 20%, and 24%, respectively, with the differences being statistically insignificant. However, there was a significantly (P = 0.0064) higher non-compliance rate among Buddhist patients (66.7%). Though comprising only nine patients, these patients mostly are either descendants of Tibetan refugees, or citizens of India hailing from remote Himalayan villages.
There was a higher non-compliance rate for patients without the BPL cards when compared to patients holding BPL cards (30.5% vs. 11.6%, P = 0.0001).
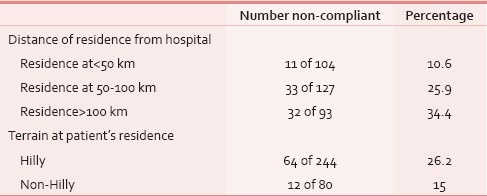
Patients with residences <50 km from the treatment center were very less likely to default planned course of treatment in comparison to patients who were living at distances greater than 50 km (11.8% vs. 41.9%, P = 0.0001) [Table 3]. Patients from hilly regions were more likely for non-compliance than patients from non-hilly regions (26.2% vs. 15%, P = 0.0476).
Table 3.
Patient's location of residence in relation to non-compliance
Lastly, disease and treatment related factors were analyzed in relation to treatment non-compliance [Table 4]. A very low proportion of patients belonged to stages I-III, making up a mere 11.6% of the total patients. Rest of the patients (88.4%) were staged IV-A/B. There was a greater non-compliance rate among patients with stages IV-A/B than in comparison to patients with stages I-III (13.3% vs. 33.8%), a difference which was almost statistically significant (P = 0.0538). No significant difference was observed with regards to the sub-site location of disease.
Table 4.
Disease and treatment related factors in relation to treatment non-compliance
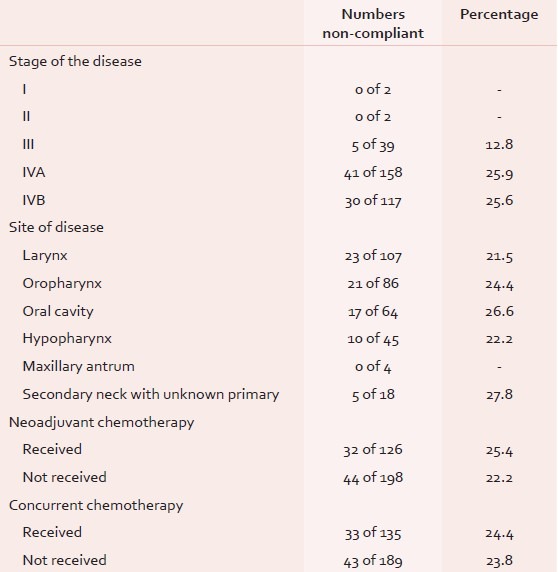
Many patients especially with T4b and N3 nodal status (n = 86) were treated with neoadjuvant chemotherapy prior to initiation of radical radiotherapy/chemoradiotherapy. The extended duration of overall treatment due to addition of neoadjuvant chemotherapy had no bearing on the rate of non-compliance to RT. There was no significant difference between patients who had received, or not received neoadjuvant chemotherapy (25.4% vs. 22.2%, P = 0.5908).
The use of concurrent cisplatin chemotherapy is preferred over the use of radiotherapy alone for patients with HNSCC. However, a significant proportion of these patients are treated with RT alone due to contraindications for concurrent chemotherapy such as advanced age beyond 70 years, poor performance status, and compromised renal function. The rate of non-compliance for patients treated with RT alone vs. concurrent chemoradiotherapy was 24.4% vs. 23.8%, respectively (P = 0.7905).
DISCUSSION
Successful outcome of RT-based treatment for HNSCC largely depends upon the total dose delivered. A minimum of 66-70 Gy (in conventionally fractionated doses) is required for a treatment regimen to be termed as “curative/radical” in intent.[8,9] Non-compliance to RT is a serious issue, since it not only results in incurability, but could also alter the natural progression of the disease for the worse. Sub-curative doses of radiation can result in the onset of accelerated-repopulation, and makes subsequent re-initiation of therapy difficult.[10,11] However, this is a neglected issue, and the adverse impact of non-compliance upon the cure-rates is often not provided due emphasis.
It has been acknowledged in previous studies that there is a high non-compliance rate among HNSCC patients treated with RT. Mohanti et al. analyzed 2,167 HNSCC patients treated with radical/palliative RT and observed only a 56% compliance rate.[12] Sharma et al. in their study confined to elderly HNSCC patients also observed non-compliance to be a major obstacle to intended treatment, with a compliance rate of only 62%.[13] Our study with a sample size of 324 patients has revealed a 23.5% rate of non-compliance.
Our study also assessed factors (socioeconomic, disease related, and treatment related) for a possible association with non-compliance. Patients’ age and educational status did not have any significant impact upon non-compliance rates. There was no relation with regards to major religions namely Hinduism, Islam, and Sikhism. There was a very high rate of non-compliance for Buddhist patients. This could be explained by the fact that these patients were often descendants of Tibetan refugees, or Indian citizens hailing from very far flung remote trans-Himalayan villages, mostly close to the Indo-Sino border.
Unemployed patients were more likely to default than those with some form of employment. This highlights the need for special emphasis upon additional attention and support for unemployed and financially challenged cancer patients. An unusual observation in this study was that there was higher non-compliance rate among patients without the BPL cards when compared to patients with BPL cards (30.5% vs. 11.6%, P = 0.0001). This was possibly due to the fact that BPL card holders were given free RT as per government rules (while BPL card non-holders were charged a nominal fee).
When disease-related factors were analyzed, patients with advanced stage disease defaulted more often. It is possible that patients presenting at advanced stages could be more defeatist in their approach owing to the lower cure likelihood. It could also be possible that patients with advanced stages usually warrant a larger irradiated tissue volume which leads to higher toxicities, and thus higher likelihood of non-compliance.
A rather pleasant observation was that there was no increased non-compliance with the addition of concurrent or neoadjuvant chemotherapy. These results must however be viewed with caution, since the addition of concurrent chemotherapy to RT is known to increase toxicity.
We could only establish communication with 54 of 76 patients who had not complied with treatment. When these patients were telephonically asked about the prime reason as to their non-compliance with treatment [Figure 1], the most commonly cited reason was “financial difficulties” (24.1%). Despite the provision of extremely subsidised treatment, patients cited that staying for 2 months in a new city for the purpose of RT is in itself an expensive undertaking.
Figure 1.
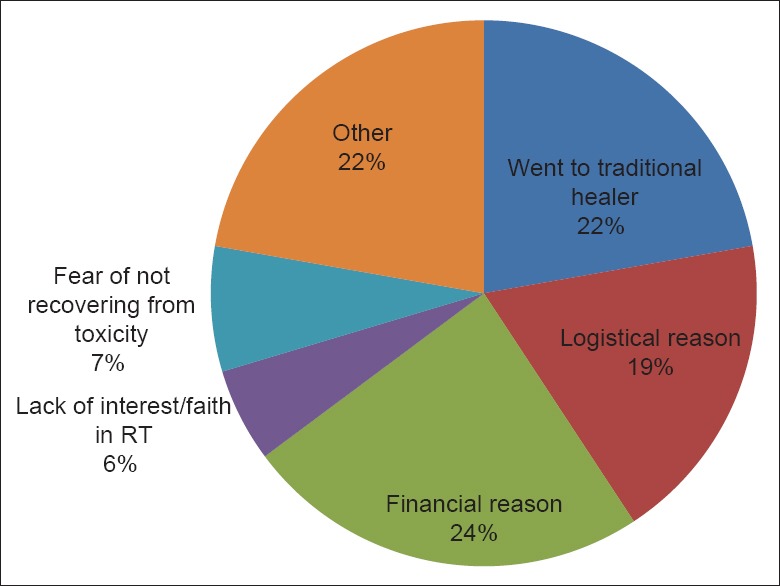
Cited reason as to explain non-compliance
The second most commonly cited reason was that the patients (22.2%) preferred traditional healers. This is possibly a situation unique to the Himalayan region, where the belief in traditional medicines is rather strong.
Logistical reasons (18.5%) were the third common cited reason. This is again likely to be unique to the region, since many patients travel from hilly terrain, which often gets subjected to natural difficulties such as landslides during autumns, and snow-blockade of roads during winters. Indeed, being the only RT center in the Kumaon region, patients travel for long distances, across difficult terrain for treatment. It was observed that there was a significantly higher non-compliance rate among patients with residences >50 km away from the treatment center, in comparison to those staying at lesser than 50 km (41.9% vs. 11.8%; P = 0.0001).
Understanding that about one in four patients in our center had defaulted treatment, we have since the study initiated many measures so as to curb non-compliance. All patients are now as a rule contacted via telephone if in case they fail to report for treatment for more than three consecutive days (the earlier practise in our institution was to perform weekly evaluations of patients, and there was no fixed mechanism in place to trace patients who defaulted from treatment). Defaulting patients are now contacted and provided detailed information about the impact of non-compliance upon prognosis, and are invited to return back to treatment. Patients hailing from distant regions are provided priority for admission in the wards, and also patients with poor financial background are offered charity in collaboration with governmental and non-governmental agencies.
Limitations of the study
Even though new insights have been gained with regards to treatment non-compliance among HNSCC patients, we have to admit a few shortcomings of this study. The study was designed to involve patients during a short span of 2 years only, since full-fledged RT was initiation in this center as early as 3 years ago. We had obstacleswith regards to establishing communication and it was impossible to meet patients/relatives for face-to-face meetings. Though questionnaires were prepared for use in interviewing defaulting patients, it could not actually be used since tracking patients from the mountainous terrain of the state of Uttarakhand requires immense amounts of time, manpower, and costs. Though telephone contact was established with 54 defaulting patients, we could not establish any sort of contact with 22 patients or their relatives.
CONCLUSIONS
Among patients with HNSCC, successful outcome from radiation-based treatment largely depends upon treatment compliance, since total dose of at least 66-70 Gy of conventionally fractionated dose is a basic minimum requirement if a treatment regimen is to be termed as “curative.” However, in the Indian scenario, one of the commoner (yet least spoken of) cause of treatment failure happens to be treatment non-compliance. This study reveals that almost one in four of the HNSCC patients initiated on radical RT will not comply with the treatment plan. There was higher likelihood of non-compliance among patients who were unemployed, patients who lived far away from the treatment center, patients hailing from hilly regions, those without BPL cards and, patients with advanced stages. Special attention in the future will hence have to be provided to these sub-sections of the population given the understanding that they are more likely to non-comply with ideal treatment plans. Effective plans need to be devised to track and communicate with patients who absent themselves from treatment.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Nugent B, Lewis S, O’Sullivan JM. Enteral feeding methods for nutritional management in patients with head and neck cancers being treated with radiotherapy and/or chemotherapy. Cochrane Database Syst Rev. 2013;1:CD007904. doi: 10.1002/14651858.CD007904.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins R, Flynn A, Melville A, Richardson R, Eastwood A. Effective health care: Management of head and neck cancers. Qual Saf Health Care. 2005;14:144–8. doi: 10.1136/qshc.2005.013961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campos MI, Campos CN, Aarestrup FM, Aarestrup BJ. Oral mucositis in cancer treatment: Natural history, prevention and treatment. Mol Clin Oncol. 2014;2:337–40. doi: 10.3892/mco.2014.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Overgaard J, Alsner J, Eriksen J, Horsman MR, Grau C. Importance of overall treatment time for the response to radiotherapy in patients with squamous cell carcinoma of the head and neck. Rays. 2000;25:313–9. [PubMed] [Google Scholar]
- 5.Pandey KC, Revannasiddaiah S, Pant NK, Bhatt HC. Stage-wise presentation of non-metastatic head and neck cancer: An analysis of patients from the Kumaon hills of India. Asian Pac J Cancer Prev. 2014;15:4957–61. doi: 10.7314/apjcp.2014.15.12.4957. [DOI] [PubMed] [Google Scholar]
- 6.Bag A, Rawat S, Pant NK, Jyala NS, Singh A, Pandey KC. Cancer patterns in Nainital and adjoining districts of Uttarakhand: A one year survey. J Nat Sci Biol Med. 2012;3:186–8. doi: 10.4103/0976-9668.101911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. [Last accessed on 2014 Oct 23]. Available from: http://www.pbplanning.gov.in/pdf/BPL16-3-07.pdf .
- 8.Taylor JM, Withers HR, Mendenhall WM. Dose-time considerations of head and neck squamous cell carcinomas treated with irradiation. Radiother Oncol. 1990;17:95–102. doi: 10.1016/0167-8140(90)90096-f. [DOI] [PubMed] [Google Scholar]
- 9.Sadat F, Wienke A, Dunst J, Kuhnt T. Survival of patients with head and neck cancer. Impact of physical status and comorbidities. Strahlenther Onkol. 2012;188:62–70. doi: 10.1007/s00066-011-0009-8. [DOI] [PubMed] [Google Scholar]
- 10.Withers HR, Taylor JM, Maciejewski B. The hazard of accelerated tumor clonogen repopulation during radiotherapy. Acta Oncol. 1988;27:131–46. doi: 10.3109/02841868809090333. [DOI] [PubMed] [Google Scholar]
- 11.Yang J, Yue JB, Liu J, Yu JM. Repopulation of tumor cells during fractionated radiotherapy and detection methods (Review) Oncol Lett. 2014;7:1755–60. doi: 10.3892/ol.2014.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohanti BK, Nachiappan P, Pandey RM, Sharma A, Bahadur S, Thakar A. Analysis of 2167 head and neck cancer patients’ management, treatment compliance and outcomes from a regional cancer centre, Delhi, India. J Laryngol Otol. 2007;121:49–56. doi: 10.1017/S0022215106002751. [DOI] [PubMed] [Google Scholar]
- 13.Sharma A, Madan R, Kumar R, Sagar P, Kamal V, Thakar A, et al. Compliance to therapy–elderly head and neck carcinoma patients. [Last accessed on 2014 Oct 22];Can Geriatr J. 2014 17:83–7. doi: 10.5770/cgj.17.101. Available from: http://www.cgjonline.ca/index.php/cgj/article/view/101/196 . [DOI] [PMC free article] [PubMed] [Google Scholar]


